Abstract
Background
Anticoagulant therapy with heparin is the first-line treatment for acute mesenteric vein thrombosis and is effective in improving outcomes. Conversely, patients with failed early anticoagulant therapy occasionally develop bowel infarction requiring surgery. The efficacy of long-term anticoagulant therapy on recanalizing mesenteric vein thrombosis in patients with failed early anticoagulant therapy remains unclear. Herein, we report a patient who achieved recanalization of port-superior mesenteric vein thrombosis treated with anticoagulant therapy for 10 years after failed early anticoagulant therapy, followed by bowel resection.
Case presentation
A 38-year-old male patient visited an outpatient clinic due to acute exacerbation of abdominal pain that had persisted for a month. He was diagnosed with port-superior mesenteric vein thrombosis on contrast-enhanced computed tomography (CT) scan and was transferred to our institution. Although he presented with abdominal pain, his respiration and circulation were stable upon hospital arrival. Anticoagulant therapy with heparin was started, and the patient was admitted to the intensive care unit. However, the patient’s abdominal pain worsened, and he began to develop signs of peritonitis. Repeat CT scan revealed bowel infarction. Thus, the patient underwent bowel resection 6 h after admission. The initial surgery was completed with open abdomen management. Bowel anastomosis was performed on the second-look surgery on the first postoperative day. Finally, the abdomen was closed on the third postoperative day after confirming the absence of bowel ischemia progression. The patient had prolonged impaired bowel function with paralytic ileus, but was discharged on the 60th postoperative day. He was then diagnosed with protein C and S deficiency based on the tests performed. Anticoagulant therapy with warfarin was initiated. He also received anticoagulant therapy in the outpatient setting. The patient’s port-superior mesenteric vein thrombosis had improved gradually with warfarin during the follow-up period. At 10 years after surgery, total occlusion of the port-superior mesenteric vein was recanalized with improvement of the portal collateral vessels. In addition, no gastric or esophageal varices were observed.
Conclusions
Long-term anticoagulation therapy could affect the recanalization of extensive thrombus in multiple segments in patients with mesenteric venous thrombosis.
Similar content being viewed by others
Background
Mesenteric venous thrombosis (MVT) accounts for < 10% of all mesenteric infarction cases [1]. Anticoagulant therapy with heparin is the first-line therapy for acute MVT and is effective in improving outcomes [2]. Conversely, patients with failed early anticoagulant therapy occasionally develop bowel infarction requiring surgery. Recanalization of MVT is dependent on the spread of the thrombus [3]. The efficacy of long-term anticoagulant therapy in recanalizing different types of MVT in patients with failed early anticoagulant therapy remains unclear. Herein, we report a patient who underwent recanalization of port-superior MVT treated with anticoagulant therapy for 10 years after failed early anticoagulant therapy, followed by bowel resection.
Case presentation
A 38-year-old male patient visited the emergency department of an acute-care hospital because of acute exacerbation of abdominal pain that had persisted for a month. He was previously diagnosed with Wolff–Parkinson–White syndrome and was under observation due to no history of arrhythmia. Although his general condition was stable, he presented with strong spontaneous pain and tenderness at the upper abdomen. Consequently, he was admitted to the hospital and was followed-up. He underwent abdominal contrast-enhanced computed tomography (CT) scan on the next day. Results revealed an extensive thrombus from the intrahepatic portal vein to the supra-mesenteric vein without findings of thrombus in other regions or embolization in the arterial system. The patient was diagnosed with port-superior MVT and was transferred to a tertiary hospital.
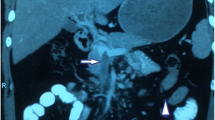
Upon hospital arrival, he was alert, and his vital signs were stable (respiratory rate: 12 cycles/min, heart rate: 69 beats/min with sinus rhythm, and blood pressure: 135/74 mmHg). He complained of diffuse abdominal pain with localized mild upper abdominal tenderness. Laboratory test results were almost normal except for the following: white blood cell count, 15,700/μL; C-reactive protein level 3.2 mg/dL, prothrombin time international normalized ratio, 1.46; and D-dimmer level 21.9 μg/mL. CT scan performed in a previous hospital revealed the development of collateral blood vessels around the portal vein, and there was no reduction in the contrast effect on the bowel wall (Fig. 1). Hence, the symptoms could have been caused by chronic MVT. The patient was managed with conservative therapy particularly anticoagulation therapy using heparin in the intensive care unit. However, he complained of abdominal pain exacerbation 6 h after admission. He underwent repeat abdominal CT scan. Results revealed increased peritoneal ascites and reduced contrast effect on the small intestine wall in the right upper quadrant (Fig. 2). Small bowel infarction was strongly suspected, emergent laparotomy was performed.
During emergent laparotomy, we found approximately 500 mL of light-brown ascites in the peritoneal cavity and a 90-cm-long ileum, which was 210 cm away from the Treitz ligament to the anal side, discolored with dark brown color and sclerotic. The ileum that was evidently necrosed was partially resected. Moreover, temporary abdominal closure with the Barker method for the purpose of a second-look surgery was introduced. On postoperative day (POD) 1, a part (50-cm-long) of the small intestine was additionally resected, and anastomosis was created via hand sewing using the end-to-end Albert–Lembert suture. Abdominal compartment syndrome had been a cause of concern because the whole bowel was edematous. Open abdomen was continued for several days. Open thrombectomy was not performed due to the absence of progression in intestinal necrosis after the initial surgery. The abdomen was closed on POD 3 after bowel edema improvement.
Paralytic ileus developed after surgery and lasted long. Although anticoagulation therapy with heparin was administered during the perioperative period, oral warfarin was initiated after paralytic ileus improvement. The patient was tested for various coagulation abnormalities during hospitalization and the protein C and S activities was reduced by 20% and 46.7%, respectively. In addition, protein C antigen was reduced by 23%. However, the patient did not have a family history of thrombosis. He was evaluated by an in-house hematologist. The patient was discharged on foot on POD 60.
He was followed-up at the outpatient clinic every 3 months. Anticoagulation therapy with warfarin was continued. During follow-up, he was referred to the department of hematology of a university by our in-house hematologist. Protein C and S deficiency was diagnosed. Although the genetic diagnosis including family members was proposed, the patient declined the offer, and no further test was conducted. The patient was initiated on lifetime anticoagulant therapy. For follow-up evaluation of portal hypertension, esophago-gastroduodenal endoscopies and contrast-enhanced CT scans were performed on postoperative years 3, 5, and 10. Endoscopies showed neither gastrointestinal ulcer nor gastroesophageal varices. CT scans revealed gradual recanalization, and the port-superior mesenteric vein was eventually recanalized with improvement of the collateral vessels around the portal vein on postoperative year 10 (Figs. 3 and 4). During the 10-year period, the patient did not experience any event suggesting thrombosis or embolus at other sites.
Axial view of computed tomography scans showing changes in port-superior mesenteric venous thrombus and collateral vessels over time. Thrombus in the portal vein (arrows) disappeared three years later, and the diameter of the portal vein increased over time. Collateral vessels around the portal vein improved over time. Stenosis of superior mesenteric vein (dotted arrows) gradually improved compared with the superior mesenteric artery (arrowheads)
Discussion
The pathogenesis of MVT is mainly divided into three mechanisms: inflammatory process around the vein, local venous congestion due to portal hypertension, and thrombophilia [4]. Anticoagulation therapy is the mainstay therapy for MVT regardless of cause. If the therapy is introduced at an early stage, the recanalization rate is as high as > 80% [2]. However, progression to bowel ischemia requiring surgery is significantly frequent in genetic hypercoagulable disorders [5]. To prevent progression and recurrence of thrombosis, after the initial therapy, the duration of anticoagulant therapy is at least 3–6 months [2]. Lifelong anticoagulation therapy is recommended in case of thrombophilia, as in our patient, recurrence of thrombus, or thrombosis, which can lead to severe clinical complications [2]. Combined protein C and S deficiency is rare, as in our patient [6]. Case reports of adult patients with combined protein C and S deficiency who developed acute venous mesenteric ischemia are shown in Table 1 [7,8,9,10].
Recanalization is associated with the extent of thrombus. Further, it is more frequently observed in patients with thrombosis involving the portal vein or superior mesenteric vein alone than in those with more extensive thrombosis [3]. In addition, patients with multi-segmental thrombus have a significantly lower survival [11]. A prospective study reported that the portal vein was patent in 39% of patients with anticoagulation therapy, the splenic vein in 80%, and the superior mesenteric vein in 73% after a median follow-up of 234 days [12]. Although the long-term recanalization rate remains uncertain [2, 5, 13], our case suggests that long-term anticoagulation therapy can affect the recanalization of thrombotic veins.
If there is extensive thrombus in multiple segments, thrombectomy is occasionally recommended. The role of open thrombectomy and endovascular thrombectomy is not clear [2, 4, 14, 15]. Open thrombectomy during surgery is considered an optional treatment [16]. However, intimal injury of the vessel could promote rethrombosis [2, 17].
Bleeding is the main adverse effect of anticoagulation therapy [2]. Generally, the recurrence risk without anticoagulation therapy is higher than the bleeding risk with anticoagulation therapy [11,12,13, 18]. The gastrointestinal tract is the main bleeding site in most cases, and the presence of gastroesophageal varices is a predictor of major hemorrhage [12, 13, 18]. Routine follow-up of gastrointestinal ulcer and gastroesophageal varices via endoscopies can be beneficial in reducing major bleeding. In our case, routine esophago-gastroduodenal endoscopy showed no findings of ulcer or varices development.
Conclusion
Herein, we present a patient who achieved recanalization of port-superior mesenteric vein thrombosis with long-term anticoagulant therapy after failed early anticoagulant therapy. Long-term anticoagulation therapy could affect the recanalization of extensive thrombus in multiple segments in patients with MVT.
Availability of data and materials
Not applicable.
Abbreviations
- CT:
-
Computed tomography
- MVT:
-
Mesenteric venous thrombosis
- POD:
-
Postoperative day
References
Bala M, Catena F, Kashuk J, De Simone B, Gomes CA, Weber D, et al. Acute mesenteric ischemia: updated guidelines of the World Society of Emergency Surgery. World J Emer Surg. 2022;17:54.
Bjorck M, Koelemay M, Acosta S, Bastos Goncalves F, Kolbel T, et al. Management of the disease of mesenteric arteries and veins: clinical practice guidelines of the European society of vascular surgery. Eur J Vasc EndoVasc Surg. 2017;53:460–510.
Condat B, Pessione F, Denninger MH, Hillaire S, Valla D. Recent portal or mesenteric venous thrombosis: increased recognition and frequent recanalization on anticoagulant therapy. Hematology. 2000;32:466–70.
Acosta S, Salim S. Management of acute mesenteric venous thrombosis: a systematic review of contemporary studies. Scand J Surg. 2020;110:123–9.
Andraska E, Haga L, Reitz K, Li X, Ramos R, Avgerinos E, et al. Acute superior mesenteric venous thrombosis results in high rates of readmission and morbidity. Vasc Surg Venous Lymphat Disord. 2020;8:748–55.
Formstone CJ, Hallam PJ, Tuddenham EG, Voke J, Layton M, Nicolaides K, et al. Severe perinatal thrombosis in double and triple heterozygous offspring of a family segregating two independent protein S mutations and a protein C mutation. Blood. 1996;87:3731–7.
Gorden MB, Beckman JA. Successful anticoagulation with hirudin in a patient with mesenteric venous thrombosis and multiple coagulation abnormalities. Vasc Med. 2000;5:159–62.
Choi BK, Yang SH, Suh KH, Hwang JA, Lee MH, Si WK, et al. A case of portal vein thrombosis by protein C and s deficiency completely recanalized by anticoagulation therapy. Chonnam Med J. 2011;47:185–8.
Ozdogan M, Gurer A, Gokakin AK, Kulacoglu H, Aydin R. Thrombolysis via an operatively placed mesenteric catheter for portal and superior mesenteric vein thrombosis: report of a case. Surg Today. 2006;36:846–8.
Rodríguez-Leal GA, Morán S, Corona-Cedillo R, Brom-Valladares R. Portal vein thrombosis with protein C-S deficiency in a noncirrhotic patient. World J Hepatol. 2014;6:532–7.
Thatipelli MR, McBane RD, Hodge DO, Wysokinski WE. Survival and recurrence in patients with splanchnic vein thromboses. Clin Gastroenterol Hepatol. 2010;8:200–5.
Plessier A, Darwish-Murad S, Hernandez-Guerra M, Consigny Y, Fabris F, Trebicka J, et al. Acute portal vein thrombosis unrelated to cirrhosis: a prospective multicenter follow-up study. Hepatology. 2010;51:210–7.
Condat B, Pessione F, Hillaire S, Denninger MH, Guillin MC, Poliquin M, et al. Current outcome of portal vein thrombosis in adults: risk and benefit of anticoagulant therapy. Gastroenterology. 2001;120:490–7.
Hiranuma W, Shimizu T, Takeda M, Matsuoka T, Minagawa T, Fukutomi T, et al. A case of superior mesenteric venous thrombosis managed by thrombectomy without bowel resection. Ann Vasc Dis. 2020;13:447–9.
Blumberg SN, Maldonado TS. Mesenteric venous thrombosis. J Vasc Surg Venous Lym Dis. 2016;4:501–7.
Klempnauer J, Grothues F, Bektas H, Pichlmayr R. Results of portal thrombectomy and splanchnic thrombolysis for the surgical management of acute mesentericoportal thrombosis. Br J Surg. 1997;84:129–32.
Hedayati N, Riha GM, Kougias P, Huynh TT, Cheng C, Bechara C, et al. Prognostic factors and treatment outcome in mesenteric vein thrombosis. Vasc Endovasc Surg. 2008;42:217–24.
Ageno W, Riva N, Schulman S, Beyer-Westendorf J, Bang SM, Senzolo M, et al. Long-term clinical outcomes of splanchnic vein thrombosis: results of an international registry. JAMA Intern Med. 2015;175:1474–80.
Funding
This study did not receive funding.
Author information
Authors and Affiliations
Contributions
IO: management and follow-up of the patient, writing original draft; MH: management of the patient; HY and SK: follow-up of the patient; SY: writing—review and editing.
All authors attest that they meet the current International Committee of Medical Journal Editors criteria for authorship and approve the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
A written informed consent for the publication of this case report was obtained from the patient.
Competing interests
The authors declare no competing interest for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Okada, I., Hagiwara, M., Yoneyama, H. et al. Recanalization of port-superior mesenteric vein thrombosis with long-term anticoagulant therapy after failed early anticoagulant therapy. surg case rep 10, 154 (2024). https://doi.org/10.1186/s40792-024-01948-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-024-01948-0