Abstract
Background
Complete resection of presacral epidermoid cysts is recommended due to the potential for infection or malignancy. Transsacral and transabdominal approaches have been used to treat presacral tumors. However, there are no standard surgical approaches to resection. We present the case of a presacral epidermoid cyst in an obese male patient who underwent laparoscopic transabdominal resection.
Case presentation
A 44-year-old man was referred to our hospital for treatment of a cystic tumor on the pelvic floor. Contrast-enhanced computed tomography revealed a 45 × 40-mm tumor on the left ventral side of the rectum, right side of the ischial spine, dorsal side of the seminal vesicles, and in front of the 5th sacrum. Enhanced magnetic resonance imaging revealed a multilocular cystic tumor with high and low signal intensities on T2-weighted images. The tumor was diagnosed as an epidermoid cyst. We considered the transsacral or laparoscopic approach and decided to perform a laparoscopic-assisted transabdominal resection since the tumor was in front of away from the sacrum, and a transsacral approach would result in a larger scar due to poor visibility from the thickness of the buttocks. The entire tumor was safely resected under laparoscopic guidance, because the laparoscopic transabdominal approach can provide a good and magnified field of view even in a narrow pelvic cavity with small skin incisions, allowing safe resection of the pelvic organs, vessels, and nerves while observing the tumor contour.
Conclusions
The laparoscopic transabdominal approach is an effective method for treating presacral tumors in obese patients.
Similar content being viewed by others
Background
An epidermoid cyst is a benign congenital tumor rarely found in the presacral cavity. Complete resection is recommended due to the risks of infection, fistula, and malignant transformation [1]. The deep pelvic cavity is narrow and full of blood vessels and vital nerves around the rectum; therefore, precise anatomical knowledge is required for surgery. Transsacral and transabdominal approaches have been used to treat presacral tumors. Recently, case reports on laparoscopic approaches have increased due to the advantages of magnified vision and accessibility to the pelvic floor [2, 3]. We selected the surgical approach considering the tumor location, size, and patient physique; however, it is still controversial which approach is better, and there is no standard for the selection of the surgical approach. Here, we present a case of a presacral epidermoid cyst in an obese man that was safely resected using a pure laparoscopic approach with good visibility.
Case presentation
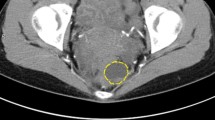
A 44-year-old man was referred to our hospital for treatment of a cystic tumor on the pelvic floor. He had been followed up for fatty liver disease at another hospital, and a presacral cystic tumor was unexpectedly detected on computed tomography (CT). He was highly obese, with a body mass index of 36.4 kg/m2. The tumor was neither palpable on digital rectal examination nor detected on colonoscopy. Tumor marker levels were within the normal range. Contrast-enhanced CT revealed a 45 × 40-mm tumor on the left ventral side of the rectum, right side of the ischial spine, dorsal side of the seminal vesicles, and in front of the 5th sacrum (Fig. 1a, b). The tumor contained highly and iso-dense areas with no enhancement effects. Enhanced magnetic resonance imaging (MRI) revealed a multilocular cystic tumor with high and low signal intensities on T2-weighted images (Fig. 2a, b). The tumor was diagnosed as an epidermoid cyst based on the imaging findings, and the patient was scheduled to undergo surgical treatment. We considered the transsacral or laparoscopic approach and decided to perform a laparoscopic-assisted transabdominal resection since the tumor was in front of away from the sacrum, and a transsacral approach would result in a larger scar due to poor visibility from the thickness of the buttocks.
The patient was placed in the lithotomy position. A 12-mm camera port was placed at the umbilicus, followed by the placement of a 12-mm port in the lower right quadrant of the abdominal region, and three 5-mm ports in the bilateral upper and left lower quadrants. We incised the peritoneum outside the sigmoid colon and entered the Toldt’s fusion fascia (Fig. 3a). We dissected the left side of the rectum and continued the dissection of the left side of the rectum, preserving the hypogastric nerves, and reached a capsulated tumor in the presacral cavity (Fig. 3b). The sparse connective tissue around the tumor was dissected with the ultrasonic scalpel and the electric scalpel (Fig. 3c). The base of the tumor was attached to the levator ani. The levator ani was partially resected with the tumor attached, without injuring the rectum (Fig. 3d). We placed the tumor in a tissue storage bag, lengthened patient’s umbilical wound slightly, then collected the tumor. The tumor was safely resected under laparoscopic observation. The operation time was 286 min, and total blood loss was 18 ml.
Intraoperative findings. We incised the peritoneum outside the sigmoid colon and entered into the Toldt’s fusion fascia (a). We dissected the left side of the rectum and proceeded to dissect the left side of the rectum preserving the hypogastric nerves, then reached a capsulated tumor in the presacral cavity (b). The sparse connective tissue around the tumor was dissected. The base of the tumor was attached to the levator ani (c). The levator ani was partially resected with the tumor attached, without injuring the rectum (d)
Macroscopically, the tumor size was 45 × 40 mm, and the cystic lesion contained yellowish-white atheromatous material (Fig. 4a). Microscopically, the wall of the cystic lesion was composed of a squamous epithelium with a granular layer and stratified keratin in the lumen (Fig. 4b). The pathological diagnosis was epidermoid cyst. The tumor did not invade the anal levator ani; however, the muscles were still resected with the tumor. There were no malignant tumor components. Although he had slight gluteal discomfort after surgery due to partial resection of the levator ani, it resolved within two months, and there was no anal dysfunction. The patient was discharged on postoperative day 8 with good progress. There was no recurrence within one year, and there were no noted symptoms.
Macroscopic and histological examination. Macroscopically, the tumor size was 45 × 40 mm, and a cystic lesion containing yellowish-white atheromatous material was observed (a). Microscopically, the wall of the cystic lesion was composed of squamous epithelium with a granular layer and stratified keratin in the lumen (b)
Discussion
Presacral tumors are estimated to occur in 1 in 40,000 hospitalizations, and the majority of tumors are reported in female (77%–94%) [4, 5]. The presacral cavity is surrounded anteriorly by the rectum, posteriorly by the sacrum/coccyx, cranially by the peritoneal reflection, and caudally by the anterior sacrococcygeal ligament and coccygeus muscle [4]. Various tumors arise in the presacral cavity due to the contact with the caudal end of the fetus and the aggregation of numerous fetal tissues, and these have been defined as developmental cysts [1, 6]. Developmental cysts are classified as dermoid, epidermoid, and tailgut cyst [1]. Dermoid and epidermoid cysts are composed of a squamous epithelium with a cheese-like keratin component without fluid [1]. Dermoid cysts contain skin appendages that distinguish them from epidermoid cysts [1]. Tailgut cysts are defined as mucinous-secreting cysts due to the remnants of the tailgut [1]. Most cases are asymptomatic and are incidentally identified by CT or MRI [4]. Surgical resection is recommended since the tumor is associated with infection and has malignant potential, such as squamous cell carcinoma arising from a presacral epidermoid cyst [3, 4, 7].
Surgical approaches include transsacral incision, transabdominal (laparoscopic), or a combination of both. Transsacral incision is an easy way to access the tumor without laparotomy. However, there are risks associated with the need for a large wound over 10 cm in size, postoperative anal dysfunction, fistula formation, and sacral nerve disorder [8]. Previous reports have cited that transsacral incision is a useful method when the tumor is located below S3, near the coccyx, or in the ischiorectal space [6, 9]. The laparoscopic transabdominal approach can help recognize the rectum, surrounding blood vessels, and nerves, especially due to a laparoscopic magnifying view with small incisions, whereas other reports suggest that the laparoscopic transabdominal approach is preferable when the tumor is located above S3 and is larger than 8 cm [4, 9]. Disadvantages of the transabdominal approach include the risk of injury to the vessels or nerves around the rectum and abdominal adhesions after surgery. In consideration of our case, we selected a laparoscopic transabdominal approach although the tumor location was below S3 and the tumor size was less than 8 cm that the transsacral incision was acceptable, because the tumor existed anterior to the rectum, separated from the sacrum in contact with the levator ani, and the patient was severely obese. If the transsacral approach is selected, it may be difficult to reach the tumor when it is anteriorly separated from the sacrum. Additionally, the transsacral approach may require a large incision, poor vision, and a narrow working space in obese patients with large buttocks. We considered that transsacral approach is suitable for the tumor which location was below S3 and close to the anterior of sacrum in non-obese patients. We would like to emphasize that the choice of surgical approach should consider not only the location, extent, and size of the tumor, but also the patient’s physique. The laparoscopic transabdominal approach can provide a good and magnified field of view even in a narrow pelvic cavity with small skin incisions, allowing safe resection of the pelvic organs, vessels, and nerves while observing the tumor contour. However, surgery for obese patients takes more operative time, blood loss, and increases the postoperative complications compared with non-obese patients [10]. Laparoscopic surgery of obese patients is hard to move small intestine for securing a field of view, and identify the exfoliation layer because of rich visceral fat. It is important to apply proper traction and counter-traction to exfoliation layer to avoid accidental injuries of nerves and vessels. We should consider strengthening the head position and adding another port when the sufficient field of view or proper traction were not secured. We could also consider preoperative weight loss before surgery because the tumor had no findings of malignancy or infection. Recently, there has been growing evidence that minimally invasive surgery, such as laparoscopic or robotic surgery, can be used successfully for lesions below the S3 level, even in obese patients [11]. The patient experienced no postoperative anal dysfunction in our case.
Conclusions
The laparoscopic transabdominal approach is effective for presacral tumors in obese patients.
Availability of data and materials
The datasets used in this report are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
References
Hawkins WS, Jackman RJ. Developmental cysts as a source of perianal abscesses, sinuses and fistulas. Am J Surg. 1953;86:678–83.
Zhou J, Zhao B, Qiu H, Xiao Y, Lin G, Xue H, et al. Laparoscopic resection of large retrorectal developmental cysts in adults: single-centre experiences of 20 cases. J Minim Access Surg. 2020;16:152–9.
Mohri K, Kamiya T, Hiramatsu K, Shibata Y, Yoshihara M, Aoba T, et al. Laparoscopic surgery of a presacral epidermoid cyst: a case report. Int J Surg Case Rep. 2019;59:23–6.
Riojas CM, Hahn CD, Johnson EK. Presacral epidermoid cyst in a male: a case report and literature review. J Surg Educ. 2010;67:227–32.
Jao SW, Beart RW Jr, Spencer RJ, Reiman HM, Ilstrup DM. Retrorectal tumors. Mayo Clinic experience, 1960–1979. Dis Colon Rectum. 1985;28:644–52. https://doi.org/10.1007/BF02553440.
Sakurai T, Mukai T, Kawachi H, Hiyoshi Y, Yamaguchi T, Nagasaki T, et al. Laparoscopic resection for a relapsed presacral epidermoid cyst penetrating the ischiorectal fossa. Asian J Endosc Surg. 2022;15:656–9.
Wu X, Chen C, Yang M, Yuan X, Chen H, Yin L. Squamous cell carcinoma malignantly transformed from frequent recurrence of a presacral epidermoid cyst: report of a case. Front Oncol. 2020;10:458.
Buchs N, Taylor S, Roche B. The posterior approach for low retrorectal tumors in adults. Int J Colorectal Dis. 2007;22:381–5.
Localio SA, Eng K, Ranson JHC. Abdominosacral approach for retrorectal tumors. Ann Surg. 1980;191:555–9.
Kashihara H, Shimada M, Yoshikawa K, Higashijima J, Tokunaga T, Nishi M, et al. The influence and countermeasure of obesity in laparoscopic colorectal resection. Ann Gastroenterol Surg. 2021;5:677–82.
Eftaiha SM, Kochar K, Pai A, Park JJ, Prasad LM, Marecik SJ. Robot-assisted approach to a retrorectal lesion in an obese female. J Vis Surg. 2016;2:59.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
There are no study sponsors or sources of funding.
Author information
Authors and Affiliations
Contributions
NY and KN conceptualized the study. TS, KF, KK, TY, and FF collaborated in patient care. JA performed pathological diagnosis. TI, NM, TS, HS, TH, NI, and FF provided input on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We obtained institutional review board approval from our Hospital (Approval No: 2023-156).
Consent for publication
Written informed consent was obtained from patient for publication of this case report and accompanying images.
Competing interests
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yoshida, N., Nakamura, K., Shigaki, T. et al. Laparoscopic transabdominal approach for resection of presacral epidermoid cyst in an obese man: a case report. surg case rep 10, 120 (2024). https://doi.org/10.1186/s40792-024-01924-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-024-01924-8