Abstract
Background
Left ventricle aneurysm (LVA) as a sequela to myocardial infarction or iatrogenic injury is required surgical treatment with full median sternotomy. Herein, we report a case of successful surgical treatment of left ventricle aneurysm performed by minimally invasive cardiac surgery (MICS).
Case presentation
We describe a case of a LVA treated by minimally invasive cardiac surgery in an 82-year-old woman who reported to the hospital with the complaint of chest pains at rest. Computed tomography (CT) coronary angiography revealed a left ventricle apical aneurysm. The aneurysm was suspected to be a pseudoaneurysm caused by a previous myocardial infarction. Surgery was performed under general anesthesia, with the patient in a supine position. A small incision was made in the 3rd intercostal space through which an aortic root vent cannula and aortic clamp were inserted, followed by exposing the aneurysm via incision of the left 6th intercostal space. The aneurysm was resected and pathologically examined, revealing it to be a “true” aneurysm. The left ventricle wall was closed using polypropene mattress sutures. Postoperative CT scan revealed successful resection of the aneurysm. Usually, a surgical treatment with full median sternotomy and left ventriculostomy is indicated for LVA. We decided to treat the LVA with bilateral thoracotomy MICS. We preferred to perform this procedure under cardiac arrest to ensure safe and secure closure of the aneurysm. The right small thoracotomy was necessary for aortic cross-clamping and aortic root venting.
Conclusions
The procedure was safe and simple and yielded excellent postoperative outcomes. Therefore, we speculate that this method can be applied to the management of larger aneurysms.
Similar content being viewed by others
Background
Aneurysm of the left ventricle that arises as a sequela to myocardial infarction or iatrogenic injury. An idiopathic left ventricle aneurysm is rare. Typically, a surgical treatment with full median sternotomy is required for the management of this lesion. Herein, we report a case of successful surgical treatment of left ventricle aneurysm performed by minimally invasive cardiac surgery (MICS).
Case presentation
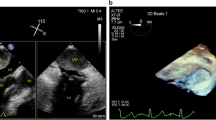
An 82-year-old female patient with a history of hypertension visited a local hospital after experiencing chest pains at rest during the night. As a result of suspected angina, coronary computed tomography (CT) angiography was performed, revealing an intact coronary artery; however, an apical aneurysm of the left ventricle was detected (Fig. 1a). Transthoracic echocardiography showed dyskinetic wall motion consistent with the left ventricle aneurysm. Based on the CT findings and clinical history of the patient, a vasospastic angina was suspected. The patient was started on a calcium-channel blocker, which relieved the symptoms effectively. The left ventricle apical aneurysm was caused by a previous myocardial infarction due to vasospastic angina. Therefore, we planned to conduct a surgical intervention for the aneurysm via MICS procedure.
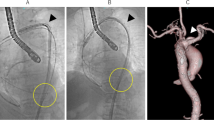
The patient was placed in a supine position with both arms raised (Fig. 2). General anesthesia was induced by a standard technique with a double-lumen tube for unilateral ventilation. Peripheral extracorporeal circulation was established via the right femoral artery and vein. An aortic root vent cannula and aortic clamp were inserted via the right 3rd intercostal space after creating a small incision. The aneurysm was exposed via a small incision of the left 6th intercostal space. When the left ventricle was filled with blood, an area of dyskinetic movement was detected, which was confirmed as an aneurysm on epicardial echocardiography. There was no adhesion or scarring from the old myocardial infarction. The aneurysm was 1.5 cm × 1.5 cm (Fig. 3a) in size. Cardiac arrest was achieved by administrating antegrade cardioplegia, and the aneurysm was resected. The left ventricle wall was closed using felt-pledgetted 3–0 polypropylene mattress suture (Fig. 3b). Operation time was 184 min.
The postoperative course was uneventful without any complications, and she was discharged after 14 days. Postoperative CT images revealed successful resection of the left ventricle aneurysm (LVA) (Fig. 1b). Pathological examination demonstrated that the cardiac muscle had little fibrotic and hypertrophic changes, and there was no evidence of secondary cardiomyopathy and cardiac infarction. Finally, the aneurysm was diagnosed as an idiopathic LVA.
Discussion
An LVA is an infrequent (5–10%) complication of myocardial infarction [1]. Other reported potential etiologies of LVAs are trauma, hypertrophic cardiomyopathy, cardiac sarcoidosis, and more exotic causes such as Chagas disease [2]. Cases of idiopathic LVA have also been reported, but the exact incidence is unknown. An idiopathic LVA is diagnosed by ruling out all possible etiologies of LVA based on the patient’s medical history, clinical examination, and laboratory test results [3, 4].
Usually, a surgical treatment with full median sternotomy and left ventriculostomy is indicated for LVA. Alternatively, closure via the left atrium and percutaneous closure have also been reported [5, 6]. However, to date, there has been no report on LVA closure with lateral thoracotomy MICS.
In this case, we decided to treat the LVA with bilateral thoracotomy MICS. Theoretically, “off-pump” closure or “on-pump beating” closure of the LVA was possible in the present case, which would have spared the right thoracotomy. However, we preferred to perform this procedure under cardiac arrest to ensure safe and secure closure of the aneurysm. Moreover, to achieve complete closure of the aneurysm at its neck, we considered it essential to get a clear view inside the aneurysm by adequate drainage of blood from the heart, and therefore root vent cannula was indispensable in order to prevent air embolism during cardiopulmonary bypass support. The right small thoracotomy was necessary for aortic cross-clamping and aortic root venting. Preoperative CT scan and transthoracic echocardiogram results obtained with the patient in the surgical position proved to be exceedingly useful for the selection of the left thoracotomy height. The left thoracotomy made it possible to approach the cardiac apex with ease, and a good field of view of the aneurysm was obtained. We believe that this technique has the potential to be applied to left ventriculoplasty for treatment of larger aneurysms. However, this technique can’t be applied if concomitant coronary artery bypass grafting is required.
Conclusions
We performed a successful operation for repair of LVA by MICS via bilateral thoracotomy. The procedure was safe and simple and yielded excellent postoperative outcomes. Therefore, we speculate that this method can be applied to the management of larger aneurysms.
Availability of data and materials
Not applicable.
Abbreviations
- LVA:
-
Left ventricular aneurysm
- MICS:
-
Minimally invasive cardiac surgery
References
Toda G, Iliev I, Kawahara F, Hayano M, Yano K. Left ventricular aneurysm without coronary artery disease, incidence and clinical features: clinical analysis of 11 cases. Intern Med. 2000;39:531–6.
Xia S, Wu B, Zhang X, Hu X. Left ventricular aneurysm in patients with idiopathic dilated cardiomyopathy: clinical analysis of six cases. Neth Heart J. 2009;17:475–80.
Altay H, Altin C, Coner A, Muderrisoglu H. Normal coronary artery patient presenting with left ventricular aneurysm. Case Rep Med. 2011;2011: 183050.
Leucker TM, Agrawal V, Rahim H, Price J, Jones SR. Idiopathic ‘true’ left ventricular aneurysm. J Cardiol Cases. 2015;12:202–4.
Da Col U, Di Bella I, Ramoni E, Affronti A, Rossi A, Ragni T. Repair of posterior left ventricular aneurysm through transatrial approach. J Card Surg. 2010;25:23–5.
Gladding PA, Ruygrok PN, Greaves SC, Gerber IL, Hamer W. Images in cardiovascular medicine. Percutaneous closure of a left ventricular free-wall rupture site. Circulation. 2006;113:e748–9.
Acknowledgements
The authors would like to thank Editage (www.editage.com) for English language editing.
Funding
None.
Author information
Authors and Affiliations
Contributions
SS, YK and SH performed the surgery. SS and HF were major contributors to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent to publish was obtained from the patient presented in this article.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kanazawa, Y., Saito, S., Shibasaki, I. et al. Minimally invasive cardiac surgery via bilateral thoracotomy in treatment of left ventricle aneurysm: a case report. surg case rep 9, 60 (2023). https://doi.org/10.1186/s40792-023-01640-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-023-01640-9