Abstract
Background
Polymyositis and myocarditis associated with thymoma are exceptionally rare conditions and usually accompanied by myasthenia gravis (MG) and have been recognized as critical conditions. Thymoma-associated multiorgan autoimmunity was reported recently with skin, liver, and intestinal manifestations similar to those seen in graft-versus-host disease.
Case presentation
A 77-year-old female presented to our department with exacerbation of ptosis and local recurrence of thymoma. Chest computed tomography revealed local recurrence of thymoma. Following 6 month observation, erythema on the extremities and body trunk suddenly appeared. Afterwards, the patient developed progressive muscle weakness and fatigue. We diagnosed as myocarditis and polymyositis. She was transferred to the intensive-care unit and received artificial ventilation. Steroid pulse therapy was induced immediately. The blood test findings were markedly improved, but the symptoms of MG and weakness of the muscles persisted. Various treatment including eculizumab was induced, and the symptoms of MG and weakness of the muscles were improved. On the 136th day of hospitalization, she was discharged.
Conclusion
We were able to cure this patient, as we were able to start treatment immediately after the appearance of severe symptoms. An early diagnosis and treatment are important for curing such patients.
Similar content being viewed by others
Background
Polymyositis and myocarditis associated with thymoma are exceptionally rare conditions and usually accompanied by myasthenia gravis (MG). Since the first report of four autopsy cases, polymyositis and myocarditis associated with thymoma have gradually come to be recognized as critical conditions [1, 2]. Thymoma-associated multiorgan autoimmunity (TAMA) was reported recently with skin, liver, and intestinal manifestations similar to those seen in graft-versus-host disease (GVHD) [3]. We herein report a case with issues associated with multiple autoimmune diseases, including MG, GVHD-like erythroderma, polymyositis, and myocarditis.
Case presentation
A 77-year-old female presented to our department with exacerbation of ptosis and local recurrence of thymoma. Five years earlier, she had been diagnosed with an anterior mediastinal tumor with a symptom of ptosis and underwent thymectomy for type B2 thymoma of Masaoka stage II disease. Following the operation, her ptosis was well controlled with tacrolimus 3 mg/day, prednisolone 5 mg/day, and pyridostigmine 180 mg/day.
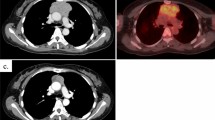
When she underwent an operation for colon cancer, chest computed tomography as a preoperative examination revealed local recurrence of a nodule 1 cm in diameter on the innominate vein and a small nodule in the anterior mediastinum (Fig. 1). We recommended radiotherapy for the recurrent lesions, but she wished to undergo observation for a while. She hoped to receive treatment for the exacerbation of ptosis.
The dose of tacrolimus was increased according to the trough value of the blood concentration, and her ptosis improved. The value of anti-acetylcholine receptor (AChR) antibody gradually decreased (71 to 10 nmol/L). Following 6 month observation, erythema on the extremities and body trunk suddenly appeared (Fig. 2), which was diagnosed as drug eruption. The drugs for MG were thus reduced or interrupted. The patient developed progressive muscle weakness and fatigue and was admitted to the hospital.
The post-administration course and blood examination values are shown in Fig. 3. Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels were significantly increased, and complication of drug-induced or autoimmune hepatitis was suspected. She slept in the sitting position, because her dyspnea worsened in the supine position. Her neck hung down without bulbar palsy symptoms. We once experienced a similar situation in an MG patient who died of myocarditis and polymyositis. She was transferred to the intensive-care unit (ICU) 5 days after admission and received artificial ventilation.
Post-administration course and blood examination values. Muscle weakness did not recover quickly, even after the abnormal values had normalized. Respiration assistance was continued. mPSL methylprednisolone, IAPP immunoadsorption plasmapheresis, IVIg intravenous immunoglobulin, ICU intensive-care unit, CK creatine kinase, ALT alanine aminotransferase, AST aspartate aminotransferase, LDH lactate dehydrogenase, anti-AChR antibody anti-acetylcholine receptor antibody
A laboratory examination performed immediately before treatment revealed that the serum levels of creatinine phosphokinase (3098 U/L; normal range 45–163 U/L), creatine kinase isozyme MB (257 U/L; normal range 45–163 U/L), ALT (311 U/L; normal range 6–27 U/L) and AST (351 U/L; normal range 13–33 U/L) were elevated. In addition, cardiac troponin I was elevated to 679.6 pg/mL (normal range 0–26.2 pg/mL). Serum electrolyte and calcium values were normal. The electrocardiogram at admission to the ICU showed only a slightly prolonged QT time (0.392 s). The echocardiogram demonstrated a preserved left ventricular systolic function, with an ejection fraction (EF) of 63%. There were no findings of cardiac infarction. Although a myocardial biopsy could not be performed, we diagnosed as polymyositis and myocarditis which is rarely associated with thymoma. This diagnosis was valid considering the positive findings of anti-striational autoantibodies (anti-titin and anti-Kv1.4), elevation of myosin light chain I and luck of elevation of anti-AChR antibody, which were revealed later.
The clinical course is shown in Fig. 3. Steroid pulse therapy was induced immediately for polymyositis and myocarditis. As the cardiac function was maintained, catecholamine administration was not needed. The blood test findings were markedly improved, as shown in Table 1, but the symptoms of MG and weakness of the muscles persisted. Therefore, we performed tracheostomy and immunoadsorption plasmapheresis (IAPP).
Pancytopenia and hypogammaglobulinemia (Good's syndrome) were also found, and intravenous immunoglobulin therapy was performed. She was also diagnosed with cytomegalovirus infection, and ganciclovir was administered. Eculizumab was induced, and the symptoms of MG and weakness of the muscles were improved. On the 136th day of hospitalization, she was discharged. Since then, immune therapy with medicine has been continued, excluding eculizumab. There has been no recurrence of any of her autoimmune diseases, excluding MG, for 1 year.
Discussion
We experienced a case with multiple autoimmune diseases, including MG, GVHD-like erythroderma, polymyositis, myocarditis, hypogammaglobulinemia, and pancytopenia. Thymoma is the most common tumor of the anterior mediastinum. It is often associated with autoimmune diseases. The representative disorder is MG, and thymomas are sometimes detected following the appearance of MG symptom. Complication only with MG has not been considered a poor prognostic factor of thymoma [4]. Meanwhile, other autoimmune diseases, such as pure red cell aplasia (PRCA) and hypogammaglobulinemia, are also widely recognized as being associated with thymoma, and these conditions are often found in patients with advanced disease or recurrence [5]. Treatment of advanced thymoma along with various autoimmune disease can, therefore, be complex.
TAMA is a recently delineated and rare paraneoplastic syndrome reported in patients with thymoma. The first report of TAMA described GVHD-like manifestations in the skin, liver, and intestines [3]. Since then, similar cases have been reported. Shiba et al. reviewed 29 cases of TAMA. Among those patients, 72.4% (21/29) had skin lesions, and 17 of those 21 cases with skin lesions had a fatal course [6]. Complications of TAMA, especially skin lesions, can thus lead to a poor prognosis. In the 29 patients with TAMA, complication with MG or PRCA was recognized, but polymyositis and myocarditis which were not found. However, 2 of the 29 patients died suddenly for no obvious reason. It may be possible that those patients were complicated with myocarditis. The present case showed a variety of symptoms, such as GVHD-like skin lesions, liver dysfunction, polymyositis and myocarditis, MG and PRCA, which were not mentioned in previous reports.
Polymyositis and myocarditis associated with thymoma are exceptionally rare and usually accompanied by MG [1, 2]. These entities are diagnosed in approximately 1% of patients with thymoma and are characterized by acute heart failure, ventricular arrhythmias, or heart block that rapidly develops a fatal course, usually within 10 days [7]. Notably, some cases do show a good response to steroid, azathioprine, and cyclosporine therapy. However, Tanahashi et al. reported that glucocorticoid pulse therapies were not effective [8]. Delayed detection of this disease may reduce the effectiveness of treatment. The present case was the second such case we had ever experienced [9]. Unfortunately, the first patient died before treatment could be administered, because we were unfamiliar with this disease and took a long time to diagnose it. The diagnosis of myocarditis associated with is not easy without performing an autopsy. This time, however, we were able to start steroid pulse therapy immediately after the diagnosis before the cardiac function had deteriorated. It took some time for the patient to recover her muscle strength due to the complication with MG, but she eventually recovered with a good course.
We administered eculizumab to the present patient. Eculizumab is a humanised monoclonal antibody that specifically binds with high affinity to human terminal complement protein C5. Recently, the REGAIN study showed that eculizumab was effective and well tolerated in patients with anti-acetylcholine receptor antibody-positive refractory generalized MG (gMG). Oyama et al. reported that patients with refractory gMG with myasthenia crisis and thymoma-associated MG were suitable for eculizumab administration. Whether or not eculizumab was effective in the present patient is unclear, but it can be expected to be effective against thymoma-associated MG and polymyositis and myocarditis, as both diseases are caused by autoimmune antibodies.
Conclusions
We experienced a rare case with multiple autoimmune diseases, including TAMA, polymyositis, and myocarditis. Fortunately, we could successfully treat this patient, as we were able to start treatment immediately after the appearance of severe symptoms. An early diagnosis and treatment are important for curing such patients.
Availability of data and materials
All data supporting this article are including in the published article.
Abbreviations
- MG:
-
Myasthenia gravis
- TAMA:
-
Thymoma-associated multiorgan autoimmunity
- GVHD:
-
Graft-versus-host disease
- AChR:
-
Anti-acetylcholine receptor
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- IAPP:
-
Immunoadsorption plasmapheresis
- PRCA:
-
Pure red cell aplasia
References
Giordano A, Haymondo J. Myasthenia gravis: a report of two cases with necropsy findings. Am J Clin Pathol. 1944;14:253–65.
Burke JS, Medline NM, Katz A. Giant cell myocarditis and myositis. Associated with thymoma and myasthenia gravis. Arch Pathol. 1969;88:359–66.
Wadhera A, Maverakis E, Mitsiades N, Lara PN, Fung MA, Lynch PJ. Thymoma-associated multiorgan autoimmunity: a graft-versus-host-like disease. J Am Acad Dermatol. 2007;57:683–9.
Nakajima J, Okumura M, Yano M, Date H, Onuki T, Haniuda M, Sano Y, Japanese Association for Research of Thymus. Myasthenia gravis with thymic epithelial tumour: a retrospective analysis of a Japanese database. Eur J Cardiothorac Surg. 2016;49:1510–5.
Moriyama S, Yano M, Haneda H, Okuda K, Kawano O, Sakane T, Oda R, Watanabe T, Nakanishi R. Pure red cell aplasia associated with thymoma: a report of a single-center experience. J Thorac Dis. 2018;10:5066–72.
Shiba K, Fujita Y, Miyazawa H, Muramatsu K, Watanabe M, Nishimura M, Shinkuma S, Nomura T, Nishie W, Taguchi J, Kinoshita I, Shimizu H. Thymoma-associated multi-organ autoimmunity: two cases and a review of the literature. J Eur Acad Dermatol Venereol. 2017;31:e324–6.
Davies MJ, Pomerance A, Teare RD. Idiopathic giant cell myocarditis—a distinctive clinoco-pathological entity. Br Heart J. 1975;37:192–5.
Tanahashi N, Sato H, Nogawa S, et al. A case report of giant cell myocarditis and myositis observed during the clinical course of invasive thymoma associated with myasthenia gravis. Keio J Med. 2004;53:30–42.
Sasaki H, Yano M, Kawano O, Hikosaka Y, Fujii Y. Thymoma associated with fatal myocarditis and polymyositis in a 58-year-old man following treatment with carboplatin and paclitaxel: a case report. Oncol Lett. 2012;3:300–2.
Kaplan M. Eculizumab (Alexion). Curr Opin Investig Drugs. 2002;3(7):1017–23.
Howard JF Jr, Utsugisawa K, Benatar M, Murai H, Barohn RJ, Illa I, Jacob S, Vissing J, Burns TM, Kissel JT, Muppidi S, Nowak RJ, O’Brien F, Wang JJ, Mantegazza R, REGAIN Study Group. Safety and efficacy of eculizumab in anti-acetylcholine receptor antibody-positive refractory generalised myasthenia gravis (REGAIN): a phase 3, randomised, double-blind, placebo-controlled, multicentre study. Lancet Neurol. 2017;16:976–86.
Oyama M, Okada K, Masuda M, Shimizu Y, Yokoyama K, Uzawa A, Kawaguchi N, Ikeguchi R, Hoshino Y, Hatano T, Ozawa Y, Nakahara J, Aizawa H, Kitagawa K, Hattori N, Kuwabara S, Murai H, Suzuki S. Suitable indications of eculizumab for patients with refractory generalized myasthenia gravis. Ther Adv Neurol Disord. 2020;13:1756286420904207.
Acknowledgements
Not applicable.
Funding
The authors declare that this study was not funded externally.
Author information
Authors and Affiliations
Contributions
CF, HN, and MY performed the surgery and management on the patient, RT and CF collected data. CF and MY have written the manuscript and HM reviewed and edited it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent for publication and presentation was obtained from this patient and her family.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Furuta, C., Yano, M., Numanami, H. et al. A case of thymoma-associated multiorgan autoimmunity including polymyositis and myocarditis. surg case rep 7, 226 (2021). https://doi.org/10.1186/s40792-021-01309-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-021-01309-1