Abstract
Background
There is a lack of evidence that multidrug use triggers adverse events. Therefore, the main purpose of this study was to clarify the relationship between the total number of drugs and number of high-risk prescriptions administered to Japanese elderly patients.
Methods
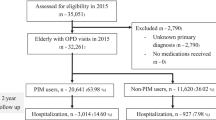
Using hospital electronic medical records (EMR), we evaluated the prescriptions of outpatients aged 65 years or older. We defined prescriptions of potentially inappropriate medications (PIMs) and overlapping prescription of drugs with the same mechanism of action (DSAs) as high-risk prescriptions. We analyzed the relationship among total number of drugs and high-risk prescriptions. In addition, we performed a secondary research to determine whether the hospitalization rate and concomitant medication contents differ depending on the high-risk prescriptions.
Results
Data for 13,630 outpatients were analyzed. A significant positive correlation between the numbers of total drugs and PIMs was found. The prescription frequency of individual PIMs rose as the total number of prescription drugs increased. The odds ratio (OR) of overlapping DSAs was significantly higher in patients using 5 or more drugs. In addition, there were significantly more prescriptions of laxatives among patients with overlapping prescriptions of anticholinergic drugs. The use of almost all PIMs was not an independent risk factor for hospitalization; instead, the number of PIMs was an independent risk factor for hospitalization [OR 1.18 (95% CI, 1.12–1.26)].
Conclusions
The number of PIMs and overlapping DSAs were high in patients receiving multidrug treatment. To avoid adverse events and hospitalization, it might be useful to review prescriptions and consider the number of PIMs and overlapping DSAs.
Similar content being viewed by others
Background
Multidrug use, often termed “polypharmacy,” has negative consequences [1, 2]. However, there is a lack of evidence that multidrug use triggers adverse events. Some reports suggested a relationship between the number of drugs and lower rate of adherence [3], risk of potential drug-drug interactions [4], and inappropriate prescriptions, such as potentially inappropriate medications (PIMs).
PIMs pose a high risk of adverse events in the elderly and should be avoided. Two sets of criteria for PIMs, the Beers criteria [5] and the Screening Tool of Older Persons’ Prescriptions (STOPP) [6, 7], are used globally. In Japan, the “Screening Tool for Older Persons’ Appropriate Prescriptions for Japanese (STOPP-J) [8]” is used. The use of drugs related to the Beers or STOPP criteria and the consequent under-prescribing of medications were reported to be frequent in patients receiving multidrug treatment [9,10,11]; similar reports were also published in Japan [12, 13]. We hypothesize that adverse events tend to occur in patients receiving multidrug treatment because of high-risk prescriptions. However, to date, a detailed analysis from this perspective has not been performed.
This study aimed to clarify the relationship between total number of drugs and high-risk prescriptions administered to Japanese elderly patients, and to clarify whether hospitalization rate and concomitant medication differ based on high-risk prescriptions used by these patients.
Methods
Survey method and subjects
This survey was conducted at Chiba University Hospital, which has 37 clinical departments conducting consultations for an estimated 2500 outpatients/day. Using the electronic medical records (EMR) system at this hospital, we surveyed prescriptions for outpatients aged ≥65 years who were presented at this hospital between October–December 2016 and prescribed at least one regular medication. All regular medications except for as-needed medications, injections, and topical drugs were analyzed.
Examination of prescriptions and hospitalization
We extracted 21 categories from the list of drugs that should be prescribed with special caution in the STOPP-J; these were defined as PIMs. In the STOPP-J, eight categories had limited disease and patient background, which were excluded from PIMs because it was impossible to extract their data from the EMR using our method.
To find overlapping of drugs with the same mechanism of action (DSAs), we surveyed drugs with anticholinergic effects (39 drugs) and benzodiazepine receptor agonists (22 drugs). DSAs include drugs with different medical effects. Because constipation is a typical adverse event of anticholinergic action, we considered that laxative prescription may be an indicator for the occurrence of adverse events.
We defined prescriptions of PIMs and overlapping prescription of DSAs as high-risk prescriptions. We examined the relationship between the number of drugs and high-risk prescriptions. We also investigated the number of hospitalizations that occurred for one year following the prescription survey (January to December 2017).
Statistical analysis
To compare the median values of PIMs, the Mann-Whitney U test was performed following the Kruskal-Wallis test. Correlation between the total number of prescribed drugs and number of PIMs was obtained using the Spearman’s rank correlation coefficient. For the prescription status of PIMs and overlapping DSAs, we performed a χ2 test or Fisher’s exact test, as appropriate. Logistic regression analysis was performed on the prescription of PIMs and the effect of the number of PIMs on hospital admission. All analyses were carried out using IBM SPSS Statics ver. 23 (IBM Corp., Armonk, NY). Significance was set to 5%, and correction for multiple comparisons was conducted using the Bonferroni method.
Results
Patient characteristics are shown in Table 1. A total of 11,241 elderly outpatients received at least one regular medication. As the total number of drugs increased, the prescription frequency of PIMs also increased (Table 2). For 17 of the 21 PIM categories, prescription frequency was significantly higher in the 5–9-drugs group than in the 1–4-drugs group. It was similar in the 10 or more-drugs group, compared to the 1–4-drugs group. A significant correlation was found between the number of PIMs and total number of prescribed drugs ((Fig. 1, Spearman’s r = 0.529, p < .001). The median number of PIMs was 0, 1, and 2 in the 1–4-, 5–9-, and 10 or more-drugs groups (p < .001 in each case), respectively.
Percentage of overlapping prescription of anticholinergics or benzodiazepine receptor agonists in the 5–9-drugs group was higher than in the 1–4-drugs group (Fig. 2). No significant difference in overlapping prescription for anticholinergics or benzodiazepine receptor agonists was found between the 5–9-drugs and 10 or more-drugs groups. Patients receiving overlapping prescriptions for anticholinergic drugs received significantly more prescriptions for laxatives [OR 2.44 (95% CI, 1.30–4.61)].
Overlapping drugs with the same mechanism of action. (a) Overlapping anticholinergic drugs (b) Overlapping benzodiazepine receptor agonists The χ2 test was used to compare the differences between each group (a,b). Correction with the Bonferroni method was performed, and p values < .017 were considered significant. *p < .017
In the year following the prescription survey, 1900 (16.9%) patients in the study were hospitalized (Table 3). We identified loop diuretics and nonsteroidal anti-inflammatory drugs (NSAIDs) as independent risk factors for hospitalization [OR 1.73 (95% CI, 1.38–2.16) and 1.29 (95% CI, 1.08–1.54), respectively]. The number of PIMs was an independent risk for hospitalization [OR 1.18 (95% CI, 1.12–1.26), p < .001], but not the use of PIMs other than loop diuretics and NSAIDs.
Discussion
This study showed that increases in the total number of drugs prescribed for outpatients were associated with the prescribing of more PIMs and more overlapping DSA. Previous reports on prescriptions for the elderly in Japan are limited. As this survey obtained similar results to those of other countries, increased PIMs due to multidrug use may be a common issue across countries. Presently, little information exists on the status of the prescription issuance of PIMs in the STOPP-J. Therefore, our findings may be useful for future medical care of the elderly in Japan.
Our findings showed that overlapping DSAs increased remarkably in the 5–9-drugs group compared to that in the 1–4-drugs group. We found many cases where laxatives were prescribed for patients receiving overlapping drugs with anticholinergic effects, suggesting that drug-induced constipation increased owing to the overlapping of drugs with anticholinergic effects. The proportion of overlapping DSAs was markedly higher in the 5–9-drugs group than in the 1–4-drugs group without significant difference. Kojima et al. reported that falling and other drug-related adverse events increase in elderly patients concurrently using more than 5 or 6 drugs [14, 15], and our results may explain one of these events.
We also found that the number of PIMs was an independent risk factor for hospitalization, but the use of PIMs except for loop diuretics and NSAIDs was not. The presence or absence of PIMs was reported to affect hospitalization [16, 17], and a high number of hospitalizations was indicated in patients using specific drugs, such as loop diuretics and NSAIDs [18, 19]. It was reported that the use of loop diuretics is more likely to lead to cardiac death and re-hospitalization, even after correction for differences in background factors, including the severity of heart failure [20]. Reports showed that the use of NSAIDs is the most common cause of drug adverse events in elderly people, and that the use of NSAIDs has increased [21]. We think that these reports support our results. However, all hospitalizations in our study were not the results of drug adverse events; thus, future studies are warranted.
To date, there are several reports that multidrug use is associated with adverse events and hospitalization [2, 14, 15, 22]. However, the mechanisms by which multidrug use increases these risks remain unknown. In addition, as mentioned above, PIMs affect adverse events and hospitalization. Our results clearly showed that multidrug use was correlated with increased high-risk prescriptions, i.e., the number of PIMs and overlapping DSAs. This result may be linked to increased risk of adverse events and hospitalization due to multidrug use. It was also reported that reviewing a patient’s prescription reduces the risk of re-hospitalization of the patient [23]. Therefore, reviewing high-risk prescriptions might prevent adverse events and hospitalization.
Our study had several limitations. First, our study analyzed only the drugs prescribed in our hospital. Therefore, it is possible that the results of this survey underestimated the actual state of prescription issuance. The total number of prescribed drugs was lower than that reported in other studies in Japan [12, 24]. Second, we did not examine any prescription changes during the study period. Third, we were unable to include hospitalization that occurred in other hospitals. In addition, our method could not be used to analyze, in-depth, the backgrounds of the hospitalized patients. There are several reports showing the relationship between multidrug use and frailty, decreased activities of daily living, decreased renal function, and worsening of nutritional status [24]. More knowledge can be obtained by identifying these conditions and conducting detailed analysis.
Multidrug use is often considered inappropriate under any circumstances. A more nuanced view holds that a combination of more drugs than necessary should be defined as “polypharmacy,” for distinction from appropriate multidrug combinations [25]. Our results may contribute to elucidate multidrug combinations that should be avoided.
Conclusion
This study revealed that the number of PIMs and overlapping DSAs were higher in patients receiving multidrug treatment, and that the number of PIMs was an independent risk factor for hospitalization. Reviewing prescriptions and considering the number of PIMs and overlapping DSAs may reduce adverse events and hospitalization.
Availability of data and materials
All data analyzed in this study are included in this published article.
Abbreviations
- DSAs:
-
Drugs with the same mechanism of action
- EMR:
-
Electronic medical records;
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- OR:
-
odds ratio
- PIMs:
-
Potentially inappropriate medications
- STOPP:
-
Screening Tool of Older Persons’ Prescriptions
- STOPP-J:
-
Screening Tool for Older Persons’ Appropriate Prescriptions for Japanese
References
Bourgeois FT, Shannon MW, Valim C, Mandl KD. Adverse drug events in the outpatient setting: an 11-year national analysis. Pharmacoepidemiol Drug Saf. 2010;19:901–10.
Saedder EA, Lisby M, Nielsen LP, Bonnerup DK, Brock B. Number of drugs most frequently found to be independent risk factors for serious adverse reactions: a systematic literature review. Br J Clin Pharmacol. 2015;80:808–17.
Stoehr GP, Lu SY, Lavery L, Bilt JV, Saxton JA, Chang CC, et al. Factors associated with adherence to medication regimens in older primary care patients: the Steel Valley seniors survey. Am J Geriatr Pharmacother. 2008;6:255–63.
Castilho ECD, Reis AMM, Borges TL, Siqueira LDC, Miasso AI. Potential drug-drug interactions and polypharmacy in institutionalized elderly patients in a public hospital in Brazil. J Psychiatr Ment Health Nurs. 2018;25:3–13.
American Geriatric Society. Beers criteria update expert panel. American geriatric society 2015 update beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227–46.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (screening tool of older Person’s prescriptions) and START (screening tool to alert doctors to right treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46:72–83.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: Version2. Age Ageing. 2015;44:213–8.
Kojima T, Mizukami K, Tomita M, Arai H, Ohrui T, Eto M, et al. Screening tool for older persons’ appropriate prescriptions for Japanese: report of the Japan geriatrics society working group on “guidelines for medical treatment and its safety in the elderly”. Geriatr Gerontol Int. 2016;16:983–1001.
Steinman MA, Landefeld CS, Rosenthal GE, Berthenthal D, Sen S, Kaboli PJ. Polypharmacy and prescribing quality in older people. J Am Geriatr Soc. 2006;54:1516–23.
Tommelein E, Mehuys E, Petrovic M, Somers A, Colin P, Boussery K. Potentially inappropriate prescribing in community-dwelling older people across Europe: a systematic literature review. Eur J Clin Pharmacol. 2015;71:1415–27.
Kuijpers MA, van Marum RJ, Egberts AC, Jansen PA, OLDY (OLd people Drugs & dYsregulations) Study Group. Relationship between polypharmacy and underprescribing. Br J Clin Pharmacol. 2008;65:130–3.
Hamano J, Tokuda Y. Inappropriate prescribing among elderly home care patients in Japan: prevalence and risk factors. J Prim Care Community Health. 2014;5:90–6.
Ogura F, Kimura T, Uda A, Toda A, Akazawa Y, Yamamoto K, et al. Pharmaceutical intervention to manage polypharmacy in elderly patients based on STOPP criteria. Iryouyakugaku. 2016;42:78–86.
Kojima T, Akishita T, Kameyama Y, et al. High risk of adverse drug reactions in elderly patients taking six or more drugs: analysis of inpatient database. Geriatr Gerontol Int. 2012;12:761–2.
Kojima T, Akishita M, Nakamura T, Yamaguchi K, Yamamoto H, Eto M, et al. Association of polypharmacy with fall risk among geriatric outpatients. Geriatr Gerontol Int. 2011;11:438–44.
Lau DT, Kasper JD, Potter DE, Lyles A, Bennett RG. Hospitalization and death associated with potentially inappropriate medication prescriptions among elderly nursing home residents. Arch Intern Med. 2005;165:68–74.
Endres HG, Kaufmann-Kolle P, Steeb V, Bauer E, Böttner C, Thürmann P. Association between potentially inappropriate medication (PIM) use and risk of hospitalization in older adults: an observational study based on routine data comparing PIM use with use of PIM alternatives. PLoS One. 2016;11:e0146811. https://doi.org/10.1371/journal.pone.0146811.
Wauters M, Elseviers M, Vaes B, Degryse J, Vander Stichele R, Christiaens T, et al. Mortality, hospitalisation, institutionalisation in community-dwelling oldest old: the impact of medication. Arch Gerontol Geriatr. 2016;65:9–16.
Price SD, Holman CD, Sanfilippo FM, Emery JD. Association between potentially inppropriate medications from the beers criteria and the risk of unplanned hospitalization in elderly patients. Ann Pharmacother. 2014;48:6–16.
Hamaguchi S, Kinugawa S, Tsuchihashi-Makaya M, et al. Loop diuretic use at discharge is associated with adverse outcomes in hospitalized patients with heart failure: a report from the Japanese cardiac registry of heart failure in cardiology (JCARE-CARD). Circ J. 2012;76:1920–7.
Cooper JW. Adverse drug reaction-related hospitalizations of nursing facility patients: a 4-year study. South Med J. 1999;92:485–90.
Marcum ZA, Amuan ME, Hanlon JT, Aspinall SL, Handler SM, Ruby CM, et al. Prevalence of unplanned hospitalizations caused by adverse drug reactions in older veterans. J Am Geriatr Soc. 2012;60:34–41.
Ravn-Nielsen LV, Duckert ML, Lund ML, Henriksen JP, Nielsen ML, Eriksen CS, et al. Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: a randomized clinical trial. JAMA Intern Med. 2018;178:375–82.
Komiya H, Umegaki H, Asai A, Kanda S, Maeda K, Shimojima T, et al. Factors associated with polypharmacy in elderly home-care patients. Geriatr Gerontol Int. 2018;18:33–41.
Hanlon JT, Schmader KE, Ruby CM, Weinberger M. Suboptimal prescribing in older inpatients and outpatients. J Am Geriatr Soc. 2001;49:200–9.
Acknowledgments
The prescription data was obtained from the planning information department of Chiba University Hospital. We would like to thank Editage (http://www.editage.jp) for English language editing.
Funding
This study was supported in part by JSPS KAKENHI Grant Number 18H00428 and AMED under Grant Number JP18dk0207027h0003.
Author information
Authors and Affiliations
Contributions
SA designed the study, analyzed and interpreted the data, and wrote the initial draft of the manuscript TI and HK contributed to analysis and interpretation of data and were involved in the important revision process of the manuscript YM, TN and TS contributed to analysis of data and critically reviewed the manuscript. M.K. verified the analytical methods KY and II supervised the project. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was conducted with approval from the Chiba University Graduate School of Medical Research Institute Ethics Review Committee (approval number 3090). Informed consent was formally waived by the Medical Research Institute Ethics Review Committee as data were collected from medical records and patients were not contacted. However, due to Japanese Ethical Guidelines, we displayed a poster in the waiting room of the hospital that consisted of the information regarding the collection and use of data for this study, and guaranteed the protection of personal information.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Arai, S., Ishikawa, T., Kato, H. et al. Multidrug use positively correlates with high-risk prescriptions in the Japanese elderly: a longitudinal study. J Pharm Health Care Sci 5, 20 (2019). https://doi.org/10.1186/s40780-019-0150-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40780-019-0150-6