Abstract
Purpose
To evaluate the radiographic and peri-implant outcomes of intramobile cylinder implants (IMZs) and the feasibility of long-term follow-up studies after nearly 30 years.
Methods
Of the 94 patients treated with IMZ implants between 1981 and 1995, 39 patients were successfully contacted (contact group, CG), of which 15 patients with a total of 32 implants agreed to participate in the present follow-up study (clinical evaluation group, CEG). The overall implant survival rate was calculated. Information on implant status and oral and general health data was collected. Marginal bone level was evaluated and then compared to the patients’ baseline data. Possible risk factors for peri-implantitis were also identified.
Results
In total, 16 implants in seven patients were lost, amounting to an overall survival rate of 79.5% after 30 years with a mean follow-up time of 24 ± 10 years (CG). Eight patients were treated with bar-retained mandibular overdentures and seven patients had fixed partial dentures. After a mean observation time of 29 ± 3 years, the surviving implants showed a peri-implantitis rate of 9.4% with a mean marginal bone loss of 2.5 ± 1.8 mm (CEG). No significant correlation between peri-implantitis and possible risk factors could be found.
Conclusions
Long-term follow-up studies with acceptable response rates after nearly 30 years are not feasible. Contact was only possible with 41% of the patients. This contact group showed a high implant survival rate. Due to the retrospective study design, additional risk factors could not be considered in a conclusive analysis.
Graphical Abstract

Similar content being viewed by others
Background
The discovery of osseointegration by Branemark in 1969 [1] opened up a multitude of new possibilities for restoring health, esthetics, and function in edentulous patients and those with extensive damage to their dentition. Therefore, implant therapy has revolutionized dental practice. Along with the implant ad modum Branemark, intramobile cylinder implants (IMZs) were among the first fixtures used in implant therapy. The IMZ implant system was particularly popular in the 1980s and the early 1990s, before it was replaced by the Camlog implant system in the late 1990s. The key component of the IMZ implant system is the intramobile element (IME), whose purpose is to simulate the viscoelasticity of the periodontal ligament and reduce the forces transmitted to the marginal bone–implant interface [2]. Since the implant and IME are rigidly connected, the IME serves to reduce the displacement differential between the osseointegrated implant and a natural tooth while also impeding the intrusion of natural teeth, which can occur if a nonrigid interlock is used [3]. Several previous studies have reported excellent results on survival rate and radiographic and clinical data [3,4,5,6,7]. However, to date, longitudinal studies with a follow-up period greater than 10 years are scarce. Previous prospective studies with a follow-up period of up to 10 years have reported findings on the IMZ Implant system [6, 8, 9]. There are also a few additional retrospective studies reporting on IMZ implants after a period of more than 10 years, but as implants of significantly lower age were also included in those studies, the overall mean observation time was considerably shorter [7, 10]. A literature search in MEDLINE on the IMZ Implant system regarding follow-ups with a mean observational period of at least 5 years reveals a total of four studies of heterogenous design shown in Table 1. Further, additional three studies report results after up to 13 years of follow-up without specifying the mean observation time. Although all authors report on implant survival or success rates, data on peri-implant conditions such as marginal bone loss is hardly mentioned [2,3,4,5,6,7,8,9,10,11]. While existing data indicate high survival rates of over 90% and minimal marginal bone-level changes of less than 2 mm after a period of 10 years [6], the long-term outcome of the IMZ implant system is still unknown, as there are no studies reporting data after at least 20 years.
Notably, middle-aged or younger patients with multiple agenesis are often treated with endosseous implants and are reliant on the function of their implants for many decades. Considering these patients’ age, longer observation periods than those typically seen in 5- to 10-year follow-up periods are appropriate and needed. While many aspects of implant design have changed over the years, the overall principle and structure of endosseous implants have remained unaltered. Importantly, data on older implant systems might provide valuable insights into long-term implant therapy, even with the current systems. Therefore, the aims of the present retrospective study were: 1) to examine the feasibility of implant therapy follow-up examinations after a mean observation time of at least 20 years; 2) to investigate the outcome of IMZ implant therapy providing clinical and radiographical long-term results.
Methods
Patient selection
In this study, patients treated with intramobile cylinder implants (IMZ) at the Department of Prosthodontics of the University Hospital of RWTH Aachen between 1981 and 1995 were preselected. The only additional selection criteria were the availability of baseline radiographs. Of the 94 possible candidates, 29 patients died and 26 were unavailable. In total, 39 patients with 78 implants were successfully contacted. Information on general health and implant status was gathered through telephone interviews and mail questionnaires (contact group = CG). In addition, archived patient records were consulted to calculate the implant survival rate in the CG. After excluding four patients who had moved to a new address far from the study location, five patients who did not want to participate due to senility, and 13 patients who lost all of the IMZ implants originally inserted, 17 patients agreed to participate in a clinical examination. There was no indication for radiographic examination in two patients, thus a total of 15 patients with 32 implants were included in the present follow-up study (clinical examination group = CEG) (Figs. 1, 2).
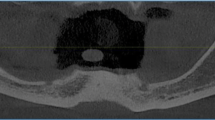
Clinical photographs and radiograph of a combined tooth–implant retained fixed partial denture in clinical examination group (CEG) after 26 years in situ. Note the radiolucent intramobile element (IME) between the IMZ implant and the superstructure as well as the transmucosal implant extension (TIE), which can be distinguished from the implant itself by a subtle radiolucent line.
Clinical analysis
During the follow-up examination, which was conducted from May–July 2017, information on oral and general health was collected. Patients were asked if they had been previously diagnosed with periodontitis, diabetes, or osteoporosis. Additionally, data on smoking habits were collected. The pocket probing depth (PPD) was measured at four sites for each implant (mesial, labial, distal, and oral) using a calibrated periodontal probe. Additionally, the average probing depth for each individual implant was calculated. At the same time, the BOP Index (bleeding on probing) was evaluated for each of the four implant sites. The bleeding points for each implant were counted, amounting to a maximal Bleeding Index of 4 for each implant. The width of the attached mucosa was measured using the same periodontal probe. The presence of plaque was assessed using the index according to Mombelli et al. [12]. PIaque Index (PI) was also evaluated at four sites, but only the highest index value for each implant was used for the analysis. Furthermore, implants were categorized into two groups according to the type of restoration, to differentiate between implants in fixed and removable prostheses. Rates for implants diagnosed with peri-implantitis were calculated for the whole study population as well as for implants in the fixed and removable prostheses, using the case definition for peri-implantitis proposed in the Consensus report of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. Implants with a marginal bone loss of ≥ 3 mm compared to baseline in combination with bleeding or suppuration on probing as well as probing depths of ≥ 6 mm were classified as peri-implantitis cases [13].
Radiographic analysis
For the radiographic assessment, we compared the patient’s latest radiographs to their baseline data. Unfortunately, due to the long observation period, some archived patient health records were incomplete. As it was not possible to recollect all accurate baseline radiographs, we decided to include radiographs, panoramic radiographs, and standardized intra-oral radiographs taken up to 18 months after implant insertion as baseline. For the current analysis, radiographs collected within the last year of the follow-up examination were accepted. If there were signs of inflammation or peri-implantitis, radiographs were also obtained during the follow-up examination. Linear measurements were performed by two independent examiners with correction of the radiograph magnification using an implant of known length as the measuring gauge. The reference points were defined as shown in Fig. 3. Estimations for mean marginal bone (MBL) loss comparing bone levels at baseline and follow-up were performed mesially and distally as well as for each implant individually, same as with PPD.
Statistical analysis
Descriptive statistics of both study groups were obtained by analyzing the frequency distributions of patient and implant characteristics. Possible implant site-dependent differences in marginal bone loss were analyzed using the Mann–Whitney U-test. Inter-rater reliability was assessed using the intraclass correlation coefficient. Analysis of possible patient risk factors with regard to the presence of peri-implant disease was performed using the Chi-squared test. Differences in clinical and radiographic findings between implants in fixed and removable prostheses were analyzed using the t-test and Mann–Whitney U test, whereas possible correlations between radiographic and clinical parameters were identified using the Spearman-Rho test. Values of all parameters were checked on a standard distribution using the Shapiro–Wilk test. Statistical analysis was performed using SPSS (Statistical Package Social Sciences, version 25, SPSS Incorporated, Chicago, IL, USA). In all tests, a significance level of 0.05 was chosen.
Results
Study data
The contact group with 39 patients and 78 implants consisted of 28 female and 11 male subjects with an average age of 74.7 ± 8.5 years. In total, six patients were diagnosed with diabetes, eight with osteoporosis, and 15 with periodontitis in the past, while 10 patients described themselves as smokers. Of the 78 implants, 56 were placed in the mandible. Most patients received implant treatment with 12 and 22 patients receiving one or two implants, respectively. In five cases, three or more implants were inserted.
In the examination group, a total of 15 patients with 32 implants attended follow-up. The study population consisted of 10 female and five male patients with an average age of 75.3 ± 1.5 years. Of the 32 included implants, 27 were placed in the mandible and five were inserted in the maxilla. Eight patients received implant treatment with two implants, while four patients received treatment with one or three implants.
Implant survival rates
After a mean follow-up time of 24 ± 10 years a total of 16 implants in 7 patients were lost. The implant survival rate amounts to 79.5% in contact group (Fig. 4).
In the examination group, no implant was lost after an observation period of 29 ± 3 years.
Clinical examination
The overall average PPD was 2.4 ± 1.5 mm. Mean values for BOP and Plaque Index were 0.9 ± 1.1 and 1.0 ± 1.2, respectively. The frequency distribution of the severity levels of these parameters is shown in Fig. 5. A total of 3 implants were diagnosed with peri-implantitis leading to a peri-implantitis rate of 9.4%, which corresponds to an overall success rate of 90.6%.
Frequency distribution on severity level of implant characteristics grouped into four circle diagrams for each parameter: Plaque Index (PI); Bleeding on Probing (BOP); Pocket Probing Depth (PPD); and Marginal Bone Loss (MBL) after a mean observation time of 29 years in CEG (32 implants). Diagrams for PI, PPD and MBL show the highest measured value for each implant
Marginal bone levels
Seven out of the 15 baseline radiographs were taken immediately after implant placement or within one week after insertion. For the current radiographic analysis, in one case, we had to resort to a radiograph not taken at follow-up. The mean loss of marginal bone was 2.5 ± 1.5 mm at the mesial implant site and 2.5 ± 2.1 mm at the distal implant site corresponding to a global average marginal bone loss of 2.5 ± 1.8 mm (Table 2). There was no significant difference between marginal bone loss at the mesial and distal implant sites (P = 0.6). Importantly, the inter-rater variations were not significant for linear bone-level measurements (P = 0.9). The inter-rater class coefficient was 1.0, indicating very good inter-rater conformity [14, 15]. The frequency distribution of the severity of marginal bone-level changes is shown in Fig. 5.
Correlation analysis
The statistical analysis identified significant positive correlations between “MBL” and “PPD” (P = 0.032) as well as between both just mentioned parameters and “BOP “ (P = 0.006 and P < 0.001, respectively) indicating that more pronounced marginal bone loss is associated with higher pocket probing depths and more bleeding on probing. A significant but weak linear correlation was identified between “MBL” and “observation time” (P = 0.017). According to the Shapiro–Wilk test, all values of the evaluated parameters showed a nonparametric distribution apart from “observation time”, as the significance levels for this parameter did not differ between the nonparametric Spearman-Rho and the parametric test according to Pearson. Table 3 shows the correlation coefficients according to Spearman-Rho.
Risk factors
In the CEG, two patients had been diagnosed with diabetes, five with osteoporosis, and seven with periodontitis. Four patients had a smoking habit, of which three also had periodontitis (Table 4). The proportions of smokers and diabetics in the CEG and CG were nearly identical, while the percentages of patients with osteoporosis and diabetes (33–21% and 47–38%, respectively) were notably higher. At the implant level, only one implant in each group of smokers, patients with diabetes and patients with periodontitis was associated with peri-implantitis, while patients with osteoporosis did not exhibit any compromised implant. No significant correlation between the described risk factors and the presence of peri-implant disease was identified in the Chi-squared test.
Fixed vs. removable prostheses
Out of the 32 implants, 14 implants in seven patients were treated with fixed dental prostheses (FDPs), while 18 implants in eight subjects were treated with removable dental prostheses (RPDs). Differences in clinical and radiographic findings between implants in the FDPs and RDPs groups were found for MBL with the t-test and Mann–Whitney U test (P = 0.02 and P = 0.01, respectively). While the mean marginal bone-level change for implants in the FDPs group was 1.7 ± 1.3 mm, MBL for implants in the RDPs group amounted to 3.2 ± 2.0 mm. Further comparisons of the clinical parameters showed no significant differences in PPD and BOP between the two groups (Fig. 6). Despite being statistically significant, differences in the PI and width of the attached mucosa could not be compared properly because of major differences in the variance of the parameter values. Regarding peri-implantitis, one implant in the FDPs group and two implants in RDPs group were compromised. The analysis with the Chi-square test showed no significant correlation (P = 0.702).
Discussion
Of the 94 preselected and possible participants in this study, 30.9% passed away, and 27.6% were unavailable, leading to a positive response rate of 41.5% (CG). A further 25.5% of these patients had to be excluded for the various reasons listed in Table 5, ultimately leaving 16% of the patients from our original cohort who were examined after a mean observation time of 28.3 years. Comparable long-term studies with observation periods of up to 25 years showed dropout rates ranging from 31.6–71.7%, which is significantly lower than the 84% dropout rate in our study [16,17,18,19,20,21,22,23,24,25,26]. Variations in observation periods may be a decisive factor for this discrepancy, as our study had a longer mean observation time. Thus, on average, patients in our study cohort were older, leading to a higher number of deaths (Table 5). Only one previous study by Bakker et al. (2019) included a cohort whose average age (85.5 + years) significantly surpassed the mean age found in our study, as patients younger than 60 years at baseline were excluded [17]. Consequently, the proportion of patient deaths (62.3%) in this cohort was the highest, leading to a dropout rate of 71.7%. The relatively small number of “unavailable” patients compared to our study might be explained by its prospective study design, since those patient cohorts have been meticulously followed up several times over the course of the last 20 years [17]. Generally, dropout rates are very high, with most studies observing at best, about 30%, and more often about 60% after 20 years, regardless of the study design. Importantly, cutting out such a large proportion of potential information limits the validity of the collected data.
Owing to steadily evolving implant technology, the lack of sufficient long-term data is an issue, especially for outdated implant systems, as the benefit of data on those systems is arguable. Furthermore, the presented studies indicate that the feasibility of long-term follow-up studies spanning 20 years or longer is complicated due to high patient dropout rates [16,17,18, 20, 22, 24, 26].
The present study showed a relatively high survival rate of 79.5% after a mean observation time of 28 years. However, it falls short of the survival rates of follow-up studies with comparable observation periods, ranging from a survival rate between 87.8. and 100% [16,17,18, 20,21,22,23,24,25,26]. Interestingly, studies exclusively examining Branemark implants have reported the highest survival rates, regardless of the study design. On the other hand, Frisch et al. (2020) observed excellent survival rates in a cohort of patients with various implant types, who were part of a permanent supportive implant therapy program [22]. Nevertheless, due to the heterogeneity of study designs and the generally high dropout rates described in all studies to date, the results should be interpreted with caution.
Regarding the radiographic analysis, we found a mean marginal bone loss of 2.5 mm after an average observation time of 28.3 years. While slightly higher, our results are comparable to those of previous studies [16, 17, 20, 22,23,24,25,26] reporting mean marginal bone loss in the range of 0.02–2.5 mm analyzing predominantly Branemark implants (Table 6). Regarding clinical outcomes, we recorded an average probing pocket depth of 2.4 mm. In relation to the mean pocket probing depths ranging from 2.5 to 4.0 mm in comparable studies (Table 6), our results stand out in a positive way. Owing to the variability of PPD which depends on the width of the peri-implant mucosa, information on the progression or stagnation of PPD is essential for peri-implant diagnostics. In addition, our favorable findings can be explained by the reduced accessibility of the peri-implant pocket due to the geometry of the implant’s suprastructure [27], as in our study the implant suprastructures were not removed for clinical evaluation.
Comparing the MBL of the IMZ implants among the FDPs and RDPs groups, we found significantly less bone-level changes in the FDPs group (1.7 mm and 3.2 mm, respectively). To date, no studies have analyzed bone-level changes in IMZ implants in fixed dental prostheses. Regarding the MBL of IMZ implants in removable prostheses, we observed significantly higher bone loss than the 1.4 mm described by Meijer et al. (2009) after 10 years. Therefore, owing to the vast differences in observation times, comparisons must be performed with caution. Notably, based on differences observed in MBL between the FDPs and RDPs groups, Berglundh et al. (2002) concluded, that the percentage of implants showing MBL of at least 2.5 mm is notably higher (4.76%) in overdentures than in FDPs or single-implant restorations (1.01% and 1.28%, respectively) [28]. These results confirm our findings. The increased bone loss might be explained by the unfavorable bending forces that are applied to the implants due to the free-ending saddles typically used in RDPs [29].
Of the 32 implants included in our study, 3 (9.4%) were diagnosed as peri-implantitis, which is a slightly higher prevalence rate than that reported in comparable studies ranging from 2.4–7% [16, 22, 24]. However, the value is in accordance with the 10% proportion of peri-implant diseased implants reported in the review by Mombelli et al. (2012) after an observation time of 5–10 years [30]. As pointed out in the review by Mombelli et al. (2012), a wide range of different disease-defining criteria were used in the selected studies, so the comparability of peri-implantitis rates is generally difficult. For example, according to Astrand et al. (2008), a crater or beaker-like type of bone loss is required to diagnose peri-implantitis [16], while Jokstad et al. (2017) defined diseased implants as unsuccessful implants according to the criteria of Buser et al. (1990) [24, 31].
Due to these different definitions, the 2017 Consensus Conference established a uniform standard. Consequently, the new definition for peri-implantitis was used in the current study. As one of the latest long-term follow-ups on implant therapy Frisch et al. (2020) also followed this new standard allowing a more concise comparison of the presented per-implantitis rates [22]. Frisch et al. (2020) observed a prevalence of peri-implantitis of 7% in a cohort of patients participating in a strict supportive implant therapy program. In contrast, a peri-implantitis incidence rate of 40% was observed among patients that were not part of a supportive structured implant therapy program but instead kept control examination appointments on their own initiative. In contrast to these data, the results of our study seem very favorable, even if on our patient cohort a strict supportive implant therapy program was not performed. Further, because of the absence of previous examinations in contrast to Frisch et al. (2020) we had to rely on the thresholds proposed in the Consensus report [13] limiting the comparability between the presented peri-implantitis rates. Due to the geometry of the implant’s suprastructure, the access to the peri-implant pocket was reduced possibly leading to a more positive outcome, as suprastructures were not removed in our study [27]. Nevertheless, a recent systematic review also observed significant differences in the prevalence of peri-implantitis between patients who participated regularly in a prophylaxis program (9.0%) and those without regular preventive maintenance care (18.8%). These findings confirm a tendency towards an increased risk for developing peri-implantitis in patients with a lack of prophylaxis on a medium level of evidence [32]. Although several studies have found a strong tendency to favor peri-implantitis in smokers, patients with periodontitis and patients with diabetes [30, 32], our study failed to show a significant connection between these risk factors and the development of peri-implantitis. As we predominantly relied on self-reported medical history, it is most likely that many patients did not know or remember the exact reason for their teeth loss leading to implant therapy. In our study, 46.7% of the patients had previously suffered from periodontitis, although the actual number might be greater, considering that the fifth German oral health study reported that 65% of elderly people suffer from periodontal disease, which is considerably higher than that observed in our study [33]. With regard to osteoporosis as a potential risk factor for peri-implantitis, neither our study nor the systematic review by Dreyer et al. (2018) found any significant associations [32].
Our literature search in MEDLINE did not reveal any meta-analysis nor systematic review on implant survival and marginal bone loss after an observation time of 15 years or longer. This applies not only to IMZ implants but also in general to other implant systems. Latest systematic reviews on this topic present data on implant therapy after 10 years, while studies with longer follow-up periods were occasionally included [34, 35]. In these studies, implant survival ranges from 73.4 to 100% with a cumulative mean value of 94.6% [35].
According to the aims of the presented study, we compiled publications analyzing patient drop out, implant survival and peri-implant conditions with long-term data after more than 15 years (Tables 5, 6). We included all studies with a prospective as well as retrospective design. Publications not providing a distinct description of patient drop out were excluded. The selected studies partially providing detailed investigation on long-term implant therapy suggest that a systematic review and meta-analysis on this topic in a dedicated publication is meaningful.
The major limiting factor of our study was the small number of patients, who attended the follow-up appointment. Of the 94 patients with 199 implants, 15 patients with 32 implants agreed to undergo clinical and radiographic examinations. This was equivalent to a dropout rate of 84%. Since most of the dropped-out patients were deceased or unavailable, and the patient’s status was considered independent of the condition of the implants, we assume that our contact group is representative of the original patient pool. However, it is arguable whether patients with CEG were generally healthier and therefore more compliant than patients who were not available for a follow-up appointment because of senility or death. Additionally, as the clinical and radiographical data of lost implants could not be considered, our results are probably based on a positive selection of largely successful implants. Despite these assumptions, the influence of a largely reduced study population accompanied by a corresponding loss of information is unclear and could equally lead to false-positive or false-negative outcomes, which is why the results of our study should be interpreted with caution. This applies especially to the results from the radiographic analysis. Although differences in the reported bone loss across all the studies mentioned are minimal, strict comparisons are difficult, and exact conclusions cannot be drawn. As seen in our study, the number of patients examined at follow-up after 10–20 years was comparably small. Hence, individual findings and statistical outliers could drastically affect the results, leading to greater variability in the reported outcomes.
In addition, one major problem in analyzing the radiographs was the rather difficult identification of the reference points of the implant according to our definition. Since it was not possible to remove the implant suprastructures for examination, the radiographic reference points were often overlaid by the intramobile connector (IMC). In addition, radiographic superimposition and motion blur led to varying image quality and in some cases, the position of the radiographic reference point had to be gauged. The bone-level measurements were performed by two individual examiners with the help of optical magnification, thus any possible deviations between the estimated and actual reference points should be minor and clinically irrelevant.
Due to the retrospective nature of this study, combined with missing or incomplete patient files, no statements on changes in clinical parameters could be made, as no baseline data were reported. In addition, we often had to rely on self-reported medical history, limiting the validity of the presented analysis of risk factors, as the senescence of the patients has to be considered. The lack of memory and understanding for their anamnesis could explain the relatively small number of patients with a history of periodontitis found in our study.
Conclusions
Conducting long-term follow-up studies with a retrospective design after a mean observation time of nearly 30 years with acceptable response rates was not feasible. Therefore, owing to the high dropout rate of 84%, the results cannot be generalized and should be interpreted with caution. The limited data we could gather presented an overall implant survival rate of 79.5%, while the surviving implants showed a peri-implantitis rate of 9.4%, exhibiting a mean marginal bone loss of 2.5 mm. Due to the retrospective study design and the high dropout rate, additional risk factors could not be considered in a conclusive analysis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IMZ:
-
Intramobile cylinder
- IME:
-
Intramobile element
- IMC:
-
Intramobile connector
- CG:
-
Contact group
- CEG:
-
Clinical evaluation group
- PPD:
-
Pocket probing depth
- BOP:
-
Bleeding on probing
- PI:
-
Plaque Index
- MBL:
-
Marginal bone loss
- FDP:
-
Fixed dental protheses
- RDP:
-
Removable dental protheses
References
Branemark PI, Adell R, Breine U, Hansson BO, Lindstrom J, Ohlsson A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969;3(2):81–100.
Kirsch A, Ackermann KL. The IMZ osteointegrated implant system. Dent Clin N Am. 1989;33(4):733–91.
Fugazzotto PA, Gulbransen HJ, Wheeler SL, Lindsay JA. The use of IMZ osseointegrated implants in partially and completely edentulous patients: success and failure rates of 2,023 implant cylinders up to 60+ months in function. Int J Oral Maxillofac Implants. 1993;8(6):617–21.
Babbush CA, Shimura M. Five-year statistical and clinical observations with the IMZ two-stage osteointegrated implant system. Int J Oral Maxillofac Implants. 1993;8(3):245–53.
Haas R, Mensdorff-Pouilly N, Mailath G, Watzek G. Survival of 1,920 IMZ implants followed for up to 100 months. Int J Oral Maxillofac Implants. 1996;11(5):581–8.
Meijer HJ, Raghoebar GM, Batenburg RH, Vissink A. Mandibular overdentures supported by two Branemark, IMZ or ITI implants: a ten-year prospective randomized study. J Clin Periodontol. 2009;36(9):799–806.
Spiekermann H, Jansen VK, Richter EJ. A 10-year follow-up study of IMZ and TPS implants in the edentulous mandible using bar-retained overdentures. Int J Oral Maxillofac Implants. 1995;10(2):231–43.
Meijer HJ, Raghoebar GM, Van’t Hof MA. Comparison of implant-retained mandibular overdentures and conventional complete dentures: a 10-year prospective study of clinical aspects and patient satisfaction. Int J Oral Maxillofac Implants. 2003;18(6):879–85.
Willer J, Noack N, Hoffmann J. Survival rate of IMZ implants: a prospective 10-year analysis. J Oral Maxillofac Surg. 2003;61(6):691–5.
Noack N, Willer J, Hoffmann J. Long-term results after placement of dental implants: longitudinal study of 1,964 implants over 16 years. Int J Oral Maxillofac Implants. 1999;14(5):748–55.
Visser A, Stellingsma C, Raghoebar GM, Meijer HJ, Vissink A. A 15-year comparative prospective study of surgical and prosthetic care and aftercare of overdenture treatment in the atrophied mandible: augmentation versus nonaugmentation. Clin Implant Dent Relat Res. 2016;18(6):1218–26.
Mombelli A, van Oosten MA, Schurch E Jr, Land NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987;2(4):145–51.
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, et al. Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the classification of periodontal and peri-implant diseases and conditions. J Clin Periodontol. 2018;45(Suppl 20):S286–91.
Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–90.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–63.
Astrand P, Ahlqvist J, Gunne J, Nilson H. Implant treatment of patients with edentulous jaws: a 20-year follow-up. Clin Implant Dent Relat Res. 2008;10(4):207–17.
Bakker MH, Vissink A, Meijer HJA, Raghoebar GM, Visser A. Mandibular implant-supported overdentures in (frail) elderly: a prospective study with 20-year follow-up. Clin Implant Dent Relat Res. 2019;21(4):586–92.
Chappuis V, Buser R, Brägger U, Bornstein MM, Salvi GE, Buser D. Long-term outcomes of dental implants with a titanium plasma-sprayed surface: a 20-year prospective case series study in partially edentulous patients. Clin Implant Dent Relat Res. 2013;15(6):780–90.
Deporter D, Pharoah M, Yeh S, Todescan R, Atenafu EG. Performance of titanium alloy sintered porous-surfaced (SPS) implants supporting mandibular overdentures during a 20-year prospective study. Clin Oral Implant Res. 2014;25(2):e189–95.
Dierens M, Vandeweghe S, Kisch J, Nilner K, De Bruyn H. Long-term follow-up of turned single implants placed in periodontally healthy patients after 16–22 years: radiographic and peri-implant outcome. Clin Oral Implant Res. 2012;23(2):197–204.
Donati M, Ekestubbe A, Lindhe J, Wennström JL. Marginal bone loss at implants with different surface characteristics—a 20-year follow-up of a randomized controlled clinical trial. Clin Oral Implant Res. 2018;29(5):480–7.
Frisch E, Wild V, Ratka-Krüger P, Vach K, Sennhenn-Kirchner S. Long-term results of implants and implant-supported prostheses under systematic supportive implant therapy: a retrospective 25-year study. Clin Implant Dent Relat Res. 2020;22(6):689–96.
Jacobs R, Pittayapat P, van Steenberghe D, De Mars G, Gijbels F, Van Der Donck A, et al. A split-mouth comparative study up to 16 years of two screw-shaped titanium implant systems. J Clin Periodontol. 2010;37(12):1119–27.
Jokstad A, Gussgard AM, Fava J, Lin M, Shokati B, Somogyi-Ganss E, et al. Benchmarking outcomes in implant prosthodontics: partial fixed dental prostheses and crowns supported by implants with a turned surface over 10 to 28 years at the University of Toronto. Int J Oral Maxillofac Implants. 2017;32(4):880–92.
Jung RE, Brügger LV, Bienz SP, Hüsler J, Hämmerle CHF, Zitzmann NU. Clinical and radiographical performance of implants placed with simultaneous guided bone regeneration using resorbable and nonresorbable membranes after 22–24 years, a prospective, controlled clinical trial. Clin Oral Implant Res. 2021;32(12):1455–65.
Lekholm U, Grondahl K, Jemt T. Outcome of oral implant treatment in partially edentulous jaws followed 20 years in clinical function. Clin Implant Dent Relat Res. 2006;8(4):178–86.
Serino G, Turri A, Lang NP. Probing at implants with peri-implantitis and its relation to clinical peri-implant bone loss. Clin Oral Implant Res. 2013;24(1):91–5.
Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29(Suppl 3):197–212; discussion 32-3.
Rammelsberg P, Lorenzo-Bermejo J, Kappel S. Effect of prosthetic restoration on implant survival and success. Clin Oral Implant Res. 2017;28(10):1296–302.
Mombelli A, Muller N, Cionca N. The epidemiology of peri-implantitis. Clin Oral Implant Res. 2012;23(Suppl 6):67–76.
Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants. 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990;1(1):33–40.
Dreyer H, Grischke J, Tiede C, Eberhard J, Schweitzer A, Toikkanen SE, et al. Epidemiology and risk factors of peri-implantitis: a systematic review. J Periodontal Res. 2018;53(5):657–81.
Rainer Jordan WMA. Fünfte Deutsche Mundgesundheitsstudie (DMS V). (IDZ) IDDZ, editor: Deutscher Zahnärzte Verlag DÄV; 2016.
Hjalmarsson L, Gheisarifar M, Jemt T. A systematic review of survival of single implants as presented in longitudinal studies with a follow-up of at least 10 years. Eur J Oral Implantol. 2016;9(Suppl 1):S155–62.
Moraschini V, Poubel LA, Ferreira VF, Barboza ES. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015;44(3):377–88.
Acknowledgements
We thank Martin Lemos, head of the audiovisual media department of the RWTH Aachen University for the assistance in the creation of the illustrations.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
CM collected and analyzed the data as well as led the writing; SW supervised the writing and contributed with ideas; WM edited the manuscript and contributed with ideas; AR conceived the study design, supervised data collection, and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants provided informed consent prior to their inclusion in the study according to the 1964 Declaration of Helsinki. The study protocol was approved by the local ethics committee (EK 133/17).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mautsch, C., Wolfart, S., Mautsch, W. et al. Long-term outcome of the IMZ implant system: a retrospective clinical study with a follow-up between 23 and 34 years. Int J Implant Dent 8, 54 (2022). https://doi.org/10.1186/s40729-022-00452-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40729-022-00452-0