Abstract
Background
The present study was based on the null hypothesis that there is no difference in clinicoradiographic parameters and whole salivary alpha amylase (AA) and mucin-4 levels before and after non-surgical mechanical debridement (NSMD) of patients with peri-implant mucositis (PM). The aim was to assess whole salivary AA and mucin-4 levels before and after treatment of PM.
Methods
Patients with PM (Group-1) and individuals without peri-implant diseases (Group-2) were included. Demographic data was collected and peri-implant modified plaque and bleeding indices (mPI and mBI, respectively), probing depth (PD) and crestal bone loss were measured at baseline. Levels of AA and mucin-4 were assessed in unstimulated whole saliva samples. All patients underwent full-mouth non-surgical periodontal therapy (NSPT) and NSMD; and clinical parameters and salivary biomarkers were re-assessed after 3 months. Level of significance was set at P < 0.01.
Results
Twenty-six and 32 individuals were included in groups 1 and 2, respectively. None of the participants had periodontitis. At baseline clinical periodontal parameters (PI [P < 0.001], GI [P < 0.001], clinical AL [P < 0.001] and PD [P < 0.001]) were significantly high in Group-1 than Group-2. At 3-month follow-up, there was a statistically significant reduction in clinical periodontal and peri-implant parameters (PI [P < 0.01], GI [P < 0.01], and PD [P < 0.01]) in Group-1 compared with their baseline values. At baseline, salivary AA levels were significantly high in Group-1 than Group-2 (P < 0.01). At 3-month follow-up, there was no significant difference in whole salivary AA levels among patients in groups 1 and 2.
Conclusions
The AA and mucin-4 levels are potential biomarkers for evaluation of peri-implant diseases including PM. Mechanical instrumentation continues to be the most predictable treatment option for the management of peri-implant diseases.
Similar content being viewed by others
Introduction
Oral rehabilitation with dental implants is a modern alternate to traditional fixed and removable dental prostheses, such as bridges and dentures. Despite the fact that dental implants can osseointegrate and demonstrate success and survival rates of up to 100% [1, 2]; peri-implant diseases are a complication that cannot be overlooked. Peri-implant diseases initially manifest as peri-implant mucositis (PM) during which, gingival tissues appear red and puffy and demonstrate increased bleeding on gently probing (with or without suppuration) and probing depth (PD) [3, 4]. If PM is left undiagnosed and untreated for prolonged durations, the inflammatory process worsens and results in peri-implant crestal bone loss (CBL) or peri-implantitis [3, 4]. This may result in loosening of implant and even implant failure. The pathophysiology of peri-implant diseases is complex and driven by a cascade of events including immunoinflammatory and microbiological imbalances and genetic heterogeneity [5,6,7,8,9].
Studies [10, 11] have shown that patients with existing or with a history of periodontitis are more susceptible to peri-implant diseases compared with individuals with a healthy periodontal status. Unstimulated whole saliva (UWS) is a biologic oral fluid that expresses raised levels of destructive inflammatory cytokines among patients with periodontal and peri-implant diseases [12,13,14,15,16]. Alpha-amylase (AA) protein represents the autonomic nervous system and contributes towards maintenance of mucosal immunity by inhibiting bacterial colonization, reproduction and adhesion [17, 18]. Under oral inflammatory conditions, the production of AA is increased in an attempt to counteract the inflammatory insult [19]. It has been reported that a direct correlation exists between salivary AA activity and severity of periodontitis [20]. Similarly, mucins (primary organic constituent of mucus) envelop all mucosal surfaces of the body are glycoproteins that also contribute in innate immunity by facilitating bacterial clearance from the oral cavity [21]. In addition, mucins hydrate oral tissues thereby protecting oral hard and soft tissues from exogenous insults [22]. Furthermore, it has also been proposed such mucins act as receptors initiating intracellular signaling transduction pathways [23]. With reference to oral inflammatory conditions, Lundmark et al. [21] reported that mucin-4 is expressed in lower concentrations in UWS of saliva of patients with periodontitis compared with individuals with a healthy periodontal status. To date, there is one study [24] in indexed literature that has assessed salivary AA levels in relation to clinical implantology and associated research. However, this study [24] assessed salivary AA levels in relation to implant surgical interventions and not with reference to pathophysiology and/or severity of peri-implant diseases. It is worth mentioning that there are no clinical studies that have compared whole salivary mucin levels among patients with and without peri-implant diseases.
Non-surgical mechanical debridement (NSMD) is the gold standard for the management of PM and peri-implantitis [25, 26]. It is known that NSMD helps reduce the severity of clinical peri-implant inflammatory parameters (modified plaque index [mPI], modified bleeding index [mBI] and PD) in patients with peri-implant diseases [26, 27]. From a periodontal standpoint, non-surgical periodontal therapy has been reported to reduce salivary levels of destructive inflammatory cytokines, such as intrleukin-1beta (β) and matrix metalloproteinase (MMP)-8 [13]. Nevertheless, there are no studies in indexed literature that have compared whole salivary AA and mucin levels before and after NSMD in patients with PM. The aim was to assess whole salivary AA) and mucin-4 levels before and after NSMD of patients with PM. The present study was based on the null hypothesis that there is no difference in clinicoradiographic parameters and whole salivary AA and mucin levels before and after NSMD of patients with PM.
Materials and methods
Ethical standards
The present study was carried out in accordance with the Declaration of Helsinki as revised in 2013 guidelines involving human subjects. Volunteers were asked to sign a consent form. Withdraw did not bear any penalization or/and consequences. Ethical approval was obtained from ethics research committee of the Sharavathi Dental College and Hospital, Shivamogga, Karnataka, India (19/2022/CR). All individuals were also given verbal and written information about brushing and flossing techniques.
Location and duration of study
The patients were recruited from the outpatient department at the College of Dentistry, Sharavathi Dental College and Hospital, Shivamogga, Karnataka 577204, India. The study was performed between August 2021 and March 2022. The co-author from this institution performed the clinicoradiographic investigations and laboratory-based investigations were done by a trained and calibrated technician.
Inclusion and exclusion criteria
Patients having undergone dental implant therapy were included. Peri-implant mucositis was clinically defined as presence of peri-implant signs of soft-tissue swelling, redness and bleeding within 30 s of gently probing, and no additional CBL following initial healing [28]. Clinical definition of peri-implantitis was based on the following characteristics: (a) peri-implant signs of soft-tissue inflammation, (b) radiographic evidence of CBL after initial healing, and (c) increasing PD as compared to PD values recorded after prosthetic loading (PL) [28]. Peri-implant health was defined on the following features: absence of peri-implant clinical signs of soft-tissue inflammation, and absence of further CBL following PL [28]. In the present study, patients with a healthy periodontal and peri-implant status served as controls. Individuals habitually using combustible and non-combustible tobacco-products, habitual alcohol users, patients with existing or with a history of periodontitis and patients with self-reported systemic diseases such as prediabetes, diabetes mellitus (DM), cardiovascular diseases (CVD), obesity and oral and/or systemic cancer were excluded. Patients that had used antibiotics, bisphosphonates, probiotics, steroids and non-steroidal analgesics within the past 90 days were also excluded. Mandibular third molars, supernumerary teeth and broken-down teeth with embedded root remnants were not evaluated.
Questionnaire
A questionnaire was used to gather information pertaining to patients’ age and gender, routine domestic oral hygiene maintenance (DOHM) protocols (brushing and interproximal flossing) and most recent visit to oral healthcare providers.
Evaluation of patients’ dental records
Patients’ dental records were evaluated to gather the following information: number of implants per patient, implant dimensions (diameter and length), implant surface characteristics, implant loading protocol (delayed, immediate or early), implant abutment connection, implant jaw location, depth of placement (bone-level or submerged), duration in years for which, implants were in function and mode of prosthesis retention (cement and/or screw retention).
Periodontal and peri-implant clinical and radiographic parameters
Full-mouth plaque index (PI) [29], gingival index (GI) [30], PD [31] and clinical attachment loss (AL) [32] were assessed around all teeth. Peri-implant mPI [33], mBI [33] and PD [34] were also measured. Clinical AL and PD were measured to the nearest millimeter (mm) with a plastic graded probe (Hu-Friedy InC, Chicago, IL, USA). Full-mouth digital intra-oral radiographs (Planmeca Romexis Intra oral X-Ray, Planmeca OY, Helsinki, Finland) were taken [35]; and standardization of all X-rays was done as described elsewhere [36, 37]. Marginal bone loss (MBL) and CBL around teeth and implants, respectively, were measured at baseline; and defined as linear distances from 2 mm below the cemento-enamel junction and implant abutment interface, respectively, to the alveolar crest [38, 39]. Clinical peri-implant and periodontal parameters were assessed at baseline and after 3 months of therapy.
Non-surgical periodontal and peri-implant therapy
All patients underwent full-mouth non-surgical periodontal therapy (NSPT) and NSMD around teeth and implants, respectively. Sterile curettes (Gracey Curets, Hu-Friedy, Chicago, IL, USA) and an ultrasonic scaler (PIEZO-soft ultrasonic scaler; equipped with PIEZO Scaler tip 201, KaVo Dental, Germany) were used to perform NSPT. Peri-implant NSMD was done using sterile plastic curettes. Post-operatively, oral hygiene instructions were reinforced; and all patients were instructed to rinse every 12 h with 15 ml of 0.12% chlorhexidine gluconate for the next 14 days.
Collection of whole saliva and assessment of alpha amylase and mucin levels
Collection of whole saliva samples was performed 24 h after clinical and radiographic evaluations. The protocol described by Ali et al. [35] was used to collect UWS samples. The whole salivary flow rate was determined. The UWS samples were collected during early morning hours (between 7 and 8am) with participants being in a fasting state. All saliva samples were immediately centrifuged at 1500×g for 15 min in a cold room; and the supernatants were stored at – 70 °C. All samples were assessed with 24 h of collection. The AA levels were as described by Haririan et al. [20]. In summary, whole salivary AA levels were determined using commercially available kits (Olympus-System-Reagents/6182, Olympus AU-640, Olympus Diagnostic Systems, PA, USA). A dilution protocol of 1:50 was used (assay range: 10–4800 U/L; intraassay CV < 1.4%; interassay CV < 3.3%). Whole salivary mucin-4 levels were measured as described by Lundmark et al. [21]. In summary, commercially available assay kits (Kamiya Biomedical Company, Seattle, WA, USA), were used according to the manufacturer’s instructions. The sensitivity for mucin-4 kits was 0.134 ng/ml, respectively. All samples were assessed by a trained and calibrated investigator (Kappa score 0.88).
Sample-size estimation and statistical analyses
Data normality was assessed using the Kolmogorov–Smirnov test. Results of this test showed that all groups had a normality P value > 0.05 indicating normal distribution. Sample size was calculated to provide 95% power to recognize a significant difference of 2 mm among groups with a 95% confidence interval (α = 0.05); and assuming a standard deviation of 1 mm, considering the changes in mean PD. Therefore, at least 23 participants were required per group. Group comparisons were done using the paired t test. For multiple comparisons Bonferroni post-hoc adjustment test was performed. Correlation between demographic and clinicoradiographic parameters and whole salivary AA and mucin-4 levels were assessed using logistic regression models. When P values were less than 0.01, they are considered “statistically significant”.
Results
Participant screening
Initially, 96 patients with dental implants in function were invited to participate in the present study. Nineteen patients refused to sign the written informed consent form. On the remaining (n = 77), 14 patients were tobacco-smokers and five individuals had systemic diseases (three and two patients with DM and CVD, respectively). In total, 58 individuals (34 males and 24 females) signed the written informed consent form and were included in the present investigation.
Demographics
Of the 58 individuals, 26 individuals (14 males and 12 females) had PM (Group-1) and the remaining (n = 32) had healthy peri-implant tissues (Group-2/controls). There was no statistically significant difference in the mean age of patients in groups 1 and 2. There was no significant difference in the mean age of males and females among patients with PM and controls. Tooth brushing twice daily was reported by 42.3% and 87.5% individuals with PM and controls, respectively. None of the patients with PM reported to have ever used a dental floss (Table 1).
Implants
A total of 58 implants were assessed. All implants were placed in the regions of missing premolars or molars. In groups 1 (n = 26) and 2 (n = 32), 19 and 21 implants, respectively, were located in the posterior maxilla (Table 1). All implants were placed at bone level, delayed-loaded and platform switched with moderately rough surfaces and had diameters and lengths ranging between 4 and 4.1 mm and 11 and 13 mm, respectively. Each implant was restored with a single ceramic crown using cement-retained restorations. In groups 1 and 2, implants were in function for a mean duration of 3.06 ± 0.2 and 3.4 ± 0.3 years, respectively.
Periodontal and peri-implant clinicoradiographic status
At baseline clinical periodontal parameters (PI [P < 0.001], GI [P < 0.001], clinical AL [P < 0.001] and PD [P < 0.001]) were significantly high in Group-1 compared with Group-2. At 3-month, follow-up, there was a statistically significant reduction in clinical periodontal and peri-implant parameters (PI [P < 0.01], GI [P < 0.01], and PD [P < 0.01]) in Group-1 compared with their respective baseline values. None of the patients had active periodontal diseases, such as periodontitis. Clinical attachment levels, MBL and CBL did not demonstrate any significant difference when baseline values were compared with those measured at 3-month follow-up in both groups. In Group-2, there was no significant difference in periodontal and peri-implant clinicoradiographic status at both time intervals (Table 2).
Salivary flow rate and whole salivary alpha amylase and mucin-4 levels
There was no significant difference in SFR among patients in groups 1 and 2 throughout the study period. At baseline, salivary AA levels were significantly high in Group-1 compared with Group-2 (P < 0.01). At 3-month follow-up, there was no significant difference in whole salivary AA levels among patients in groups 1 and 2. Salivary mucin-4 levels were significantly high in Group-2 compared with Group-1 at baseline (P < 0.01). There was no significant difference in whole salivary mucin-4 levels among patients in groups 1 and 2 at 3-month follow-up (Table 3).
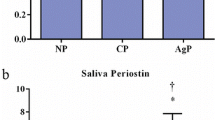
Correlation between whole salivary alpha amylase and mucin-4 levels and demographic and clinicoradiographic parameters
In Group-1, there was a statistically significant correlation between peri-implant PD and whole salivary AA and mucin-4 levels at baseline (Fig. 1). There was no statistically significant correlation between peri-implant PD and whole salivary AA and mucin-4 levels at baseline in Group-2 (Fig. 1). At 3-month follow-up, there was no statistically significant correlation between periodontal and peri-implant clinicoradiographic parameters in groups 1 and 2 (data not shown). There was no statistically significant correlation between age, gender, years of implants in function, and whole salivary AA and mucin-4 levels in both groups (data not shown).
Discussion
The present study was based on the null hypothesis that there is no difference in clinicoradiographic parameters and whole salivary AA and mucin levels before and after NSMD of patients with PM. To date, there is one study [24] in indexed literature that has assessed salivary AA levels in relation to dental implants. Similarly, there are no studies that have correlated whole salivary mucin-4 levels with peri-implant diseases. Sabbagh et al. [24] assessed fluctuations in salivary AA levels during surgical placement of dental implants and correlated it with patients’ heart rate. Laboratory-based results of the present investigation correlated whole salivary AA and mucin-4 levels in patients with and without PM. Our results showed that whole salivary mucin-4 and AA levels were significantly lower and higher, respectively, in patients with PM and controls. Lundmark et al. [21] reported significantly lower salivary mucin-4 levels in patients with periodontitis. The authors support the results reported by Lundmark et al. [21] as the current results showed significantly lower mucin-4 levels in Group-1 (patients with PM) than controls (patients without peri-implant diseases). There is a likelihood that salivary AA and mucin-4 levels significantly altered in patients with peri-implantitis than those with PM; however, this evaluation could not be performed in the current investigation. A variety of salivary markers including interleukin-1 beta, tumor necrosis factor-alpha, and soluble urokinase plasminogen activating receptor have been suggested to play a role in the etiopathogenesis and progression of periodontal and peri-implant diseases [16, 35, 40, 41]; however, a consensus on the most reliable and predictable salivary biomarker peri-implant disease activity is yet to be reached. Nevertheless, results based on logistic regression analysis showed a significant correlation between baseline peri-implant PD and salivary AA and mucin-4 levels in patients with PM. Based upon the present results, whole salivary AA and mucin-4 levels can also be considered as potential biomarkers of peri-implant disease activity.
As far as controls (Group-2) are concerned, these individuals had healthy implants (defined according to criteria reported elsewhere [28]); and were visiting the oral healthcare facility for routine dental prophylactic/hygiene maintenance. Studies [42, 43] have shown that patients with a history of periodontitis are at an increased risk of developing peri-implant diseases, such as peri-implantitis compared with individuals with a healthy periodontal health status. Despite the fact that none of the participants included in Group-1 had existing or a history of periodontitis, peri-implant diseases (PM) occurred in these individuals. One reasoning for this is that DOHM protocols appeared compromised in these individuals. As shown in Table 1, approximately 42% individuals in Group-1 reported that they were brushing teeth twice daily compared with individuals with “healthy implants”/controls, where approximately 87% individuals reported that they were brushing twice daily. Moreover, flossing of interproximal spaces was being routinely performed by nearly 10% patients in the control group, whereas none of the individuals in Group-1 reported to have ever used a dental floss. These are potential factors that may have facilitated the accumulation of supra- and subgingival plaque accumulation around periodontal and peri-implant tissues thereby reflecting significantly higher baseline scores of PI, mPI, GI, mGI, and clinical AL among patients in Group-1 compared with Group-2. Interestingly, the mean crestal and MBL was less than 3 mm in both groups at baseline despite routine OHM protocols being compromised among patients in group 1 than Group-2. By no means should these outcomes suggest that toothbrushing once daily and lack of flossing sufficient for routine DOHM. However, there are certain factors that could be used to explain this finding. In the present investigation, all participants were relatively young with a mean age of approximately 40 years (Table 1). It has been reported that periodontitis is more often manifested in older patients (aged at least 60 years and above) compared with individuals that are in their fourth decade of life [38]. This may be a risk-factor of peri-implantitis as well; however, there is no consensus in this regard. In the present study, all implants were in function for a mean duration of approximately 3 years, which is a relatively short duration. Studies [2, 44, 45] have shown that under physiologic conditions dental implants demonstrate minimal CBL up to 7 years of PL. The authors applaud results reported in a non-interventional multicenter study [45] according to which, dental implants placed in individuals (mean age approximately 50 years) demonstrate CBL of 0.52 ± 0.55 mm after 36 months of PL. In the current investigation, the CBL values at 3 years of PL were approximately 0.7 mm and 0.4 mm, respectively, in groups 1 and 2. It is, therefore, speculated that severity of peri-implant diseases is worse and salivary mucin-4 and AA levels are markedly altered in elderly individuals with a duration of implant PL (over 10 years) compared with younger individuals with a shorter duration (≤ 5 years) of implant PL. Further studies are needed to test this hypothesis.
Non-surgical debridement of periodontal and peri-implant surfaces and tissues is classically performed for the management of periodontal and peri-implant diseases [27]. However, the contribution of improvements in oral hygiene maintenance protocols cannot be ignored. There is a possibility that the participants, especially those in Group-1 improved their DOHM protocols after therapeutic interventions. However, an oral health questionnaire was not administered to all participants at the follow-up visit.
Although stringent eligibility criteria were imposed for patient inclusion to minimize the risk of bias and standardize the study groups; this may be considered as a potential limitation of the present study. Studies [46, 47] have reported that habitual use of nicotinic products (such as cigarettes, waterpipe and electronic nicotine delivery systems) and a compromised medical health status (such as poor glycemic control) are risk factors of periodontal and peri-implant diseases (PM and peri-implantitis). It is tempting to speculate that salivary AA and mucin-4 levels are significantly altered in diabetic smokers compared with systemically healthy smokers and never-smokers. However, despite the fact that CBL is higher in smokers than never-smokers, there is insufficient evidence in indexed literature to nominate smoking as a risk-factor of peri-implantitis [48]. Likewise, results from a narrative review [48] reported that patients with DM diagnosed with peri-implant mucositis are not at a higher risk to develop peri-implantitis when compared to systemically healthy controls. Therefore, it is challenging to declare that smoking and DM are “risk-factors” of peri-implant diseases. It is also noteworthy that there were a limited number of implants assessed in the present study and that all patients had a healthy periodontal status. It is, therefore, speculated that the AA and mucin-4 levels reported in the present study could be indicative of a healthy periodontal status. Furthermore, due to the ethically approved study design and limitations in funding resources, other laboratory-based investigations such as assessment of whole salivary total protein concentrations and assessment of microbes in the subgingival oral biofilm before and after NSPT and NSMD were not done. This warrants further studies with specific objectives.
Conclusions
The AA and mucin-4 levels are potential biomarkers for evaluation of peri-implant diseases including PM. Mechanical instrumentation continues to be the most predictable treatment option for the management of peri-implant diseases.
Availability of data and materials
The data are available from the corresponding author on reasonable request.
Abbreviations
- AA:
-
Alpha amylase
- CBL:
-
Crestal bone loss
- DOHM:
-
Domestic oral hygiene maintenance
- GI:
-
Gingival index
- mPI:
-
Modified plaque index
- mBI:
-
Modified bleeding index
- NSMD:
-
Non-surgical mechanical debridement
- NSPT:
-
Non-surgical periodontal therapy
- PD:
-
Probing depth
- PI:
-
Plaque index
- PM:
-
Peri-implant mucositis
- UWS:
-
Unstimulated whole saliva
References
Papaspyridakos P, De Souza A, Vazouras K, Gholami H, Pagni S, Weber HP. Survival rates of short dental implants (≤6 mm) compared with implants longer than 6 mm in posterior jaw areas: a meta-analysis. Clin Oral Implants Res. 2018;29(Suppl 16):8–20. https://doi.org/10.1111/clr.13289.
Beschnidt SM, Cacaci C, Dedeoglu K, et al. Implant success and survival rates in daily dental practice: 5-year results of a non-interventional study using CAMLOG SCREW-LINE implants with or without platform-switching abutments. Int J Implant Dent. 2018;4(1):33. https://doi.org/10.1186/s40729-018-0145-3.
Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant diseases and conditions—introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45(Suppl 20):S1–8. https://doi.org/10.1111/jcpe.12935.
Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S173–82. https://doi.org/10.1002/jper.17-0721.
Hamdy AA, Ebrahem MA. The effect of interleukin-1 allele 2 genotype (IL-1a(-889) and IL-1b(+3954)) on the individual’s susceptibility to peri-implantitis: case-control study. J Oral Implantol. 2011;37(3):325–34. https://doi.org/10.1563/aaid-joi-d-09-00117.1.
Javed F, Al-Hezaimi K, Salameh Z, Almas K, Romanos GE. Proinflammatory cytokines in the crevicular fluid of patients with peri-implantitis. Cytokine. 2011;53(1):8–12. https://doi.org/10.1016/j.cyto.2010.08.013.
Akram Z, Al-Aali KA, Alrabiah M, et al. Current weight of evidence of viruses associated with peri-implantitis and peri-implant health: a systematic review and meta-analysis. Rev Med Virol. 2019;29(3):e2042. https://doi.org/10.1002/rmv.2042.
Binshabaib M, ALHarthi SS, Salehpoor D, Michelogiannakis D, Javed F. Contribution of herpesviruses in the progression of periodontal and peri-implant diseases in systemically healthy individuals. Rev Med Virol. 2018;28(5):e1996. https://doi.org/10.1002/rmv.1996.
Preethanath RS, AlNahas NW, Bin Huraib SM, et al. Microbiome of dental implants and its clinical aspect. Microb Pathog. 2017;106:20–4. https://doi.org/10.1016/j.micpath.2017.02.009.
Do TA, Le HS, Shen YW, Huang HL, Fuh LJ. Risk factors related to late failure of dental implant-a systematic review of recent studies. Int J Environ Res Public Health. 2020. https://doi.org/10.3390/ijerph17113931.
Kullar AS, Miller CS. Are there contraindications for placing dental implants? Dent Clin North Am. 2019;63(3):345–62. https://doi.org/10.1016/j.cden.2019.02.004.
Kawamoto D, Amado PPL, Albuquerque-Souza E, et al. Chemokines and cytokines profile in whole saliva of patients with periodontitis. Cytokine. 2020;135:155197. https://doi.org/10.1016/j.cyto.2020.155197.
Kim JY, Kim HN. Changes in inflammatory cytokines in saliva after non-surgical periodontal therapy: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020. https://doi.org/10.3390/ijerph18010194.
Fonseca FJ, Moraes Junior M, Lourenço EJ, TelesDde M, Figueredo CM. Cytokines expression in saliva and peri-implant crevicular fluid of patients with peri-implant disease. Clin Oral Implants Res. 2014;25(2):e68-72. https://doi.org/10.1111/clr.12052.
Lira-Junior R, Teixeira MKS, Lourenço EJV, Telles DM, Figueredo CM, Boström EA. CSF-1 and IL-34 levels in peri-implant crevicular fluid and saliva from patients having peri-implant diseases. Clin Oral Investig. 2020;24(1):309–15. https://doi.org/10.1007/s00784-019-02935-8.
Abduljabbar T, Al-Sahaly F, Kellesarian SV, et al. Comparison of peri-implant clinical and radiographic inflammatory parameters and whole salivary destructive inflammatory cytokine profile among obese and non-obese men. Cytokine. 2016;88:51–6. https://doi.org/10.1016/j.cyto.2016.08.017.
Acquier AB, Pita AK, Busch L, Sánchez GA. Comparison of salivary levels of mucin and amylase and their relation with clinical parameters obtained from patients with aggressive and chronic periodontal disease. J Appl Oral Sci. 2015;23(3):288–94. https://doi.org/10.1590/1678-775720140458.
Granger DA, Kivlighan KT, El-Sheikh M, Gordis EB, Stroud LR. Salivary alpha-amylase in biobehavioral research: recent developments and applications. Ann N Y Acad Sci. 2007;1098:122–44. https://doi.org/10.1196/annals.1384.008.
Gonçalves Lda R, Soares MR, Nogueira FC, et al. Comparative proteomic analysis of whole saliva from chronic periodontitis patients. J Proteomics. 2010;73(7):1334–41. https://doi.org/10.1016/j.jprot.2010.02.018.
Haririan H, Bertl K, Laky M, et al. Salivary and serum chromogranin A and α-amylase in periodontal health and disease. J Periodontol. 2012;83(10):1314–21. https://doi.org/10.1902/jop.2012.110604.
Lundmark A, Johannsen G, Eriksson K, et al. Mucin 4 and matrix metalloproteinase 7 as novel salivary biomarkers for periodontitis. J Clin Periodontol. 2017;44(3):247–54. https://doi.org/10.1111/jcpe.12670.
Tabak LA. Structure and function of human salivary mucins. Crit Rev Oral Biol Med. 1990;1(4):229–34. https://doi.org/10.1177/10454411900010040201.
Liu B, Lague JR, Nunes DP, et al. Expression of membrane-associated mucins MUC1 and MUC4 in major human salivary glands. J Histochem Cytochem. 2002;50(6):811–20. https://doi.org/10.1177/002215540205000607.
Sabbagh A, Nakata H, Abdou A, Kasugai S, Kuroda S. Fluctuation of salivary alpha-amylase activity levels and vital signs during dental implant surgery. Int J Implant Dent. 2021;7(1):58. https://doi.org/10.1186/s40729-021-00339-6.
Wagner TP, Pires PR, Rios FS, et al. Surgical and non-surgical debridement for the treatment of peri-implantitis: a two-center 12-month randomized trial. Clin Oral Investig. 2021;25(10):5723–33. https://doi.org/10.1007/s00784-021-03874-z.
Barootchi S, Ravidà A, Tavelli L, Wang HL. Nonsurgical treatment for peri-implant mucositis: a systematic review and meta-analysis. Int J Oral Implantol (Berl). 2020;13(2):123–39.
Alqutub MN, Alhumaidan AA, Alali Y, et al. Comparison of the postoperative anti-inflammatory efficacy of chlorhexidine, saline rinses and herbal mouthwashes after mechanical debridement in patients with peri-implant mucositis: a randomized controlled trial. Int J Dent Hyg. 2022. https://doi.org/10.1111/idh.12582.
Renvert S, Persson GR, Pirih FQ, Camargo PM. Peri-implant health, peri-implant mucositis, and peri-implantitis: case definitions and diagnostic considerations. J Periodontol. 2018;89(Suppl 1):S304–12. https://doi.org/10.1002/jper.17-0588.
Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–35. https://doi.org/10.3109/00016356408993968.
Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. https://doi.org/10.3109/00016356309011240.
Armitage GC, Svanberg GK, Loe H. Microscopic evaluation of clinical measurements of connective tissue attachment levels. J Clin Periodontol. 1977;4(3):173–90.
Genco RJ, Grossi SG, Ho A, Nishimura F, Murayama Y. A proposed model linking inflammation to obesity, diabetes, and periodontal infections. J Periodontol. 2005;76(11 Suppl):2075–84. https://doi.org/10.1902/jop.2005.76.11-S.2075.
Mombelli A, van Oosten MA, Schurch E Jr, Land NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987;2(4):145–51. https://doi.org/10.1111/j.1399-302x.1987.tb00298.x.
Renvert S, Persson GR, Pirih FQ, Camargo PM. Peri-implant health, peri-implant mucositis, and peri-implantitis: case definitions and diagnostic considerations. J Clin Periodontol. 2018;45(Suppl 20):S278–85. https://doi.org/10.1111/jcpe.12956.
Ali D, Qasem SS, Baskaradoss JK. Periodontal clinicoradiographic status and whole saliva soluble urokinase plasminogen activation receptor and tumor necrosis factor alpha levels in type-2 diabetic and non-diabetic individuals. Oral Health Prev Dent. 2021;19(1):481–8. https://doi.org/10.3290/j.ohpd.b2082019.
Updegrave WJ. The paralleling extension-cone technique in intraoral dental radiography. Oral Surg Oral Med Oral Pathol. 1951;4(10):1250–61.
Khocht A, Janal M, Harasty L, Chang KM. Comparison of direct digital and conventional intraoral radiographs in detecting alveolar bone loss. J Am Dent Assoc. 2003;134(11):1468–75.
Javed F, Näsström K, Benchimol D, Altamash M, Klinge B, Engström PE. Comparison of periodontal and socioeconomic status between subjects with type 2 diabetes mellitus and non-diabetic controls. J Periodontol. 2007;78(11):2112–9. https://doi.org/10.1902/jop.2007.070186.
Alahmari F, Javed F, Ahmed ZU, Romanos GE, Al-Kheraif AA. Soft tissue status and crestal bone loss around conventionally-loaded dental implants placed in cigarette- and waterpipe (narghile) smokers: 8-years’ follow-up results. Clin Implant Dent Relat Res. 2019;21(5):873–8. https://doi.org/10.1111/cid.12746.
Abduljabbar T, Vohra F, Ullah A, Alhamoudi N, Khan J, Javed F. Relationship between self-rated pain and peri-implant clinical, radiographic and whole salivary inflammatory markers among patients with and without peri-implantitis. Clin Implant Dent Relat Res. 2019;21(6):1218–24. https://doi.org/10.1111/cid.12866.
Javed F, Al-Kheraif AA, Al Amri MD, et al. Periodontal parameters and whole salivary cytokine profiles among habitual gutka chewers and non-chewers. J Periodontol. 2015;86(5):689–95. https://doi.org/10.1902/jop.2015.140556.
Altay MA, Tozoğlu S, Yıldırımyan N, Özarslan MM. Is history of periodontitis a risk factor for peri-implant disease? A pilot study. Int J Oral Maxillofac Implants. 2018;33(1):152–60. https://doi.org/10.11607/jomi.5781.
Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A. Periodontitis, implant loss and peri-implantitis. A meta-analysis. Clin Oral Implants Res. 2015;26(4):e8–16. https://doi.org/10.1111/clr.12319.
Ackermann KL, Barth T, Cacaci C, Kistler S, Schlee M, Stiller M. Clinical and patient-reported outcome of implant restorations with internal conical connection in daily dental practices: prospective observational multicenter trial with up to 7-year follow-up. Int J Implant Dent. 2020;6(1):14. https://doi.org/10.1186/s40729-020-00211-z.
Cacaci C, Ackermann KL, Barth T, Kistler S, Stiller M, Schlee M. A non-interventional multicenter study to document the implants success and survival rates in daily dental practices of the CONELOG screw-line implant. Clin Oral Investig. 2019;23(6):2609–16. https://doi.org/10.1007/s00784-018-2646-0.
Javed F, Rahman I, Romanos GE. Tobacco-product usage as a risk factor for dental implants. Periodontol 2000. 2019;81(1):48–56. https://doi.org/10.1111/prd.12282.
Javed F, Romanos GE. Chronic hyperglycemia as a risk factor in implant therapy. Periodontol 2000. 2019;81(1):57–63. https://doi.org/10.1111/prd.12283.
Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Clin Periodontol. 2018;45(Suppl 20):S246–66. https://doi.org/10.1111/jcpe.12954.
Acknowledgements
The authors thank the Deanship of Scientific Research and College of Dentistry Research Center (CDRC) at King Saud University, Saudi Arabia for supporting the present research study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization, HAA, ASA, and AMB; methodology, ASA, HAA, MYS, DDD and AMB; validation, DA; formal analysis, DDD; investigation, HAA, ASA, AMB and MYS; data curation, DDD, DA and MYS; writing—original draft preparation, ASA, DA, HAA, MYS, DDD and AMB; writing—review and editing, HAA, ASA, DA, AMB, DDD and MYS; HAA, ASA and AMB; project administration, HAA, MYS; funding acquisition, ASA. All authors have read and agreed to the published version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was carried out in accordance with the Declaration of Helsinki as revised in 2013 guidelines involving human subjects. Volunteers were asked to sign a consent form. Withdraw did not bear any penalization or/and consequences. Ethical approval was obtained from ethics research committee of the Sharavathi Dental College and Hospital, Shivamogga, Karnataka, India (19/2022/CR). All individuals were also given verbal and written information about brushing and flossing techniques.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aldulaijan, H.A., Al-Zawawi, A.S., Shaheen, M.Y. et al. Assessment of salivary alpha amylase and mucin-4 before and after non-surgical treatment of peri-implant mucositis. Int J Implant Dent 8, 30 (2022). https://doi.org/10.1186/s40729-022-00429-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40729-022-00429-z