Abstract
Background
The neutrophil-to-lymphocyte ratio (NLR) proves to be a convenient and cost-effective marker with studies showing that a high NLR can serve as a mortality indicator in burn cases. We conducted a meta-analysis aiming to explore whether on-admission NLR values could serve as predictors of mortality in burn patients.
Methods
PubMed, Web of Science, Scopus and Embase were searched from inception until January 2024. We included all studies investigating burn patients that contain information on the NLR value at the time of hospital admission and mortality outcomes. The studies were critically appraised using the NIH Quality Assessment Tool.
Results
Nine studies fulfilled our criteria with a total population of 1837 participants, including 1526 survivor Burn patients and 311 non-survivor Burn patients. The overall mean difference measured by random model showed a significant increase in NLR by 5.06 (95% CI 3.42, 6.68) p ≤ 0.001 for the non-survivor group over the survivors group with heterogeneity I2 = 67.33%, p ≤ 0.001. A meta-regression was done to investigate the potential source of heterogeneity among studies. The results showed that age (p = 0.394), gender (p = 0.164), and sample size (p = 0.099) did not contribute to the source of heterogeneity, however, the burn surface area contributed significantly (p = 0.002). A leave-one-out meta-analysis was done, showing that omitting Le Qui et al., leads to significantly decrease the heterogeneity to be I2 = 2.73%. Meta-regression repeated to assess the burn surface area again to be found noncontributing (p = 0.404).
Conclusions
Our findings support that elevated NLR values can serve as a mortality indicator in burn cases. This will have a great clinical impact by aiding in stratifying the burn patients on admission.
Similar content being viewed by others
Background
Burn injuries rank as the fourth most prevalent form of trauma globally [1]. The World Health Organization reports that ~ 180,000 deaths occur annually worldwide due to burns, with a predominant occurrence in low- and middle-income countries [2].
A systemic inflammatory response is activated by thermal injuries, and it is thought to significantly contribute to the pathophysiology of the primary disturbances observed in individuals with burn injuries [3]. Traditionally, a range of clinical and laboratory indicators has been employed to assess the prognosis of burn patients. These include burn injury severity scores, RYAN score, R-BAUX score, as well as inflammatory markers such as erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and procalcitonin (PCT) [4,5,6].
As the quest for new inflammatory and prognostic markers persists, it becomes imperative to identify more readily accessible parameters, particularly given that 90% of deaths related to burns occur in low- and middle-income countries [1]. Neutrophils, which accumulate in organs due to the systemic inflammatory response following burn injuries, serve as the primary generators of free oxygen radicals. Additionally, there is an inhibition of the cellular immune response, leading to a decrease in delayed-type hypersensitivity reactions and lymphocyte count in peripheral blood [7].
The neutrophil-to-lymphocyte ratio (NLR) is recognized as a marker of systemic inflammation and has been associated with disease severity and survival across various conditions such as cancer, heart failure, sepsis, and acute respiratory distress syndrome [8,9,10,11,12,13]. The NLR is determined by dividing the absolute neutrophil count by the absolute lymphocyte count [14].
Significant burn injuries result in various changes in complete blood count (CBC) following admission [15, 16]. Likely influenced by several factors, such as hemodilution due to fluid resuscitation and bone marrow depression [17], the use of a ratio proves beneficial in illustrating the relative alterations in CBC parameters.
Numerous studies have reported the prediction of burn patient mortality based on the admission NLR [17,18,19,20,21,22,23]. Conducting a systematic review and meta-analysis, we aimed to explore whether on-admission NLR values could serve as predictors of mortality in burn patients.
Methods
Search strategy
This analysis was conducted in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [24].
PubMed, Web of Science, Scopus and Embase were systematically searched to identify suitable articles published until January 2024. The search terms included: (neutrophil to lymphocyte) OR (NLR) OR (neutrophil-to-lymphocyte) AND (Burn) AND (mortality). We searched for articles in all languages, which were translated when necessary. Articles were also identified using the “related articles” function in PubMed and by manually searching the references within identified articles. The full search strategy is described in Fig. 1.
Eligibility criteria
We included all research papers investigating burn patients that contain information on the NLR value at the time of hospital admission and mortality outcomes. The following articles were excluded from this review: non-research letters, correspondences, case reports, review articles, animal studies and studies that included only pediatrics.
Study selection
All articles obtained through systematic searches of electronic databases were transferred to EndNote 20 bibliographic and reference manager. Rayyan software was employed to eliminate duplicates. The titles and abstracts underwent independent screening by two reviewers, and potentially relevant articles were further assessed for eligibility against the predefined criteria. Any discrepancies were resolved through discussion until a mutual consensus was achieved.
Data extraction
Three reviewers separately gathered data from the included papers. Before the data extraction process, a customized, standardized form for data extraction was created. The extracted data encompassed various elements, including the first author, year of the study, publication type, study location, study design, baseline population characteristics, exposures, and outcomes.
In this context, exposure was defined as the NLR value upon admission to the hospital, presented in terms of continuous NLR values. The primary outcome of interest was mortality. The data initially presented as median and IQR were transformed into mean and SD using established tools from previous publications [25, 26].
Quality assessment
The studies were critically appraised using the NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies and the NIH quality assessment tool for observational case–control studies by three independent reviewers, and when there was a discrepancy in the assessment score, discussions were done to reach an agreement [27].
Statistical analysis
The meta-analysis was performed using the Stata 18 software. Continuous variables were expressed as MD (mean difference), with each effect size expressed as a 95% confidence interval (CI). The value of I2 < 50% indicated the lack of heterogeneity across the studies, when statistical heterogeneity was indicated; Meta-regression was done to detect source. Sensitivity analysis was done using a leave-one-out meta-analysis to show how each individual study affects the overall estimate by removing one study alternately from the meta-analysis. Publication bias was assessed qualitatively using the funnel plot and quantitatively using Egger's linear regression test to evaluate the presence of small-study effects. A meta-regression was performed for the following potential confounders: age, gender, burn area and sample size. A statistically significant difference was considered if a two-tailed p < 0.05.
Results
Search results
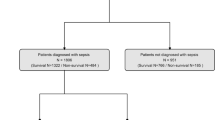
Our search strategy resulted in a total number of 264 studies. After the title and abstract screening and removing the duplicates, 134 articles were eliminated, and 16 full-text articles were evaluated for eligibility. Following the full-text screening, 9 papers [17,18,19,20,21,22,23, 28, 29] met our criteria and were included in our systematic review and meta-analysis (Fig. 1).
NLR and mortality
We included 9 studies (6 cross sectional, 2 retrospective cohort and 1 case control) with a total population of 1837 participants, including 1526 survivor burn patients and 311 non-survivor burn patients. The mean age of participants was 38.15 year. Of which, 1284 were males, and 557 were females. The main characteristics of the included studies are summarized in Table 1.
The overall mean difference showed a significant increase in NLR by 5.06(95% CI 3.42, 6.68) p ≤ 0.001 for the non-survivors group over the Survivors group with heterogeneity I2 = 67.33%, p ≤ 0.001 (Fig. 2).
A meta-regression was done to investigate the potential source of heterogeneity among studies. The results showed that age (p = 0.394), gender (p = 0.164), and sample size (p = 0.099) did not contribute to the source of heterogeneity; however the burn surface area contributed significantly (p = 0.002).
A leave-one-out meta-analysis was done (Fig. 3), showing that omitting Le Qui et al. [29] leads to significantly decrease the heterogeneity to be I2 = 2.7%. Meta-regression repeated to assess the burn surface area again to be found noncontributing (p = 0.404).
Publication bias
Visual inspection of the funnel plot of the first meta-analysis did not show asymmetry, as shown in Fig. 4, Egger’s test showed that publication bias was statistically insignificant (p = 0.7371).
Quality assessment
For the cohort and cross-sectional studies reviewed by the NIH tool, one was good quality, and seven were fair quality and for observational case–control study reviewed by the NIH tool, the study was fair (Figs. 5, 6).
Discussion
Burn injuries trigger the activation of complex mediator systems, resulting in pathophysiological changes within the body [30]. Various biochemical values have been utilized as prognostic factors for sepsis and mortality in burn patients [31]. The neutrophil-to-lymphocyte ratio (NLR) proves to be a convenient and cost-effective marker, readily available without the need for additional laboratory testing. Previous research has demonstrated that a high NLR is associated with increased morbidity and prolonged hospital stays [32], indicating its potential as an indicator of the inflammatory process. Accumulating evidence from several studies suggests that an elevated NLR can serve as a mortality indicator in burn cases.
While several studies, including ours, have evaluated the use of NLR as a prognostic factor in burn patients, a meta-analysis specifically focusing on the admission neutrophil-to-lymphocyte ratio in predicting mortality in burn patients has not been conducted to our knowledge. All studies included in our meta-analysis were retrospective.
Our analysis, incorporating nine studies and a total of 1837 patients (1526 survivors and 311 non-survivors), revealed that the mean admission NLR was significantly higher in non-survivors compared to survivors. The overall mean difference indicated a significant increase in NLR by 5.06 (95% CI 3.42, 6.68), with a p-value of < 0.001 for the non-survivors group over the survivors group. However, there was heterogeneity observed (I2 = 67.33%, p ≤ 0.001). A leave-one-out meta-analysis demonstrated that omitting the study by Le Qui et al. [29] led to a significant decrease in heterogeneity to I2 = 2.73%.
The observed heterogeneity introduced by Le Qui et al. may be attributed to their specific inclusion criteria. Notably, they excluded patients who died within the first 7 days of admission, potentially overlooking cases with high neutrophil-to-lymphocyte ratio (NLR) in the early phase, which might have otherwise contributed to the mortality group. Additionally, their study incorporated individuals with the highest percentage of total body surface area (%TBSA) of ≥ 30%, further influencing the composition of their participant cohort.
Neutrophils, accumulating in organs due to the systemic inflammatory response triggered by burn injuries, serve as the primary source of free oxygen radicals, inducing tissue damage. There is also a suppression in cellular immune response results in reduction of lymphocyte count in the peripheral blood [7]. This process aligns with our findings that demonstrated higher NLR values in the non-survivor group. The results suggest that on-admission NLR can function as a prognostic factor for burn patients, as it reflects the systemic inflammatory response and correlates with adverse outcomes.
In a meta-analysis by Huang et al., it was suggested that neutrophil-to-lymphocyte ratio (NLR) could serve as a prognostic biomarker in sepsis patients, indicating poor outcomes for those with elevated NLR levels. It is worth noting that this conclusion, although applicable to sepsis, was not specific to burn cases. Additionally, conditions like cachexia might not trigger an increase in neutrophils, leading to a potential false-negative interpretation of neutrophil values in predicting sepsis. Simultaneously, the inflammatory process could cause a decrease in lymphocyte levels. The NLR, considering both parameters, is considered more reliable than relying solely on neutrophil or lymphocyte levels alone [33].
Previous studies reported normal mean value of NLR across all ages as 1.65, with men having a mean of 1.63 and women 1.66 [14, 34].
The Baux score, a prediction model for mortality after acute burn injury, incorporates age and burn size (TBSA%). Two studies analyzing Baux score correlated with NLR values found that patients with higher NLR values were in the mortality group and exhibited persistently higher R-BAUX scores [20, 28].
Despite our study's contributions, it has several limitations. Firstly, all the studies included are retrospective, introducing potential biases. Secondly, some crucial individual information was not provided, limiting the ability to perform a more accurate analysis stratified by different risk factors. Comorbidities were not reported in any of the studies, as most excluded patients with preexisting chronic diseases. None of the studies documented wound culture during admission to exclude wound infection. Time until admission was reported in only one study [20]. Admission severity scores (SOFA and ABSI) were mentioned only once [17, 20], while the BAUX score was reported in only two studies [20, 28]. Additionally, there was insufficient data on treatment modalities. The type and degree of burns were not detailed in most studies, an important factor, such as the surface area of burns, was mentioned in only 7 out of our 9 studies as shown in Table 1. Three studies only reported the sensitivity and specificity of the NLR as a marker, but was not sufficient to perform a reliable diagnostic test accuracy [17, 21, 29].
Thirdly, the inclusion of four out of the eight studies conducted in Asian countries raises the potential for immune variability among diverse ethnic populations [35]. Future studies with larger, more homogeneous populations are essential for advanced assessment of the true role of NLR in predicting outcomes for burn patients.
Conclusions
NLR was found to be a feasible marker for predicting outcomes for burn patients. We think it should be studied in combination with other clinical parameters to be more accurate and precise.
Availability of data and materials
The presented data in the manuscript are available from the authors with a reasonable request.
Abbreviations
- NLR:
-
Neutrophil-to-lymphocyte ratio
- NIH:
-
National Institutes of Health
References
Peck MD (2011) Epidemiology of burns throughout the world. Part I: distribution and risk factors. Burns 37(7):1087–1100
Smolle C, Cambiaso-Daniel J, Forbes AA, Wurzer P, Hundeshagen G, Branski LK et al (2017) Recent trends in burn epidemiology worldwide: a systematic review. Burns 43(2):249–257
Farina JAJ, Rosique MJ, Rosique RG (2013) Curbing inflammation in burn patients. Int J Inflam 2013:715645
Halgas B, Bay C, Foster K (2018) A comparison of injury scoring systems in predicting burn mortality. Ann Burns Fire Disasters 31(2):89–93
Egea-Guerrero JJ, Martínez-Fernández C, Rodríguez-Rodríguez A, Bohórquez-López A, Vilches-Arenas A, Pacheco-Sánchez M et al (2015) The utility of C-reactive protein and procalcitonin for sepsis diagnosis in critically burned patients: a preliminary study. Plast Surg (Oakville, Ont) 23(4):239–243
Mokline A, Garsallah L, Rahmani I, Jerbi K, Oueslati H, Tlaili S et al (2015) Procalcitonin: a diagnostic and prognostic biomarker of sepsis in burned patients. Ann Burns Fire Disasters 28(2):116–120
Jacob S, Herndon DN, Hawkins HK, Enkhbaatar P, Cox RA (2017) Xanthine oxidase contributes to sustained airway epithelial oxidative stress after scald burn. Int J Burns Trauma 7(6):98–106
Zahorec R (2001) Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 102(1):5–14
Hwang SY, Shin TG, Jo IJ, Jeon K, Suh GY, Lee TR et al (2017) Neutrophil-to-lymphocyte ratio as a prognostic marker in critically-ill septic patients. Am J Emerg Med 35(2):234–239
Wang Y, Ju M, Chen C, Yang D, Hou D, Tang X et al (2018) Neutrophil-to-lymphocyte ratio as a prognostic marker in acute respiratory distress syndrome patients: a retrospective study. J Thorac Dis 10(1):273–282
Benites-Zapata VA, Hernandez AV, Nagarajan V, Cauthen CA, Starling RC, Tang WHW (2015) Usefulness of neutrophil-to-lymphocyte ratio in risk stratification of patients with advanced heart failure. Am J Cardiol 115(1):57–61
Yoldas H, Karagoz I, Ogun MN, Velioglu Y, Yildiz I, Bilgi M et al (2020) Novel mortality markers for critically ill patients. J Intensive Care Med 35(4):383–385
Yao C, Liu X, Tang Z (2017) Prognostic role of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio for hospital mortality in patients with AECOPD. Int J Chron Obstruct Pulmon Dis 12:2285–2290
Forget P, Khalifa C, Defour J-P, Latinne D, Van Pel M-C, De Kock M (2017) What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res Notes 10(1):12
Sen S, Hsei L, Tran N, Romanowski K, Palmieri T, Greenhalgh D et al (2019) Early clinical complete blood count changes in severe burn injuries. Burns 45(1):97–102
Osuka A, Ishihara T, Shimizu K, Shintani A, Ogura H, Ueyama M (2019) Natural kinetics of blood cells following major burn: impact of early decreases in white blood cells and platelets as prognostic markers of mortality. Burns 45(8):1901–1907
Angulo M, Moreno L, Aramendi I, Dos Santos G, Cabrera J, Burghi G (2020) Complete blood count and derived indices: evolution pattern and prognostic value in adult burned patients. J Burn care Res Off Publ Am Burn Assoc 41(6):1260–1266
Ciftci A, Esen O, Yazicioglu MB, Haksal MC, Tiryaki C, Gunes A et al (2019) Could neutrophil-to-lymphocyte ratio be a new mortality predictor value in severe burns? J Surg Surg Res 5(1):26–28
Juárez Guzmán U, Sánchez Zúñiga M de J. Asociación entre índice neutrófilo/linfocito como biomarcador de mortalidad en pacientes con quemaduras mayores durante el periodo del 01 de febrero de 2020 al 28 de enero de 2022. Med crítica (Colegio Mex Med Crítica). 2023;37(1):17–20.
Steinvall I, Elmasry M, Abdelrahman I, El-Serafi A, Sjöberg F (2021) Addition of admission lactate levels to Baux score improves mortality prediction in severe burns. Sci Rep 11(1):18038. https://doi.org/10.1038/s41598-021-97524-9
Lesmanawati FE, Saputro ID, Hariani L (2023) Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in burn patients with and without COVID-19. Int J Res Publ. 121(1):e6
Setiawan AA, Prayoga GH, Sanjaya I, Herawati S, Adnyana I, Hamid ARRH et al (2022) High neutrophil–lymphocyte ratio as a predictor of mortality in major burn patients. Int J Health Sci (Qassim) 6(S8):3966–3975
Temiz A, Albayrak A, Peksöz R, Dışcı E, Korkut E, Tanrıkulu Y et al (2020) Factors affecting the mortality at patients with burns: single centre results. Ulus travma ve acil cerrahi Derg Turkish J Trauma Emerg Surg TJTES. 26(5):777–783
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1-34
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27(6):1785–1805
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services. Study Quality Assessment Tools. 2019. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
Bhuyan G, Pathak C, Ranga S (2020) The value of neutrophil to lymphocyte ratio, platelet count and red cell distribution width to platelet ratio as prognostic markers in burn patients. Int J Med Lab Res 5(3):19–23
Qiu L, Jin X, Wang J-J, Tang X-D, Fang X, Li S-J et al (2021) Plasma neutrophil-to-lymphocyte ratio on the third day postburn is associated with 90-day mortality among patients with burns over 30% of total body surface area in two Chinese burns centers. J Inflamm Res 14:519–526
Nielson CB, Duethman NC, Howard JM, Moncure M, Wood JG (2017) Burns: pathophysiology of systemic complications and current management. J Burn care Res Off Publ Am Burn Assoc 38(1):e469–e481
Zhang P, Zou B, Liou Y-C, Huang C (2021) The pathogenesis and diagnosis of sepsis post burn injury. Burn Trauma. 9:ktkaa047
Gunduz M, Ciftci I, Yasti AC, Guven A (2020) Red cell distribution width and neutrophil-to-lymphocyte ratio as a predictive factor in treatment of pediatric patients with burns. Int J Burns Trauma 10(4):101–106
Huang Z, Fu Z, Huang W, Huang K (2020) Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: a meta-analysis. Am J Emerg Med 38(3):641–647
Lee JS, Kim NY, Na SH, Youn YH, Shin CS (2018) Reference values of neutrophil–lymphocyte ratio, lymphocyte–monocyte ratio, platelet–lymphocyte ratio, and mean platelet volume in healthy adults in South Korea. Medicine (Baltimore) 97(26):e11138
Chen M-H, Raffield LM, Mousas A, Sakaue S, Huffman JE, Moscati A et al (2020) Trans-ethnic and ancestry-specific blood-cell genetics in 746,667 individuals from 5 global populations. Cell 182(5):1198-1213.e14
Acknowledgements
None.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). No fund has been received for this work and the first author is responsible for all charges related to the manuscript.
Author information
Authors and Affiliations
Contributions
Study design: MKA and AE; searched databases and collected studies: MKA and MA; extracted and analyzed the data: RA, NG and MR; evaluation of the quality of the literature: AMAS, MR and GE; statistical analyses: AE and MKA; wrote the manuscript: MKA, AE and RERA; manuscript reviewed: FF. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Since this is a meta-analysis, consent for data collection was already given during enrollment in the original studies.
Consent for publication
Not applicable.
Competing interests
None of the authors have any financial or nonfinancial competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Awad, M.K.A., Elsahhar, A., Alwakeel, M. et al. Admission neutrophil-to-lymphocyte ratio to predict mortality in burn patients: a meta-analysis. ICMx 12, 86 (2024). https://doi.org/10.1186/s40635-024-00668-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-024-00668-x