Abstract
Therapeutic plasma exchange (TPE) is a therapeutic intervention that separates plasma from blood cells to remove pathological factors or to replenish deficient factors. The use of TPE is increasing over the last decades. However, despite a good theoretical rationale and biological plausibility for TPE as a therapy for numerous diseases or syndromes associated with critical illness, TPE in the intensive care unit (ICU) setting has not been studied extensively. A group of eighteen experts around the globe from different clinical backgrounds used a modified Delphi method to phrase key research questions related to “TPE in the critically ill patient”. These questions focused on: (1) the pathophysiological role of the removal and replacement process, (2) optimal timing of treatment, (3) dosing and treatment regimes, (4) risk–benefit assumptions and (5) novel indications in need of exploration. For all five topics, the current understanding as well as gaps in knowledge and future directions were assessed. The content should stimulate future research in the field and novel clinical applications.
Similar content being viewed by others
Background
Therapeutic plasma exchange (TPE) is a routine method that separates plasma from blood cells to remove pathological factors or to deliver deficient ones. Consistently, it is used for numerous diseases characterized by the presence of harmful circulating factors or the deficiency of protective components. Given a biological plausibility of benefit in many critical care syndromes [1], it is surprising that there is remarkably little evidence concerning to potential indications, dosing, timing, regimen, and adverse events in the critically ill patient. Given the huge potential of plasma exchange, a recent review has summarized its use in the ICU setting [1]. Here, a group of experts from mixed medical backgrounds used a modified Delphi method to identify remaining gaps in knowledge and framed key research questions for studies on the use of TPE in critically ill patients.
Methods
This research agenda was developed in a stepwise approach starting with the development of a panel of 18 international experts from different fields (intensive care medicine, hematology/oncology, nephrology, transfusion medicine Additional file 1: Table S1). An initial list of potential key research questions yielded 16 potential questions. In a next step, 16 of the experts from the panel scored each question from 0 to 5 using an electronic survey tool (Table 1). The five topics with the highest rankings were considered top research priorities and have been addressed in this article (Fig. 1). Each topic was elaborated in a sub-panel of 5 to 7 experts in a structured standardized fashion summarizing both the current knowledge and the knowledge gaps.
Results
Question 1. What is the pathophysiological role of removal and/or replacement of circulating factors during critical illness?
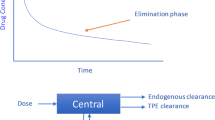
Filling in the knowledge gaps about the pathophysiologic concepts of TPE, particularly in explorative settings, is important. Increased circulating levels of a molecule that is typically thought injurious might be part of a crucial compensatory mechanism and its removal may harm certain patients. Furthermore, it is important to recognize that TPE combines two procedures in one (i.e.: the removal of potentially harmful plasma components and the replacement of potentially protective ones, Fig. 2).
Schematic illustration of potential (explorative) targets for replacement and removal by plasma exchange (adjusted from [99]). DAMPs damage associated molecular patterns, VWF von Willebrand factor, ULVWM ultralarge von Willebrand multimers, Angpt-1/-2 angiopoietin, VEGF vascular endothelial growth factor, Hpa-1/-2 heparanase, ATIII antithrombin III, ADAMTS13 A disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13
What is known
Both the removal and replacement of factors are dependent on the exchange fluid being used (plasma vs. albumin), the volume replaced, and the kinetics and dynamics of the individual target factor (such as protein binding, volume of distribution). Table 2 summarizes injurious circulating factors that are elevated and/or protective factors that are depleted during various conditions. A prototype of this “replacement” aspect is the vWF-cleaving protease termed “A disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13” (ADAMTS13) deficiency [2]. Lack of this protease is the characteristic feature of thrombotic thrombocytopenic purpura (TTP) for which TPE is still considered the gold standard treatment [3]. Obviously, in any type of disease, deficient plasma components can only be supplemented if plasma from healthy donors is used as a replacement solution.
What is not known
-
What is the effect of TPE on host immune response?
Most studies investigating TPE have shown a decrease in pro-inflammatory cytokines after TPE in a broad range of diseases, such as Systemic Lupus Erythematosus (SLE) and Chimeric Antigen Receptor (CAR) T-cells associated cytokine release syndrome (CRS) [4,5,6,7,8]. Conversely, the anti-inflammatory cytokine IL-10 increased after TPE in patients with myasthenia gravis [7].
However, a fundamental question behind the concept of removal is the consideration that it might not be beneficial per se to remove “bad things”. This concept is of interest for any blood purification technique and refers to the fact that even a massive elevation of an injurious mediator might be a protective strategy of the organism in the sense of an evolutionary preserved compensatory mechanism in a given disease state. In this case, pure extracorporeal removal could be harmful as it has recently been demonstrated for some adsorptive techniques [9].
Another known phenomenon is the “rebound” that occurs after completion of TPE sessions, suggesting a transient effect on cytokines [10] or a re-distribution from third spaces. De novo production of cytokines may also greatly vary [11] and influence plasma cytokine levels according to the underlying disease and the degree of extracorporeal removal. Along these lines, it remains uncertain how the removal of systemically elevated cytokines can modulate their levels within organs and tissues.
Beyond the mechanical removal of circulating antibodies, TPE might be able to indirectly modulate cellular host immune responses as well. TPE has been associated with a decline in B-cell and T-cell activation [5]. However, the potential impact of TPE on skewing T helper (Th) 1/Th2 balance is controversial [6, 12].
Although the clinical consequences remain uncertain to date, the risk of procedure-associated infection appears to be very low [13, 14].
-
How to predict the effect of TPE on individual coagulation factors?
TPE results in a ‘regression to the mean’ of circulating proteins, in which coagulation factors that are lacking will increase following exchange with normal donor plasma, whereas factors that are elevated might be diluted to a “normal” level following TPE. As there is significant heterogeneity of individual coagulation factors among healthy donors, the effect of TPE with single donor plasma is hard to predict [11, 15]. Studies that compared TPE sessions using single donor versus pooled plasma (where the anticoagulation factor profile is known and relatively stable) are lacking.
Dilutional coagulopathy occurs when the patients’ plasma is exchanged with albumin or saline [1, 16]. However, TPE does not remove single factors but leads to a balanced reduction of pro- and anticoagulant proteins [17], which might explain the relatively low prevalence of bleeding [18]. Nevertheless, there is significant uncertainty with regards to both coagulation monitoring during exchange regimens and the cumulative effect of multiple exchange sessions [19].
-
What is the pathophysiological effect of plasma exchange on the endothelium?
Endothelial dysfunction is a cornerstone of several diseases such as sepsis, COVID-19 or preeclampsia [20,21,22] and may be modulated by TPE. Rheological phenomena provoked by the exchange process are not well understood [23]. Given the surface localization, the dynamics and susceptibility to flow, the endothelial glycocalyx may be shed due to altered shear stress [24] and to altered plasmatic protein composition. On the other hand, some reports connect properties of human plasma and albumin with stabilization or even restoration of glycocalyx components [25]. Antagonistic glycocalyx modulating enzymes termed heparanases (e.g.: Hpa-1 and Hpa-2) are also re-balanced by TPE and might contribute to endothelial health [26, 27].
-
What is the effect of the type of replacement fluids on host responses?
Apart from coagulation, the effects of plasma or non-plasma replacement fluids on immune signalling, endothelial function, inflammation, complement activity, etc. remain largely unexplored. If plasma is the selected replacement fluid, additional questions emerge, such as “what is the optimal type of plasma”—for instance, the potentially different, subtle effects of liquid (never-frozen) plasma compared to fresh frozen plasma (FFP) or plasma frozen within 24 h (FP-24), or standard plasma (FFP or FP-24) compared to cryo-poor plasma (CPP). On an even deeper level, variables such as age/sex/ethnicity/immune status of the donor or proteomic/metabolomics/transcriptomic composition of the units and the processing technique [28] may potentially influence the effects of plasma exchange on the recipient beyond that of the intended primary effect of antibody removal or replacement.
Question 2. What is the optimal timing of TPE with respect to other concomitant treatments?
The timing of TPE might be crucial in terms of both desired therapeutic and undesired off-target effects, which occur by removing concomitantly administered treatments for the underlying disease, for instance intravenous immunoglobulins (IVIG), rituximab, cyclophosphamide, caplacizumab, and antibiotics.
What is known
The amount of components that are removed depends on the volume of distribution of the drug, the half-life of the drug in the circulation, and whether the agent is administered immediately before or even during TPE. In general, compounds with a low volume of distribution (< 0.2 L/Kg) or high protein binding (80%) are removed during TPE [29, 30]. A recent manuscript summarized the theoretical removal rates of COVID-19 drugs based on these pharmacokinetic considerations [31].
What is not known
-
How should drug administration be timed if a critically ill patient is on a TPE regime?
Current information leaflets of literally any drug completely lack dose recommendations for patients receiving TPE. A list of drugs commonly prescribed in the ICU with a high likelihood of removal by TPE—analogous to the recent COVID-19 paper by Shokouhi [31]—is highly desirable.
It is reasonable to administer drugs after a TPE session to avoid unwanted removal. Nevertheless, for large drugs with a long intravascular half-life, it remains unclear if drug removal still occurs during the next session of TPE up to 24 h later. Re-dosing of drugs such as antibiotics should be considered. Therapeutic drug monitoring (TDM) before and after TPE together with the measurement of levels of drugs in the removed plasma might increase knowledge.
-
How should established treatments of an underlying disease be timed if a critically ill patients is on a TPE regimen?
The comparison with alternative strategies such as IVIG e.g. in neurological entities for the induction of disease remission is under-studied and it remains unknown if such gold-standard treatments should be given upfront or at the end of a TPE course in the sense of a rescue approach in refractory scenarios.
Question 3. What is the optimal dose and regimen of TPE?
Most centres perform three to five sessions on a daily or alternate day fashion. In addition, TPE doses (i.e. the exchanged plasma volumes) are undetermined and there is huge heterogeneity in clinical practice. In TTP, stopping criteria are biologically driven including an increase in platelets above a certain threshold. In other conditions, stopping criteria are less clear.
What is known
Knowledge about the removal capacities of plasma proteins is based on studies that assessed IgG and IgM levels during the course of multiple types of TPE. Small molecules with a large volume of distribution (e.g. IgG) have a removal of 65–70% after the first session with a significant redistribution following TPE [29]. The removal of large molecules with a small volume of distribution (e.g. IgM) is similar but lacks the subsequent re-distribution. Under steady-state conditions, 3–5 sessions exchanging 1–1.5 plasma volumes are sufficient to remove most molecules to a level below 90% [1]. However, if the substances are predominantly intravascular (e.g.: IgM), even one session with a high exchange volume might be satisfactory and can remove 86 to 92%. Mathematical models to predict the removal kinetics have been computed [29].
What is not known
Known removal rates of IgG and IgM have been generated in stable patients and are likely not applicable to critically ill individuals with alterations in distribution volumes, renal function and nutritional status.
Future pharmacokinetic studies must attempt to identify the ideal regimen in terms of the total number of sessions, frequency intervals, and plasma volume to exchange, and these questions must be evaluated in various disease states.
The monitoring of absolute circulating levels of a putative pathophysiological factor to steer the optimal TPE treatment regimen could be an interesting approach to test. In other words, the actual level of an elevated target (e.g. autoimmune antibody) has never been tested as a predictor of TPE response nor as stopping criteria in a longitudinal fashion.
An apheresis registry collecting the type of apheresis procedures performed in the ICU as well as indications, intensity of therapeutic procedures, reasons to continue or discontinue and associated outcomes is strongly encouraged.
Question 4. How to identify critically ill patients at risk of complications?
What is known
TPE is associated with several complications and undesirable effects. Besides removal of beneficial molecules (discussed earlier), technical complications of TPE comprise catheter- and procedure-related events. Potentially life-threatening complications are rare. The most important ones are anaphylactic reactions occurring in < 0.1 up to 2% of patients [14, 32]. Hypocalcemia is often observed due to a combination of citrate-based TPE circuit anticoagulation and the addition of citrate to plasma as anticoagulant. TPE may cause or worsen bleeding in susceptible patients if the exchange is not performed with plasma [33]. Nevertheless, the incidence remains low (from 0.5 to 5.4%) [34] and most bleeding events are related to central vascular catheter complications. Other complications relate to misinterpretation of routine diagnostic biomarkers as these may also be removed during TPE. An observational study showed that a single TPE reduced the plasma levels of N-terminal (NT)-pro b-type natriuretic peptide (BNP) (NT-pro BNP) by 23%, C-reactive protein (CRP) by 64%, procalcitonin by 31% and troponin-T by 14% [35].
What is not known
-
What factors are removed unintentionally?
So far, no studies have investigated undesired off-target effects of TPE as a results of unintentional removal, particularly not in critically ill patients with severely altered volumes of distribution. Along these lines, data on drug removal by TPE are scarce and mostly based on case reports or series; only a few pharmacokinetic studies have been performed [36,37,38], and for most drugs, there is no information available. Although kinetic models for the prediction of substance removal have been developed, drug dosing in TPE remains challenging and requires further research.
-
How to prevent allergic reactions and deal with re-exposure?
The use of premedication regimens might reduce allergic reactions in certain patient groups [39], but it remains unclear whether pre-medication (and which) should be routinely administered. Within different centers, the standard procedure varies substantially from no pretreatment to antihistamines alone or in combination with steroids. In addition, data on timing and standardized dosing remains scant. Appropriate strategies for re-exposure to FFP following anaphylactic type reactions vary and proposals for standardized investigations to determine risk factors for allergic reactions in the context of TPE are lacking.
-
How to reduce the bleeding risk and to dose anticoagulation?
Guidelines from the American Society For Apheresis (ASFA) recommend (based on weak evidence) that physicians consider replacing coagulation factors in patients receiving daily TPE with albumin [40]. Specific therapeutic strategies to prevent bleeding in high-risk patients are not well defined. Also, the need for anticoagulation is not completely elucidated. In a study of 367 TPE sessions it appeared that TPE without anticoagulation may be safe [34], although this strategy has not been adopted in routine clinical practice.
-
How to interpret routine biomarkers during TPE?
The interpretation of any circulating biomarker during TPE is challenging. For instance, in patients with an infection, a decrease in CRP is usually interpreted as disease resolution. If a patient is simultaneously receiving TPE daily regimen, such a fall in CRP cannot be attributed only to resolving infection but may also be due to removal during TPE. These considerations are valid for any marker circulating in plasma (e.g.: liver enzymes, renal test, cardiac biomarker, etc. [35]) the degree of removal of these biological markers during TPE is unknown. The most effective strategies to monitor organ function during TPE and recognize complications are not fully understood. Studies that analyze the elimination rate of routine biomarkers by TPE are highly desirable.
Question 5. What are explorative TPE indications for critically ill patients?
In theory, any condition induced by a known or suspected circulating factor might benefit from its removal. Diseases and syndromes such as sepsis, hemophagocytic lymphohistiocytosis (HLH), CAR T-cell associated cytokine release syndrome (CRS), and pancreatitis share common phenotypic features of systemic hyper-inflammation with endothelial dysfunction and coagulopathy. The excess release of injurious cytokines, damage-associated molecular patterns (DAMPs), cell-free DNA and neutrophil extracellular traps (NETs) together with a reduction in protective plasmatic factors are involved in many pathophysiological processes. In this section, we discuss the potential of TPE to improve some of these syndromes (structured in seven core topics summarized in Additional file 1: Table S2.
Systemic inflammatory conditions
What is known
In sepsis, TPE might modulate biological efficacy endpoints related to inflammation, coagulation, microcirculation and endothelial function [27, 41, 42]. A recent pilot randomized controlled trial (RCT) in early refractory septic shock demonstrated improved hemodynamics within 6 h compared to standard of care [43] and a propensity score matched analysis [44] revealed a potential survival benefit. Mechanistically, it has been shown that restoration of the balance between reduced ADAMTS13 activity and elevated VWF-antigen to a normal ratio might improve microvascular perfusion and flow. Along the same line, TPE can replace consumed anticoagulant proteins such as Protein C [42].
TPE has also been proposed as a therapeutic option to treat critically ill COVID-19 patients [45]. A recent systematic review of 267 patients demonstrated safety and some biological efficacy with regards to inflammation and immune activation [46]. An RCT of 87 patients with life-threatening COVID-19 found a shorter ventilation time and even a trend towards lower mortality (20.9 vs. 34.1%) [47].
Data on TPE in sterile systemic inflammatory conditions such as acute pancreatitis, CAR T-cell associated CRS, HLH or macrophage activation syndrome (MAS) etc. are mostly limited to case series [48,49,50,51,52].
What is not known
-
Is TPE associated with a positive clinical effect?
We still fail to comprehensively monitor the immune system confronting us with a situation where some patients might benefit from the removal of inflammatory mediators while others could suffer harm by the same intervention. Besides a theoretical rationale and an increasing body of evidence regarding biological and some efficacy endpoints, it remains unclear whether improvements in surrogates such as circulating mediators actually translate into improved clinical conditions.
-
Which inflammatory patient would benefit?
In terms of response prediction, it has been reported that baseline lactate levels were predictive of the effect of TPE on hemodynamic stabilization during the initial 24 h [42]. Given the role of lactate in states of microcirculatory compromise, it can be speculated that systemically inflamed patients with microvascular coagulopathy might be more susceptible to TPE (which might close the loop to the ADAMTS13/vWF axis as mentioned earlier).
Trauma, thermal injury, burns
What is known
Trauma and burns can result in strong pro-inflammatory host responses mostly driven by enormous amounts of circulating DAMPs with ensuing endothelial hyper-permeability and organ failure. Circulating levels of endothelial glycocalyx constituents in trauma are associated with adverse outcome [53].
Despite increasing recognition of the pleiotropic effects of plasma in bleeding trauma patients and the fact that plasma transfusion can improve outcomes [54,55,56], there are no data on the use of TPE in critically ill trauma patients. In a limited number of burn patients, TPE as a rescue intervention was associated with rapid resolution of shock parameters [57, 58].
What is not known
-
Could plasma exchange modulate the injurious host response to severe trauma?
As alluded to above, pleiotropic effects of plasma have been studied increasingly but the procedure of TPE per se has been neglected so far. In general, it is also uncertain whether plasma is beneficial or just that the comparator fluid (i.e. crystalloids) is detrimental, as dilution of the protein content following clear fluid infusion may result in shedding of the glycocalyx. In line with this thought, it is not known whether merely improving protein content is beneficial or whether there are specific repair factors in plasma. The ADAMTS13/vWF imbalance in sepsis also exists in patients with trauma-induced organ injury [59]. Also, it is unknown whether removal of compounds such as DAMPs with TPE is superior over plasma transfusion alone.
Severe capillary leakage is a common phenomenon in severe burn patients. In other inflammatory conditions, it has been demonstrated that TPE might be able to modulate endothelial permeability rebalancing various systems such as glycocalyx, Angiopoietin/Tie2 and potentially also bioactive adrenomedullin (bio-ADM). These observations make TPE a desirable tool to study in severely burned patients [60].
Coagulopathies (HIT and DIC)
What is known
Heparin-induced thrombocytopenia (HIT) is a pro-thrombotic complication of heparin where platelet-activating antibodies develop after exposure to heparin leading to thrombosis and thrombocytopenia [61]. TPE has been described for refractory HIT conditions to remove such specific antibodies [62].
TPE has also repeatedly been reported as a therapeutic option in sepsis-mediated disseminated intravascular coagulopathy (DIC). A recent prospective study found improved platelet counts, coagulation function and even increased survival rates after TPE [63] which is in line with observations in patients with organ failure, DIC, meningococcal septicemia, Capnocytophaga canimorsus infection and scorpion bites [63,64,65,66].
What is not known
-
What is the specific molecular target of TPE in DIC patients?
Despite the rationale to rebalance a disturbed coagulation system, in DIC, the exact target molecule is unknown. Potential candidates may be NETs and DAMPs [67], removal of which might result in an improvement of DIC. As the degree of hypofibrinolysis may vary depending on the underlying condition [68, 69], it is possible that certain subtypes of DIC where the suppression of the fibrinolytic system dominates will be more responsive to TPE. Altogether, TPE will most likely remove D-Dimers and alter fibrinogen levels but will not directly affect thrombocytopenia.
Neurological conditions
What is known
Improved recognition of rapidly progressive severe antibody-mediated central nervous system disorders, has led to an increasing interest in the use of TPE for a variety of different neurological disorders [1].
The main potential indications include antibody-mediated central nervous system (CNS) disorders such as anti- N-methyl-D-aspartate (NMDA) receptor encephalitis [70], myasthenia gravis and Guillain-Barré syndrome (GBS) [70,71,72]. Most of the experience however is limited to case series in multiple sclerosis and neuromyelitis optical spectrum disorders [73].
What is not known
-
Are there therapeutic effects of TPE in neuro-immunological diseases that go beyond the sole removal of antibodies?
In autoimmune encephalitis, the underlying mechanism of the benefit of TPE seems to be more complex than simply removing circulating pathogenic antibodies. Removal of immune complexes and cytokines or modification of the representation and function of regulatory T-cells (Treg) and natural killer cells [3] might also be beneficial.
-
Is there a role for TPE in the maintenance of disease remission?
Further research is needed to determine the role of long- term treatment effects and also TPE regimens as maintenance strategies. Overall, current TPE regimens with regard to duration, frequency as well as cessation criteria are largely arbitrary and there is huge variation between individual centers. In general, this holds true for established and explorative TPE indications, too, and is not limited to neurological entities.
Non-hematological (auto)immune conditions
What is known
While TPE has an already established role in certain autoimmune diseases, its role in non-hematological autoimmune disorders and rheumatic diseases is less clear [74].
Based on a negative RCT in patients with systemic lupus erythematosus (SLE) and nephritis [75], TPE is not recommended by the current ASFA guidelines [76]. In renal crisis due to systemic sclerosis, a single-center observational study reported better outcomes in patients where a combination therapy of TPE and angiotensin-converting-enzyme inhibitors was used [77]. In severe ANCA-associated vasculitis (AAV) a benefit of TPE to standard immunosuppressive regimens could not be demonstrated [78]. Nevertheless, these patients were not necessarily critical ill and did not suffer from diffuse alveolar hemorrhage. In patients with thyroid storm, TPE was shown to be effective in a small case series, in particular for those with poor response to conventional standard therapies [79, 80]. Obviously, the mode of action in thyrotoxicosis lies in the ability to remove thyroid hormones [81].
What is not known
-
What is the differential response at the individual organ level in systemic diseases involving multiple organs?
Apart from nephritis, the role of TPE in SLE with serious organ involvement, such as diffuse alveolar hemorrhage (DAH), pulmonary capillaritis [71, 82, 83], neuropsychiatric involvement [84] or myocarditis is not clear. Evidence provided by small case series and reports support a potential benefit in this context [85].
With regard to systemic sclerosis, despite the aforementioned potential role in severe renal crisis, the role of TPE in other forms of systemic sclerosis, such as diffuse skin sclerosis is unclear [86]. Given the rationale that the pathogenesis of skin sclerosis is closely related to circulating factors, some authors recommend the use of TPE in these situations [87]. However, the literature is mostly outdated and does not reflect modern techniques. Another limitation is based on the heterogeneity of study design in which a wide range of adjunctive strategies were administered along with TPE [88, 89].
-
When to start TPE in (refractory) thyroid storm?
Despite promising data suggesting that TPE could be an effective therapy in patients with thyroid storm, the exact criteria for initiation, i.e. severity or clinical manifestations are unclear. In particular, it remains unknown whether TPE should be used as a first line therapy for severe manifestations or be reserved for refractory situations when traditional treatments have failed [81].
Transplantation
What is known
TPE has an established role in transplantation, both prior and afterwards. The transplant recipient`s defense mechanisms can be triggered in numerous ways of which some build the biological plausibility for the use of TPE.
TPE is implemented in desensitization protocols for ABO-incompatible (ABOi) transplantation to lower the isoagglutinin titers and has been used to mitigate hyperacute rejection mediated by class 1 antigens [90, 91]. TPE has also been used to remove so-called donor specific antibodies (DSA) to treat humoral rejection [92,93,94]. Transplant-associated thrombotic microangiopathy is a complication for which complement inhibition has emerged as a treatment of choice, but in situations where this approach is ineffective, TPE could be used as an alternative adjunctive strategy [95, 96].
TPE in addition to immunosuppression has been reported to show reasonable success in inducing remission of recurrent autoimmune disease in a successfully transplanted graft [97, 98].
What is not known
-
What are the ideal pre- and post- transplant TPE protocols?
TPE is included in numerous pre- and post-transplant protocols as standard of care, mostly because of the biological plausibility of the concept. However, the best frequency, timing of initiation, dosing and modality remain unclear due to lack of standardization in practice and controlled trials.
-
Are all antibody-mediated rejections (AMR) the same or is there a hierarchy of clinical significance of certain Donor Specific Antibodies (DSA) that could help to guide individual TPE strategies?
The close interplay between cellular (T-cell mediated) and humoral rejection is increasingly being recognized [93]. The underlying reasons for TPE refractoriness are not clear and a systematic histological analysis may offer some additional clues to group AMR patients from a tissue phenotype point of view to avoid the unnecessary use of TPE.
The correlation between antibody levels and onset of immunological phenomena such as AMR is not straightforward. Whether the risk is linear or whether additional factors play a cumulative role is not delineated. Hence, the goal of TPE in this context remains open for debate. In other words, it is unclear whether DSA concentrations (i.e. mean fluorescence intensity (MFI)) and classes (HLA type 1 vs type 2) should determine the intensity and duration of treatments.
Future directions
As highlighted in this manuscript, there are many promising areas with a strong biological plausibility for the use of TPE but most of the evidence suggesting a potential benefit in the context of explorative indications stems from case reports, small case-series, and retrospective or uncontrolled prospective data. There is an urgent need for trials to justify the clinical application of TPE in these settings. However, given the low incidence of some of the diseases discussed, appropriately powered trials are only feasible as a team effort with international collaboration. There are also relevant concerns about unwanted off-target effects, and uncertainties in dosing and timing.
Both observational and interventional studies are needed to determine parameters (i.e., imaging, biomarkers) to identify patients likely to benefit from TPE and those who may come to harm. Along the same lines, reliable stopping criteria are highly desirable. A development of a TPE registry would facilitate better understanding of the challenges in rarer conditions and possibly highlight any differences based on demographics.
Longitudinal bio-banking data collection could help to analyse the effect of TPE on host immune responses. Regarding the simultaneous removal of circulating biomarkers, alternative tools to assess resolution of infection are needed along with such TPE-driven changes in humoral inflammatory parameters (such as CRP or PCT).
Therapeutic drug monitoring (TDM) with determination of antibiotic levels and other essential drugs before and after treatment as well as in the apheresis waste plasma could provide novel pharmacokinetic insights, especially for drugs necessary to treat the underlying illness, such as immunosuppressants, monoclonal antibodies and anti-microbial agents. Using this information to develop a simple tool to support clinicians in predicting the impact of TPE on drug levels in individual patients should be an essential goal.
More systematic multicentric standardized data collection to evaluate the risk of allergic reactions should be encouraged to evaluate risk factors related to underlying disease, patient and choice of replacement fluid, anticoagulation, circuit, etc. Head-to-head comparisons of the various types of plasma may also be useful to understand the immunological basis for the adverse reactions. We also need prospective studies evaluating the effects of the replacement fluid (albumin versus plasma) and anticoagulant use on bleeding complications during the TPE procedure, thereby working towards defining specific preventive strategies in high-risk patients.
Two multicenter sepsis trials both in Europe and Canada (NCT05093075) will commence in 2023 investigating the role of TPE in systemic inflammatory conditions. Also, in severe COVID-19, several RCTs are still recruiting (e.g.: NCT04685655). On the other hand, syndromes with less heterogeneity than sepsis (e.g.: CAR-T associated CRS) might be easier to study. Particularly, in neurological critical care where the discovery of novel characteristic antibodies has been accelerating, a progressive increase in the number of clinical TPE applications can be expected but will need further guidance from clinical trials. Besides the known role of plasma application in the trauma patient, the exchange of plasma has never been evaluated in trauma-associated organ failure opening potential avenues for a novel approach. The role of TPE in the whole field of autoimmunity and transplantation seems more established but evidence is not much stronger.
Not all knowledge gaps can be answered in such observational clinical studies. Some molecular questions, e.g.: on the endothelial microcirculatory environment are best studied in animal disease models.
Finally, future studies must include patients' views to ensure that patient-centered outcomes are evaluated and the benefit-risk balance is assessed.
Take home message
The use of therapeutic plasma exchange in the critically ill patient is increasing, but the biological concept of simultaneous removal of injurious and replacement of protective molecules is double-edged and requires future research. A group of experts around the globe elaborated on key research questions focusing on pathophysiology, timing, dosing, side effects and explorative indications.
Availability of data and materials
Not applicable.
Abbreviations
- TPE:
-
Therapeutic plasma exchange
- ICU:
-
Intensive care unit
- VWF:
-
Von Willebrand factor
- ADAMTS13:
-
A disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13
- TTP:
-
Thrombotic thrombocytopenic purpura
- SLE:
-
Systemic Lupus Erythematosus
- CAR:
-
Chimeric Antigen Receptor
- CRS:
-
Cytokine release syndrome
- COVID-19:
-
Coronavirus disease 2019
- Hpa:
-
Heparanase
- FFP:
-
Fresh frozen plasma
- CPP:
-
Cryo-poor plasma
- IVIG:
-
Intravenous immunoglobulins
- TDM:
-
Therapeutic drug monitoring
- NT-proBNP:
-
N-terminal (NT)-pro b-type natriuretic peptide (BNP)
- CRP:
-
C-reactive protein
- PCT:
-
Procalcitonin
- TropT:
-
Troponin-T
- ASFA:
-
American Society For Apheresis
- HLH:
-
Hemophagocytic lymphohistiocytosis
- DAMPs:
-
Damage-associated molecular patterns
- NETs:
-
Neutrophil extracellular traps
- RCT:
-
Randomized controlled trial
- MAS:
-
Macrophage activation syndrome
- Bio-ADM:
-
Bioactive adrenomedullin
- HIT:
-
Heparin-induced thrombocytopenia
- DIC:
-
Disseminated intravascular coagulopathy
- CNS:
-
Central nervous system
- NMDA:
-
N-methyl-d-aspartate
- GBS:
-
Guillain–Barré syndrome
- ACE:
-
Angiotensin-converting-enzyme
- DAH:
-
Diffuse alveolar hemorrhage
- DSA:
-
Donor specific antibodies
- AMR:
-
Antibody-mediated rejection
- HLA:
-
Human leucocyte antigen
- MFI:
-
Mean fluorescence intensity
- ALF:
-
Acute liver failure
- ACLF:
-
Acute on chronic liver failure
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- ANCA:
-
Anti-neutrophil cytoplasmic antibody
- PF4:
-
Platelet factor 4
- SIRS:
-
Systemic inflammatory response syndrome
- ARDS:
-
Acute respiratory distress syndrome
- HSV:
-
Herpes simplex virus
- EBV:
-
Ebstein barr virus
- SOC:
-
Standard of care
- OBS:
-
Observational study
- CR:
-
Case report
- CS:
-
Case series
- ULVWM:
-
Ultra-large von Willebrand multimers
- Angpt:
-
Angiopoietin
- VEGF:
-
Vascular endothelial growth factor
- ATIII:
-
Antithrombin III
References
Bauer PR, Ostermann M, Russell L, Robba C, David S, Ferreyro BL, Cid J, Castro P, Juffermans NP, Montini L, Pirani T, Van De Louw A, Nielsen N, Wendon J, Brignier AC, Schetz M, Kielstein JT, Winters JL, Azoulay E, Nine II (2022) Plasma exchange in the intensive care unit: a narrative review. Intensive Care Med 48:1382–1396
Coppo P, Schwarzinger M, Buffet M, Wynckel A, Clabault K, Presne C, Poullin P, Malot S, Vanhille P, Azoulay E, Galicier L, Lemiale V, Mira JP, Ridel C, Rondeau E, Pourrat J, Girault S, Bordessoule D, Saheb S, Ramakers M, Hamidou M, Vernant JP, Guidet B, Wolf M, Veyradier A, French Reference Center for Thrombotic M (2010) Predictive features of severe acquired ADAMTS13 deficiency in idiopathic thrombotic microangiopathies: the French TMA reference center experience. PLoS ONE 5:e10208
Azoulay E, Bauer PR, Mariotte E, Russell L, Knoebl P, Martin-Loeches I, Pene F, Puxty K, Povoa P, Barratt-Due A, Garnacho-Montero J, Wendon J, Munshi L, Benoit D, von Bergwelt-Baildon M, Maggiorini M, Coppo P, Cataland S, Veyradier A, Van de Louw A, Nine-i I (2019) Expert statement on the ICU management of patients with thrombotic thrombocytopenic purpura. Intensive Care Med 45:1518–1539
Larsen FS, Schmidt LE, Bernsmeier C, Rasmussen A, Isoniemi H, Patel VC, Triantafyllou E, Bernal W, Auzinger G, Shawcross D, Eefsen M, Bjerring PN, Clemmesen JO, Hockerstedt K, Frederiksen HJ, Hansen BA, Antoniades CG, Wendon J (2016) High-volume plasma exchange in patients with acute liver failure: an open randomised controlled trial. J Hepatol 64:69–78
Sadeghi M, Daniel V, Wang H, Zeier M, Schemmer P, Mehrabi A, Lahdou I, Morath C, Opelz G (2013) Plasmapheresis adjusts inflammatory responses in potential kidney transplant recipients. Transplantation 95:1021–1029
Soltesz P, Aleksza M, Antal-Szalmas P, Lakos G, Szegedi G, Kiss E (2002) Plasmapheresis modulates Th1/Th2 imbalance in patients with systemic lupus erythematosus according to measurement of intracytoplasmic cytokines. Autoimmunity 35:51–56
Yeh JH, Wang SH, Chien PJ, Shih CM, Chiu HC (2009) Changes in serum cytokine levels during plasmapheresis in patients with myasthenia gravis. Eur J Neurol 16:1318–1322
Zenti MG, Stefanutti C (2011) Effects of selective H.E.L.P. LDL-apheresis on plasma inflammatory markers concentration in severe dyslipidemia: implication for anti-inflammatory response. Cytokine 56:850–854
Wendel Garcia PD, Hilty MP, Held U, Kleinert EM, Maggiorini M (2021) Cytokine adsorption in severe, refractory septic shock. Intensive Care Med 47:1334–1336
Shariatmadar S, Nassiri M, Vincek V (2005) Effect of plasma exchange on cytokines measured by multianalyte bead array in thrombotic thrombocytopenic purpura. Am J Hematol 79:83–88
Schirmer M, Kumar V, Netea MG, Xavier RJ (2018) The causes and consequences of variation in human cytokine production in health. Curr Opin Immunol 54:50–58
Goto H, Matsuo H, Nakane S, Izumoto H, Fukudome T, Kambara C, Shibuya N (2001) Plasmapheresis affects T helper type-1/T helper type-2 balance of circulating peripheral lymphocytes. Ther Apher 5:494–496
Coirier V, Lesouhaitier M, Reizine F, Painvin B, Quelven Q, Maamar A, Gacouin A, Tadie JM, Le Tulzo Y, Camus C (2022) Tolerance and complications of therapeutic plasma exchange by centrifugation: a single center experience. J Clin Apher 37:54–64
Lu J, Zhang L, Xia C, Tao Y (2019) Complications of therapeutic plasma exchange: a retrospective study of 1201 procedures in 435 children. Medicine (Baltimore) 98:e18308
Dielis AW, Castoldi E, Spronk HM, van Oerle R, Hamulyak K, Ten Cate H, Rosing J (2008) Coagulation factors and the protein C system as determinants of thrombin generation in a normal population. J Thromb Haemost 6:125–131
Kohli R, Allen E, Platton S, Griffin J, Manson L, MacCallum P, Green L (2022) Effect on haemostasis of different replacement fluids during therapeutic plasma exchange—a comparative multicentre observational study. J Clin Apher 37:534–543
Soares Ferreira Junior A, Hodulik K, Barton KD, Onwuemene OA (2022) Hemostatic effects of therapeutic plasma exchange: a concise review. J Clin Apher 37:292–312
Soares Ferreira Junior A, Boyle SH, Kuchibhatla M, Onwuemene OA (2022) Bleeding outcomes of inpatients receiving therapeutic plasma exchange: a propensity-matched analysis of the National Inpatient Sample. Transfusion 62:386–395
Zrimsek M, MarnPernat A (2021) Hemostasis assessment with standard coagulation tests and rotational thromboelastometry (ROTEM) during therapeutic plasma exchange treatment. Clin Nephrol 96:96–100
Fernandez S, Moreno-Castano AB, Palomo M, Martinez-Sanchez J, Torramade-Moix S, Tellez A, Ventosa H, Segui F, Escolar G, Carreras E, Nicolas JM, Richardson E, Garcia-Bernal D, Carlo-Stella C, Moraleda JM, Richardson PG, Diaz-Ricart M, Castro P (2022) Distinctive biomarker features in the endotheliopathy of COVID-19 and septic syndromes. Shock 57:95–105
Fernandez S, Palomo M, Molina P, Diaz-Ricart M, Escolar G, Tellez A, Segui F, Ventosa H, Torramade-Moix S, Rovira M, Carreras E, Nicolas JM, Castro P (2021) Progressive endothelial cell damage in correlation with sepsis severity. Defibrotide as a contender. J Thromb Haemost 19:1948–1958
Palomo M, Youssef L, Ramos A, Torramade-Moix S, Moreno-Castano AB, Martinez-Sanchez J, Bonastre L, Pino M, Gomez-Ramirez P, Martin L, Garcia Mateos E, Sanchez P, Fernandez S, Crovetto F, Escolar G, Carreras E, Castro P, Gratacos E, Crispi F, Diaz-Ricart M (2022) Differences and similarities in endothelial and angiogenic profiles of preeclampsia and COVID-19 in pregnancy. Am J Obstet Gynecol 227:277 e271-277 e216
Kirschkamp T, Schmid-Schonbein H, Weinberger A, Smeets R (2008) Effects of fibrinogen and alpha2-macroglobulin and their apheretic elimination on general blood rheology and rheological characteristics of red blood cell aggregates. Ther Apher Dial 12:360–367
Wang G, Kostidis S, Tiemeier GL, Sol W, de Vries MR, Giera M, Carmeliet P, van den Berg BM, Rabelink TJ (2020) Shear stress regulation of endothelial glycocalyx structure is determined by glucobiosynthesis. Arterioscler Thromb Vasc Biol 40:350–364
Barry M, Pati S (2022) Targeting repair of the vascular endothelium and glycocalyx after traumatic injury with plasma and platelet resuscitation. Matrix Biol Plus 14:100107
Pape T, Hunkemoller AM, Kumpers P, Haller H, David S, Stahl K (2021) Targeting the “sweet spot” in septic shock—a perspective on the endothelial glycocalyx regulating proteins Heparanase-1 and -2. Matrix Biol Plus 12:100095
Stahl K, Hillebrand UC, Kiyan Y, Seeliger B, Schmidt JJ, Schenk H, Pape T, Schmidt BMW, Welte T, Hoeper MM, Sauer A, Wygrecka M, Bode C, Wedemeyer H, Haller H, David S (2021) Effects of therapeutic plasma exchange on the endothelial glycocalyx in septic shock. Intensive Care Med Exp 9:57
Dhantole L, Dubey A, Sonker A (2019) A study on factors influencing the hemostatic potential of fresh frozen plasma. Asian J Transfus Sci 13:23–29
Reverberi R, Reverberi L (2007) Removal kinetics of therapeutic apheresis. Blood Transfus 5:164–174
Ward DM (2011) Conventional apheresis therapies: a review. J Clin Apher 26:230–238
Shokouhi S, Barati S, Kazeminia N, Jamali F, Roshan B, Sahraei Z (2021) Evaluating the elimination status of medications used for COVID-19 during hemoperfusion and therapeutic plasma exchange: a review. Int Immunopharmacol 97:107707
Lemaire A, Parquet N, Galicier L, Boutboul D, Bertinchamp R, Malphettes M, Dumas G, Mariotte E, Peraldi MN, Souppart V, Schlemmer B, Azoulay E, Canet E (2017) Plasma exchange in the intensive care unit: technical aspects and complications. J Clin Apher 32:405–412
Shunkwiler SM, Pham HP, Wool G, Ipe TS, Fang DC, Biller E, Treml A, Weiss J, Baron BW, Berg M, Therapeutic Apheresis Subsection of the A (2018) The management of anticoagulation in patients undergoing therapeutic plasma exchange: a concise review. J Clin Apher 33:371–379
Cordoba JP, Larrarte C, Ruiz A (2013) Is anticoagulation required in plasmapheresis? A University Hospital Experience in Bogota, Colombia. Transfus Apher Sci 48:301–305
Tutarel O, Golla P, Beutel G, Bauersachs J, David S, Schmidt BM, Lichtinghagen R, Kielstein JT (2012) Therapeutic plasma exchange decreases levels of routinely used cardiac and inflammatory biomarkers. PLoS ONE 7:e38573
Goto Y, Nakajima T, Suzuki T, Yamazaki S, Suzuki T, Yoshino I, Ishii I (2021) Evaluation of tacrolimus and mycophenolic acid removal by simultaneous continuous hemodiafiltration and plasma exchange in a lung transplant patient. J Clin Pharm Ther 46:515–518
Jaruratanasirikul S, Neamrat P, Jullangkoon M, Samaeng M (2022) Impact of therapeutic plasma exchange on meropenem pharmacokinetics. Pharmacotherapy 42:659–666
Li H, Gao C, Lin L, Zhang G, Fan S, Hai X (2022) Pharmacokinetics of cefoperazone/sulbactam in critically Ill thrombotic thrombocytopenic purpura patients undergoing therapeutic plasma exchange. J Clin Pharm Ther 47:1232–1239
Lee T, Yang JJ, Kim S, Lee HJ, Ko DH, Hwang SH, Kwon HS, Oh HB (2020) Risk management strategy for reducing therapeutic plasma exchange-related allergic reactions. Allergy 75:962–965
Padmanabhan A, Connelly-Smith L, Aqui N, Balogun RA, Klingel R, Meyer E, Pham HP, Schneiderman J, Witt V, Wu Y, Zantek ND, Dunbar NM, Schwartz GEJ (2019) Guidelines on the use of therapeutic apheresis in clinical practice—evidence-based approach from the writing committee of the American Society for Apheresis The Eighth Special Issue. J Clin Apher. 34:171–354
Stahl K, Bikker R, Seeliger B, Schmidt JJ, Schenk H, Schmidt BMW, Welte T, Haller H, Hoeper MM, Brand K, David S (2021) Effect of therapeutic plasma exchange on immunoglobulin deficiency in early and severe septic shock. J Intensive Care Med 36:1491–1497
Stahl K, Wand P, Seeliger B, Wendel-Garcia PD, Schmidt JJ, Schmidt BMW, Sauer A, Lehmann F, Budde U, Busch M, Wiesner O, Welte T, Haller H, Wedemeyer H, Putensen C, Hoeper MM, Bode C, David S (2022) Clinical and biochemical endpoints and predictors of response to plasma exchange in septic shock: results from a randomized controlled trial. Crit Care 26:134
David S, Bode C, Putensen C, Welte T, Stahl K, group Es (2021) Adjuvant therapeutic plasma exchange in septic shock. Intensive Care Med 47:352–354
Keith PD, Wells AH, Hodges J, Fast SH, Adams A, Scott LK (2020) The therapeutic efficacy of adjunct therapeutic plasma exchange for septic shock with multiple organ failure: a single-center experience. Crit Care 24:518
Fernandez J, Gratacos-Gines J, Olivas P, Costa M, Nieto S, Mateo D, Sanchez MB, Aguilar F, Bassegoda O, Ruiz P, Caballol B, Pocurull A, Llach J, Mustieles MJ, Cid J, Reverter E, Toapanta ND, Hernandez-Tejero M, Martinez JA, Claria J, Fernandez C, Mensa J, Arroyo V, Castro P, Lozano M, Covid Clinic Critical Care G (2020) Plasma exchange: an effective rescue therapy in critically ill patients with coronavirus disease 2019 infection. Crit Care Med 48:e1350–e1355
Beraud M, Hashami SA, Lozano M, Bah A, Keith P (2022) Role of therapeutic plasma exchange in the management of COVID-19-induced cytokine storm syndrome. Transfus Apher Sci 61:103433
Faqihi F, Alharthy A, Abdulaziz S, Balhamar A, Alomari A, AlAseri Z, Tamim H, Alqahtani SA, Kutsogiannis DJ, Brindley PG, Karakitsos D, Memish ZA (2021) Therapeutic plasma exchange in patients with life-threatening COVID-19: a randomised controlled clinical trial. Int J Antimicrob Agents 57:106334
Bosnak M, Erdogan S, Aktekin EH, Bay A (2016) Therapeutic plasma exchange in primary hemophagocytic lymphohistiocytosis: reports of two cases and a review of the literature. Transfus Apher Sci 55:353–356
Knaak C, Schuster FS, Nyvlt P, Spies C, Feinkohl I, Beutel G, Schenk T, La Rosee P, Janka G, Brunkhorst FM, Keh D, Lachmann G (2020) Treatment and mortality of hemophagocytic lymphohistiocytosis in adult critically ill patients: a systematic review with pooled analysis. Crit Care Med 48:e1137–e1146
Valade S, Azoulay E, Galicier L, Boutboul D, Zafrani L, Stepanian A, Canet E, Lemiale V, Venot M, Veyradier A, Mariotte E (2015) Coagulation disorders and bleedings in critically ill patients with hemophagocytic lymphohistiocytosis. Medicine (Baltimore) 94:e1692
Weber AL, Pape T, Zender S, Seeliger B, Schmidt JJ, Busch M, Rath AK, Schneider A, Schmidt BMW, Fuge J, Wedemeyer H, David S, Stahl K (2022) Therapeutic plasma exchange in patients with acute pancreatitis associated refractory shock and multi-organ failure. J Crit Care 72:154139
Xiao X, He X, Li Q, Zhang H, Meng J, Jiang Y, Deng Q, Zhao M (2019) Plasma exchange can be an alternative therapeutic modality for severe cytokine release syndrome after chimeric antigen receptor-T cell infusion: a case report. Clin Cancer Res 25:29–34
Suzuki K, Okada H, Sumi K, Tomita H, Kobayashi R, Ishihara T, Mizuno Y, Yamaji F, Kamidani R, Miura T, Yasuda R, Kitagawa Y, Fukuta T, Suzuki K, Miyake T, Kanda N, Doi T, Yoshida T, Yoshida S, Tetsuka N, Ogura S, Suzuki A (2022) Syndecan-1 as a severity biomarker for patients with trauma. Front Med (Lausanne) 9:985955
Gruen DS, Brown JB, Guyette FX, Vodovotz Y, Johansson PI, Stensballe J, Barclay DA, Yin J, Daley BJ, Miller RS, Harbrecht BG, Claridge JA, Phelan HA, Neal MD, Zuckerbraun BS, Billiar TR, Sperry JL, Group PAs (2020) Prehospital plasma is associated with distinct biomarker expression following injury. JCI Insight. 2020;5(8):e135350.
Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, del Junco DJ, Brasel KJ, Bulger EM, Callcut RA, Cohen MJ, Cotton BA, Fabian TC, Inaba K, Kerby JD, Muskat P, O’Keeffe T, Rizoli S, Robinson BR, Scalea TM, Schreiber MA, Stein DM, Weinberg JA, Callum JL, Hess JR, Matijevic N, Miller CN, Pittet JF, Hoyt DB, Pearson GD, Leroux B, van Belle G, Grioup PS (2015) Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA 313:471–482
Straat M, Muller MC, Meijers JC, Arbous MS, Spoelstra-de Man AM, Beurskens CJ, Vroom MB, Juffermans NP (2015) Effect of transfusion of fresh frozen plasma on parameters of endothelial condition and inflammatory status in non-bleeding critically ill patients: a prospective substudy of a randomized trial. Crit Care 19:163
Klein MB, Edwards JA, Kramer CB, Nester T, Heimbach DM, Gibran NS (2009) The beneficial effects of plasma exchange after severe burn injury. J Burn Care Res 30:243–248
Neff LP, Allman JM, Holmes JH (2010) The use of theraputic plasma exchange (TPE) in the setting of refractory burn shock. Burns 36:372–378
Matsumoto H, Takeba J, Umakoshi K, Kikuchi S, Ohshita M, Annen S, Moriyama N, Nakabayashi Y, Sato N, Aibiki M (2021) ADAMTS13 activity decreases in the early phase of trauma associated with coagulopathy and systemic inflammation: a prospective observational study. Thromb J 19:17
Linden K, Stewart IJ, Kreyer SF, Scaravilli V, Cannon JW, Cancio LC, Batchinsky AI, Chung KK (2014) Extracorporeal blood purification in burns: a review. Burns 40:1071–1078
Greinacher A (2015) Clinical practice. Heparin-induced thrombocytopenia. N Engl J Med 373:252–261
Moreno-Duarte I, Cooter M, Onwuemene OA, Ghadimi K, Welsby IJ (2021) Clinical outcomes of cardiac surgery patients undergoing therapeutic plasma exchange for heparin-induced thrombocytopenia. Vox Sang 116:217–224
Weng J, Chen M, Fang D, Liu D, Guo R, Yang S (2021) Therapeutic plasma exchange protects patients with sepsis-associated disseminated intravascular coagulation by improving endothelial function. Clin Appl Thromb Hemost 27:10760296211053312
Churchwell KB, McManus ML, Kent P, Gorlin J, Galacki D, Humphreys D, Kevy SV (1995) Intensive blood and plasma exchange for treatment of coagulopathy in meningococcemia. J Clin Apher 10:171–177
Mostafazadeh B, Gorbani A, Mogaddaspour M, KhoddamiVishteh HR (2017) The effect of plasmapheresis on treating disseminated intravascular coagulation (DIC) caused by a Hemiscorpius lepturus (Gadim) sting. Clin Toxicol (Phila) 55:902–907
Tani N, Nakamura K, Sumida K, Suzuki M, Imaoka K, Shimono N (2019) An immunocompetent case of Capnocytophaga canimorsus infection complicated by secondary thrombotic microangiopathy and disseminated intravascular coagulation. Intern Med 58:3479–3482
Liaw PC, Ito T, Iba T, Thachil J, Zeerleder S (2016) DAMP and DIC: the role of extracellular DNA and DNA-binding proteins in the pathogenesis of DIC. Blood Rev 30:257–261
Asakura H (2014) Classifying types of disseminated intravascular coagulation: clinical and animal models. J Intensive Care 2:20
Gando S, Wada H, Thachil J, Scientific, Standardization Committee on DICotISoT, Haemostasis (2013) Differentiating disseminated intravascular coagulation (DIC) with the fibrinolytic phenotype from coagulopathy of trauma and acute coagulopathy of trauma-shock (COT/ACOTS). J Thromb Haemost 11:826–835
Osman C, Jennings R, El-Ghariani K, Pinto A (2020) Plasma exchange in neurological disease. Pract Neurol 20:92–99
(1985) Plasmapheresis and acute Guillain–Barre syndrome. The Guillain–Barre syndrome Study Group. Neurology 35: 1096–1104
Chevret S, Hughes RA, Annane D (2017) Plasma exchange for Guillain–Barre syndrome. Cochrane Database Syst Rev 2:CD001798
Huang X, Wu J, Xiao Y, Zhang Y (2021) Timing of plasma exchange for neuromyelitis optica spectrum disorders: a meta-analysis. Mult Scler Relat Disord 48:102709
Zanatta E, Cozzi M, Marson P, Cozzi F (2019) The role of plasma exchange in the management of autoimmune disorders. Br J Haematol 186:207–219
Lewis EJ, Hunsicker LG, Lan SP, Rohde RD, Lachin JM (1992) A controlled trial of plasmapheresis therapy in severe lupus nephritis. The Lupus Nephritis Collaborative Study Group. N Engl J Med 326:1373–1379
Schwartz J, Padmanabhan A, Aqui N, Balogun RA, Connelly-Smith L, Delaney M, Dunbar NM, Witt V, Wu Y, Shaz BH (2016) Guidelines on the use of therapeutic apheresis in clinical practice-evidence-based approach from the Writing Committee of the American Society for Apheresis: The Seventh Special Issue. J Clin Apher 31:149–162
Cozzi F, Marson P, Cardarelli S, Favaro M, Tison T, Tonello M, Pigatto E, De Silvestro G, Punzi L, Doria A (2012) Prognosis of scleroderma renal crisis: a long-term observational study. Nephrol Dial Transplant 27:4398–4403
Walsh M, Merkel PA, Peh CA, Szpirt WM, Puechal X, Fujimoto S, Hawley CM, Khalidi N, Flossmann O, Wald R, Girard LP, Levin A, Gregorini G, Harper L, Clark WF, Pagnoux C, Specks U, Smyth L, Tesar V, Ito-Ihara T, de Zoysa JR, Szczeklik W, Flores-Suarez LF, Carette S, Guillevin L, Pusey CD, Casian AL, Brezina B, Mazzetti A, McAlear CA, Broadhurst E, Reidlinger D, Mehta S, Ives N, Jayne DRW, Investigators P (2020) Plasma exchange and glucocorticoids in severe ANCA-associated vasculitis. N Engl J Med 382:622–631
Koball S, Hickstein H, Gloger M, Hinz M, Henschel J, Stange J, Mitzner S (2010) Treatment of thyrotoxic crisis with plasmapheresis and single pass albumin dialysis: a case report. Artif Organs 34:E55-58
Petry J, Van Schil PE, Abrams P, Jorens PG (2004) Plasmapheresis as effective treatment for thyrotoxic storm after sleeve pneumonectomy. Ann Thorac Surg 77:1839–1841
Muller C, Perrin P, Faller B, Richter S, Chantrel F (2011) Role of plasma exchange in the thyroid storm. Ther Apher Dial 15:522–531
Hoshi K, Matsuda M, Ishikawa M, Mitsuhashi S, Gono T, Hashimoto T, Ikeda S (2004) Successful treatment of fulminant pulmonary hemorrhage associated with systemic lupus erythematosus. Clin Rheumatol 23:252–255
Huang DF, Tsai ST, Wang SR (1994) Recovery of both acute massive pulmonary hemorrhage and acute renal failure in a systemic lupus erythematosus patient with lupus anticoagulant by the combined therapy of plasmapheresis plus cyclophosphamide. Transfus Sci 15:283–288
Bartolucci P, Brechignac S, Cohen P, Le Guern V, Guillevin L (2007) Adjunctive plasma exchanges to treat neuropsychiatric lupus: a retrospective study on 10 patients. Lupus 16:817–822
Bonnan M, Valentino R, Debeugny S, Merle H, Ferge JL, Mehdaoui H, Cabre P (2018) Short delay to initiate plasma exchange is the strongest predictor of outcome in severe attacks of NMO spectrum disorders. J Neurol Neurosurg Psychiatry 89:346–351
Harris ES, Meiselman HJ, Moriarty PM, Metzger A, Malkovsky M (2018) Therapeutic plasma exchange for the treatment of systemic sclerosis: a comprehensive review and analysis. J Scleroderma Relat Disord 3:132–152
Rossi D, Zanatta E, Marson P, Sciascia S, Polito P, Roccatello D, Cozzi F (2017) How I treat patients with systemic sclerosis in clinical practice. Autoimmun Rev 16:1024–1028
Cozzi F, Marson P, Rosada M, De Silvestro G, Bullo A, Punzi L, Todesco S (2001) Long-term therapy with plasma exchange in systemic sclerosis: effects on laboratory markers reflecting disease activity. Transfus Apher Sci 25:25–31
Szekanecz Z, Aleksza M, Antal-Szalmas P, Soltesz P, Veres K, Szanto S, Szabo Z, Vegvari A, Szamosi S, Lakos G, Sipka S, Szegedi G, Varga J, Szucs G (2009) Combined plasmapheresis and high-dose intravenous immunoglobulin treatment in systemic sclerosis for 12 months: follow-up of immunopathological and clinical effects. Clin Rheumatol 28:347–350
Marfo K, Lu A, Ling M, Akalin E (2011) Desensitization protocols and their outcome. Clin J Am Soc Nephrol 6:922–936
Zachary AA, Leffell MS (2014) Desensitization for solid organ and hematopoietic stem cell transplantation. Immunol Rev 258:183–207
Loupy A, Lefaucheur C (2018) Antibody-mediated rejection of solid-organ allografts. N Engl J Med 379:1150–1160
Nakamura T, Shirouzu T (2021) Antibody-mediated rejection and recurrent primary disease: two main obstacles in abdominal kidney, liver, and pancreas transplants. J Clin Med. 2021;10(22):5417.
Schinstock CA, Mannon RB, Budde K, Chong AS, Haas M, Knechtle S, Lefaucheur C, Montgomery RA, Nickerson P, Tullius SG, Ahn C, Askar M, Crespo M, Chadban SJ, Feng S, Jordan SC, Man K, Mengel M, Morris RE, O’Doherty I, Ozdemir BH, Seron D, Tambur AR, Tanabe K, Taupin JL, O’Connell PJ (2020) Recommended treatment for antibody-mediated rejection after kidney transplantation: The 2019 Expert Consensus From the Transplantion Society Working Group. Transplantation 104:911–922
Jodele S, Laskin BL, Goebel J, Khoury JC, Pinkard SL, Carey PM, Davies SM (2013) Does early initiation of therapeutic plasma exchange improve outcome in pediatric stem cell transplant-associated thrombotic microangiopathy? Transfusion 53:661–667
Young JA, Pallas CR, Knovich MA (2021) Transplant-associated thrombotic microangiopathy: theoretical considerations and a practical approach to an unrefined diagnosis. Bone Marrow Transplant 56:1805–1817
Lanaret C, Anglicheau D, Audard V, Buchler M, Caillard S, Couzi L, Malvezzi P, Mesnard L, Bertrand D, Martinez F, Pernin V, Ducloux D, Poulain C, Thierry A, Del Bello A, Rerolle JP, Greze C, Uro-Coste C, Aniort J, Lambert C, Bouvier N, Schvartz B, Maillard N, Sayegh J, Oniszczuk J, Morin MP, Legendre C, Kamar N, Heng AE, Garrouste C (2021) Rituximab for recurrence of primary focal segmental glomerulosclerosis after kidney transplantation: results of a nationwide study. Am J Transplant 21:3021–3033
Uffing A, Perez-Saez MJ, Mazzali M, Manfro RC, Bauer AC, de Sottomaior DF, O’Shaughnessy MM, Cheng XS, Chin KK, Ventura CG, Agena F, David-Neto E, Mansur JB, Kirsztajn GM, Tedesco-Silva H Jr, Neto GMV, Arias-Cabrales C, Buxeda A, Bugnazet M, Jouve T, Malvezzi P, Akalin E, Alani O, Agrawal N, La Manna G, Comai G, Bini C, Muhsin SA, Riella MC, Hokazono SR, Farouk SS, Haverly M, Mothi SS, Berger SP, Cravedi P, Riella LV (2020) Recurrence of FSGS after kidney transplantation in adults. Clin J Am Soc Nephrol 15:247–256
Stahl K, Seeliger B, David S, Schmidt J (2020) What is evidence-based in the treatment of sepsis? Internist (Berl) 61:1238–1248
Acknowledgements
We highly appreciate the ongoing support from Elie Azoulay and Philipp Bauer.
Funding
This research was not supported by any funding.
Author information
Authors and Affiliations
Consortia
Contributions
SD, LR, PC, AvdL, LZ, TP, NN, EM, BLF, JTK, LM, AB, JC, CR, MO and NJ have been actively involved in the modified Delphi process to generate a list of 16 research questions and to the appropriate ranking. Question 1 was worked out by LR, TP, PC, CR, BF, SD, NJ and MK. Question 2 was worked out by JC, AvdL, NN, and BF. Question 3 was worked out by JC, AvdL, NN, EM and JTK. Question 4 was worked out by LR, TP, PC, MO, LZ, EM, JTK and LM. Question 5 was worked out by NN, CR, SD, LZ, NJ, LM and MK. MK and SD prepared Tables and Figures. The final manuscript was prepared from individual packages from the 5 groups by SD and NJ and was then proof-read by all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
SD has received research support and lecture honoraria from Terumo Blodd and Cell Technology, Octapharms and Bayer. JC received research funding from Cerus, Kawasumi Laboratories, Sanofi, Janssen, Incyte, and Sobi; he also received speaker or advisory fees from Cerus, Fresenius Kabi, Grifols, Macopharma, Pharm-Olam, Sanofi, and Terumo Blood and Cell Technologies. ACB received support from Octapharma for attending a meeting. PC has received honoraria for scientific collaboration with Pfizer, MSD and Gilead, and has participated in Advisory Boards for Alexion, Janssen and Gilead.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
. Expert panel composition. Table S2. ASFA recommendations for explorative indicationsadopted from Schwartz et al. [76].
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
David, S., Russell, L., Castro, P. et al. Research priorities for therapeutic plasma exchange in critically ill patients. ICMx 11, 26 (2023). https://doi.org/10.1186/s40635-023-00510-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-023-00510-w