Abstract
Background
Low hemoglobin concentration (Hb) and low mean arterial blood pressure (MAP) impact outcomes in critically ill patients. We utilized an experimental model of “normotensive” vs. “hypotensive” acute hemodilutional anemia to test whether optimal tissue perfusion is dependent on both Hb and MAP during acute blood loss and fluid resuscitation, and to assess the value of direct measurements of the partial pressure of oxygen in tissue (PtO2).
Methods
Twenty-nine anesthetized rats underwent 40% isovolemic hemodilution (1:1) (or sham-hemodilution control, n = 4) with either hydroxyethyl starch (HES) (n = 14, normotensive anemia) or saline (n = 11, hypotensive anemia) to reach a target Hb value near 70 g/L. The partial pressure of oxygen in the brain and skeletal muscle tissue (PtO2) were measured by phosphorescence quenching of oxygen using G4 Oxyphor. Mean arterial pressure (MAP), heart rate, temperature, arterial and venous co-oximetry, blood gases, and lactate were assessed at baseline and for 60 min after hemodilution. Cardiac output (CO) was measured at baseline and immediately after hemodilution. Data were analyzed by repeated measures two-way ANOVA.
Results
Following “normotensive” hemodilution with HES, Hb was reduced to 66 ± 6 g/L, CO increased (p < 0.05), and MAP was maintained. These conditions resulted in a reduction in brain PtO2 (22.1 ± 5.6 mmHg to 17.5 ± 4.4 mmHg, p < 0.05), unchanged muscle PO2, and an increase in venous oxygen extraction. Following “hypotensive” hemodilution with saline, Hb was reduced to 79 ± 5 g/L and both CO and MAP were decreased (P < 0.05). These conditions resulted in a more severe reduction in brain PtO2 (23.2 ± 8.2 to 10.7 ± 3.6 mmHg (p < 0.05), a reduction in muscle PtO2 (44.5 ± 11.0 to 19.9 ± 12.4 mmHg, p < 0.05), a further increase in venous oxygen extraction, and a threefold increase in systemic lactate levels (p < 0.05).
Conclusions
Acute normotensive anemia (HES hemodilution) was associated with a subtle decrease in brain tissue PtO2 without clear evidence of global tissue hypoperfusion. By contrast, acute hypotensive anemia (saline hemodilution) resulted in a profound decrease in both brain and muscle tissue PtO2 and evidence of inadequate global perfusion (lactic acidosis). These data emphasize the importance of maintaining CO and MAP to ensure adequacy of vital organ oxygen delivery during acute anemia. Improved methods of assessing PtO2 may provide an earlier warning signal of vital organ hypoperfusion.
Similar content being viewed by others
Background
The optimal care of critically ill patients often involves management of multiple risk factors for inadequate organ perfusion, including hypotension and anemia. Assessment of the impact of hypotension and anemia in the perioperative period demonstrates that both factors are associated with serious adverse outcomes. Interoperative hypotension has been associated with increased brain [1, 2], heart [3–5], and kidney injury [3, 6, 7] and mortality [8–10]. These outcomes often depend on the magnitude and duration of hypotension; for example, a 40% drop in mean arterial pressure (MAP) from baseline for more than 30 min has been associated with myocardial injury [5]. Perioperative and acute interoperative anemia have also been associated with similar patterns of adverse events; including evidence of brain [11, 12], heart [13, 14], and kidney injury [15, 16] and mortality [14, 16–18]. Experimental models of acute anemia suggest that inadequate microcirculatory perfusion and tissue hypoxia contribute as a mechanism of vital organ injury and mortality [19–21].
Additionally, current clinical practice often favors a restrictive fluid therapy and red blood cell (RBC) transfusion approaches in surgical and critically ill patients. While many of the completed prospective randomized clinical trials favor the non-inferiority of a restrictive transfusion threshold near a hemoglobin concentration (Hb) of 70–80 g/L [22–24], more recent analysis of these data suggest that low Hb levels in the restrictive arms of these studies may be associated with increased organ injury and mortality in specific patient populations [25, 26].
We performed an experimental study to measure the partial pressure of oxygen in tissue (PtO2) in the brain and skeletal muscle, and other parameters of systemic perfusion, under conditions of acute normotensive vs. hypotensive hemodilutional anemia to assess the combined impact of acute anemia and hypotension on tissue perfusion. We hypothesize that optimal tissue perfusion depends on multiple interactive physiological parameters, including Hb and blood pressure, during acute blood loss and fluid resuscitation.
Methods
Overview and preparation
The Animal Care and Use Committee at St. Michael’s hospital approved all animal protocols. Twenty-nine male Sprague-Dawley rats (Jackson laboratory) with a mean weight near 500 g were anesthetized with isoflurane 2–3% in 21% oxygen for the duration of the experiment. The trachea was intubated and the lungs were mechanically ventilated using a pressure controlled ventilator, with peak inspiratory pressure between 15 and 17 cm H2O and a respiratory rate between 60 and 70 breaths per minute and no additional PEEP, to a target partial pressure of arterial carbon dioxide (PaCO2) near 40 mmHg (Kent Scientific Corp., Torrington, CT 06790).
The tail artery and vein were cannulated to perform the hemodilution and to monitor MAP, arterial blood gases, and Hb by co-oximetry. A jugular venous catheter was inserted in a retrograde manner toward the right atrium to provide measurements of venous blood gases. Ventilation was monitored by arterial blood gases to maintain normoxia and normocapnia. Blood pressure, ECG, and body temperature were measured using a computerized data-acquisition system (PowerLab, ADInstruments Inc., Colorado Springs CO 80906). Rectal temperature was maintained between 35 and 36 °C using a heating plate. The partial pressure of oxygen in the tissue (brain, skeletal muscle) or PtO2 was measured using oxygen-dependent quenching of phosphorescence as previously described [27] utilizing a novel microsensor G4 Oxyphor technology (PMOD1000 instrument, Oxygen Enterprises, Ltd., Philadelphia, PA 19104–1808).
Hemodilution protocol
After performing all of the procedures, baseline measurements were collected for 10 min. Rats then underwent either “normotensive” hemodilution with 1:1 volume exchange of 40% estimated total blood volume (30 ml/kg) with either 6% hydroxyethyl starch (HES) 130/0.4 in 0.9% sodium chloride (Voluven, n = 14, Fresenius Kabi Canada, Mississauga ON L4W 4Y3), or “hypotensive” hemodilution with 0.9% sodium chloride (saline, n = 11). During hemodilution, arterial blood was exchanged with HES or saline at a fixed rate over 10 min, using the push-pull infusion pump (PHD2000, Harvard Apparatus Canada, St. Laurent, Quebec, H4S 1R9). Following hemodilution, physiologic parameters were continuously acquired during a 60-min recovery period. Brain and hind limb skeletal muscle tissue PtO2 were recorded continuously. Arterial and venous blood gases and co-oximetry measurements were collected at baseline, immediately following hemodilution, and at 30 and 60 min following completion of hemodilution using a heparinized syringe. Samples were analyzed using a blood gas analyzer and co-oximeter (ABL 800, Radiometer Canada, London ON, N5V 4T7).
An additional four rats were placed in a sham control group and did not undergo hemodilution, to serve as a time-based negative control group.
Cardiac output measurements
These experiments included four rats per hemodilution group, which underwent cardiac output (CO) measurements before and after hemodilution. Transthoracic echocardiography was performed in hemodiluted rats in the supine position at baseline and within 15 to 30 min following hemodilution utilizing a high-frequency ultrasound system (Vevo 2100, MS-250 transducer, Visualsonics, Toronto, ON). Two dimensional long-axis images of the left ventricle in parasternal long- and short-axis views with M-mode measurements at mid-papillary muscle level and linear dimensions were analyzed offline (Vevo 2100 software v. 1.3) using the standard leading edge to leading edge technique. CO was calculated as SV × HR, where SV and HR are stroke volume and heart rate, respectively. SV and ejection fraction (EF) were measured using the Teicholz cubed formula, LV volume = 7 × LVID3/(2.4 + LVID), followed by the difference between ESV and EDV, where LVID, ESV, and EDV are left ventricular internal diameter, end systolic volume, and end diastolic volume, respectively. Fractional shortening (FS%) was calculated as (LVIDd − LVIDs)/LVIDd × 100, where LVIDd and LVIDs are left ventricular end diastolic and end systolic internal diameters, respectively. Three consecutive cardiac cycles were averaged for all analyses.
Statistical analysis
All data are presented as mean ± SD. Data were analyzed by repeated measures two-way ANOVA and post hoc Tukey test, where appropriate according to Sigmaplot software (SigmaStat 11.0).
Results
Baseline values were comparable for all parameters measured between the three experimental and control groups. No differences in heart rate (299.0 ± 29.5, 309.7 ± 51.8, 290.5 ± 3.2 bpm) or body temperature (36.1 ± 0.5, 36.0 ± 0.4, 35.9 ± 0.3 °C) were observed at baseline or at any time point for the HES, saline, and sham control groups, respectively. Arterial and venous blood gases and Hb concentrations are reported in Tables 1 and 2.
Arterial and venous co-oximetry and blood gas analysis
In the normotensive hemodilution (HES) group, mean Hb values decreased from a baseline of 131 ± 9 to 66 ± 6 g/L immediately following hemodilution (p < 0.001). In the hypotensive hemodilution saline group, Hb decreased from 130 ± 11 to 79 ± 5 g/L (Table 1; p < 0.001). The Hb concentration in the saline hemodilution group was initially higher than in the HES hemodilution group (Table 1). In the sham control rats, Hb did not decrease over time.
Arterial oxygen tension (PaO2) and Hb saturation remained stable and did not decrease throughout the experimental protocol in any group (Tables 1 and 2, Fig. 1). Venous oxygen tension (PvO2) and saturation decreased from baseline after 60 min in all groups. There was no difference between PvO2 between the sham controls and the HES hemodilution group. By contrast, there was a more profound decrease in PvO2 and saturation in the saline hemodiluted group (Tables 1 and 2, Fig. 1, p < 0.05). Following saline hemodilution, the PaO2 was increased transiently at 30 min following hemodilution. This change was associated with a reduction in PaCO2 (Table 2; p < 0.001), which is consistent with a respiratory compensation to metabolic acidosis. Animals in this group developed a lactic acidosis, as indicated by a significant increase in lactate, a reduction in pH, and HCO3 − (Table 2, Fig. 1, p < 0.001 for all). A maximal rise in arterial lactate was achieved by 60 min following hemodilution (3.5 ± 1.3 to 10.9 ± 6.2 mmol/L, p < 0.05).
Upper panel Arterial PO2 remained stable except for a transient increase at 30 min (associated with hyperventilation) in the saline hemodilution group. A significant reduction in venous PO2 was observed in the saline hemodilution group relative to the controls (*p < 0.001 vs. baseline, #p < 0.05 vs. control). Middle panel Arterial oxygen saturation remained stable in all groups. A significant reduction in venous PO2 was observed in all groups relative to baseline. The venous oxygen saturation in the saline hemodilution group was reduced relative to the controls and HES group (*p < 0.001 vs. baseline, #p < 0.05 vs. control and HES). Lower panel A significant rise in arterial lactate was only observed in the saline hemodilution group (*p < 0.001 vs. baseline, #p < 0.05 vs. control and HES)
Mean arterial blood pressure measurements
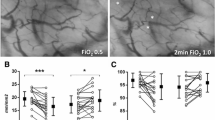
There was a significant treatment, time, and interaction effect (two-way ANOVA; p < 0.001 for all). MAP was maintained for the duration of the 60-min recovery period in both the normotensive hemodilution and control group (Fig. 2). By contrast, there was an immediate decrease in MAP following hemodilution in the saline hemodilution group (77.3 ± 4.0 vs. 42.8 ± 5.2 mmHg, p < 0.05), which persisted to the 60-min recovery period (31.1 ± 12.8 mmHg). MAP was significantly lower in the saline hemodilution group, relative to both controls and starch hemodilution groups at all post-hemodilution time points (Fig. 2, p < 0.001).
Upper panel Mean arterial pressure remained stable in controls and after hemodilution with hydroxyethyl starch (HES) but decreased significantly, relative to controls and HES hemodilution groups, following hemodilution with saline (*p < 0.001 vs. baseline, #p < 0.05 vs. control and HES). Middle panel Brain PO2 decreased from baseline following hemodilution with both HES and saline (*p < 0.001 vs. baseline). Lower panel Skeletal muscle PO2 remained stable in control and HES hemodilution groups but was reduced relative to baseline and controls after saline hemodilution (*p < 0.001 vs. baseline, #p < 0.05 vs. control and HES)
Partial pressure of oxygen in brain and muscle tissue (PtO2)
There was a significant time and interaction effect for brain PtO2 when comparing all three experimental groups (two-way ANOVA; p < 0.001 for both). Brain PtO2 remained stable in the time-based control sham hemodiluted group. Following normotensive hemodilution with HES, brain PtO was reduced from a baseline value of 22.1 ± 5.6 mmHg to a value of 15.6 ± 6.5 mmHg immediately following hemodilution. The brain PtO2 remained decreased for 60 min reaching a value of 17.5 ± 4.4 mmHg (Fig. 2, p < 0.05). Rats undergoing hypotensive hemodilution with saline experienced a greater decrease in brain PtO2 which decreased from baseline (23.2 ± 8.2 mmHg) to values as low as 16.0 ± 4.5 mmHg immediately following hemodilution. The brain PtO2 reached a nadir value of 10.7 ± 3.6 mmHg after 60 min (Fig. 2, p < 0.05).
There was no time or interaction effect observed for hind limb skeletal muscle PO2 (p = 0.051 and 0.082, respectively). However, there was a significant time-treatment interaction (two-way ANOVA; p < 0.001). No change in muscle PtO2 was observed following sham procedure or HES hemodilution (Fig. 2). By contrast, muscle PO2 decreased significantly from baseline values of 44.5 ± 11.0 mmHg to 30.6 ± 10.6 mmHg immediately following hemodilution with saline (Fig. 2, p < 0.05). In this group, muscle PtO2 reached a nadir at 60 min (19.9 ± 12.4 mmHg, p < 0.05).
Cardiac output measurements
CO data from normotensive and hypotensive hemodilution groups are presented in Table 3. These experiments demonstrate that CO is increased in the normotensive HES hemodilution group, predominantly due to an increase in diastolic volume and stroke volume. These changes were not observed in the hypotensive saline hemodilution group which demonstrated a decrease in CO, SV, and diastolic volume (Table 3).
Discussion
We demonstrated a significant interaction between low Hb concentration and low MAP with respect to limiting tissue oxygen delivery in brain and muscle, in a model of normotensive vs. hypotensive hemodilution. During normotensive hemodilution with HES, blood pressure was maintained, CO increased, and systemic perfusion was generally preserved, as indicated by the absence of lactic acidosis and sustained muscle PtO2. However, under these conditions, brain tissue PtO2 was significantly reduced, suggesting that tissue oxygen delivery did not meet the higher metabolic requirements for oxygen in the brain. These data are consistent with our previous studies, which demonstrate that acute normotensive anemia is associated with brain tissue hypoxia and activation of hypoxic cellular signaling pathways, including hypoxia inducible factor (HIF) [20]. This data may help to explain why acute hemodilution and anemia are associated with increased stroke incidence in patients undergoing cardiac and non-cardiac surgery [11, 12]. In addition, acute anemic conditions which produce mild brain tissue hypoxia have been associated with evidence of more severe renal tissue hypoxia [21, 28]; providing a plausible explanation for both stroke acute kidney injury (AKI) in patient exposed to hemodilutional anemia [12, 16]. The combined effect of inadequate perfusion to vital organs during acute anemia may contribute to the observed association of increased mortality in anemic perioperative patients [16, 17].
By contrast, hemodilution with saline resulted in hypotension, a reduction in CO, a further reduction in brain PtO2, a newly observed reduction in muscle PtO2, and a severe increase in lactate suggestive of profound systemic ischemia. These data demonstrate the additive impact of combined low Hb in the face of a low CO and low MAP on tissue oxygen delivery in an experimental model. The mechanism likely involves inadequate fluid resuscitation with reduced intravascular volume and an inadequate cardiovascular response to anemia as indicated by the CO and diastolic volume analysis. From prior studies, we understand that during acute anemia, oxygen homeostasis is maintained by an active increase in CO to ensure perfusion of vital organs including the brain [19, 20]. Inhibition of the CO response results in accentuation of tissue hypoxia [19]. We observed a similar effect in the saline hemodilution group where an inadequate CO response to anemia resulted in profound tissue hypoxia further demonstrating the need to preserve adequate intravascular fluid volume during anemia.
Can measurement of tissue PO2 inform clinical practice to improve outcomes?
Clinical monitoring of the partial pressure of oxygen in brain tissue has been performed directly using invasive tissue probes in patients exposed to neurotrauma; however, the invasive nature of these probes severely limits their use clinically. Indirect assessment of brain PtO2 has been achieved utilizing near infrared spectroscopy (NIRS). NIRS measures changes in arterial and venous oxy- and deoxyhemoglobin levels which indirectly reflect levels of microvascular oxygenation. NIRS is capable of detecting cerebral microvascular oxygen desaturation in patients undergoing heart surgery [6, 29–31]. Treatment algorithms have been defined to respond to, and correct, episodes of cerebral desaturation [29, 31]. While these maneuvers are able to correct the observed cerebral desaturations, only one study has demonstrated improvement in patient outcome [31].
Other novel light-based methods for directly measuring cellular energetics and tissue PO2 are being developed. Spectroscopic approaches, including broadband spectroscopy, allowed for measurement of the oxidative state of cellular cytochromes which reflect cellular energetics [32, 33]. Measurement of cutaneous mitochondrial PO2, utilizing the oxygen-dependent delayed fluorescence of protopor-phyrin IX in the skin [34, 35], has been used to assess the mitochondrial PO2 response to acute hemodilution in an experimental pig model [35]. This approach was able to detect tissue hypoxia at an earlier stage of hemodilution relative to more traditional measurements including changes in MAP, serum lactate, VO2, and NIRS [35]. Future studies will be required to assess the impact of these technologies on patient outcomes.
In clinical studies, both hypotension [1–10] and anemia [11–18] have been independently associated with increase acute renal injury [3, 6, 7, 15, 16], myocardial infarction [3–5, 13, 14], stroke [1, 2, 11, 12], and mortality [8–10, 14, 16–18]. However, few of these retrospective analyses have formally assessed the combined impact of low Hb and low MAP on patient outcome. A 2012 post hoc analysis by Haase et al. demonstrated a 3.36 (1.34–8.41)-fold increase in cardiac surgery risk of AKI associated with a combination of anemia and hypotension during CPB relative to anemia alone [36]. However, a retrospective study by Sickeler et al. in 2014, which intended to replicate Haase’s findings, involved a much larger cohort of 3963 patients and did not find any association between the co-occurrence of hypotension and anemia in cardiac surgery-related AKI risk [37]. Further clinical research is needed to fully assess the potential interaction between anemia and hypotension and their combined impact on patient outcome.
Optimal choice of resuscitation fluid in critical care
Data to support the choice of optimal fluid for resuscitation (blood, colloid, crystalloid, blood substitute) in specific critical care settings is lacking [38]. While a complete review is beyond the scope of this manuscript, our data support some interesting observations about fluid restriction and the potential value of monitoring tissue PtO2 to assess fluid replacement and transfusion strategies. Recent assessment of clinical practice favors goal-directed and/or restrictive fluid management strategies [39]. In addition, review of management strategies in critical care demonstrate a preference toward crystalloid as the first choice for fluid therapy [40] and an overall increase in vasopressor use [41]. This combination of treatment strategies may lead to an increased risk of patients with reduced intravascular volume and support the priority of increased utilization of monitors which assess the adequacy of microvascular perfusion of vital organs [42].
Data from prospective randomized trials assessing restrictive vs. liberal RBC transfusion thresholds have largely favored a restrictive approach [43]. More recent analysis suggest that some patient populations may be harmed by this restrictive approach including patients undergoing cardiac surgery [44, 45] or those experiencing acute myocardial ischemia [25]. Data from the TITRe2 trial demonstrated that patients randomized to a restrictive transfusion threshold (Hb <7.5 g/dL) experienced a higher mortality [(4.2 vs. 2.6%; HR 1.64 (1.00 to 2.679)], relative to patients randomized to a liberal threshold [44]. Early data from the TRICS trial in cardiac surgery also demonstrated a trend to increased adverse events including stroke (3 vs. 0) and death (4 vs. 1) in the restrictive study arm [46]. Utilization of methods to directly assess tissue oxygen delivery may help to define appropriate patient-specific fluid therapy and RBC transfusion thresholds in different patient populations. Finally, direct measurement of tissue oxygen delivery may promote the development of novel blood substitutes, including hemoglobin-based oxygen carriers (HBOCs). In experimental models, HBOCs have been demonstrated to maintain oxygen delivery to tissue during severe degrees of volume exchange [47]. However, due to concerns about toxicity and adverse clinical outcomes associated with HBOC use [48], future development of HBOCs will require measures of both efficacy (PtO2) and safety.
There are several limitations to the current study. We did not provide a whole blood exchange control, as these controls had been performed previously without any effect on tissue oxygen measurements relative to time-based controls [49]. We did not directly assess changes in intravascular volume. Further, although crystalloids and colloids are used clinically, they are typically not used comparably in a direct 1:1 blood volume exchange. Thus, our saline hemodilution group likely resulted in additional hemodynamic stress, including reduced intravascular volume that is not reflective of clinical care.
Conclusions
In this study, we observed that hypotensive anemia (1:1 saline/blood fluid exchange) resulted in global ischemia and severe tissue hypoxia. By contrast, normotensive anemia (1:1 HES/blood fluid exchange) preserved global organ perfusion but was unable to prevent a subtle reduction in brain tissue PtO2. These data support the ongoing assessment of clinically applicable technologies to assess and measure tissue PtO2, in order to develop strategies maintaining tissue oxygen delivery and limiting adverse events associated with tissue hypoxia in patients with critical illness.
Abbreviations
- Hb:
-
Hemoglobin
- HES:
-
Hydroxyethyl starch
- MAP:
-
Mean arterial pressure
- PCO2 :
-
Partial pressure of carbon dioxide
- PO2 :
-
Partial pressure of oxygen
References
Bijker JB, Persoon S, Peelen LM, Moons KG, Kalkman CJ, Kappelle LJ, van Klei WA (2012) Intraoperative hypotension and perioperative ischemic stroke after general surgery: a nested case-control study. Anesthesiology 116(3):658–664
Group PS, Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC, Xavier D, Chrolavicius S, Greenspan L et al (2008) Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet 371(9627):1839–1847
Walsh M, Devereaux PJ, Garg AX, Kurz A, Turan A, Rodseth RN, Cywinski J, Thabane L, Sessler DI (2013) Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology 119(3):507–515
Devereaux PJ, Sessler DI, Leslie K, Kurz A, Mrkobrada M, Alonso-Coello P, Villar JC, Sigamani A, Biccard BM, Meyhoff CS et al (2014) Clonidine in patients undergoing noncardiac surgery. N Engl J Med 370(16):1504–1513
van Waes JA, van Klei WA, Wijeysundera DN, van Wolfswinkel L, Lindsay TF, Beattie WS (2016) Association between intraoperative hypotension and myocardial injury after vascular surgery. Anesthesiology 124(1):35–44
Ono M, Arnaoutakis GJ, Fine DM, Brady K, Easley RB, Zheng Y, Brown C, Katz NM, Grams ME, Hogue CW (2013) Blood pressure excursions below the cerebral autoregulation threshold during cardiac surgery are associated with acute kidney injury. Crit Care Med 41(2):464–471
Sun LY, Wijeysundera DN, Tait GA, Beattie WS (2015) Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology 123(3):515–523
Bijker JB, van Klei WA, Vergouwe Y, Eleveld DJ, van Wolfswinkel L, Moons KG, Kalkman CJ (2009) Intraoperative hypotension and 1-year mortality after noncardiac surgery. Anesthesiology 111(6):1217–1226
Monk TG, Bronsert MR, Henderson WG, Mangione MP, Sum-Ping ST, Bentt DR, Nguyen JD, Richman JS, Meguid RA, Hammermeister KE (2015) Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology 123(2):307–319
Sessler DI, Sigl JC, Kelley SD, Chamoun NG, Manberg PJ, Saager L, Kurz A, Greenwald S (2012) Hospital stay and mortality are increased in patients having a “triple low” of low blood pressure, low bispectral index, and low minimum alveolar concentration of volatile anesthesia. Anesthesiology 116(6):1195–1203
Ashes C, Judelman S, Wijeysundera DN, Tait G, Mazer CD, Hare GM, Beattie WS (2013) Selective beta1-antagonism with bisoprolol is associated with fewer postoperative strokes than atenolol or metoprolol: a single-center cohort study of 44,092 consecutive patients. Anesthesiology 119(4):777–787
Karkouti K, Djaiani G, Borger MA, Beattie WS, Fedorko L, Wijeysundera D, Ivanov J, Karski J (2005) Low hematocrit during cardiopulmonary bypass is associated with increased risk of perioperative stroke in cardiac surgery. Ann Thorac Surg 80(4):1381–1387
Beattie WS, Wijeysundera DN, Karkouti K, McCluskey S, Tait G, Mitsakakis N, Hare GM (2010) Acute surgical anemia influences the cardioprotective effects of beta-blockade: a single-center, propensity-matched cohort study. Anesthesiology 112(1):25–33
Wu WC, Schifftner TL, Henderson WG, Eaton CB, Poses RM, Uttley G, Sharma SC, Vezeridis M, Khuri SF, Friedmann PD (2007) Preoperative hematocrit levels and postoperative outcomes in older patients undergoing noncardiac surgery. JAMA 297(22):2481–2488
Karkouti K, Beattie WS, Wijeysundera DN, Rao V, Chan C, Dattilo KM, Djaiani G, Ivanov J, Karski J, David TE (2005) Hemodilution during cardiopulmonary bypass is an independent risk factor for acute renal failure in adult cardiac surgery. J Thorac Cardiovasc Surg 129(2):391–400
Loor G, Li L, Sabik JF 3rd, Rajeswaran J, Blackstone EH, Koch C (2012) Nadir hematocrit during cardiopulmonary bypass: end-organ dysfunction and mortality. J Thorac Cardiovasc Surg 144(3):654–662.e654
Musallam KM, Tamim HM, Richards T, Spahn DR, Rosendaal FR, Habbal A, Khreiss M, Dahdaleh FS, Khavandi K, Sfeir PM et al (2011) Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet 378(9800):1396–1407
Carson JL, Poses RM, Spence RK, Bonavita G (1988) Severity of anaemia and operative mortality and morbidity. Lancet 1(8588):727–729
Hu T, Beattie WS, Mazer CD, Leong-Poi H, Fujii H, Wilson DF, Tsui AK, Liu E, Muhammad M, Baker AJ et al (2013) Treatment with a highly selective beta(1) antagonist causes dose-dependent impairment of cerebral perfusion after hemodilution in rats. Anesth Analg 116(3):649–662
Tsui AK, Marsden PA, Mazer CD, Adamson SL, Henkelman RM, Ho JJ, Wilson DF, Heximer SP, Connelly KA, Bolz SS et al (2011) Priming of hypoxia-inducible factor by neuronal nitric oxide synthase is essential for adaptive responses to severe anemia. Proc Natl Acad Sci U S A 108(42):17544–17549
Tsui AK, Marsden PA, Mazer CD, Sled JG, Lee KM, Henkelman RM, Cahill LS, Zhou YQ, Chan N, Liu E et al (2014) Differential HIF and NOS responses to acute anemia: defining organ-specific hemoglobin thresholds for tissue hypoxia. Am J Physiol Regul Integr Comp Physiol 307(1):R13–R25
Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, Nemo G, Dragert K, Beaupre L, Hildebrand K et al (2011) Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med 365(26):2453–2462
Hajjar LA, Vincent JL, Galas FR, Nakamura RE, Silva CM, Santos MH, Fukushima J, Kalil Filho R, Sierra DB, Lopes NH et al (2010) Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA 304(14):1559–1567
Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 340(6):409–417
Carson JL, Brooks MM, Abbott JD, Chaitman B, Kelsey SF, Triulzi DJ, Srinivas V, Menegus MA, Marroquin OC, Rao SV et al (2013) Liberal versus restrictive transfusion thresholds for patients with symptomatic coronary artery disease. Am Heart J 165(6):964–971.e961
Hovaguimian F, Myles PS (2016) Restrictive versus liberal transfusion strategy in the perioperative and acute care settings: a context-specific systematic review and meta-analysis of randomized controlled trials. Anesthesiology 125(1):46–61
Yu J, Ramadeen A, Tsui AK, Hu X, Zou L, Wilson DF, Esipova TV, Vinogradov SA, Leong-Poi H, Zamiri N et al (2013) Quantitative assessment of brain microvascular and tissue oxygenation during cardiac arrest and resuscitation in pigs. Anaesthesia 68(7):723–735
van Bommel J, Siegemund M, Henny C, Ince C (2008) Heart, kidney, and intestine have different tolerances for anemia. Transl Res 151(2):110–117
Deschamps A, Hall R, Grocott H, Mazer CD, Choi PT, Turgeon AF, de Medicis E, Bussieres JS, Hudson C, Syed S et al (2016) Cerebral oximetry monitoring to maintain normal cerebral oxygen saturation during high-risk cardiac surgery: a randomized controlled feasibility trial. Anesthesiology 124(4):826–836
Subramanian B, Nyman C, Fritock M, Klinger RY, Sniecinski R, Roman P, Huffmyer J, Parish M, Yenokyan G, Hogue CW (2016) A multicenter pilot study assessing regional cerebral oxygen desaturation frequency during cardiopulmonary bypass and responsiveness to an intervention algorithm. Anesth Analg 122(6):1786–1793
Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I, Cleland A, Schaefer B, Irwin B, Fox S (2007) Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg 104(1):51–58
Kolyva C, Ghosh A, Tachtsidis I, Highton D, Smith M, Elwell CE (2013) Dependence on NIRS source-detector spacing of cytochrome c oxidase response to hypoxia and hypercapnia in the adult brain. Adv Exp Med Biol 789:353–359
Yeganeh HZ, Toronov V, Elliott JT, Diop M, Lee TY, St Lawrence K (2012) Broadband continuous-wave technique to measure baseline values and changes in the tissue chromophore concentrations. Biomed Opt Express 3(11):2761–2770
Harms F, Stolker RJ, Mik E (2016) Cutaneous respirometry as novel technique to monitor mitochondrial function: a feasibility study in healthy volunteers. PLoS One 11(7):e0159544
Romers LH, Bakker C, Dollee N, Hoeks SE, Lima A, Raat NJ, Johannes T, Stolker RJ, Mik EG (2016) Cutaneous mitochondrial PO2, but not tissue oxygen saturation, is an early indicator of the physiologic limit of hemodilution in the Pig. Anesthesiology 125(1):124–132
Haase M, Bellomo R, Story D, Letis A, Klemz K, Matalanis G, Seevanayagam S, Dragun D, Seeliger E, Mertens PR et al (2012) Effect of mean arterial pressure, haemoglobin and blood transfusion during cardiopulmonary bypass on post-operative acute kidney injury. Nephrol Dial Transplant 27(1):153–160
Sickeler R, Phillips-Bute B, Kertai MD, Schroder J, Mathew JP, Swaminathan M, Stafford-Smith M (2014) The risk of acute kidney injury with co-occurrence of anemia and hypotension during cardiopulmonary bypass relative to anemia alone. Ann Thorac Surg 97(3):865–871
Orbegozo Cortes D, Gamarano Barros T, Njimi H, Vincent JL (2015) Crystalloids versus colloids: exploring differences in fluid requirements by systematic review and meta-regression. Anesth Analg 120(2):389–402
Corcoran T, Rhodes JE, Clarke S, Myles PS, Ho KM (2012) Perioperative fluid management strategies in major surgery: a stratified meta-analysis. Anesth Analg 114(3):640–651
Miller TE, Bunke M, Nisbet P, Brudney CS (2016) Fluid resuscitation practice patterns in intensive care units of the USA: a cross-sectional survey of critical care physicians. Perioper Med (London) 5:15
Thongprayoon C, Cheungpasitporn W, Harrison AM, Carrera P, Srivali N, Kittamongkolchai W, Erdogan A, Kashani KB (2016) Temporal trends in the utilization of vasopressors in intensive care units: an epidemiologic study. BMC Pharmacol Toxicol 17(1):19
Mayer K, Trzeciak S, Puri NK (2016) Assessment of the adequacy of oxygen delivery. Curr Opin Crit Care 22(5):437–443
Carson JL, Carless PA, Hebert PC (2013) Outcomes using lower vs higher hemoglobin thresholds for red blood cell transfusion. JAMA 309(1):83–84
Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA, Angelini GD, Reeves BC (2015) Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 372(11):997–1008
Docherty AB, O'Donnell R, Brunskill S, Trivella M, Doree C, Holst L, Parker M, Gregersen M, Pinheiro de Almeida J, Walsh TS et al (2016) Effect of restrictive versus liberal transfusion strategies on outcomes in patients with cardiovascular disease in a non-cardiac surgery setting: systematic review and meta-analysis. BMJ 352:i1351
Shehata N, Burns LA, Nathan H, Hebert P, Hare GM, Fergusson D, Mazer CD (2012) A randomized controlled pilot study of adherence to transfusion strategies in cardiac surgery. Transfusion 52(1):91–99
Hare GM, Liu E, Baker AJ, Mazer CD (2009) Effect of oxygen affinity on systemic perfusion and brain tissue oxygen tension after extreme hemodilution with hemoglobin-starch conjugates in rats. Intensive Care Med 35(11):1925–1933
Natanson C, Kern SJ, Lurie P, Banks SM, Wolfe SM (2008) Cell-free hemoglobin-based blood substitutes and risk of myocardial infarction and death: a meta-analysis. JAMA 299(19):2304–2312
McLaren AT, Marsden PA, Mazer CD, Baker AJ, Stewart DJ, Tsui AK, Li X, Yucel Y, Robb M, Boyd SR et al (2007) Increased expression of HIF-1alpha, nNOS, and VEGF in the cerebral cortex of anemic rats. Am J Physiol Regul Integr Comp Physiol 292(1):R403–R414
Funding
This study was supported by the Children’s Discovery Institute and St. Michael’s Hospital AHSC AFP Innovation Fund. Dr. Hare and Dr. Mazer are supported by University of Toronto, Department of Anesthesia Merit Awards.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional files.
Authors’ contributions
GMTH, CDM, AD, SR, DFW, and AKYT conceptualized the study and designed the protocol. AKYT, NM, TK, EL, and JFD performed the experiments. GMTH, CDM, TK, NM, and AKYT analyzed the data and performed the statistical analysis. GMTH, CDM, AD, TK, NM, SR, DFW, and KC wrote and edited the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval
All animal protocols were approved by the Animal Care and Use Committee at St. Michael’s Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kei, T., Mistry, N., Tsui, A.K.Y. et al. Experimental assessment of oxygen homeostasis during acute hemodilution: the integrated role of hemoglobin concentration and blood pressure. ICMx 5, 12 (2017). https://doi.org/10.1186/s40635-017-0125-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-017-0125-6