Abstract
Purpose
To develop a standardized scoring system to evaluate pre- to post-operative repair or reconstruction of hip cartilage using magnetic resonance imaging (MRI).
Methods
A two-phase modified Delphi study was conducted. Phase 1 involved a survey with suggested criteria and diagrams to define various stages of articular cartilage repair and phase 2 involved an expert consensus meeting that discussed the survey responses and voted on final scoring criteria. The survey was emailed to members of the Canadian Hip Preservation Research Collaborative (CHIPR) and respondents included both board certified orthopedic surgeons as well as musculoskeletal radiologists.
Results
Overall, there were 17 survey respondents from Canada and most (47%, 8/17) participants agreed that the minimum MRI protocol needed to evaluate cartilage repair was a 3.0 T MRI and 94% (17/18) agreed that the minimum time post-operatively that they felt they would be able to accurately evaluate cartilage repair on an MRI was 12 months. Following phases 1 and 2, the final Magnetic Resonance Evaluation of the Repair of Cartilage in the Hip (MERCH) score was developed with 7 domains, 3 criteria per domain: 1) volume fill of cartilage defect, 2) integration into adjacent cartilage, 3) surface of the repair tissue, 4) structure of the repair tissue, 5) bony overgrowth, 6) subchondral changes, and 7) delamination. The score ranges from 60 (optimal) to -20 points (worst/none).
Conclusions
This consensus project established a new MRI scoring system to evaluate post-operative cartilage restoration of the hip. The implementation of the MERCH score is essential in our ability to guide patient management and expectations in a rapidly evolving field and will help with standardizing our evaluation of cartilage repair in future research trials.
Level of Evidence
Level II Diagnostic.
Similar content being viewed by others
Background
Articular cartilage defects of the hip typically do not heal due to the avascularity of cartilage and low proliferative capacity of articular chondrocytes – the producers of the functional extracellular matrix of articular cartilage [2, 14]. Moreover, focal articular cartilage defects, if left without repair, can develop into larger generalized lesions that cause significant pain and dysfunction. Perhaps more importantly, these generalized lesions also have the potential to hasten the early development of osteoarthritis (OA), which is irreversible [4]. While hip replacements are generally safe and effective [11], young adults that have hip replacements are at risk of poorer outcomes and early failure [1]. Currently, there are many options for the repair and reconstruction of cartilage, including chondroplasty, delamination repair, microfracture, autograft and mosaicplasty, osteochondral allografts, and autologous chondrocyte implantation [7, 9, 20].
Given the variation in chondral damage, as well as the repair techniques, broad classification of cartilage status is not very descriptive for identifying patient outcomes and reoperation strategies. The International Cartilage Repair Society (ICRS) classification was developed to classify cartilage status, but is limited to just four categories, ranging from normal to severely abnormal [10]. There are two main scores used for the classification of cartilage status specific to the hip: the Scoring Hip Osteoarthritis with Magnetic Resonance Imaging (MRI) (SHOMRI) and the Hip Osteoarthritis MRI Scoring System (HOAMS) [12, 13, 16, 19]. However, these scoring methods do not evaluate the repair and integration of hip cartilage. The SHOMRI and HOAMS comment on the thickness of the cartilage remaining, but do not provide details on the type of repair and integration that has occurred from pre- to post-operatively. The Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) Score was developed to evaluate cartilage repair, but in the knee [18]. This study has developed the novel Magnetic Resonance Evaluation of the Repair of Cartilage in the Hip (MERCH) Score whose goal is to help with describing patient outcomes and the effectiveness of cartilage repair strategies in hip arthroscopy.
As the only score known to evaluate cartilage repair in a joint using MRI, we aimed to adapt the MOCART score to develop hip-specific criteria to evaluate pre- to post-operative repair and/or reconstruction of hip cartilage with a two-phase modified Delphi study. Given the similar diagnostic accuracy and extensive clinical training amongst the hip arthroscopy community, we hypothesized that there would be a general consensus on MRI criteria defining post-operative repair and/or reconstruction of hip cartilage.
Methods
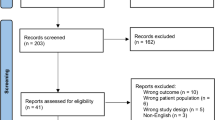
The Hamilton Integrated Research Ethics Board (HiREB) approved the study protocol prior to initiation and all consensus participants provided written informed consent prior to the meeting (#15,021). A two-phase modified Delphi study was conducted involving a Likert/multiple-choice-based survey using diagrams to define various aspects of articular cartilage repair (Phase 1) and an expert consensus meeting that discussed the survey responses and voted on the scoring criteria (Phase 2) (Fig. 1). Throughout both phases of the study process, participants were asked to consider their responses in the context of global application, meaning the minimum MRI protocols and score criteria that could be used to evaluate cartilage repair given the disparities in access to diagnostic technology in low-, middle-, and high-income countries.

(Adapted from Oxford Consensus) [5]
A flow diagram of the modified Delphi process for the MERCH study
Participants
The participants included members of the Canadian Hip Preservation Research Collaborative (CHIPR) who are board certified orthopedic surgeons with expert knowledge in the research and clinical assessment of patients with articular cartilage defects of the hip. Most CHIPR surgeons have a practice that consists of at least 50 hip arthroscopy cases per year in the last 5 years, had fellowship training in hip preservation, and are early to mid-career investigators. The Principal Investigator also identified 2 Canadian musculoskeletal radiologists with similar experience in radiological assessment of the hip and research. The radiologist participants had to have > 80% practice focus and training in musculoskeletal imaging. Participants were invited to participate in both the survey and consensus phases of the study via e-mail. Of these, 17 completed the Phase 1 survey and 18 participated in the Phase 2 consensus meeting.
Phase 1: Survey assessment
Phase 1 of the modified Delphi process utilized a web-based survey that asked about demographic information of the respondents and the 7 proposed sections and criteria therein of the MERCH score. Participants were asked to rank how strongly they agreed with a statement or criteria using a 7-point Likert scale (Appendix 1). Open-ended questions were asked at the end of each section to determine if there were other important considerations for the scoring criteria. Research personnel compiled the responses and used literal text coding to look for commonalities in the open-ended responses and presented a summary to the consensus meeting participants in Phase 2 (Appendix 2). Descriptive measures of central tendency (means, proportions) and level of dispersion (standard deviations, ranges) were calculated for all criteria and presented to the consensus meeting participants.
Phase 2: Consensus meeting
The MERCH scoring criteria was revised based on recommendations provided by the survey respondents and presented at the consensus meeting on January 14, 2023. In some cases, there were conflicting comments in the survey on how to handle specific criteria and consequently, all applicable comments were brought forward to the consensus meeting for discussion by the expert panel. The participants were also given the opportunity to consider revised wording of individual criteria. Following some discussion after reviewing each proposed section of the MERCH score, participants were asked to vote anonymously (using the poll feature of the Zoom virtual platform (Zoom Video Communications Inc., San Jose, CA, USA)) on each carefully worded criterion using a 7-point Likert scale (Appendix 1). Discussions were facilitated by a research staff member not directly involved in deciding the scoring criteria and continued until 80% of respondents agreed on inclusion or exclusion of a given criterion. If the 80% threshold could not be reached after a third round of discussion and voting, the result was to be marked as “no consensus”.
Statistics
All calculations were reported using descriptive statistics, including means, proportions, and standard deviations (performed using SPSS version 28.0.1.0).
Results
Phase 1: Survey assessment
Overall, there were 17 survey respondents who performed a mean of 75 (SD 50.7) hip arthroscopy procedures per year (Table 1). Most respondents had a minimum of 4 years in practice (15/17, 88%), worked in an academic center (14/17, 82%) and were fellowship trained (16/17, 94%). Most participants were orthopedic surgeons (11/17, 65%), with the remaining being pediatric orthopedic surgeons (4/17, 24%) and radiologists (2/17, 12%), all with experience diagnosing and treating cartilage defects in the hip.
Optimal MRI Protocol
Results from the survey demonstrated variability in what surgeons considered an appropriate MRI protocol to evaluate hip cartilage. When asked what they consider to be the minimum MRI protocol needed to evaluate cartilage repair, 47% (8/17) of respondents indicated a 3.0 T MRI and 41% (7/17) indicated a 1.5 T MRI with arthrogram. Some respondents agreed that the coronal plane alone was sufficient to evaluate articular cartilage repair, but most respondents felt that an additional plane should be incorporated into the score (10/17, 59%). However, the precise multi-planar sequence was variable with some suggesting a combined coronal/axial oblique (3/10, 30%), while others did not indicate an optimal plane (5/10, 50%). In terms of time to cartilage integration, most respondents agreed that the earliest timeframe post-operatively to accurately view cartilage repair on MRI was 6–12 months (13/17, 77%). However, there was disagreement regarding the optimal timepoint post-operatively to obtain an MRI with 47% (8/17) of respondents recommending 6–12 months post-operatively and 47% (8/17) recommending 13–18-months.
MERCH Criteria
At the survey phase, the MERCH score was presented with 7 separate domains and 2 to 5 proposed criteria therein, similar to the MOCART score but with criteria relevant to the hip joint: 1) volume fill of cartilage defect, 2) integration into adjacent cartilage, 3) surface of the repair tissue, 4) structure of the repair tissue, 5) signal intensity of the repair tissue, 6) bony defect or bony overgrowth, and 7) subchondral changes (Appendix 2).
Overall, respondents indicated that there was a need to include multiple imaging planes, diagrams that were more “zoomed in” to better see the structural abnormalities being depicted, and more simplified criteria, which were incorporated into the score for evaluation in Phase 2. Refer to Table 2 for further information regarding the initial stage comments and modifications.
Phase 2: Consensus meeting
The original survey presented a more detailed and nuanced scoring system for respondents to evaluate (Appendix 1). Based on comments from the open-ended survey questions and discussion during the Phase 2 meeting, there was a general consensus that the score should be simplified to improve the ease of administration and the accuracy and consistency of the final score. Refer to Table 3 for further information regarding modifications at the consensus meeting.
Following Phase 1 and 2, the final MERCH score was developed with 7 domains, 3 criteria per domain: 1) volume fill of cartilage defect, 2) integration into adjacent cartilage, 3) surface of the repair tissue, 4) structure of the repair tissue, 5) bony overgrowth, 6) subchondral changes, and 7) delamination (Fig. 2). For domains 1 to 4, criteria are scored as 10 (best), 5, and 0 (worst). Where any bony overgrowth has been shown to lead to poor outcomes, domain 5 was scored as 0 (no overgrowth), -5 (some overgrowth), and -10 (complete osseous overgrowth). Subchondral changes and delamination in domains 6 and 7 were scored as 10 (no changes), 0 (presence of edema/delamination), and -5 (presence of a subchondral cyst/delamination at the chondrolabral junction). Therefore, the MERCH score has a highest possible score of 60 points, representing optimal cartilage repair, and a lowest possible score of -20 points, representing the worst possible to no repair. These scores were agreed upon during the consensus meeting based on the severity of the presence or absence of these morphologies in the hip and their impact on cartilage repair.
Participants were also asked about the minimum time post-operatively that they felt they would be able to accurately evaluate cartilage repair on an MRI and 94% (16/17) agreed on 12 months post-operatively.
Discussion
Overall, in keeping with our hypothesis, this modified Delphi study demonstrated a general consensus on MRI criteria defining post-operative repair and/or reconstruction of hip cartilage. This modified Delphi study established standardized MRI criteria to evaluate hip cartilage repair from pre- to post-operatively across 7 domains including: 1) volume fill of cartilage defect, 2) integration into adjacent cartilage, 3) surface of the repair tissue, 4) structure of the repair tissue, 5) bony overgrowth, 6) subchondral changes and 7) delamination. Participants agreed that these criteria should be evaluated at a minimum of 12 months post-operatively using a 3.0 T MRI.
Throughout the process of this Delphi study, there was a general consensus to simplify the criteria used to evaluate hip cartilage repair. Specifically, the domains evaluating volume filling of the cartilage defect, integration into adjacent cartilage and subchondral changes were all simplified from 4 to 5 criteria with multiple descriptors per domain, to 3 criteria with simple descriptors, while the criteria discussing signal intensity of the repair tissue was removed entirely to help ensure the score would be useful to orthopaedic surgeons and researchers globally with varying access to different MRI technology. Further, it has been shown in the orthopaedic field that utilizing a simpler scoring system with clear terminology results in improved inter- and intra-observer agreement, especially when evaluating an MRI [3, 17, 22]. Furthermore, previous studies discussing cartilage repair in the knee support the notion that use of a 3.0 T MRI at a minimum of 12-months post-operatively is optimal to evaluate cartilage repair and integration [8, 21]. Therefore, it is important that the MERCH score be applied at 12 months or more post-operatively.
As discussed above, the main scoring systems that exist to classify cartilage status in the hip include the SHOMRI and HOAMS scores, which were generally created to evaluate OA in the hip [13, 16, 19]. Previous studies evaluating radiographic outcomes after cartilage repair in the hip used very general terms such as “well-incorporated autograft” or “intact cartilage” [6, 15]. The proposed MERCH scoring system will provide both surgeons and radiologists a structured and universal language which can be used to describe repaired cartilage in the hip post-operatively. Addressing this knowledge gap is critical in our ability to guide patient management and expectations especially in a rapidly evolving field that is seeing an increasing amount of cartilage restoration procedures.
This study was strengthened by the multi-phase, Delphi approach involving both expert surgeons and radiologists across the country. The involvement of both surgeons and radiologists adds to the validity of this study as it encompasses all viewpoints and ensures consistency in both understanding and application of the scoring system by bridging the gap between clinician and radiologist.
There were some limitations to this study. Firstly, given that all physicians who participated were located in Canada, this may limit the generalizability of the results worldwide as different centers may have differential access to high-quality MRI or may have different levels of expertise regarding the ability to read MRI scans. Moreover, inherent to any consensus discussion, it is possible that some participants had strong opinions regarding certain topics which may bias the consensus panel’s decision-making in some areas. We attempted to temper this by offering an initial survey evaluation and anonymous voting during the consensus discussion. Finally, there is potential for bias related to the smaller sample size of 17 participants involved as this may result in less robust conclusions, however this is highly unlikely given the high agreement consistently seen throughout the study.
Conclusions
This consensus project established a new MRI scoring system to evaluate post-operative cartilage restoration of the hip. The implementation of the MERCH score is essential in our ability to guide patient management and expectations in a rapidly evolving field and will help with standardizing our evaluation of cartilage repair in future research trials. Future directions include performing a validation study of the proposed scoring system to ensure sufficient agreement is present in its application, which the MERCH Investigators have planned. Ultimately, the MERCH score can be used to standardize the evaluation of cartilage repair and guide research trials when evaluating various cartilage restoration procedures in the hip.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- MERCH:
-
Magnetic Resonance Evaluation of the Repair of Cartilage in the Hip
- OA:
-
Osteoarthritis
- ICRS:
-
International Cartilage Repair Society
- SHOMRI:
-
Scoring Hip Osteoarthritis with Magnetic Resonance Imaging
- HOAMS:
-
Hip Osteoarthritis MRI Scoring System
- MOCART:
-
Magnetic Resonance Observation of Cartilage Repair Tissue
- HiREB:
-
Hamilton Integrated Research Ethics Board
References
Bayliss LE, Culliford D, Monk AP et al (2017) The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet 389(10077):1424–1430. https://doi.org/10.1016/S0140-6736(17)30059-4
Benthien JP, Behrens P (2011) The treatment of chondral and osteochondral defects of the knee with autologous matrix-induced chondrogenesis (AMIC): method description and recent developments. Knee Surg Sports Traumatol Arthrosc 19(8):1316–1319. https://doi.org/10.1007/s00167-010-1356-1
Bettuzzi C, Abati CN, Salvatori G, Zanardi A, Lampasi M (2019) Interobserver reliability of Diméglio and Pirani score and their subcomponents in the evaluation of idiopathic clubfoot in a clinical setting: a need for improved scoring systems. J Child Orthop 13(5):478–485. https://doi.org/10.1302/1863-2548.13.190010
Buckwalter JA, Mankin HJ (1998) Articular cartilage: degeneration and osteoarthritis, repair, regeneration, and transplantation. Instr Course Lect 47:487–504
Dijkstra HP, Mc Auliffe S, Ardern CL et al (2023) Oxford consensus on primary cam morphology and femoroacetabular impingement syndrome: part 1—definitions, terminology, taxonomy and imaging outcomes. Br J Sports Med 57(6):325–341. https://doi.org/10.1136/bjsports-2022-106085
Girard J, Roumazeille T, Sakr M, Migaud H (2011) Osteochondral mosaicplasty of the femoral head. Hip Int 21(5):542–548. https://doi.org/10.5301/HIP.2011.8659
Gordey EE, Wong IH. Cartilage repair in the hip (2018) Annals of Joint 3(3). https://doi.org/10.21037/aoj.2018.03.08
Hayashi D, Li X, Murakami AM, Roemer FW, Trattnig S, Guermazi A (2018) understanding magnetic resonance imaging of knee cartilage repair: a focus on clinical relevance. Cartilage 9(3):223–236. https://doi.org/10.1177/1947603517710309
Ishøi L, Thorborg K, Kraemer O, Lund B, Mygind-Klavsen B, Hölmich P (2019) Demographic and radiographic factors associated with intra-articular hip cartilage injury: a cross-sectional study of 1511 hip arthroscopy procedures. Am J Sports Med 47(11):2617–2625. https://doi.org/10.1177/0363546519861088
Jordan MA, Van Thiel GS, Chahal J, Nho SJ (2012) Operative treatment of chondral defects in the hip joint: a systematic review. Curr Rev Musculoskelet Med 5(3):244–253. https://doi.org/10.1007/s12178-012-9134-y
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet 370(9597):1508–1519. https://doi.org/10.1016/S0140-6736(07)60457-7
Lee S, Nardo L, Kumar D et al (2015) Scoring hip osteoarthritis with MRI (SHOMRI): a whole joint osteoarthritis evaluation system. J Magn Reson Imaging 41(6):1549–1557. https://doi.org/10.1002/jmri.24722
Lewińska A, Palczewski P, Piłat K, Cieszanowski A, Rongies W (2021) The use of scoring hip osteoarthritis with mri as an assessment tool for physiotherapeutic treatment in patients with osteoarthritis of the hip. J Clin Med 11(1):17. https://doi.org/10.3390/jcm11010017
Medvedeva EV, Grebenik EA, Gornostaeva SN et al (2018) Repair of damaged articular cartilage: current approaches and future directions. Int J Mol Sci 19(8):2366. https://doi.org/10.3390/ijms19082366
Nam D, Shindle MK, Buly RL, Kelly BT, Lorich DG (2010) Traumatic osteochondral injury of the femoral head treated by mosaicplasty: a report of two cases. HSS J 6(2):228–234. https://doi.org/10.1007/s11420-010-9159-y
Neumann J, Zhang AL, Schwaiger BJ et al (2019) Validation of scoring hip osteoarthritis with MRI (SHOMRI) scores using hip arthroscopy as a standard of reference. Eur Radiol 29(2):578–587. https://doi.org/10.1007/s00330-018-5623-8
Schnetzke M, Schüler S, Hoffend J et al (2017) Interobserver and intraobserver agreement of ligamentous injuries on conventional MRI after simple elbow dislocation. BMC Musculoskelet Disord 18(1):85. https://doi.org/10.1186/s12891-017-1451-2
Schreiner MM, Raudner M, Marlovits S, et al. (2021) The MOCART (Magnetic Resonance Observation of Cartilage Repair Tissue) 2.0 Knee Score and Atlas. Cartilage 13(1_suppl):571S-587S. https://doi.org/10.1177/1947603519865308
Schwaiger BJ, Gersing AS, Lee S et al (2016) Longitudinal assessment of MRI in hip osteoarthritis using SHOMRI and correlation with clinical progression. Semin Arthritis Rheum 45(6):648–655. https://doi.org/10.1016/j.semarthrit.2016.04.001
Steadman JR, Rodkey WG, Rodrigo JJ (2001) Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res (391 Suppl):S362–369.https://doi.org/10.1097/00003086-200110001-00033
Trattnig S, Winalski CS, Marlovits S, Jurvelin JS, Welsch GH, Potter HG (2011) Magnetic resonance imaging of cartilage repair. Cartilage 2(1):5–26. https://doi.org/10.1177/1947603509360209
Verma K, Sitoula P, Gabos P, et al. (2014) Simplified skeletal maturity scoring system: learning curve and methods to improve reliability. Spine (Phila Pa 1976) 39(26):E1592–1598. https://doi.org/10.1097/BRS.0000000000000653
Acknowledgements
Please include the following authors to be searchable in PubMed as part of the MERCH Investigators and CHIPR collaborating groups:
Olufemi R. Ayeni MD, PhD, FRCSC (McMaster University, Hamilton, ON, Canada—Writing Committee Chair and Principal Investigator; ayenif@mcmaster.ca); Dan Cohen MD (McMaster University, Hamilton, ON, Canada – Writing Committee; dan.cohen@medportal.ca); Pierre-Olivier Jean MD, FRCSC (Université Laval, Québec City, QC, Canada – Writing Committee; po_jean24@hotmail.com); Kelly Johnston MD, FRCSC (University of Calgary, Calgary, AB, Canada – Writing Committee; kelly.johnston0@gmail.com); Nicole Simunovic MSc (McMaster University, Hamilton, ON, Canada – Writing Committee; simunon@mcmaster.ca); Pouyan Ahangar MD (McMaster University, Hamilton, ON, Canada; pouyan.ahangar@medportal.ca); Paul E. Beaulé MD, FRCSC (University of Ottawa, Ottawa, ON, Canada; pbeaule@toh.ca); Etienne L Belzile MD, FRCSC (CHU de Québec, Université Laval, Québec City, QC, Canada; etienne.belzile.med@ssss.gouv.qc.ca); Jordan Buchko MD, FRCSC (University of Saskatchewan, Regina, SK, Canada; jordanbuchko@gmail.com); Sasha Carsen MD, MBA, FRCSC (University of Ottawa, Ottawa, ON, Canada; scarsen@cheo.on.ca); Jas Chahal MD, FRCSC, MSc, MBA (University of Toronto, Toronto, ON, Canada; jchahal@utosm.com); Hema Choudur MBBS, FRCPC (McMaster University, Hamilton, ON, Canada; hnalinic@yahoo.com); Ryan Degen MD, MSc, FRCSC (Western University, London, ON, Canada; rdegen2@uwo.ca); George Grammatopoulos MBBS, DPhil, FRCS(Tr&Orth) (University of Ottawa, Ottawa, ON, Canada; ggrammatopoulos@toh.ca); Waleed Kishta MD, PhD, FRCSC (McMaster University, Hamilton, ON, Canada; waleed.kishta@medportal.ca); Devin Lemmex MD, FRCSC (Pan Am Clinic, Winnipeg, MB, Canada; dlemmex@panamclinic.com); Parth Lodhia MD, FRCSC (University of British Columbia, Vancouver, BC, Canada; parth.lodhia@ubc.ca); Marie-Lyne Nault MD, PhD, FRCSC (University of Montreal, Montreal, QC, Canada; marie-lyne.nault@umontreal.ca); Naveen Parasu MD, FRCPC (McMaster University, Hamilton, ON, Canada; parasun@hhsc.ca); Thierry Pauyo MD, FRCSC (McGill University, Montreal, QC, Canada; tpauyo@shrinenet.org); Kevin Smit MD, FRCSC (University of Ottawa, Ottawa, ON, Canada; ksmit@cheo.on.ca); Daniel Whelan MD, MSc, FRCSC (University of Toronto, Toronto, ON, Canada; daniel.whelan@unityhealth.to); Geoffrey Wilkin MD, FRCSC (University of Ottawa, Ottawa, ON, Canada; gwilkin@toh.ca); Kevin Willits MD, FRCSC (Western University, London, ON, Canada; kwillit@uwo.ca); Ivan Wong MD, FRCSC, Dip. Sports Med, MACM, FAANA (Dalhousie University, Halifax, NS, Canada; iw@drivanwong.com).
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Consortia
Contributions
The authors on the Writing Committee (DC, POJ, NS, KJ, ORA) contributed to the study design, data acquisition, formal analysis, interpretation of data, methodology, project administration, supervision, validation, and writing the original draft of the manuscript (DC, POJ, NS, ORA), as well as the study investigation and providing critical revisions of the manuscript (POJ, NS, KJ, ORA). All authors participated in the study investigation and have provided final approval of the manuscript version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by Hamilton Integrated Research Ethics Board (HiREB) prior to initiation and all consensus participants provided written informed consent prior to the meeting (#15021).
Consent for publication
Not applicable.
Competing interests
ORA is funded in part by a Tier 2 Canada Research Chair in Joint Preservation Surgery, and is the Editor-In-Chief of the Journal of ISAKOS. NS is the Managing Editor of the Journal of ISAKOS.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
The Magnetic Resonance Evaluation of the Repair of Cartilage in the Hip (MERCH) Investigators and The Canadian Hip Preservation Research Collaborative (CHIPR)., Ayeni, O.R. Defining hip cartilage repair: a modified delphi study to establish the Magnetic Resonance Evaluation of the Repair of Cartilage in the Hip (MERCH) score. J EXP ORTOP 10, 129 (2023). https://doi.org/10.1186/s40634-023-00676-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-023-00676-y