Abstract
Purpose
To investigate the correlation between postoperative limb/component alignments and clinical/functional outcomes following medial unicondylar knee arthroplasty (mUKA).
Methods
Inclusion criteria included peer-reviewed English- or German-language publications assessing postoperative limb or implant alignment and clinical outcomes of mUKA. Methodological Index for Non-Randomized Studies (MINORS) was used to assess article quality.
Results
A total of 2767 knees from 2604 patients were evaluated. Significant correlations were observed between postoperative limb/component alignments and clinical/functional outcomes after mUKA. Inferior outcomes were associated with lower placement and excessive valgus alignment of the tibia component (> 3°). A recommended external rotation of 4°-5° was identified for the tibia component, with specific cut-off values for the femoral and tibia components.
Conclusions
Optimal outcomes in mUKA were associated with a varus coronal limb alignment. The tibia implant component performed well within a specific alignment range. An exact external rotation value was recommended for the tibia component, while internal rotation correlated negatively with the femoral component.
Level of evidence
IV (level IV retrospective case series were included).
Similar content being viewed by others
Background
Unicondylar knee arthroplasty (UKA) is a well-established treatment option for osteoarthritis and osteonecrosis, specifically targeting either the lateral or the medial compartments of the knee joint [5]. Long-term studies have shown that UKA offers advantages such as improved range of motion, preservation of knee kinematics, and faster recovery compared to total knee arthroplasty (TKA) [1]. However, registry data has indicated higher revision rates for UKA compared to TKA, primarily attributed to limb and component malalignment and the progression of arthritis to the contralateral side [2]. Consequently, the optimal alignment in UKA remains a topic of ongoing debate [19, 28].
Traditionally, patients undergoing medial UKA (mUKA) have a preoperative varus phenotype and overall varus limb alignment. However, recent research challenges this notion, suggesting a more nuanced understanding of knee phenotypes and alignments; Hirschmann et al. analyzed 308 non-osteoarthritic knees and identified 43 different knee phenotypes, with functional and anatomical alignment targets observed in varying proportions [12]. Furthermore, a wide range of femoral mechanical angle (FMA) values and tibial mechanical angle (TMA) values were observed [11]. Given the considerable variability in coronal alignment alone, the extent to which limb alignment influences mUKA outcomes and potential avenues for improving outcomes through alignment adjustments warrant investigation.
It is well known that undercorrection may contribute to increased polyethylene wear, while overcorrection may lead to osteoarthritis in the lateral knee compartment [9, 29]. Additionally, component position and alignment are believed to impact clinical and functional outcomes [3, 31]. Previous studies have cautioned against valgus alignment in the coronal plane and excessive posterior slope in the sagittal plane of the tibia component [4, 10].
The objectives of this systematic review are twofold: to identify significant correlations between different postoperative limb/component alignments and clinical/functional outcomes in mUKA, and to examine whether specific postoperative coronal limb or coronal/axial component alignments yield superior clinical and/or functional outcomes compared to alternative alignments. It is hypothesized that significant correlations between postoperative limb/component alignment and clinical/functional outcomes exist in mUKA. However, it is presumed that no single postoperative limb/component alignment strategy can unequivocally be proven superior in terms of clinical/functional outcomes.
Materials and methods
A systematic literature search adhering to PRISMA guidelines [26] was conducted on PubMed, Embase, and Web of Science from their inception until September 2022 to identify potentially relevant articles for this review. Specific search terms such as “unicondylar knee replacement”, “unicondylar knee arthroplasty”, “unicondylar knee prosthesis”, “partial knee replacement”, “partial knee arthroplasty”, “partial knee prosthesis”, “unicompartmental knee replacement”, “unicompartmental knee arthroplasty”, “unicompartmental knee prosthesis”, “UKR”, “UKA”, “coronal alignment”, “clinical outcome”, “functional outcome” and “radiological outcome” were searched for in the title and abstract. Additional details regarding the search strategy can be found in Online Resource 1.
After removing duplicates and collecting all relevant articles, the studies were screened based on inclusion criteria using the title and abstract. Inclusion criteria encompassed English- or German-language publications in peer-reviewed journals that assessed the clinical and/or functional outcomes of medial unicondylar knee arthroplasty (mUKA) based on postoperative overall limb or component alignment. Studies unrelated to mUKA, pertaining to lateral unicondylar knee arthroplasty (lUKA), sagittal alignment, revision arthroplasty or failure rates were excluded. Only full-text articles with available numeric data (excluding graphical data) were considered.
Next, the selected articles were independently reviewed for eligibility through full-text analysis by two authors. The same authors then manually screened the reference lists for additional articles meeting the inclusion criteria but not covered by the original search terms. In case of uncertainty regarding inclusion a third author was consulted. The endpoints of the included studies comprised postoperative limb and component alignments, various clinical and functional scores, and patient-reported outcome measures (PROMs) such as the Knee Society Score (KSS), Oxford Knee Score (OKS), Knee Injury and Osteoarthritis Outcome Score (KOOS), Western Ontario and McMasters Universities Arthritis Index (WOMAC), and Forgotten Joint Score (FJS).
Quality assessment
The methodological quality of the included studies was independently assessed by two authors using the Methodological Index for Non-Randomized Studies (MINORS) for non-randomized comparative and non-comparative clinical intervention studies [32]. The maximum ideal score was 16 for non-comparative studies and 24 for comparative studies. The level of evidence of the included studies was also reported. Varus values have been reported as positive angles and valgus ones as negative angles.
Data extraction
Relevant information such as title, author, year of publication, study design, level of evidence, number of knees, follow-up period, patient demographics, clinical and functional outcome scores, and radiological outcomes were extracted from the selected publications by one author into a Microsoft Excel spreadsheet.
Statistical analysis
Continuous variables were described using means and standard deviations or means and ranges, while categorical variables were reported as absolute and relative frequencies. A significance level of p < 0.05 was considered statistically significant for data interpretation.
Results
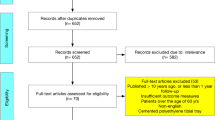
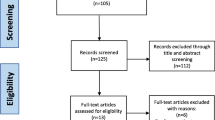
The initial literature search yielded 215 publications, of which 12 met the inclusion criteria (Fig. 1). Three additional studies were identified through reference list screening. Table 1 presents the characteristics of the included studies.
Flow-chart of the study selection process according to the PRISMA 2020 statement: an updated guideline for reporting systematic reviews [26]
Coronal limb alignment
When discussing WOMAC scores, it was observed that the 1–4° HKA group had better outcomes [36]. No significant differences were found in WOMAC and FJS scores between the -1–3° and 3–7° HKA groups [34]. Varus HKA alignments were however associated with lower OKS scores [7, 22], while the 0° to -2.5° tibiofemoral angle (TFA) group showed superior KSS scores [5]. Additionally, favorable KSS knee scores were found in the valgus HKA group [7, 24]. For detailed KSS and OKS data, please refer to Table 2.
Coronal implant alignment
The findings regarding the femoral component coronal angle (FCCA) were inconsistent, with varying optimal intervals for KSS and OKS scores reported across studies (Table 3). However, for the tibia component coronal angle (TCCA), most authors identified the -2.5° to 5° range as associated with the best clinical and functional outcomes (Table 4). In the study by Kamenaga et al. [20], a negative correlation was found between different tibia component angles and heights with OKS and OKS recovery, indicating worse outcomes for lower-placed tibia components (Table 5).
Axial implant alignment
When examining the tibia component, higher values of external rotation were linked to lower KSS and OKS scores (Table 6). Ng et al. [25] established significant cut-off values of 8–9° for the femoral component and 10–12° for the tibia component, indicating an impact on KSS and OKS scores. Studies conducted by Kamenaga et al. [21], Ng et al. [25], and Inui et al. [17] investigated the relationship between axial component angles and patient-reported outcomes, revealing negative associations between tibia component external/internal rotations and outcome scores (Table 7).
Discussion
The main finding of this review is the presence of significant correlations between different limb/component alignments and clinical/functional outcomes following mUKA. Specifically, the 1º-4º HKA alignment was reported as an optimal range for the coronal alignment of the knee, resulting in superior functional and clinical outcomes compared to other analyzed intervals. However, findings regarding the coronal alignment of the femoral component are somewhat heterogeneous and ambiguous, with different values presented by multiple authors as yielding the best outcomes. On the other hand, when discussing the coronal alignment of the tibia component, the analyzed studies predominantly suggest the -2.5º (valgus)—5º (varus) interval as generating the best clinical and functional outcomes. Furthermore, worse outcomes have been observed for patients with a tibia component positioned lower than the intercondylar eminence and the lateral joint, and/or in excessive valgus alignment relative to the lower limb axis. In terms of the axial alignment of the implant, a clear recommended interval of external rotation for the tibia component has been identified as 4º-5º. Cut-off values for external rotation of the tibia and femoral components have also been determined, with 10º-12º for the femoral component and 8º-9º for the tibia component. Additionally, a negative correlation has been observed between internal rotation of the tibia component and the femoral component. In conclusion, the study has achieved its aims and partially confirmed the hypothesis.
One interesting finding is the debatable reliability of the Knee Society Score (KSS) in calculating clinical outcomes, particularly the clinical/objective KSS. Several included studies question the deduction of KSS scores for varus or valgus limb alignments that fall outside the recommended intervals, such as 5º-10º valgus FTA for the 1989 KSS or 2º-10º valgus for the 2011 KSS [13, 14, 16, 30]. Authors such as Gulati et al. [7], Kim et al. [24], and Kennedy et al. [22] have reported poorer clinical/objective KSS scores associated with increasing valgus alignments solely because points were deducted for alignment values outside the recommended interval. Furthermore, patient satisfaction, pain (VAS), and functional scores (WOMAC, OKS) did not align with the clinical/objective KSS values (1989/2011), as some patients with inferior clinical/objective KSS scores exhibited superior WOMAC, OKS, and VAS scores. The use of different KSS scores by the authors of the included studies contributes significantly to the contradictory nature of some of the results.
This systematic review is the first to analyze both limb and implant component alignments following mUKA from the perspective of clinical and functional outcomes. While Riviere et al. conducted a systematic review on limb alignment in mUKA [28]; their focus on kinematic alignment led them to exclude any alignment strategy different from the kinematic approach. Additionally, they did not describe specific limits for the kinematic mUKA alignment technique. Furthermore, they are the only authors who use the term "kinematic alignment" in the context of medial UKA, making a direct comparison between their results and ours impossible.
However, this study has several limitations. One drawback is the lack of differentiation between fixed and mobile bearing medial UKA. The risks associated with overstuffing the medial compartment in mobile bearing UKA, as highlighted by Smith et al. [33], were not analyzed. Conversely, mobile bearing mUKA carries the risk of overcorrection, where a neutral to minor valgus alignment may lead to the initiation or progression of arthritic changes in the lateral compartment [15]. The loss of tension in the lateral collateral ligament or medial collateral ligament, which can result in bearing dislocation, especially in mobile bearing UKA, was also not discussed. Additionally, while there has been an increase in the number of papers on mUKA, long-term follow-up data in the literature are still limited. Moreover, the quality of the included studies is not very high, as no randomized controlled trials (RCTs) were available, and most studies were retrospective cohorts or case series. The retrospective nature of the majority of the studies included may have introduced patient selection bias, leading to potentially misleading results. The results also exhibit a significant degree of heterogeneity.
Despite these limitations, the reported results should provide guidance to orthopedic surgeons and improve the understanding of mUKA as a valid option for reducing knee pain and restoring functionality in patients with isolated medial osteoarthritis. However, future studies with higher levels of evidence and larger cohorts are needed. An international conversation should also be initiated regarding the criteria used in the KSS to award or deduct points for knee alignment. Additionally, given the existence of two KSS scores (1989 and 2011) in circulation, it is recommended that orthopedic surgeons reach a consensus and recommend the use of only one KSS while discontinuing the other. This will help prevent the dissemination of heterogeneous and contradictory results in the scientific community.
Conclusion
Optimal outcomes in mUKA were associated with a varus coronal limb alignment. The tibia implant component performed well within a specific alignment range. An exact external rotation value was recommended for the tibia component, while internal rotation correlated negatively with the femoral component.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article and its additional files.
Abbreviations
- FJA:
-
Femoral mechanical angle
- FJS:
-
Forgotten Joint Score
- FCCA:
-
Femoral component coronal angle
- FMA:
-
Femoral mechanical angle
- HKA:
-
Hip-knee-ankle
- KSS:
-
Knee Society Score
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- lUKA:
-
Lateral unicondylar knee arthroplasty
- MINORS:
-
Methodological Index for Non-Randomized Studies
- mUKA:
-
Medial unicondylar knee arthroplasty
- OKS:
-
Oxford Knee Score
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROMs:
-
Patient-reported outcome measures
- TFA:
-
Tibiofemoral angle
- TCCA:
-
Tibia component coronal angle
- TKA:
-
Total knee arthroplasty
- UKA:
-
Unicondylar knee arthroplasty
- UKR:
-
Unicompartmental knee replacement
- VAS:
-
Visual Analog Scale
- WOMAC:
-
Western Ontario and McMaster Universities Arthritis Index
References
Argenson JA, Chevrol-Benkeddache Y, Aubaniac J (2002) Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am 84(12):2235–2239
Australian Orthopaedic Association National Joint Replacement Registry (2019) Hip and Knee Arthroplasty Annual Report 2019. https://aoanjrr.sahmri.com. Accessed 11.09.2022.
Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M (2016) Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am 98(8):627–35. https://doi.org/10.2106/JBJS.15.00664
Chatellard R, Sauleau V, Colmar M, Robert H, Raynaud G, Brilhault J (2013) Medial unicompartmental knee arthroplasty: Does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res 99(4):219–225. https://doi.org/10.1016/j.otsr.2013.03.004
Ekhtiari S, Bozzo A, Madden K, Winemaker MJ, Adili A, Wood TJ (2021) Unicompartmental Knee Arthroplasty: Survivorship and Risk Factors for Revision: A Population-Based Cohort Study with Minimum 10-Year Follow-up. J Bone Joint Surg Am. Epub ahead of print. https://doi.org/10.2106/JBJS.21.00346
Gill JR, Vermuyten L, Wastnedge E, Nicolai P (2021) The effect of component alignment on clinical outcomes in fixed bearing unicompartmental knee arthroplasty. Knee 29:126–133. https://doi.org/10.1016/j.knee.2021.01.012
Gulati A, Chau R, Simpson DJ, Dodd CF, Gill HS, Murray DW (2009) The effect of leg alignment on the outcome of unicompartmental knee replacement. J Bone Joint Surg Br 91(4):469–474. https://doi.org/10.1302/0301-620X.91B4.22105
Gulati A, Chau R, Simpson DJ, Dodd CF, Gill HS, Murray DW (2009) Influence of component alignment on outcome for unicompartmental knee replacement. Knee 16(3):196–199. https://doi.org/10.1016/j.knee.2008.11.001
Hernigou P, Deschamps C (2004) Alignment Influences Wear in the Knee after Medial Unicompartmental Arthroplasty. Clin Orthop Relat Res 423(6):161–165. https://doi.org/10.1097/01.blo.0000128285.90459.12
Hernigou P, Deschamps G (2004) Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am 86(3):506–11
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg Sports Traumatol Arthrosc 27(5):1385–1393. https://doi.org/10.1007/s00167-019-05508-0
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27(5):1394–1402. https://doi.org/10.1007/s00167-019-05509-z
https://orthotoolkit.com/knee-society-score/. Last accessed 02.01.2023
https://www.kneesociety.org/assets/docs/2011-KS-Score-c-Pre-Op_ENG.pdf. Last accessed 02.01.2023
Inoue A, Arai Y, Nakagawa S, Inoue H, Yamazoe S, Kubo T (2016) Comparison of alignment correction angles between fixed-bearing and mobile-bearing UKA. J Arthroplasty 31(1):142–145. https://doi.org/10.1016/j.arth.2015.07.024
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 11(248):13–4 PMID: 2805470
Inui H et al (2020) Femorotibial rotational mismatch of the Oxford unicompartmental knee in the flexion position is a risk for poor outcomes. Knee 27(3):1064–1070. https://doi.org/10.1016/j.knee.2020.03.008
Iriberri I, Aragón JF (2014) Alignment of the tibial component of the unicompartmental knee arthroplasty, assessed in the axial view by CT scan: does it influence the outcome? Knee 21(6):1269–1274. https://doi.org/10.1016/j.knee.2014.06.008
Johal S, Nakano N, Baxter M, Hujazi I, Pandit H, Khanduja V (2018) Unicompartmental knee arthroplasty: the past, current controversies, and future perspectives. J Knee Surg 31(10):992–998. https://doi.org/10.1055/s-0038-1625961
Kamenaga T, Hiranaka T, Hida Y, Fujishiro T, Okamoto K (2018) Effect of tibial component position on short-term clinical outcome in Oxford mobile bearing unicompartmental knee arthroplasty. J Orthop Sci 23(5):807–810. https://doi.org/10.1016/j.jos.2018.04.012
Kamenaga T, Hiranaka T, Kikuchi K, Hida Y, Fujishiro T, Okamoto K (2018) Influence of tibial component rotation on short-term clinical outcomes in Oxford mobile-bearing unicompartmental knee arthroplasty. Knee 25(6):1222–1230. https://doi.org/10.1016/j.knee.2018.06.016
Kennedy JA, Molloy J, Jenkins C, Mellon SJ, Dodd CF, Murray DW (2019) Functional outcome and revision rate are independent of limb alignment following Oxford medial unicompartmental knee replacement. J Bone Joint Surg Am 101(3):270–275. https://doi.org/10.2106/JBJS.18.00497
Khow YZ, Liow MHL, Lee M, Chen JY, Lo NN, Yeo SJ (2021) Coronal alignment of fixed-bearing unicompartmental knee arthroplasty femoral component may affect long-term clinical outcomes. J Arthroplasty 36(2):478–487. https://doi.org/10.1016/j.arth.2020.07.070
Kim KT, Lee S, Kim TW, Lee SJ, Boo KH (2012) The influence of postoperative tibiofemoral alignment on the clinical results of unicompartmental knee arthroplasty. Knee Surg Relat Res 24(2):85–90. https://doi.org/10.5792/ksrr.2012.24.2.85
Ng JP et al (2020) Does component axial rotational alignment affect clinical outcomes in Oxford unicompartmental knee arthroplasty? Knee 27(6):1953–1962. https://doi.org/10.1016/j.knee.2020.10.016
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Polat AE, Polat B, Gurpinar T, Peker B, Tuzuner T (2020) Factors affecting the functional outcome of Oxford phase 3 unicompartmental knee arthroplasty. Acta Ortop Bras 28(2):78–83. https://doi.org/10.1590/1413-785220202802225137
Rivière C et al (2022) Kinematic alignment of medial UKA is safe: a systematic review. Knee Surg Sports Traumatol Arthrosc 30(3):1082–1094. https://doi.org/10.1007/s00167-021-06462-6
Sarmah SS, Patel S, Hossain FS et al (2015) The radiological assessment of total and unicompartmental knee replacements. J Bone Jt Surg 41(1):41–44. https://doi.org/10.1302/0301-620X.94B10.29411
Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN (2012) The new knee society knee scoring system. Clin Orthop Relat Res 470(1):3–19. https://doi.org/10.1007/s11999-011-2135-0
Shelton TJ, Nedopil AJ, Howell SM, Hull ML (2017) Do varus or valgus outliers have higher forces in the medial or lateral compartments than those which are in-range after a kinematically aligned total knee arthroplasty? limb and joint line alignment after kinematically aligned total knee arthroplasty. Bone Joint J 99-B(10):1319–1328. https://doi.org/10.1302/0301-620X.99B10.BJJ-2017-0066.R1
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Smith TO, Hing CB, Davies L, Donell ST (2009) Fixed versus mobile bearing unicompartmental knee replacement: A meta-analysis. Orthop Traumatol Surg Res 95(8):599–605. https://doi.org/10.1016/j.otsr.2009.10.006
Van der List JP, Chawla H, Villa JC, Pearle AD (2016) Different optimal alignment but equivalent functional outcomes in medial and lateral unicompartmental knee arthroplasty. Knee 23(6):987–995. https://doi.org/10.1016/j.knee.2016.08.008
Yamagami R et al (2020) Implant alignment and patient factors affecting the short-term patient-reported clinical outcomes after Oxford unicompartmental knee. Arthroplasty J Knee Surg 34(13):1413–1420. https://doi.org/10.1055/s-0040-1709678
Zuiderbaan HA, Van der List JP, Chawla H, Khamaisy S, Thein R, Pearle AD (2016) Predictors of subjective outcome after medial unicompartmental knee arthroplasty. J Arthroplasty 31(7):1453–1458. https://doi.org/10.1016/j.arth.2015.12.038
Acknowledgements
The authors would like to extend their thanks to Silvia Reichl, Iris Spörri and Felix Amsler, for offering their invaluable research knowledge, when conducting this systematic review.
Funding
Open access funding provided by University of Basel The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and/or analysis were performed by Manuel-Paul Sava, Isabel Scala and Alexandra Leica. The final draft of the manuscript was written by Manuel-Paul Sava and all authors commented on previous versions of it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical review and approval were waived for this study, because, unlike primary research, no new personal, sensitive or confidential information are collected from participants. Only publicly available documents were used for this systematic review.
No consent to participate was required due to the nature of this study.
Consent for publication
No consent to publish was required due to the nature of this study.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sava, MP., Leica, A., Scala, I. et al. Significant correlations between postoperative outcomes and various limb and component alignment strategies in medial unicompartmental knee arthroplasty: a systematic review. J EXP ORTOP 10, 93 (2023). https://doi.org/10.1186/s40634-023-00655-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-023-00655-3