Abstract
Purpose
The objective of this study was to investigate whether RCR (rotator cuff repair) with BMS (bone marrow stimulation) can provide a lower retear rate and better shoulder function than arthroscopic RCR alone in rotator cuff tear (RCT) patients.
Method
The PubMed, Cochrane Library, EMBASE and Web of Science databases were searched until Feb 2022. Risk of bias for randomized controlled trials was evaluated by two independent reviewers with Cochrane collaboration risk bias of tool, and that for cohort studies was evaluated with the Newcastle–Ottawa Scale (NOS). The primary outcome was the retear rate. Secondary outcomes included the American Shoulder and Elbow Surgeons (ASES) score, University of California, Los Angeles Shoulder Scale (UCLA) score, Constant-Murley score (CMS) and visual analogue scale (VAS) score. Subgroup analysis was performed to explore the effect of suture method and tear size on BMS procedure.
Result
Five randomized controlled trials and four cohort studies with a total of 827 patients were included. The pooled retear rate between the RCR with BMS group and the RCR alone group was significantly different (17.5% vs. 28.9%; P < 0.0001). There were no differences in the ASES score, UCLA score and VAS score. The CMS was significantly higher in RCR with BMS group than the RCR alone groups (P = 0.02), while the difference was well below the MCID. RCR with BMS resulted in a significantly lower retear rate than RCR alone for large and massive RCTs (19.7% vs. 32.5%; P = 0.01).
Conclusion
Compared with RCR alone, RCR with BMS can significantly reduce the retear rate in arthroscopic RCT patients while not clinically relevant differences were found. BMS may further reduce the retear rate of large and massive RCTs.
Level of evidence
Level III; Systematic Review and Meta-analysis.
Similar content being viewed by others
Introduction
Rotator cuff tear (RCT) is a common injury that causes shoulder pain and dysfunction. When conservative treatment fails, arthroscopic rotator cuff repair (RCR) can provide good clinical outcomes [1,2,3,4]. Despite advances in arthroscopic techniques, the retear rate of RCR is reported to range between 18% and 94%. Previous studies have shown that the retear rate of RCR is closely correlated with the initial biomechanical strength, tear size and tendon tissue quality [1, 5]. Therefore, providing a proper biological environment is one of the most effective ways to improve tendon-to-bone healing.
In 2009, Snyder et al. first used BMS combined with a single-row repair technique in RCT patients. By making several bone vents on the footprint area, a “crimson duvet”, which contains abundant marrow mesenchymal stem cells (MSCs), platelets and growth factors to promote tendon healing and reduce the retear rate after RCR, was formed [6]. While the effect of BMS remains controversial in the literature [7, 8]. Ruiz Ibán et al. reported no difference on constant score and EQ-5D-3 L in medium to massive RCT between groups [8]. Jo et al. reported no significant differences in clinical outcomes [7]. Sun et al. found that large-diameter microfractures may worsen rotator cuff healing in an animal study [9]. To our knowledge, there is no universally accepted conclusion on the effect of BMS on promoting the healing of tendons during RCR procedures.
The primary purpose of this study was to identify, summarize, and synthesize the evidence available of BMS in RCR and compare the retear rate between RCR combined with BMS and RCR alone in RCT patients. We hypothesized that in combination with RCR, BMS would significantly decrease retear rates and provide better clinical outcomes than RCR alone.
Methods
Search strategy
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and this study was registered in PROSPERO (CRD42022351459), two independent reviewers performed this systematic review and meta-analysis. The PubMed, Cochrane Library, EMBASE and Web of Science databases were searched until Feb 2022. The following keywords were used: rotator cuff repair, rotator cuff tear, micro-fracture, bone marrow stimulation, multi-drilling, multiple channels, multiple drills, nano-fracture, bone marrow vents, multiple channeling, and marrow-stimulating. The more details were shown in the Appendix 1. The key words were restricted to the title or abstract. The references of all included studies were manually cross-referenced for further review to ensure a complete search of relevant studies not located in the original systematic search.
Inclusion and exclusion criteria
Studies eligible for inclusion had to meet the following criteria: (1) two- or three-arm randomized controlled trials or cohort studies (Level of evidence: I-III) that reported clinical outcomes after primary arthroscopic RCR (ARCR), (2) BMS was used in one of the study groups, (3) at least 12 months of follow-up, and (4) patients older than 18 years. Exclusion criteria for the studies were as follows: (1) reviews and studies with no control group, (2) basic science studies such as cadaveric and animal studies, (3) studies investigating revision RCR, and (4) studies with incomplete data. Using these inclusion and exclusion criteria, the titles and abstracts of each of the papers were screened, and the full texts of potentially relevant studies were subsequently reviewed. A third senior author made a final decision on literature inclusion and exclusion if any discrepancy arose between the two independent reviewers.
Quality assessment
The Cochrane collaboration risk-of-bias tool was used by two reviewers to evaluate the risk of bias for randomized controlled trials [10]. Any discrepancy was judged by another senior author to reach a consensus through discussion. With reference to the risk-of-bias tool items, we classified the study bias into high risk of bias, low risk of bias or unclear risk of bias. For cohort studies, the Newcastle–Ottawa Scale (NOS) was utilized to assess bias of the study. Studies with scores greater than or equal to 7 were classified as having a low risk of bias, those with scores of 4 to 6 were classified as having a moderate risk of bias, and those with scores less than 4 were classified as having a high risk of bias.
Data extraction
All data from the included studies were extracted. The main data extracted in this study included author, publication year, research design, sample size, average age, sex, ARCR and BMS procedure. These data were imported into RevMan 5.3 meta-analysis software (The Cochrane Collaboration, Oxford, United Kingdom), data on the retear rate, the pre- and postoperative shoulder functional outcome scores, tear size and method of repair from all included studies were used for statistical analysis.
All patients were classified into two groups: the RCR with BMS group and the RCR alone group. The primary outcome of this study was the retear rate. Secondary shoulder functional outcomes consisted of the American Shoulder and Elbow Surgeons (ASES) score [11], University of California, Los Angeles Shoulder Scale (UCLA) score [12], Constant-Murley score (CMS) [13], and visual analogue scale (VAS) score [14, 15]. We compared the changes in the mean differences in the ASES score, UCLA score, CMS and VAS score to minimal clinically important difference (MCID) thresholds determined by previous rotator cuff studies: 17.9, 3, 6.7 and 1.4, respectively [16,17,18].
Statistical analysis
For continuous outcomes, the mean difference was obtained and calculated from the inverse variance method. When the standard deviation was not provided for specific continuous outcomes, a well-established statistical formula described by Hozo et al. was used for imputation [19]. For dichotomous outcomes, the risk ratio (RR) was calculated using the Cochran-Mantel-Haenszel method. The heterogeneity of studies was tested by the standard χ2 test, and the I2 statistic was calculated to quantify heterogeneity. When the heterogeneity achieved significance (I2 < 50%), a fixed-effects model was used for the meta-analysis between two groups. When the heterogeneity did not achieve significance (I2 > 50%), a random-effects model was used for the meta-analysis between two groups. We calculated 95% confidence intervals (CIs) from all point estimates, and p < 0.05 was considered statistically significant for all outcome measurements.
Results
Literature search
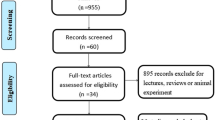
The literature screen yielded 216 unique results. After screening the full texts, nine studies were deemed appropriate for inclusion in this study. There were five randomized controlled trials [8, 20,21,22,23], and four cohort studies [7, 24,25,26] (Fig. 1).
Study quality assessment
In the quality evaluation of the five randomized controlled trials, allocation concealment was inadequate in one study by Osti et al., and it didn’t meet the rules of blinding as well because of inadequate patient blinding. Two studies did not meet our criterion for complete outcome data, one study by Lapner had a possibility of a type II error given the follow-up rate of 78%, while in another one by Ruiz Ibán, a power of only 0.5 was selected to limit the sample size. No study contained detection, selective reporting or other biases (Fig. 2).
In the quality evaluation of the four cohort studies, the NOS scores of two cohort studies were 9, and those of the other two studies were 7. Seven articles were of good quality, with a standardized research design and good research value (Table 1).
Patient demographics
There were a total of 827 patients included in the nine studies. Among the 827 patients, 749 had postoperative radiologic outcomes regarding the retear condition. The follow-up time ranged from 12 to 24 months. A total of 403 of 827 (48.7%) patients were in the RCR with BMS group, with an average age of 60.6 years (range, 58.1-64.7 years), 182 males and 221 females. Among them, 201 patients were treated by single-row repair, and 202 patients were treated by double-row repair (traditional double-row or suture-bridge technique). A total of 424 of 827 (51.3%) patients were in the RCR alone group, with an average age of 60.7 years (range, 57.8-64.3 years), 218 males and 206 females. Among them, 194 patients were treated by single-row repair, and 230 patients were treated by double-row repair (traditional double-row or suture-bridge technique). The author, publication year, research design, sample size, average age, sex, clinical outcome, method of BMS, and definition of retear are shown in Table 2. The method of suture repair, retear rates, functional outcome, VAS score, and duration of follow-up are shown in Table 3.
Clinical outcomes
Retear rate
The overall retear rate was 23.2% (174 of 749):17.5% (65 of 372) in the RCR with BMS group and 29.0% (109 of 377) in the RCR alone group. There was a significant difference between the two groups, with good homogeneity (I2 = 0%, P = 0.73; RR, 0.58; 95% CI, 0.44 to 0.76; P < 0.0001) (Fig. 3, A). When only pooling the retear rate of the five randomized controlled trials, which included 369 patients, there was a significant difference between the RCR with BMS group and the RCR alone group (15.3% vs. 24.7%; RR, 0.62; 95% CI, 0.42 to 0.93; I2 = 0%; P = 0.02). When only pooling the four cohort studies, which included 380 patients, there was also a significant difference in the retear rate between the RCR with BMS group and the RCR alone group (19.6% vs. 33.0%; RR, 0.55; 95% CI, 0.39 to 0.79; I2 = 0%; P = 0.001).
A Forest plot for the pooled retear rate. B Forest plot of the visual analogue scale score. C Forest plot of the University of California, Los Angeles Shoulder Scale score. D Forest plot of the American Shoulder and Elbow Surgeons score. E Forest plot of the Constant-Murley score. F Forest plot of the results of the subgroup analysis of single-row repair. G Forest plot of the results of the subgroup analysis of double-row repair. H Forest plot of the results of the subgroup analysis of large or massive tears. CI, confidence interval; IV, inverse variance; SD, standard deviation
Pain
Four studies (372 patients) performed a VAS evaluation and revealed no significant difference between RCR with BMS and RCR alone (mean difference, 0.11; 95% CI, − 0.21 to 0.43; I2 = 41%; P = 0.51) (Fig. 3, B) [16, 20, 27, 28]. The mean difference in the VAS score did not reach the MCID threshold.
Functional outcomes
Three studies including 279 patients utilized the UCLA and found no significant difference between the two groups (mean difference, 0.55; 95% CI, − 0.73 to 1.82; I2 = 0%; P = 0.40) (Fig. 3, C) [7, 22, 24]. Four studies including 391 patients reported the ASES score at the final follow-up and found that it was not significantly different between the two groups (mean difference, 1.10; 95% CI, − 0.93 to 3.13; I2 = 0%; P = 0.29) (Fig. 3, D) [7, 20, 23, 24]. Seven studies including 576 patients used the CMS and found a significant difference between the two groups (mean difference, 2.30; 95% CI, 0.43 to 4.16; I2 = 0%; P = 0.02) (Fig. 3, E) [7, 8, 20,21,22,23, 25]. In each article that included the CMS, the BMS group had a higher CMS than the non-BMS group, but there were no significant differences.
Subgroup analysis
Two studies were excluded from the subgroup analysis because details on the suture repair method were lacking [7, 23]. Among nine studies, single-row repair was used in four (312 patients) [21, 22, 24, 25]. In the subgroup analysis on single-row repair, there was a significant difference in the retear rate between the RCR with BMS group and the RCR alone group (rate, 22.7% vs. 32.9%; RR, 0.68; 95% CI, 0.48 to 0.98; I2 = 0%; P = 0.04) (Fig. 3, F). Double-row/suture bridge repair was used in three studies [8, 20, 26], which included 255 patients. In the subgroup analysis on double-row/suture bridge repair, there was a significant difference in the retear rate between the RCR with BMS group and the RCR alone group (rate, 12.9% vs. 24.5%; RR, 0.50; 95% CI, 0.29 to 0.88; I2 = 0%; P = 0.02) (Fig. 3, G). The retear rate was lower in the double-row alone group than in the single-row alone group (24.5% vs. 32.9%). The retear rate was also lower in the double-row RCR with BMS group than in the single-row RCR with BMS group (12.9% vs. 22.7%). Although the suture repair method did not affect the tendency of BMS to reduce the retear rate, it was impossible to perform further statistical analysis because of the limited number of relevant studies.
Only three cohort studies involved large and massive RCTs [24,25,26]. There was a significant difference in the retear rate between the RCR with BMS group and the RCR alone group (rate, 19.7% vs. 32.5%; RR, 0.56; 95% CI, 0.35 to 0.89; I2 = 51%; P = 0.01) (Fig. 3, H). It was impossible to analyse other tear sizes because most of the studies did not mention the distribution and details of the sizes of the RCTs in their series.
Discussion
The most important finding of the present study is that RCR combined with BMS can significantly reduce the retear rate in RCT patients. However, it cannot provide better clinical outcomes than RCR alone. BMS may further reduce the retear rate for large and massive RCTs, but its effect according to different suture methods for performing RCR has yet to be determined.
Snyder and Burns first proposed RCR with BMS using the term “crimson duvet” in 2009 [6], which describes a reddish purple-coloured clot formed from the bone marrow vent. It is known to contain MSCs, platelets with growth factors and vascular elements, which may provide important elements for tendon healing. In their subsequent study in 2020, 91% of their patients were satisfied with the results, 92% showed an intact rotator cuff at a minimum of 24 months of follow-up [29]. Pulatkan et al. and Yoon et al. both reported that the BMS group had a lower retear rate than the non-BMS group (33% vs. 14% and 46% vs. 19%, respectively) [31, 42]. In 2020, Ruiz Ibán reported lower retear in BMS group (19.4% vs 42.4%, p = 0.038) [8]. In 2019, Ajrawat et al. reported a statistically significant difference in pooled retear rates favouring BMS over RCR alone but included only two randomized studies and two cohort studies. When pooling the retear rate of the included randomized studies, there was no significant difference between the two groups [30]. In the present study, which incorporated a larger number of studies, the retear rate of the RCR with BMS group, regardless of the kind of study, was significantly lower than that of the RCR alone group (17.5% vs. 29.0%, P < 0.0001), which led us to conclude that the expected effect of BMS on reducing the retear rate in the RCR procedure was achieved.
In the present study, none of the shoulder functional outcomes in the RCR with BMS group except for the CMS were significantly different from those of the RCR alone group. This result is consistent with that of previous studies [31, 32]. The possible explanations are as follows: First, functional outcomes do not strongly correlate with retearing of the rotator cuff. Russell et al. reported no clinically significant differences in functional outcome scores or pain regardless of the structural integrity of the repair [33]. Second, the exudation of growth factors after BMS may result in a lack of long-term effects on tendon healing. Yoon et al. indicated that even though the “crimson duvet” covers the tendon-bone area, it probably subsequently vanishes into the subacromial space [34].
The size of RCTs may play a role in the efficiency of BMS. Taniguchi et al. reported no significant difference in the effect on medium RCTs between the two groups, while there were significant differences in the retear rate between the two groups for large to massive tears [26]. Milano et al. also performed a subgroup analysis for tear size, which suggested that the application of BMS could result in better healing for large tears [6]. This finding might indicate that the size of RCTs can affect the effect of BMS in reducing the retear rate. The present study showed a significant difference in the retear rate between the RCR with BMS group and the RCR alone group for large and massive tears (19.7% vs. 32.5%, P = 0.01). However, it should be noted that only three cohort studies were included in this subgroup analysis. Although BMS significantly reduced the retear rate in patients with large and massive RCTs, further investigation with more patient involvement and longer follow-up times is needed.
The suture method may also have an effect on the efficiency of BMS. Single-row and double-row repair techniques both achieve satisfactory clinical outcomes by restoring the footprint and providing adequate initial fixation [35,36,37]. In the present study, when subdivided into different repair method groups, the retear rate of the double-row RCR alone group was lower than that of the single-row RCR alone group (24.5% vs. 32.9%), which is comparable to the results reported in previous studies. Furthermore, the retear rate of the double-row repair RCR with BMS group was lower than that of the single-row repair RCR with BMS group (12.9% vs. 22.7%), which indicated that the additional BMS procedure did not change the effect of the repair technique on the retear rate of RCR. However, we were unable to obtain the p value for these analyses because of the limited number of relevant studies and the limitations of the relevant statistics.
Limitation
Our study has several limitations, as follows. First, the present study only included nine studies involving 827 patients with 12-24 months of follow-up. Regarding the evaluations of retear RCRs and functions, the number of patients was still low, and long-term follow-up data are lacking. Second, there were only three cohort studies involved in the subgroup analysis of tear size and seven in the subgroup analysis of the RCR technique, which limits the generalizability of the conclusions of this study. Although the subgroup analysis reduced the heterogeneity, it would result in insufficient statistical power in the RCR with BMS group. Finally, only four studies were deemed to have a low risk of bias. This also reduces the credibility of the conclusion of this study.
Conclusions
The present study demonstrated that RCR with BMS can significantly reduce the retear rate compared with RCR alone, especially in patients with large and massive RCTs. There were no significant differences in shoulder functional outcomes between the two groups except for the CMS, and all of the shoulder functional outcomes changes didn’t achieve the minimal clinically important difference (MCID). Neither single-row nor double-row RCR changed the tendency of BMS to reduce the retear rate.
References
Abtahi AM, Granger EK, Tashjian RZ (2015) Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop 6(2):211–220
Chung SW, Huong CB, Kim SH, Oh JH (2013) Shoulder stiffness after rotator cuff repair: risk factors and influence on outcome. Arthroscopy 29(2):290–300
Gartsman GM, Drake G, Edwards TB, Elkousy HA, Hammerman SM, O'Connor DP, Press CM (2013) Ultrasound evaluation of arthroscopic full-thickness supraspinatus rotator cuff repair: single-row versus double-row suture bridge (transosseous equivalent) fixation. Results of a prospective, randomized study. J Shoulder Elb Surg 22(11):1480–1487
Mall NA, Tanaka MJ, Choi LS, Paletta GA Jr (2014) Factors affecting rotator cuff healing. J Bone Joint Surg Am 96(9):778–788
Madry H, Gao L, Eichler H, Orth P, Cucchiarini M (2017) Bone marrow aspirate concentrate-enhanced marrow stimulation of chondral defects. Stem Cells Int 2017:1609685
Snyder SJ, Burns J (2009) Rotator cuff healing and the bone marrow “ crimson duvet ” from clinical observation to science. Tech Should Elbow Surg 10(4):130–137
Jo CH, Shin JS, Park IW, Kim H, Lee SY (2013) Multiple channeling improves the structural integrity of rotator cuff repair. Am J Sports Med 41(11):2650–2657
Ruiz Ibán MA, Sanchez Alepuz E, Diaz Heredia J, Hachem AI, Ezagüi Bentolila L, Calvo A, Verdú C, de Rus Aznar I, Soler Romagosa F (2021) Footprint preparation with nanofractures in a supraspinatus repair cuts in half the retear rate at 1-year follow-up. A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 29(7):2249–2256
Sun Y, Kwak JM, Kholinne E, Zhou Y, Tan J, Koh KH, Jeon IH (2020) Small subchondral Drill holes improve marrow stimulation of rotator cuff repair in a rabbit model of chronic rotator cuff tear. Am J Sports Med 48(3):706–714
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group, & Cochrane Statistical Methods Group (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Michener LA, McClure PW, Sennett BJ (2002) American shoulder and elbow surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elb Surg 11(6):587–594
Amstutz HC, Sew Hoy AL, Clarke IC (1981) UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res 155:7–20
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE (2008) Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 31(2):165–169
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short Form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and Constant osteoarthritis pain (ICOAP). Arthritis Care Res 63(Suppl 11):S240–S252
Gagnier JJ, Robbins C, Bedi A, Carpenter JE, Miller BS (2018) Establishing minimally important differences for the American shoulder and elbow surgeons score and the Western Ontario rotator cuff index in patients with full-thickness rotator cuff tears. J Shoulder Elb Surg 27(5):e160–e166
Tashjian RZ, Deloach J, Porucznik CA, Powell AP (2009) Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elb Surg 18(6):927–932
Xu S, Chen JY, Lie H, Hao Y, Lie D (2019) Minimal clinically important difference of Oxford, Constant, and UCLA shoulder score for arthroscopic rotator cuff repair. J Orthop 19:21–27
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Lapner P, Pollock JW, Laneuville O, Uhthoff HK, Zhang T, Sheikh A, McIlquham K, Trudel G (2021) Preoperative bone marrow stimulation does not improve functional outcomes in arthroscopic cuff repair: a prospective randomized controlled trial. Bone Joint J 103-B(1):123–130. https://doi.org/10.1302/0301-620X.103B1.BJJ-2020-0011.R2
Milano G, Saccomanno MF, Careri S, Taccardo G, De Vitis R, Fabbriciani C (2013) Efficacy of marrow-stimulating technique in arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy 29(5):802–810
Osti L, Del Buono A, Maffulli N (2013) Microfractures at the rotator cuff footprint: a randomised controlled study. Int Orthop 37(11):2165–2171
Toro F, Pinochet F, Ruiz F, Moraga C, Pozo R, Oliva JP, Reinares F, Mardones P (2022) Functional and radiologic results of the crimson duvet procedure in rotator cuff treatment: a randomized controlled clinical trial. J Shoulder Elb Surg 31(6):1200–1207
Kim C, Lee YJ, Kim SJ, Yoon TH, Chun YM (2020) Bone marrow stimulation in arthroscopic repair for large to massive rotator cuff tears with incomplete footprint coverage. Am J Sports Med 48(13):3322–3327
Pulatkan A, Anwar W, Tokdemir S, Akpinar S, Bilsel K (2020) The clinical and radiologic outcome of microfracture on arthroscopic repair for full-thickness rotator cuff tear. J Shoulder Elb Surg 29(2):252–257
Taniguchi N, Suenaga N, Oizumi N, Miyoshi N, Yamaguchi H, Inoue K, Chosa E (2015) Bone marrow stimulation at the footprint of arthroscopic surface-holding repair advances cuff repair integrity. J Shoulder Elb Surg 24(6):860–866
Degan TJ, Hartzler RU, Rahal A, DeBerardino TM, Burkhart SS (2022) Prospective 1-year outcomes are maintained at short-term final follow-up after superior capsular reconstruction augmentation of complete rotator cuff repair. Arthroscopy 38(5):1411–1419
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 86(2):219–224
Dierckman BD, Frousiakis P, Burns JP, Barber FA, Wodicka R, Getelman MH, Karzel RP, Snyder SJ (2021) Arthroscopic repair of medium to large rotator cuff tears with a triple-loaded medially based single-row technique augmented with marrow vents. Arthroscopy 37(1):28–37
Ajrawat P, Dwyer T, Almasri M, Veillette C, Romeo A, Leroux T, Theodoropoulos J, Nauth A, Henry P, Chahal J (2019) Bone marrow stimulation decreases retear rates after primary arthroscopic rotator cuff repair: a systematic review and meta-analysis. J Shoulder Elb Surg 28(4):782–791
Anderson K, Boothby M, Aschenbrener D, van Holsbeeck M (2006) Outcome and structural integrity after arthroscopic rotator cuff repair using 2 rows of fixation: minimum 2-year follow-up. Am J Sports Med 34(12):1899–1905
Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D (2007) Can a double-row anchorage technique improve tendon healing in arthroscopic rotator cuff repair?: a prospective, nonrandomized, comparative study of double-row and single-row anchorage techniques with computed tomographic arthrography tendon healing assessment. Am J Sports Med 35(8):1247–1253
Russell RD, Knight JR, Mulligan E, Khazzam MS (2014) Structural integrity after rotator cuff repair does not correlate with patient function and pain: a meta-analysis. J Bone Joint Surg Am 96(4):265–271
Yoon JP, Chung SW, Kim JY, Lee BJ, Kim HS, Kim JE, Cho JH (2016) Outcomes of combined bone marrow stimulation and patch augmentation for massive rotator cuff tears. Am J Sports Med 44(4):963–971
Dines JS, Bedi A, ElAttrache NS, Dines DM (2010) Single-row versus double-row rotator cuff repair: techniques and outcomes. J Am Acad Orthop Surg 18(2):83–93
Park MC, Cadet ER, Levine WN, Bigliani LU, Ahmad CS (2005) Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med 33(8):1154–1159
Roth KM, Warth RJ, Lee JT, Millett PJ, ElAttrache NS (2014) Arthroscopic single-row versus double-row repair for full-thickness Posterosuperior rotator cuff tears: a critical analysis review. JBJS Rev 2(7):e6
Funding
This study was supported by the National Nature Science Foundation of China 82172513.
Author information
Authors and Affiliations
Contributions
Guang Yang designed the study, systematic search, and drafted the paper. Shangzhe Li designed and supervised the study; Guang Yang and Shangzhe Li performed the data extraction and analysis. Hailong Zhang and Chunyan Jiang made contribution to data analysis and interpretation and co-drafted the paper. Yi Lu designed the study, systematic search, co-drafted the paper. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This review did not involve primary data collection from patients and as such research approval was not obtained.
Competing interests
The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, G., Li, S., Jiang, C. et al. The role of bone marrow stimulation in rotator cuff repair: a systematic review and meta-analysis. J EXP ORTOP 10, 27 (2023). https://doi.org/10.1186/s40634-023-00589-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-023-00589-w