Abstract
Purpose
The study aims were to assess the kinematic data, Internal-External (IE) rotation, and Antero-Posterior (AP) translation of the contact points between the femoral condyles and polyethylene insert and to develop a combined dynamic RSA-FE (Radiostereometric – Finite Element) model that gives results congruent with the literature.
Methods
A cohort of 15 patients who underwent cemented cruciate-retaining highly congruent mobile-bearing total knee arthroplasty were analyzed during a sit-to-stand motor task. The kinematical data from Dynamic RSA were used as input for a patient-specific FE model to calculate condylar contact points between the femoral component and polyethylene insert.
Results
The femoral component showed an overall range about 4 mm of AP translation during the whole motor task, and the majority of the movement was after 40° of flexion. Concerning the IE rotation, the femoral component started from an externally rotate position (− 6.7 ± 10°) at 80° of flexion and performed an internal rotation during the entire motor task. The overall range of the IE rotation was 8.2°.
Conclusions
During the sit to stand, a slight anterior translation from 40° to 0° of flexion of the femoral component with respect to polyethylene insert, which could represent a paradoxical anterior translation. Despite a paradoxical anterior femoral translation was detected, the implants were found to be stable. Dynamic RSA and FE combined technique could provide information about prosthetic component’s stress and strain distribution and the influence of the different designs during the movement.
Similar content being viewed by others
Background
Total knee arthroplasty (TKA) is the gold standard treatment for patients with primary osteoporosis, as it can relief pain and restore joint function. The prosthetic implant has a survival rate of 82% at 25 years [14]. Moreover, a patient satisfaction about 80–90% after 1-5 years has been reported [5, 10]. The main causes of TKA failure and revision are infection, aseptic loosening, periprosthetic fracture, stiffness, and instability [26, 28]. The last one may be evaluated through knee kinematics using different techniques, both in vitro and in vivo [2, 9].
Model-based RSA is already used to assess in vivo knee kinematics in several prosthesis designs during daily life motor tasks [1, 7, 21, 27]. Although dynamic RSA allows to analyze in-vivo knee kinematics, it does not provide with the same accuracy the exactly contact points between the femoral condyles and polyethylene insert. Furthermore, the kinematical data have been assessed frame by frame not considering the mechanical patterns of the knee prosthetic materials, such as deformation and surface contact behavior [9].
To reach this goal, Catani et al. [9] reported a technique using the in vivo 3D kinematics obtained from fluoroscopy as input for FE models in order to determinate the contact points between the femoral component and the insert in patients with TKA. This method was recently used by another study that combined the kinematic data carried out by dynamic fluoroscopy with FE models in order to investigate articular surface contacts, both at the condyles and at the post-cam [2].
As reported in the literature [4, 24], custom specific knee finite element models (FEM) has recently been developed, both in clinical applications and in the process of medical devices design [13, 23], to investigate native and replaced knee joint kinematics and kinetics [6, 15, 18]. These models represent a valid alternative to in-vivo or experimental assessments since they were able to provide results comparable to those two methods while maintaining lower cost in comparison [2, 9].
In this study, an innovative technique, combining dynamic RSA and patient-specific finite element models, was applied to analyze a group of 15 patients who underwent total knee arthroplasty with a cemented CR highly congruent MB TKA during the execution of a sit to stand from chair. Specifically, this technique utilized real in vivo 3D kinematics obtained from RSA dynamic as input data for finite element analyses of the prosthesis.
The aim of our study was to assess the kinematic data, Internal-External (IE) rotation and Antero-Posterior (AP) translation of the contact points between the femoral condyles and polyethylene insert, through a patient-specific FE model, based on a validated FE technique [9, 16]. The secondary purpose was to develop a combined dynamic RSA-FE model that give results congruent with the literature [7, 12, 29].
The hypothesis of the present study was that the kinematic data acquired by dynamic RSA may be used to evaluate the contact points translation at polyethylene-femoral component interface by finite element analysis obtaining results congruent with the literature.
Materials and methods
The patient recruitment, demographic data, study method, and kinematic data analyzed through dynamic RSA using in this work have been acquired according to the Ethics approval by Institutional Review Board (IRB) of XXX Institute (IRCCS) (ID: 0035595 October 22,2015), and have been already published [7].
Briefly, Cardinale et al. [7] randomly selected a cohort of 15 patients who underwent cemented CR highly congruent MB TKA (Gemini, Waldemar LINK GmbH & Co. KG, Barkhausenweg 10, 22,339 Hamburg, Germany) with patella resurfacing for primary osteoarthritis (OA). The evaluation was performed after a minimum nine-month follow-up using Model-based dynamic RSA in weight-bearing conditions and during the execution of a sit to stand from chair. The RSA methods and accuracy are previously published [1, 7, 21, 27].
The validated dynamic RSA method allows to measure with sub-millimetric accuracy [3] (average 0.2 mm, SD ± 0.5 mm for the model position, and 0.3° ± 0.2° for the model orientation), according to the ISO − 5725 regulation [30].
The kinematical data acquired thought Dynamic RSA were used as input for a patient-specific FE models, developed on the basis of a validated FE technique [9], to calculate condylar contact points between the femoral component and polyethylene insert. The first FE model of the femoral component and polyethylene insert was developed in Abaqus/Explicit version 2019 (Dassault Systèmes, Vélizy-Villacoublay, France) from the original CAD models of the implant provided by the manufacturer. Three size femoral components (CR2, CR3, CR5) were used and considered as a rigid surface and represented by triangular surface elements with 2 mm element size (*3233 elements for CR2, 3750 elements for CR3 and 4576 elements for CR5) (Fig. 1). The polyethylene insert was modelled by two fixed box and represented by eight-node 3D hexahedral elements. To create an element size variation from 2 mm (surface in contact with femoral component) to 10 mm, a single bias was applied in z-direction, obtaining 4400 elements for each box (Fig. 1).
Initially, the boxes were considered fixed, and the femoral component moved according to the in vivo relative kinematics obtained from RSA. Subsequently, to avoid excessive polyethylene deformation or lift-off between the femoral condyles and the insert, and to guarantee a constant penetration of 1 mm, the fixed boxes was replaced with movable boxes. Following previous model [2, 9], the latters were assumed to move in the superior-inferior direction together the femoral component using the superior-inferior displacement of the contact points calculated in the first analysis. No movement was allowed for the boxes in antero-posterior and medio-lateral direction.
Young’s modulus and Poisson ratio assumed for the femoral component, assumed linear elastic isotropic, were, respectively, 240 GPa and 0.3 [17]. The polyethylene insert was treated as a homogenous and isotropic material according to literature data [8, 16,17,18,19, 25].
The contact points were determined by the FE software as the centroid of the pressure distribution between the femoral condyles and the polyethylene insert [11].
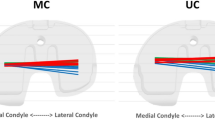
As output, for each patient, the IE rotation and the AP translation of the whole femoral component was calculated. Moreover, the AP displacement of the medial and lateral compartments, normalized with respect to prosthesis size, were evaluated and all kinematical results were plotted versus the knee flexion angle. All reported data, calculated for each patient, were evaluated starting from the same initial position, aligning the coordinate systems of femoral component and of polyethylene on z-axis (Fig. 2).
Results
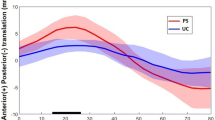
The AP translation (Fig. 3) showed that the femoral component started from a posterior position (− 2 mm ± 3.4 mm) at 80° of flexion, kept an almost constant position up to 40° and translate anteriorly during the last 40° of flexion. In average, the AP translation overall range during the whole motor task was about 4 mm.
Analysing the IE rotation plotted versus knee flexion, the femoral component started from an externally rotate position (− 6.7 ± 10°) at 80° of flexion and performed an internal rotation during the entire motor task (Fig. 4). The overall range of the IE rotation was 8.2°.
The normalized AP translation, reported as percentage value of the length of the prosthesis (Fig. 5), showed that both medial and lateral condyles started from posterior position and moved in anterior direction during the motor task. An almost constant offset of about 8% was observed between 80° and 40° of flexion. Later, the offset decreased between 40° and 0° of flexion (from 8% to 1%) bringing the AP position of both condyles almost at the same position in full extension. Analysing the overall AP translation and IE rotation ranges (Fig. 6), a greater motion in AP direction occurred in low flexion angle then in high ones. Whilst, the femoral component maintained an extra-rotated position from 80° to 40°, and performed an internal-rotation in the last degrees of flexion.
Discussion
The most important finding of the present study was that during the sit-to-stand, a slight anterior translation was observed from 40° to 0° of flexion in the femoral component with respect to polyethylene insert, which could represent a paradoxical anterior translation as reported in several studies [7, 12, 29].
The dynamic RSA technique allows to accurately investigate in-vivo the kinematical behavior of a total knee prosthesis analyzing the relative movement between femoral compartment and tibial plateau frame by frame. Instead, the FE analysis provides more information taking account both kinematical, kinetic and biomechanical behaviors. The innovative feature of the present study is the combination of dynamic RSA technique and finite element analysis. The reliability of a combined technique, finite element analysis and in vivo 3D fluoroscopic kinematics, was already tested and confirmed [2, 9].
The paradoxical anterior translation is an important and very common result that could be related to different factors and may cause implant instability. Analyzing the literature, higher AP translation could be led by a not congruent prosthesis design and by cruciate resection [20].
Based on these considerations, the slight AP range reported in this study could be associated to the high congruent design and to the anterior cruciate retaining, typical of the CR mobile bearing TKA [16].
Analyzing the normalized AP translation reported in Fig. 6, the femoral component performed a medial pivot movement during the whole task starting from an external rotation, coherently with the results reported in the literature [22].
As showed by results, a similar kinematical behavior was observed in all patients. Despite a paradoxical anterior femoral translation was detected, the implants showed a great stability. It could be related to the highly congruent polyethylene design.
Dynamic RSA and FE combined technique could provide information about prosthetic component’s stress and strain distribution and the influence of the different designs during the movement.
This study presents some limitations. Firstly, the number of patients is not enough large to produce strong evidence, although it is in line with similar studies [2, 7]. Secondly, all patients performed the sit-to stand motor task without standardisation not providing homogeneous data, but ensuring the most natural movement as possible. Finally, this study investigated only the extension phase of movement, not finding a good comparison with the literature where most of the studies that assessed in vivo kinematical patterns were focused on flexion movement.
Conclusion
During the sit-to-stand, a paradoxical anterior translation was detected, according to the literature. Dynamic RSA and FE combined technique could provide information about prosthetic component’s stress and strain distribution and the influence of the different designs during the movement.
An important outcome that should be analyzed is the success of the TKA during long time period and the influence of the mechanical behavior. For this reason, future studies will be focused on long term follow up and on other motor tasks.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PCL:
-
Posterior cruciate retaining
- OA:
-
Osteoarthritis
- CR:
-
Cruciate retaining
- MB:
-
Mobile bearing
- TKA:
-
Total knee arthroplasty
- RSA:
-
Roentgen stereophotogrammetric analysis
- FE:
-
Finite element
- FEM:
-
Finite element method
- IE:
-
Internal-external
- AP:
-
Anterior-Posterior
References
Alesi D, Marcheggiani Muccioli GM, Roberti di Sarsina T, Bontempi M, Pizza N, Zinno R, Di Paolo S, Zaffagnini S, Bragonzoni L (2020) In vivo femorotibial kinematics of medial-stabilized total knee arthroplasty correlates to post-operative clinical outcomes. Knee Surg Sports Traumatol Arthrosc 29(2):491–497. https://doi.org/10.1007/s00167-020-05975-w
Belvedere C, Leardini A, Catani F, Pianigiani S, Innocenti B (2017) In vivo kinematics of knee replacement during daily living activities: condylar and post-cam contact assessment by three-dimensional fluoroscopy and finite element analyses. J Orthop Res 35(7):1396–1403. https://doi.org/10.1002/jor.23405
Bontempi M, Cardinale U, Bragonzoni L, Marcheggiani Muccioli GM, Alesi D, di Matteo B, Marcacci M, Zaffagnini S (2020) A computer simulation protocol to assess the accuracy of a radio Stereometric analysis (RSA) image processor according to the ISO-5725. arXiv:2006.03913. [physics]. https://arxiv.org/abs/2006.03913
Bori E, Innocenti B (2020) Development and validation of an in-silico virtual testing rig for analyzing total knee arthroplasty performance during passive deep flexion: a feasibility study. Med Eng Phys 84:21–27. https://doi.org/10.1016/j.medengphy.2020.07.020
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ (2010) Patient satisfaction after Total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63. https://doi.org/10.1007/s11999-009-1119-9
Burastero G, Pianigiani S, Zanvettor C, Cavagnaro L, Chiarlone F, Innocenti B (2020) Use of porous custom-made cones for meta-diaphyseal bone defects reconstruction in knee revision surgery: a clinical and biomechanical analysis. Arch Orthop Trauma Surg 140(12):2041–2055. https://doi.org/10.1007/s00402-020-03670-6
Cardinale U, Bragonzoni L, Bontempi M, Alesi D, Roberti di Sarsina T, Lo Presti M, Zaffagnini S, Marcheggiani Muccioli GM, Iacono F (2020) Knee kinematics after cruciate retaining highly congruent mobile bearing total knee arthroplasty: an in vivo dynamic RSA study. Knee 27(2):341–347. https://doi.org/10.1016/j.knee.2019.11.003
Castellarin G, Pianigiani S, Innocenti B (2019) Asymmetric polyethylene inserts promote favorable kinematics and better clinical outcome compared to symmetric inserts in a mobile bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27(4):1096–1105. https://doi.org/10.1007/s00167-018-5207-9
Catani F, Innocenti B, Belvedere C, Labey L, Ensini A, Leardini A (2010) The mark Coventry award articular: contact estimation in TKA using in vivo kinematics and finite element analysis. Clin Orthop Relat Res 468(1):19–28. https://doi.org/10.1007/s11999-009-0941-4
Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ (2018) Three groups of dissatisfied patients exist after total knee arthroplasty: early, persistent, and late. Bone Joint J 100B(2):161–169. https://doi.org/10.1302/0301-620X.100B2.BJJ-2017-1016.R1
Dennis DA, Komistek RD, Colwell CE, Ranawat CS, Scott RD, Thornhill TS, Lapp MA (1998) In vivo anteroposterior Femorotibial translation of Total knee arthroplasty. Clin Orthop Relat Res 356:47–57. https://doi.org/10.1097/00003086-199811000-00009
Dennis DA, Komistek RD, Mahfouz MR (2003) In vivo fluoroscopic analysis of fixed-bearing Total knee replacements. Clin Orthop Relat Res 410:114–130. https://doi.org/10.1097/01.blo.0000062385.79828.72
Erdemir A, Guess TM, Halloran J, Tadepalli SC, Morrison TM (2012) Considerations for reporting finite element analysis studies in biomechanics. J Biomech 45(4):625–633. https://doi.org/10.1016/j.jbiomech.2011.11.038
Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR (2019) How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 393(10172):655–663. https://doi.org/10.1016/s0140-6736(18)32531-5
Harrysson OLA, Hosni YA, Nayfeh JF (2007) Custom-designed orthopedic implants evaluated using finite element analysis of patient-specific computed tomography data: femoral-component case study. BMC Musculoskelet Disord 8(1):91. https://doi.org/10.1186/1471-2474-8-91
Innocenti B (2019) High congruency MB insert design: stabilizing knee joint even with PCL deficiency. Knee Surg Sports Traumatol Arthrosc 28(9):3040–3047. https://doi.org/10.1007/s00167-019-05764-0
Innocenti B, Bori E (2020) Change in knee biomechanics during squat and walking induced by a modification in TKA size. J Orthop 22:463–472. https://doi.org/10.1016/j.jor.2020.10.006
Innocenti B, Pianigiani S, Ramundo G, Thienpont E (2016) Biomechanical effects of different Varus and valgus alignments in medial Unicompartmental knee arthroplasty. J Arthroplast 31(12):2685–2691. https://doi.org/10.1016/j.arth.2016.07.006
Innocenti B, Yagüe HR, Bernabé RA, Piangiani S (2015) Investigation on the effects induced by TKA features on tibio-femoral mechanics part I: femoral component designs. J Mech Med Biol 15(02):1540034. https://doi.org/10.1142/S0219519415400345
Kim TW, Lee SM, Seong SC, Lee S, Jang J, Lee MC (2016) Different intraoperative kinematics with comparable clinical outcomes of ultracongruent and posterior stabilized mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24(9):3036–3043. https://doi.org/10.1007/s00167-014-3489-0
Marcheggiani Muccioli GM, Pizza N, Di Paolo S, Zinno R, Alesi D, Roberti Di Sarsina T, Bontempi M, Zaffagnini S, Bragonzoni L (2020) Multi-radius posterior-stabilized mobile-bearing total knee arthroplasty partially produces in-vivo medial pivot during activity of daily living and high demanding motor task. Knee Surg Sports Traumatol Arthrosc 28(12):3773–3779. https://doi.org/10.1007/s00167-020-05846-4
Meccia B, Komistek RD, Mahfouz M, Dennis D (2014) Abnormal axial rotations in TKA contribute to reduced Weightbearing flexion. Clin Orthop Relat Res 472(1):248–253. https://doi.org/10.1007/s11999-013-3105-5
Mirulla AI, Di Paolo S, Di Simone F, Ingrassia T, Nigrelli V, Zaffagnini S, Bragonzoni L (2020) Biomechanical analysis of two types of osseointegrated transfemoral prosthesis. Appl Sci 10(22):1–16. https://doi.org/10.3390/app10228263
Piangiani S, Innocenti B (2015) The use of finite element modeling to improve biomechanical research on knee prosthesis. In: New developments in knee prosthesis research. Nova Science Publishers, Inc., pp 113–125
Pianigiani S, Bernabé RA, Yagüe HR, Innocenti B (2015) Investigation on the effects induced by TKA features on tibio-femoral mechanics part II: Tibial insert designs. J Mech Med Biol 15(02):1540035. https://doi.org/10.1142/S0219519415400357
Pitta M, Esposito CI, Li Z, Yu LY, Wright TM, Padgett DE (2018) Failure after modern Total knee arthroplasty: a prospective study of 18,065 knees. J Arthroplast 33(2):407–414. https://doi.org/10.1016/j.arth.2017.09.041
Pizza N, Di Paolo S, Zinno R, Marcheggiani Muccioli GM, Agostinone P, Alesi D, Bontempi M, Zaffagnini S, Bragonzoni L (2021) Over-constrained kinematic of the medial compartment leads to lower clinical outcomes after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06398-3
Postler A, Lützner C, Beyer F, Tille E, Lützner J (2018) Analysis of Total knee arthroplasty revision causes. BMC Musculoskelet Disord 19(1):55. https://doi.org/10.1186/s12891-018-1977-y
Yue B, Varadarajan KM, Rubash HE, Li G (2012) In vivo function of posterior cruciate ligament before and after posterior cruciate ligament-retaining total knee arthroplasty. Int Orthop 36(7):1387–1392. https://doi.org/10.1007/s00264-011-1481-6
ISO 5725-1:1994(en), Accuracy (trueness and precision) of measurement methods and results — Part 1: General principles and definitions. https://www.iso.org/obp/ui/#iso:std:iso:5725:-1:ed-1:v1:en. Accessed 7 Apr 2021
Acknowledgements
Maurilio Marcacci for the support to the research; Umberto Cardinale for the dynamic analysis of kinematics; Marco Bontempi for developing the RSA software;
Funding
Partially supported by Waldemar Link GmbH & Co. KG.
Author information
Authors and Affiliations
Contributions
A.I.M. participated in study design and data interpretation, drafted the manuscript; R.Z. participated in kinematics data collection and analysis, contributed to data interpretation, and helped to draft the manuscript; L.B. and S.Z. participated in study design, coordinated activities and helped to draft the manuscript; B.I. contributed to methods development and data interpretation, helped to draft the manuscript; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This FE study does not need a written informed consent by subject. However, all data used in this work refer to the Ethics approval by Institutional Review Board (IRB) of XXX Institute (IRCCS) (ID: 0035595 October 22,2015).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mirulla, A.I., Bragonzoni, L., Zaffagnini, S. et al. Assessment of paradoxical anterior translation in a CR total knee prosthesis coupling dynamic RSA and FE techniques. J EXP ORTOP 8, 50 (2021). https://doi.org/10.1186/s40634-021-00361-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-021-00361-y