Abstract
Background
Fluid resuscitation is fundamental in acute pancreatitis (AP) treatment. However, the optimal choice between normal saline (NS) and Ringer's solution (RS), and its impact on mortality in critically ill patients, remains controversial. This retrospective cohort study, utilizing a national Japanese inpatient database, investigates this question.
Methods
Using the Japanese Diagnosis Procedure Combination database between July 2010 and March 2021, we identified adult patients hospitalized in intensive care units (ICU) or high-dependency care units (HDU) for AP who survived at least three days and received sufficient fluid resuscitation (≥ [10 ml/kg/hr*1 h + 1 ml/kg/hr*71 h] ml) within three days of admission including emergency room infusions. Patients were classified into groups based on the predominant fluid type received: the NS group (> 80% normal saline) and the RS group (> 80% Ringer's solution). Propensity score matching was employed to reduce potential confounding factors and facilitate a balanced comparison of in-hospital mortality between the two groups.
Results
Our analysis included 8710 patients with AP. Of these, 657 (7.5%) received predominantly NS, and 8053 (92.5%) received predominantly RS. Propensity score matching yielded 578 well-balanced pairs for comparison.
The NS group demonstrated significantly higher in-hospital mortality than the RS group (12.8% [474/578] vs. 8.5% [49/578]; risk difference, 4.3%; 95% confidence interval, 0.3% to 8.3%).
Conclusions
In patients admitted to ICU or HDU with AP receiving adequate fluid resuscitation, RS can be a preferred infusion treatment compared to NS.
Similar content being viewed by others
Introduction
Acute pancreatitis (AP) is a common gastrointestinal disorder with significant healthcare costs exceeding 2.7 billion dollars annually in the United States alone [1]. Hospitalization rates are substantial, and despite an overall mortality of 2%, severe acute pancreatitis (SAP) carries a mortality rate nearing 20% and up to 30% in critically ill patients [2,3,4].
Early fluid replacement therapy is the cornerstone of AP management according to guidelines, with normal saline (NS) and Ringer's solution (RS) being the most commonly used solutions [5, 6]. While several systematic reviews and meta-analyses suggest potential advantages of RS in reducing local complications, severity, intensive care unit (ICU) admission, and pancreatic necrosis [7,8,9,10,11], its impact on mortality remains less clear. This lack of clarity may be due to the limited sample sizes of included randomized controlled trials (RCTs) or less severely ill patients [12,13,14,15,16].
To address this uncertainty, we conducted a study comparing in-hospital mortality in critically ill patients between AP patients treated with NS or RS, utilizing a large, nationwide Japanese inpatient database.
Methods
Study design and dataset
This retrospective cohort study employed a propensity score-matched (PSM) design to compare the clinical efficacy of different fluid resuscitation strategies in AP. We analyzed data from the Diagnosis Procedure Combination (DPC) database, a nationwide Japanese database containing discharge abstracts and administrative claims data from over 1200 acute-care hospitals [17]. This database provides the following patient-level data: age, sex, diagnoses (ICD-10 codes), daily procedures (Japanese medical procedure codes), daily drug administrations, and admission/discharge status. Previous validation studies demonstrate high specificity for diagnoses and procedures within this database [18]. The study was approved by the Institutional Review Board of The University of Tokyo (Approval number 3501-(5); May 19th, 2021).
Study population
The study period spanned from July 2010 to March 2021. We defined an ICU as a separate unit that provides critical care services, with at least one physician present on-site 24 h a day, round-the-clock nursing care, the necessary equipment to care for critically ill patients, and a nurse-to-patient ratio greater than 1:2. The definition of a high-dependency care unit (HDU) in our study was similar to that of an ICU, with the exception of the required nurse-to-patient ratio, which could be 1:3, 1:4, or 1:5. To identify patients admitted to ICU/HDU, we used specific Japanese medical procedure codes, which are listed in Supplemental Table 1.
The following exclusion criteria were applied:
-
1.
Lack of emergency admission status.
-
2.
Length of hospital stay ≤ 3 days.
-
3.
Inadequate fluid resuscitation (defined as < 10 ml/kg bolus over one hour followed by < 1 ml/kg/hour over the subsequent 71 h).
-
4.
Mixed fluid resuscitation strategy where neither NS nor RS accounted for at least 80% of the total fluids administered during hospitalization.
Treatment groups
Patients were classified based on the predominant type of external fluid administered within the first three days of admission:
-
NS Group: received NS for ≥ 80% of total fluid volume.
-
RS Group: received Ringer's lactate, Ringer's acetate, or Ringer's carbonate for ≥ 80% of total fluid volume.
Outcomes
-
Primary outcome: in-hospital mortality.
-
Secondary outcomes:
-
Development of SAP based on the Revised Atlanta Classification [18]. SAP is defined as persistent organ failure in one or more systems (cardiovascular, renal, respiratory).
-
ο
Persistent cardiovascular failure: requiring vasopressors/inotropes > 3 days.
-
ο
Persistent renal failure: requiring renal replacement therapy > 3 days.
-
ο
Persistent respiratory failure: requiring mechanical ventilation > 3 days.
-
ο
-
Intervention for necrotizing AP (necrosectomy or drainage for symptomatic walled-off necrosis (WON) or acute necrotic collection (ANC) during hospitalization; delayed interventions during re-hospitalization were excluded).
-
Length of hospital stay.
-
Length of ICU/HDU stay.
-
Total hospitalization costs (1 USD ≈ 110 JPY).
-
Covariates
We considered the following covariates for their potential impact on outcomes:
Patient characteristics
-
Age
-
Sex
-
Smoking history
-
Body mass index (BMI) at admission
-
Physical function (Barthel Index score at admission [19]
-
Level of consciousness (Japan Coma Scale score at admission [20]
-
Comorbidities (Charlson Comorbidity Index score and chronic renal disease).
Admission factors
-
Fiscal year
-
Weekend admission (Saturday or Sunday)
-
Ambulance use.
Disease and initial treatment factors
-
AP severity indicators (Japanese Ministry of Health, Labour and Welfare scoring system [21]
-
CT grade score (Japanese Ministry of Health, Labour and Welfare scoring system [22]
-
Ventilator use on arrival
-
Renal replacement therapy on arrival
-
Vasopressor/inotrope use on arrival.
Statistical analysis
PSM was employed to reduce bias and facilitate a balanced comparison of in-hospital mortality between the NS and RS groups [23]. Propensity scores were calculated using a multivariable logistic regression model where the treatment group assignment (NS vs. RS) was the dependent variable, and all covariates listed in Table 1 were independent variables. One-to-one nearest-neighbor matching without replacement was performed using a caliper width of 20% of the standard deviation of propensity scores [23]. Standardized differences were calculated to assess the balance of covariates, with absolute values ≤ 10% indicating negligible imbalance between groups [24]. After PSM, a generalized linear model compared outcomes between groups, accounting for clustering effects within individual hospitals. Differences and 95% confidence intervals (CIs) were calculated using the identity link function, regardless of outcome type.
Several sensitivity analyses were performed to assess the robustness of our findings:
-
1.
Dialysis exclusion: Analysis was repeated excluding patients receiving dialysis within the first day of admission, as their treatment may have favored the potassium-free NS.
-
2.
Inverse probability of treatment weighting (IPTW): IPTW analyses were conducted as an alternative to PSM, using stabilized weighting for greater precision and control over type I error.
-
3.
Fluid type proportion thresholds: Analyses were repeated for populations receiving > 70% and > 90% of their fluid volume as either NS or RS.
-
4.
Total fluid volume stratification: Analyses were performed after dividing patients into low-volume and high-volume fluid resuscitation groups, based on the median total fluid volume within the first three days of admission.
Results
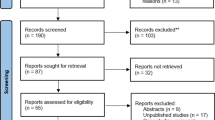
Out of 223,500 patients hospitalized for AP, 8,710 met the inclusion criteria after applying exclusions (Fig. 1). Of these, 657 (7.5%) received predominantly NS, and 8053 (92.5%) received predominantly RS. PSM yielded 578 well-balanced pairs (Table 1). Importantly, no significant differences were found in the total volume of fluid administered within the first three days between the NS and RS groups, both before and after PSM (Table 2).
Key findings after PSM
-
Mortality: The NS group had significantly higher in-hospital mortality than the RS group (12.8% vs. 8.5%; risk difference, 4.3%; 95% CI 0.3–8.3%).
-
Secondary outcomes: The NS group also demonstrated significantly worse outcomes in the SAP and persistent renal organ failure (Table 2, Fig. 2). No significant difference was found for persistent organ failure (cardiovascular and respiratory), intervention for necrotizing AP, length of hospital stay, length of ICU/HDU stay, total hospitalization costs.
Sensitive analysis
Dialysis-free patients subgroups
Excluding 247 patients receiving renal replacement therapy on admission, we still observed significantly higher in-hospital mortality in the NS group (11.5% vs. 5.9%; risk difference, 5.6%; 95% CI, 1.9–9.4%). Additional outcomes are presented in Supplementary Table 2 and Figure 2.
IPTW analysis
In the IPTW cohort, we found significantly higher in-hospital mortality for the NS group (8.5% vs. 3.8%; risk difference, 4.7%; 95% CI 2.2–7.2%). The NS group also showed significantly worse outcomes across most other endpoints, except intervention for necrotizing AP (Supplementary Table 3 and Figure 2).
Different fluid proportion thresholds
Sensitivity analyses using alternate definitions for predominant fluid use (> 70% and > 90% NS or RS) confirmed our main findings. Supplementary Tables 4 and 5 relay detailed results.
Fluid volume stratification
Dividing patients by low/high fluid resuscitation volume (median 6400 mL [5500–7300] and 10,600 mL [9250–13500], respectively), we found:
-
a.
Low-volume: NS group mortality 9.0% vs. 4.3% for RS (risk difference 4.7%; 95% CI 0.2%–9.2%, p = 0.04) after matching 256 patients per group (Supplementary Table 6).
-
b.
High-Volume: NS group mortality 15.9% vs. 11.7% for RS (risk difference 4.2%; 95% CI − 1.2–9.7%, p = 0.13) after matching 308 patients per group (Supplementary Table 7).
Discussion
The choice of fluid for treating AP remains a topic of ongoing debate, with previous research yielding mixed results [25, 26]. While RCTs and meta-analyses have not consistently demonstrated a mortality difference between NS and RS [7,8,9,10,11,12,13,14,15,16], our large-scale observational study suggests that using RS in adults admitted to ICU/HDU with AP may offer a significant survival benefit. We found a risk difference of 4.3% in favor of RS. Furthermore, our findings associate NS administration with a higher risk of developing SAP and persistent renal organ failure. Various sensitivity analyses also showed that the absolute differences for each outcome (mortality; 4.2–5.6%, SAP; 10.1–14.5%, and persistent renal organ failure; 9.6–14.6%) were in broad agreement.
Earlier RCTs investigating fluid choice in AP may have been underpowered to detect mortality differences due to their small sample sizes and the inclusion of less severely ill patients who may not have required ICU/HDU admission. [12,13,14,15,16]. Similarly, previous meta-analyses suggested improvements in certain outcomes but could not definitively establish a difference in mortality [7,8,9,10,11]. A recent meta-analysis reported lower mortality associated with RS, but only three patients died across the five included studies, and the results might be less reliable for adults due to the inclusion of both adult and pediatric studies [27].
We observed a high overall mortality rate in our study (12.8% with NS and 8.5% with RS) because we focused specifically on critically ill AP patients admitted to the ICU or HDU. Although a RCT would require approximately 1,126 total patients to confirm the 4.3% absolute mortality difference we observed (assuming 90% power and α = 0.05), our large-scale analysis utilizing 578 propensity score-matched pairs from a nationwide adult inpatient database provides compelling evidence that NS is associated with higher mortality compared to RS in the treatment of critically ill ICU/HDU patients with AP. SAP develops in about 20% of AP cases [28, 29], but our subject has a higher percentage of SAP with 40.1% with NS and 28.7% with RS because our analysis focused on critically ill ICU/HDU patients. Although the results of this study may be applicable to a limited number of subjects, the high incidence of AP, with over 280,000 hospitalizations annually in the US alone [1], and the substantial mortality difference suggest a significant clinical impact. Reducing the mortality rate of these severely ill patients could prevent a large number of deaths each year.
RS offers several potential advantages over NS in the management of AP, primarily due to its closer resemblance to the electrolyte and acid–base composition of plasma [30, 31]. RS contains calcium, which may reduce systemic inflammation by binding non-esterified fatty acids [32]. Additionally, the short-chain fatty acids found in RS may modulate inflammatory responses and promote anti-inflammatory pathways [13]. Furthermore, RS may improve renal blood flow and counter chloride-mediated vasoconstriction, potentially offering protection against acute kidney injury compared to NS [32–34]. Our study consistently found RS to be associated with significantly lower persistent renal failure, supporting this mechanism. While NS has advantages in volume expansion and lower cost, these are most relevant in cases of hypovolemic shock. In patients with AP experiencing distributive shock, RS appears to be the superior choice [7,8,9,10,11].
It is important to acknowledge the limitations of our retrospective observational study, primarily the potential for confounding due to the lack of randomization, as fluid choice was at the provider’s discretion and could be influenced by patient characteristics. To address these shortcomings, we employed propensity score matching and several sensitivity analyses, and our consistent results strengthen the reliability of our findings. However, unmeasured confounders, such as catecholamine dosage data and renal failure developed after hospitalization, may persist. Despite these limitations, our findings suggest a potential benefit associated with RS use in AP management. In Japan, while NS use for AP is decreasing, it is still being administered. Given the ease of switching between RS and NS, alongside their cost parity, a shift towards RS could translate to meaningful improvements in patient outcomes on a large scale.
Conclusion
Adults hospitalized to ICU or HDU for AP who received adequate volumes of NS for fluid resuscitation experienced higher in-hospital mortality compared to those treated with RS. These results align with studies demonstrating RS's potential to reduce complications and improve outcomes. While a large RCT would be ideal to confirm these findings, it may face challenges due to the required sample size and relatively low mortality rates in AP. Considering the observed benefits, ease of implementation, and cost parity between the solutions, RS may be considered the preferred fluid choice in managing adult ICU or HDU patients with AP.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AP:
-
Acute pancreatitis
- HDU:
-
High-dependency care unit
- NS:
-
Normal saline
- RS:
-
Ringer's solution
- ICU:
-
Intensive care unit
- SAP:
-
Severe acute pancreatitis
- CI:
-
Confidence interval
References
Peery AF, Crockett SD, Murphy CC, Lund JL, Dellon ES, Williams JL, Jensen ET, Shaheen NJ, Barritt AS, Lieber SR, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2018. https://doi.org/10.1053/j.gastro.2018.08.063.
Forsmark CE, Vege SS, Wilcox CM. Acute pancreatitis. N Engl J Med. 2016;375(20):1972–81.
Mederos MA, Reber HA, Girgis MD. Acute pancreatitis: a review. JAMA. 2021;325(4):382–90.
Schepers NJ, Bakker OJ, Besselink MG, Ahmed Ali U, Bollen TL, Gooszen HG, van Santvoort HC, Bruno MJ, Dutch Pancreatitis Study G. Impact of characteristics of organ failure and infected necrosis on mortality in necrotising pancreatitis. Gut. 2019;68(6):1044–51.
Tenner S, Baillie J, DeWitt J, Vege SS. American college of gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108(9):1400–15.
Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN, American Gastroenterological Association Institute Clinical Guidelines C. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology. 2018;154(4):1096–101.
Aziz M, Ahmed Z, Weissman S, Ghazaleh S, Beran A, Kamal F, Lee-Smith W, Assaly R, Nawras A, Pandol SJ, et al. Lactated Ringer’s vs normal saline for acute pancreatitis: An updated systematic review and meta-analysis. Pancreatology. 2021;21(7):1217–23.
Zhou S, Buitrago C, Foong A, Lee V, Dawit L, Hiramoto B, Chang P, Schilperoort H, Lee A, de-Madaria E, et al. Comprehensive meta-analysis of randomized controlled trials of Lactated Ringer’s versus normal saline for acute pancreatitis. Pancreatology. 2021;21(8):1405–10.
Vedantam S, Tehami N, de Madaria E, Barkin JA, Amin S. Lactated ringers does not reduce SIRS in acute pancreatitis compared to normal saline: an updated meta-analysis. Digestive Dis Sci. 2022;67(7):3265–74.
Chen H, Lu X, Xu B, Meng C, Xie D. Lactated Ringer solution is superior to normal saline solution in managing acute pancreatitis: an updated meta-analysis of randomized controlled trials. J Clin Gastroenterol. 2022;56(2):e114–20.
Kow CS, Burud IAS, Hasan SS. Fluid resuscitation with lactated Ringer’s solution versus normal saline in acute pancreatitis: a systematic review and meta-analysis of randomized trials. Pancreas. 2022;51(7):752–5.
Wu BU, Hwang JQ, Gardner TH, Repas K, Delee R, Yu S, Smith B, Banks PA, Conwell DL. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9(8):710-717 e711.
de Madaria E, Herrera-Marante I, Gonzalez-Camacho V, Bonjoch L, Quesada-Vazquez N, Almenta-Saavedra I, Miralles-Macia C, Acevedo-Piedra NG, Roger-Ibanez M, Sanchez-Marin C, et al. Fluid resuscitation with lactated Ringer’s solution vs normal saline in acute pancreatitis: a triple-blind, randomized, controlled trial. United Eur Gastroenterol J. 2018;6(1):63–72.
Choosakul S, Harinwan K, Chirapongsathorn S, Opuchar K, Sanpajit T, Piyanirun W, Puttapitakpong C. Comparison of normal saline versus lactated Ringer’s solution for fluid resuscitation in patients with mild acute pancreatitis, A randomized controlled trial. Pancreatology. 2018;18(5):507–12.
Kayhan S, Selcan Akyol B, Ergul M, Baysan C. The effect of type of fluid on disease severity in acute pancreatitis treatment. Eur Rev Med Pharmacol Sci. 2021;25(23):7460–7.
Karki B, Thapa S, Khadka D, Karki S, Shrestha R, Khanal A, Shrestha R, Paudel BN. Intravenous Ringers lactate versus normal saline for predominantly mild acute pancreatitis in a Nepalese Tertiary Hospital. PLoS ONE. 2022;17(1): e0263221.
Yasunaga H. Real world data in Japan: chapter II the diagnosis procedure combination database. Ann Clin Epidemiol. 2019;1(3):76–9.
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol. 2017;27(10):476–82.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–5.
Shigematsu K, Nakano H, Watanabe Y. The eye response test alone is sufficient to predict stroke outcome–reintroduction of Japan Coma Scale: a cohort study. BMJ Open. 2013. https://doi.org/10.1177/2050640616670566.
Ikeura T, Horibe M, Sanui M, Sasaki M, Kuwagata Y, Nishi K, Kariya S, Sawano H, Goto T, Hamada T, et al. Validation of the efficacy of the prognostic factor score in the Japanese severity criteria for severe acute pancreatitis: a large multicenter study. United European gastroenterology journal. 2017;5(3):389–97.
Kitamura K, Horibe M, Sanui M, Sasaki M, Yamamiya A, Ishii Y, Yoshida H, Sawano H, Goto T, Ikeura T, et al. The prognosis of severe acute pancreatitis varies according to the segment presenting with low enhanced pancreatic parenchyma on early contrast-enhanced computed tomography: a multicenter cohort study. Pancreas. 2017;46(7):867–73.
Rosenbaum PR, Rubin DB. Constructing a control-group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39(1):33–8.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107.
Haydock MD, Mittal A, Wilms HR, Phillips A, Petrov MS, Windsor JA. Fluid therapy in acute pancreatitis: anybody’s guess. Ann Surg. 2013;257(2):182–8.
Yamashita T, Horibe M, Sanui M, Sasaki M, Sawano H, Goto T, Ikeura T, Hamada T, Oda T, Yasuda H, et al. Large volume fluid resuscitation for severe acute pancreatitis is associated with reduced mortality: a multicenter retrospective study. J Clin Gastroenterol. 2019;53(5):385–91.
Ocskay K, Matrai P, Hegyi P, Parniczky A. Lactated Ringer’s solution reduces severity, mortality, systemic and local complications in acute pancreatitis: a systematic review and meta-analysis. Biomedicines. 2023;11(2):321.
van Dijk SM, Hallensleben NDL, van Santvoort HC, Fockens P, van Goor H, Bruno MJ, Besselink MG, Dutch Pancreatitis Study G. Acute pancreatitis: recent advances through randomised trials. Gut. 2017;66(11):2024–32.
Working Group IAPAPAAPG. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13(4 Suppl 2):e1-15.
Scheingraber S, Rehm M, Sehmisch C, Finsterer U. Rapid saline infusion produces hyperchloremic acidosis in patients undergoing gynecologic surgery. Anesthesiology. 1999;90(5):1265–70.
Semler MW, Rice TW. Saline is not the first choice for crystalloid resuscitation fluids. Crit Care Med. 2016;44(8):1541–4.
Khatua B, Yaron JR, El-Kurdi B, Kostenko S, Papachristou GI, Singh VP. Ringer’s lactate prevents early organ failure by providing extracellular calcium. J Clin Med. 2020;9(1):263.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and design: MH, YM and EI; analysis and interpretation of the data: MH, AK, HO, HM and HY; software and visualization: AK; drafting of the article: MH, YM, HO and FB; critical revision of the article for important intellectual content: HY, EI and TK; final approval of the article: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of The University of Tokyo approved this study (approval number 3501-(5); May 19th, 2021).
Consent for publications
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Horibe, M., Kayashima, A., Ohbe, H. et al. Normal saline versus Ringer’s solution and critical-illness mortality in acute pancreatitis: a nationwide inpatient database study. j intensive care 12, 27 (2024). https://doi.org/10.1186/s40560-024-00738-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-024-00738-y