Abstract
Background
Extracorporeal membrane oxygenation (ECMO) is a rescue therapy in patients with severe acute respiratory distress syndrome (ARDS) secondary to COVID-19. While bleeding and thrombosis complicate ECMO, these events may also occur secondary to COVID-19. Data regarding bleeding and thrombotic events in COVID-19 patients on ECMO are sparse.
Methods
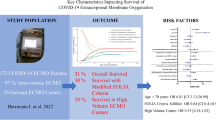
Using the COVID-19 Critical Care Consortium database, we conducted a retrospective analysis on adult patients with severe COVID-19 requiring ECMO, including centers globally from 01/2020 to 06/2022, to determine the risk of ICU mortality associated with the occurrence of bleeding and clotting disorders.
Results
Among 1,248 COVID-19 patients receiving ECMO support in the registry, coagulation complications were reported in 469 cases (38%), among whom 252 (54%) experienced hemorrhagic complications, 165 (35%) thrombotic complications, and 52 (11%) both. The hazard ratio (HR) for Intensive Care Unit mortality was higher in those with hemorrhagic-only complications than those with neither complication (adjusted HR = 1.60, 95% CI 1.28–1.99, p < 0.001). Death was reported in 617 of the 1248 (49.4%) with multiorgan failure (n = 257 of 617 [42%]), followed by respiratory failure (n = 130 of 617 [21%]) and septic shock [n = 55 of 617 (8.9%)] the leading causes.
Conclusions
Coagulation disorders are frequent in COVID-19 ARDS patients receiving ECMO. Bleeding events contribute substantially to mortality in this cohort. However, this risk may be lower than previously reported in single-nation studies or early case reports.
Trial registration ACTRN12620000421932 (https://covid19.cochrane.org/studies/crs-13513201).
Clinical Perspective
-
Coagulation disorders such as thrombotic or hemorrhagic events are frequent in COVID-19 ARDS patients receiving ECMO.
-
While older age, pre-existing cardiac disease, and diabetes were independently associated with bleeding, prone positioning and a longer time from admission to ECMO were associated with a higher percentage of thrombotic events.
-
A longer duration of ECMO was linked to an increased rate of combined hemorrhagic and thrombotic events.
Similar content being viewed by others
Background
Extracorporeal membrane oxygenation (ECMO) is a cardiopulmonary support technique that can be lifesaving in patients suffering from severe respiratory and/or circulatory failure [1,2,3]. However, ECMO exposes patients to complications such as bleeding and thrombosis [4,5,6]. Coagulation disorders in critically ill patients supported with ECMO result from a complex interplay between the underlying illness and both ECMO-related (e.g., shear stress, artificial circuit surface–blood interaction) and iatrogenic factors (e.g., systemic anticoagulation) [7,8,9]. These complications are associated with increased morbidity and mortality [5, 10]. However, the mechanisms behind coagulation disorders during ECMO are not yet fully understood, and prevention strategies are lacking.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus causing coronavirus disease-2019 (COVID-19), can result in acute respiratory distress syndrome (ARDS) requiring intensive care unit (ICU) admission and advanced respiratory failure management [11, 12]. Despite optimal medical management, including mechanical ventilation and prone positioning, mortality and morbidity rates due to refractory respiratory failure among these patients are high [13, 14]. A rescue therapy in these patients is ECMO [15, 16]. The mechanisms and clinical implications of thrombotic and hemorrhagic events in COVID-19 patients supported with ECMO are areas of ongoing research. This study aimed to define the global frequency, outcomes of, and risk factors for thrombotic and hemorrhagic disorders in COVID-19 patients with refractory ARDS supported with ECMO.
Methods
All data for this study were extracted from the global COVID-19 Critical Care Consortium (CCCC) prospective database, which was established to collect and analyze data on patients admitted to intensive care units for the treatment of severe COVID-19 [17]. The rationale and design have been previously published (Trial registration ACTRN12620000421932) [17]. Institutional Review Board (IRB) approval was obtained for each participating institution. A waiver of informed consent was granted for all patients. Additional file 1: Table S1 summarizes all the recruiting sites, including IRB approvals, contributors, and collaborators.
The CCCC database was examined for patients referred to the ICUs of 229 collaborating institutions spanning 32 countries, from January 1, 2020, through June 30, 2022. Patients who satisfied all the following criteria were entered into the registry: (1) age ≥ 16 years; (2) COVID-19 pneumonia with laboratory confirmation (real-time PCR and/ or next-generation sequencing); and (3) admission to ICU due to severe COVID-19 pneumonia. Patients admitted to critical care for conditions unrelated to COVID-19 were excluded.
Data were collected from ICU admission to either in-hospital death or hospital discharge. Data collection followed guidelines for the International Severe Acute Respiratory IncideNce sTudy of Severe Acute and Emerging Infection Consortium (ISARIC), Short-Period Incidence Study for Severe Acute Respiratory Infection (SPRINT-SARI), and the CCCC. All data obtained were de-identified and stored at a Research Electronic Data Capture (REDCap) database hosted at one of the following institutions: Oxford University, United Kingdom; University College Dublin, Ireland; or Monash University, Australia.
According to the ISARIC and the Extracorporeal Membrane Oxygenation for 2019 novel Coronavirus Acute Respiratory Distress Disease (ECMOCARD study) case report forms (CRF), adverse coagulation events included (1) thrombotic events including ischemic stroke, myocardial ischemia, myocardial infarction, deep vein thrombosis (DVT), and pulmonary embolism (PE); (2) hemorrhagic events were classified according to the bleeding site or the two predominant bleeding sources, in cases involving multiple bleeding sites; and (3) disseminated intravascular coagulation (DIC). Adverse coagulation events were diagnosed by treating physicians. The study focused on the following four patient groups treated with ECMO: (1) patients without hemorrhage or thrombosis (controls); (2) patients with both a hemorrhagic and thrombotic event; (3) patients with a hemorrhagic event only; and (4) patients with a thrombotic event only.
The study's primary outcome was mortality in COVID-19 patients supported with ECMO who suffered thrombotic and bleeding events. Secondary outcomes were the incidence of thrombotic and bleeding complications and the duration of ICU requirement (days). Additionally, we investigated risk factors for hemorrhagic or thrombotic events in COVID-19 patients on ECMO. Laboratory assessments were obtained according to the CRFs. ‘First value’ refers to a specific parameter's first recorded value in the CRFs. Minimum and maximum values are the minimum/maximum level of a parameter from enrolling in the study throughout the follow-up period.
Statistical analysis
The study cohort was limited to patients who were treated with ECMO. Patients without thrombotic or hemorrhagic complications were compared to the following subgroups: patients with a hemorrhagic event only, a thrombotic event only, or a combination of hemorrhagic and thrombotic events. Demographic characteristics, medical history, critical care treatment, and outcomes were described and checked for missing data (Additional file 1: Table S2). Continuous data were summarized as mean with standard deviation or median with interquartile range. Categorical variables were summarized as frequency count and percentage. Differences between groups were evaluated using Pearson's chi-squared test for categorical variables and the Wilcoxon–Mann–Whitney U test for continuous variables.
Survival analysis was used to estimate the effect of coagulation complications (combined and for thrombotic and hemorrhagic complications separately) on the time between ICU admission and mortality. The survival analysis cohort was limited to patients with non-missing discharge status and a valid ICU discharge date. The effect of coagulation complications on the instantaneous mortality hazard was estimated using Cox regression, assuming patients ‘discharged alive’ (alive, home, palliative care, hospitalized, or transferred to another facility) were censored independently. The proportional hazards assumption was verified with log–log plots and a test of Schoenfeld residuals. Parametric Weibull regression also was performed as a sensitivity analysis. Each survival analysis method was used to produce crude estimates and estimates adjusted a priori for patient age, sex, body mass index (BMI), and country of hospitalization. Due to a large proportion of missing BMI data, all analyses were repeated without adjusting for BMI. Regression results were presented as hazard ratios with 95% confidence intervals and p values.
Analysis was performed in SAS 9.4 (SAS Institute Inc., Cary, NC, USA), apart from survival analyses performed in Stata 15 (StataCorp, College Station, TX, USA).
Results
During the study period, 1,248 patients receiving VV- or VA-ECMO support due to COVID-19-related critical illness were included in the CCCC database. Table 1 summarizes baseline patient characteristics, including pre-existing health and management conditions. A hemorrhagic or thrombotic event was documented in 469 (38%). Among these 469 patients, 52 (11%) experienced at least one hemorrhagic and one thrombotic complication, while 252 (54%) patients experienced a hemorrhagic event only and 165 (35%) a thrombotic event only (Fig. 1),
Outcomes and causes of death
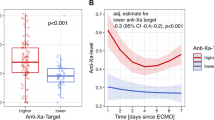
The adjusted hazard ratio (HR) for ICU mortality was higher among patients who experienced only a hemorrhagic complication than in patients who had neither type of complication (adjusted HR = 1.60, 95% CI 1.28–1.99, p < 0.001, Table 2). No statistically significant differences in ICU mortality were observed in patients with both types of complication (adjusted HR = 1.02, 95% CI 0.67–1.57, p = 0.918) or thrombotic events only (adjusted HR 0.79, 95% CI 0.59–1.05, p = 0.103) relative to patients with neither type of complication. Figure 2 depicts the survival of COVID-19 patients supported with ECMO over time in the four study groups.
The length of stay (days) within the ICU was longer for patients with both types of complication (42.0 days, 27.5–52.5, p = 0.009) and for those with a thrombotic event only (37.0 days, 24.0–57.0, p = 0.010) than in patients with neither type of complication (30.0 days, 17.0–52.0). Hospital length of stay was longer for those with both types of complication (45.0 days, 29.0–72.0, p = 0.017) and those with thrombotic events (44.0 days, 26.0–69.0, p = 0.003), but shorter among those with hemorrhagic events (28.0 days, 14.0–50.0, p = 0.001) compared to patients with neither type of complication (35.0 days, 19.0–59.0).
Overall, 617 of 1248 patients (49.4%) died in the ICU. The leading cause of death was multiorgan failure (257, 42%), followed by respiratory failure (130, 21%) and septic shock (55, 8.9%) (Table 3).
Coagulation complications (Table 4)
Thrombotic complications were documented in 217 (17.4%) of the 1248 patients with pulmonary embolism being the most common (n = 86 or 39.6%). Hemorrhagic complications occurred in 304 (24%) of all patients with the most common source being gastrointestinal (112, 36.8%). Note that bleeding severity was not part of the case report forms and, therefore, cannot be commented on.
The most common anticoagulation prophylaxis method was unfractionated heparin (UFH), followed by low molecular weight heparin (LMWH). Other anticoagulation strategies were rarely used (Table 5). Table 6 summarizes laboratory assessments.
Advanced ARDS management and ECMO
Clinical management of COVID-19 patients supported with ECMO is shown in Table 5, while Additional file 1: Table S3 provides ECMO specific data. Prone positioning during mechanical ventilation was more common in patients with thrombotic events than in controls (111, 81% vs. 354, 69%, p = 0.006). Furthermore, in patients with both types of complication (36/52, 71%, p = 0.004) as well as in patients with just a thrombotic event (112/165, 69%, p < 0.001), tracheostomy was more commonly performed than in controls (289/779, 50%).
Most patients received venovenous (864, 93.8%) rather than venoarterial ECMO (57, 6.2%). Time to admission for ECMO was statistically longer for patients with thrombotic events than in controls (p = 0.043). Duration of ECMO support also was statistically longer among patients with both complication types (p = 0.015). Maximum and mean daily ECMO blood flow was significantly less in patients with only thrombotic events than in patients with either hemorrhage events only, as well as among those with either, both, or neither type of complication (maximum daily blood flow p = 0.010, mean daily blood flow rate p = 0.015). However, there was no statistically significant difference in mean daily blood flow rates once adjusted for patient body weight. Circuit changes were most frequent in patients with both types of complications (26%), followed by those with hemorrhage complications (22%) and those with neither type of complication (16%). The incidence of any circuit change was the least frequent in patients with a thrombotic event (12%).
When considering venovenous ECMO only, we found a higher adjusted HR for ICU mortality for patients with hemorrhagic complications (adjusted HR 1.42, 95% CI 1.10–1.84, p = 0.008) compared to those without either type of complication. In contrast to the entire cohort, we observed a statistically significant reduction in HR for ICU mortality for venovenous ECMO patients with thrombotic complications only (HR, 0.64, 95% CI 0.46–0.89, p = 0.008) compared to venovenous ECMO patients without either type of complication (Table 2).
International comparison
This study involved participants mainly from the United States (n = 354), Colombia (n = 215), Spain (n = 140), Italy (n = 140), Kuwait (n = 126) and Australia (n = 12). Mortality was highest in Italy (64%), lowest in Australia (33%), and comparable (47–56%) among the other countries. However, ICU length of stay was not significantly different between regions. Table 7 summarizes further parameters by the host nation.
Discussion
In this international registry, we found that coagulation-related complications occurred in 38% of patients with severe COVID-19 requiring ECMO (hemorrhagic 20.2%; thrombotic 13.2%, and both < 5%). Hemorrhagic events were associated with increased mortality, whereas thrombotic events, alone or combined with hemorrhagic events, did not significantly impact mortality. In a recent study by Mansour et al., 66% of 620 critically ill COVID-19 patients receiving ECMO in France experienced coagulation disorders: 29% had bleeding, 16% thrombotic events, and 20% had both. Compared to this French cohort, our global CCCC study observed a lower incidence of bleeding and combined complications, with thrombotic events being comparable (13.2 vs. 16%). Differences in the choice of anticoagulant agent and/or the therapeutic target level might have contributed to the lower rate of bleeding events we observed in CCCC registry patients. Another potential explanation for the difference in the incidence of bleeding events might be how bleeding events were defined and captured. Nevertheless, both our study and that of Mansour et al. identified an association between coagulation disorders and increased mortality.
Within our population, those experiencing only hemorrhagic but not thrombotic event (alone or in combination) experienced a greater hazard of ICU mortality. This might be due to the high rates of mortality associated with certain types of bleeding, such as intracranial hemorrhage and severe bleeding requiring massive transfusion. Our finding of a reduced hazard of ICU mortality for patients experiencing thrombotic events contrasts with the reports of patients requiring ECMO due to non-Covid-19 conditions who undergo thrombosis. This might either be due to the differences of prothrombotic tendencies of different COVID-19 phenotypes or to the already increased risk of thrombosis resulting from prolonged critical care. Unfortunately, due to missing data, we could not adjust our survival analysis for other factors that might have contributed to mortality in this group. Therefore, though hypothesis generating, our mortality findings should be interpreted with caution.
In our cohort, multi-organ as well as respiratory failure and septic shock were the leading causes of death. This mirrors results reported by Peek et al. in 2009, who found that multi-organ failure accounted for 42% of the deaths in patients treated with ECMO [18]. Death due to hemorrhagic shock or cerebrovascular events was rare, even though bleeding was identified as a risk factor for mortality. Ischemic stroke and cerebrovascular accidents, generally considered frequent causes of permanent impairment after ECMO, occurred in nine patients in our study (4.1% among patients with a thrombotic event and 0.72% of the entire cohort), which is comparable to the incidence of stroke in a non-COVID ECMO group investigated in the EOLIA trial [2].
Our study identified several factors independently associated with coagulation disorders: older age, pre-existing cardiac disease, and diabetes were associated with bleeding events, while White ethnicity was associated with an increased risk of all coagulation disorders. Extended ECMO duration was associated with an increased incidence of bleeding but not thrombotic events, diverging from past reports in both in COVID and non-COVID patient populations. Longer mechanical ventilation was associated with both thrombotic and combined complications, but not with bleeding events alone. Both prone positioning during mechanical ventilation and longer time from admission to ECMO were associated with a higher incidence of thrombotic events. This aligns with Gebhard et al.’s 2021 study, which found extended prone positioning increased DVT risk in a small cohort [19]. These findings suggest a need for vigilance and close monitoring for thrombosis in ECMO patients undergoing prone positioning, awaiting further studies to clarify this relationship.
Subcutaneous administration of anticoagulation was associated with thrombotic complications (both combined and individual), suggesting that this route might not be suitable for preventing thrombosis in COVID-19 ECMO patients. This finding contrasts with Wiegele et al.’s single-center study, where ECMO patients treated with subcutaneous enoxaparin experienced fewer thrombotic or major bleeding events than those receiving unfractionated heparin [20].
Blood product transfusion was frequent in patients with either or both complications. Transfusion of packed red blood cells was independently associated with both forms of complication (alone or combined). However, platelets, fresh frozen plasma, and cryoprecipitate transfusions occurred more in patients with bleeding events, regardless of whether they were combined with thrombotic complications, but not in patients with only thrombotic events.
Strengths and limitations
This study has several limitations, including missing data and the retrospective nature of data extraction. Despite using standardized case report forms to minimize variations in data reporting, data entry depended on the discretion of physicians and research staff at each participating center and consequently, data completeness was heterogeneous. In addition, variability in ECMO and critical care management across centers, coupled with the voluntary nature of site participation, may have skewed representation to those with sufficient resources to enter the data. This variability hinders the precise assessment of potentially outcome-impacting factors such as the anticoagulation practices and ECMO management protocols.
On the other hand, extensive international collaboration offers valuable insights into thrombotic and bleeding events in COVID-19 ECMO patients globally. The pandemic’s evolving nature and the consequent adaptations in patient management strategies across different COVID waves add complexity to our analysis, particularly as our data collection tools could not be updated to reflect these changes, omitting potentially significant factors like immunomodulatory treatments and vaccination impacts on thrombotic and hemorrhagic complications. Additionally, the case report forms did not define bleeding severity, which might have led to heterogeneous reporting of bleeding events.
Notably, our study found no link between thrombotic events and mortality, possibly due to the lack of a detailed thrombosis severity assessment and the inclusion of minor thrombotic events. Future research should aim for clear definitions and severity grading of hemorrhagic and thrombotic events to enhance understanding and management of these complications.
Conclusions
In an international registry for critically ill COVID-19 patients receiving ECMO, the incidence of bleeding and thrombotic complications were high, albeit lower than previously reported. Bleeding significantly elevated mortality risk, with multi-organ failure and sepsis as the primary causes of death. Factors such as older age and White ethnicity were associated with an increased incidence of bleeding. Extended ECMO duration corresponded with higher bleeding rates but did not affect the occurrence of thrombotic events.
Availability of data and materials
The datasets used and/ or analyzed during the current study are available from the corresponding author in reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- BMI:
-
Body mass index
- CCCC:
-
COVID critical care consortium
- DIC:
-
Disseminated intravascular coagulation
- DVT:
-
Deep vein thrombosis
- ECMO:
-
Extracorporeal membrane oxygenation
- ICU:
-
Intensive care unit
- ISARIC:
-
International severe acute respiratory and emerging infection consortium
- LMWH:
-
Low molecular weight heparin
- PCR:
-
Polymerase chain reaction
- PE:
-
Pulmonary embolism
- REDCap:
-
Research electronic data capture
- SARS-CoV2:
-
Severe acute respiratory syndrome coronavirus 2
- SPRINT-SARI:
-
Short-period incidence study of severe acute respiratory infection
- UFH:
-
Unfractionated heparin
References
Brodie D, Slutsky AS, Combes A. Extracorporeal life support for adults with respiratory failure and related indications: a review. JAMA. 2019;322(6):557–68.
Combes A, Hajage D, Capellier G, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–75.
Combes A, Price S, Slutsky AS, Brodie D. Temporary circulatory support for cardiogenic shock. Lancet. 2020;396(10245):199–212.
Dalton HJ, Reeder R, Garcia-Filion P, et al. Factors associated with bleeding and thrombosis in children receiving extracorporeal membrane oxygenation. Am J Respir Crit Care Med. 2017;196(6):762–71.
Nunez JI, Gosling AF, O’Gara B, et al. Bleeding and thrombotic events in adults supported with venovenous extracorporeal membrane oxygenation: an ELSO registry analysis. Intensive Care Med. 2022;48(2):213–24.
Trudzinski FC, Minko P, Rapp D, et al. Runtime and aPTT predict venous thrombosis and thromboembolism in patients on extracorporeal membrane oxygenation: a retrospective analysis. Ann Intensive Care. 2016;6(1):66.
Doyle AJ, Hunt BJ. Current understanding of how extracorporeal membrane oxygenators activate haemostasis and other blood components. Front Med. 2018;5:352.
Xu LC, Bauer JW, Siedlecki CA. Proteins, platelets, and blood coagulation at biomaterial interfaces. Colloids Surf B Biointerfaces. 2014;124:49–68.
Seelhammer TG, Bohman JK, Schulte PJ, Hanson AC, Aganga DO. Comparison of bivalirudin versus heparin for maintenance systemic anticoagulation during adult and pediatric extracorporeal membrane oxygenation. Crit Care Med. 2021;49(9):1481–92.
Zangrillo A, Landoni G, Biondi-Zoccai G, et al. A meta-analysis of complications and mortality of extracorporeal membrane oxygenation. Crit Care Resusc. 2013;15(3):172–8.
Cui X, Zhao Z, Zhang T, et al. A systematic review and meta-analysis of children with coronavirus disease 2019 (COVID-19). J Med Virol. 2021;93(2):1057–69.
Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan. China JAMA Intern Med. 2020;180(7):934–43.
Lim ZJ, Subramaniam A, Ponnapa Reddy M, et al. Case fatality rates for patients with COVID-19 requiring invasive mechanical ventilation. A meta-analysis. Am J Respir Crit Care Med. 2021;203(1):54–66.
Zaaqoq AM, Barnett AG, Heinsar S, et al. Prone position during venovenous extracorporeal membrane oxygenation: survival analysis needed for a time-dependent intervention. Crit Care. 2022;26(1):39.
Supady A, Combes A, Barbaro RP, et al. Respiratory indications for ECMO: focus on COVID-19. Intensive Care Med. 2022;48(10):1326–37.
Ramanathan K, Shekar K, Ling RR, et al. Extracorporeal membrane oxygenation for COVID-19: a systematic review and meta-analysis. Crit Care. 2021;25(1):211.
Li Bassi G, Suen J, Barnett AG, et al. Design and rationale of the COVID-19 Critical Care Consortium international, multicentre, observational study. BMJ Open. 2020;10(12): e041417.
Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374(9698):1351–63.
Gebhard CE, Zellweger N, Gebhard C, et al. Prone positioning as a potential risk factor for deep vein thrombosis in COVID-19 patients: a hypothesis generating observation. J Clin Med. 2021;11(1):103.
Wiegele M, Laxar D, Schaden E, et al. Subcutaneous enoxaparin for systemic anticoagulation of COVID-19 patients during extracorporeal life support. Front Med. 2022;9: 879425.
Acknowledgements
We recognize the crucial importance of the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) and Short Period Incidence Study of Severe Acute Respiratory Infection (SPRINT-SARI) networks in developing and expanding the global Coronavirus Disease 2019 Critical Care Consortium (COVID-19– CCC). We thank the generous support we received from the Extracorporeal Life Support Organization and the International Extracorporeal Membrane Oxygenation Network. We owe Li Wenliang, MD from the Wuhan Central Hospital, an eternal debt of gratitude for reminding the world that doctors should never be censored during a pandemic. Finally, we acknowledge all members of the COVID-19–CCC and various collaborators.
Steering Committee
Gianluigi Li Bassi MD1,3, 4,5, 7, 8, PhD; Jacky Y. Suen BSc1, 2, PhD; Heidi J. Dalton MD, MCCM9; John Laffey, MA, MD10; Daniel Brodie, MD11; Eddy Fan, MD, PhD12; Antoni Torres, MD, PhD, FERS ATS Fellow4, 13 36 37; Davide Chiumello, MD14; Alyaa Elhazmi15; Carol Hodgson, PT, PhD16,31; Shingo Ichiba, MD17; Carlos Luna, MD18; Srinivas Murthy, MD19; Alistair Nichol, MD, PhD16, 21,31; Pauline Yeung Ng, MD22; Mark Ogino, MD23; Eva Marwali, MD, PhD35; Giacomo Grasselli MD33, 34, PhD; Robert Bartlett, MD25; Aidan Burrell, MBBS, PhD26,27; Muhammed Elhadi MBBCh38; Anna Motos39,40; Ferran Barbé MD, PhD41,42; Alberto Zanella MD33; and John F. Fraser MBChB, PhD, FRCP(Glas), FFARCSI, FRCA, FCICM1, 3, 5, 7, 8 on behalf of the COVID-19 Critical Care Consortium.
Affiliations
1. Critical Care Research Group, The Prince Charles Hospital, Brisbane, Australia
2. Faculty of Medicine, The University of Queensland, Brisbane, Australia
3. University of Queensland, Brisbane, Australia
4. Institut d'Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona, Spain
5. Queensland University of Technology, Brisbane, Australia
6. School of Public Health, Queensland University of Technology, Brisbane, Australia
7. St Andrew’s War Memorial Hospital, UnitingCare Hospitals, Brisbane Australia
8. Wesley Medical Research, Brisbane, Australia
9. INOVA Fairfax Medical Center, Heart and Vascular Institute, Falls Church VA, USA
10. Anaesthesia and Intensive Care Medicine, Galway University Hospitals, and School of Medicine, National University of Ireland, Galway, Ireland
11. Department of Medicine, Columbia University College of Physicians and Surgeons, New York-Presbyterian Hospital, NY, NY, USA
12. Interdepartmental Division of Critical Care Medicine, University of Toronto, Toronto, Canada
13. Servei de Pneumologia. Hospital Clinic de Barcelona, Barcelona, Spain
14. Ospedale San Paolo, Milan, Italy
15. Dr. Sulaiman Alhabib Medical Group—Research Center, Riyadh, Saudi Arabia
16. Australian and New Zealand Intensive Care Research Centre, Department of Epidemiology and Preventive Medicine, School of Public Health, Monash University, Melbourne, Australia
17. Department of Clinical Engineering / Department of Intensive Care Medicine, Tokyo Women’s Medical University Hospital, Japan
18. División Neumonología, Hospital de Clínicas, UBA, Buenos Aires, Argentina
19. Department of Pediatrics, Faculty of Medicine, University of British Columbia, Vancouver, Canada
20. Australian and New Zealand Intensive Care Research Centre, Department of Epidemiology and Preventive Medicine, School of Public Health, Monash University, Melbourne, Australia
21. University College Dublin-Clinical Research Centre at St Vincent’s University Hospital, Dublin
22. Division of Respiratory and Critical Care Medicine, The University of Hong Kong, Hong Kong, China
23. Nemours Alfred I duPont Hospital for Children, Wilmington, DE, USA
24. Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy
25. University of Michigan Medical Center, Ann Arbor, Michigan, USA
26. Australian and New Zealand Intensive Care Research Centre (ANZIC-RC), School of Public Health and Preventive Medicine, Monash University, Melbourne, Victoria, Australia.
27. Department of Intensive Care and Hyperbaric Medicine, The Alfred Hospital, Melbourne, VIC, Australia.
28. Australian Centre for Health Services Innovation (AusHSI) and Centre for Healthcare Transformation, School of Public Health & Social Work, Queensland University of Technology (QUT), Brisbane, Queensland, Australia
29. Child Health Research Centre, Faculty of Medicine, The University of Queensland, Brisbane, Queensland, Australia
30. ISARIC, Centre for Tropical Medicine and Global Health, University of Oxford, Oxford, UK
31. Department of Physiotherapy, Alfred Hospital, Melbourne, Australia
32. Department of Intensive Care, Alfred Hospital, Melbourne, Australia
33. Department of Anesthesia, Intensive Care and Emergency, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy
34. Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy
35. National Cardiovascular Center Harapan Kita, Jakarta, Indonesia
36. Catalan Institution for Research and Advanced Studies (ICREA), Barcelona, Spain
37. Centro de Investigación Biomédica en Red Enfermedades Respiratorias (CIBERES), Madrid, Spain
38. Faculty of Medicine, University of Tripoli, Tripoli, Libya
39. Centro de Investigación Biomedica En Red—Enfermedades Respiratorias (CIBERES), Barcelona, Spain.
40. Institut d'Investigacions August Pi i Sunyer (IDIBAPS), Barcelona, Universitat de Barcelona, Barcelona, Spain.
41. Translational Research in Respiratory Medicine, Respiratory Dept, Hospital Universitari Aranu de Vilanova and Santa Maria; IRBLleida, Lleida, Spain.
42. Centro de Investigación Biomedica En Red—Enfermedades Respiratorias (CIBERES), Barcelona, Spain
43. School of Medicine, Griffith University, Brisbane, Australia
Funding
The Bill & Melinda Gates Foundation, Grant number INV-034765; Queensland Health; The Prince Charles Hospital Foundation; The Wesley Medical Research; Fisher & Paykel Healthcare; The University of Queensland; The Health Research Board of Ireland. Jacky Y Suen is funded by the Advance Queensland fellowship program, Queensland Government, Australia. Gianluigi Li Bassi is a recipient of the BITRECS fellowship; the “BITRECS” project has received funding from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement no. 754550 and from the “La Caixa” Foundation (ID 100010434), under the agreement LCF/PR/GN18/50310006.
Author information
Authors and Affiliations
Consortia
Contributions
Study concept and design: Jonathon P. Fanning, Maximilian Feth, Gianluigi Li Bassi, Jacky Y. Suen, John F. Fraser, Acquisition, analysis, or interpretation of data: Maximilian Feth, Jonathon P. Fanning, Robert B. Fanning, Natasha Weaver Statistical analysis: Natasha Weaver, Nicole White Tables and figures: Natasha Weaver, Maximilian Feth, Jonathon P. Fanning, First drafting of the manuscript: Maximilian Feth, Jonathon Fanning. Critical revision for important intellectual content and final approval of the manuscript: Maximilian Feth, Jonathon P. Fanning, Natasha Weaver, Robert B. Fanning, Matthew J. Griffee, MD, Sung-Min Cho, Mauro Panigada, Akram M. Zaaqoq, Yew Woon Chia, Bingwen Eugene Fan, Davide Chiumello, Silvia Coppola, Ahmed Labib, Glenn JR Whitman, Rakesh C. Arora, Bo S. Kim, Anna Motos, Nicole White, Jacky Suen, Gianluigi Li Bassi, Roberto Lorusso, John F. Fraser, Giles J. Peek, Heidi Dalton. Guarantors: Maximilian Feth, Jonathon P. Fanning.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The rationale and design have been previously published (Trial registration ACTRN12620000421932) [17]. Institutional Review Board (IRB) approval was obtained for each participating institution. A waiver of informed consent was granted for all patients.
Consent for publication
All authors agree with submitting the manuscript in its current version for publication in Journal of Intensive Care.
Competing interests
This study was supported by the COVID-19 Critical Care Consortium.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Supplemental Material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Feth, M., Weaver, N., Fanning, R.B. et al. Hemorrhage and thrombosis in COVID-19-patients supported with extracorporeal membrane oxygenation: an international study based on the COVID-19 critical care consortium. j intensive care 12, 18 (2024). https://doi.org/10.1186/s40560-024-00726-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-024-00726-2