Abstract
Background
Children with community-acquired septic shock can rapidly deteriorate and die in acute-care hospitals. This study aimed to describe the mortality, timing, and risk factors in children with community-acquired septic shock.
Methods
This is a retrospective cohort study using a national inpatient database in Japan. The study population included children (age < 20 years) who were admitted to acute-care hospitals with a diagnosis of sepsis from July 2010 to March 2020, who were treated with antibiotics, and who were supported with vasoactive drugs within three days of hospitalization. We used a Cox proportional-hazards regression model to identify risk factors for earlier death.
Results
Among 761 eligible children, the median age was 3 (interquartile range, 0–11) years and 57.2% had underlying conditions. Among these, 67.1% were admitted to accredited intensive care units within three days of hospitalization and 38.6% were transported from other hospitals. The median hospital volume, defined as the number of eligible children in each hospital over the study period, was 4 (interquartile range, 2–11). Overall, 244 children died (in-hospital mortality rate, 32.1%). Among them, 77 (31.6%) died on the first day, and 156 (63.9%) died within three days of hospitalization. A Cox proportional-hazards regression model showed that earlier death was associated with lower hospital volume and age 1–5 years, whereas it was inversely associated with admission to an accredited intensive care unit and transport from other hospitals. Among 517 survivors, 178 (34.4%) were discharged with comorbidities.
Conclusions
Children with community-acquired septic shock had high mortality, and early death was common. Our findings may warrant future efforts to enhance the quality of initial resuscitation for sepsis in low-volume hospitals and to ensure a healthcare system in which children with sepsis can be treated in accredited intensive care units.
Similar content being viewed by others
Introduction
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection [1]. Sepsis accounts for 10–20% of all deaths in children [2, 3]. Among sepsis-related deaths in children, 30–50% of deaths occur within the first few days after the recognition of sepsis [4,5,6,7]. Septic shock is associated with even higher mortality and early death, suggesting the importance of initial resuscitation [8]. Community-acquired septic shock has been considered an important issue from a public health perspective due to its incidence and economic burden in comparison to hospital-acquired septic shock [9, 10].
There is accumulating evidence of community-acquired septic shock in children admitted to pediatric intensive care units (PICUs). Community-acquired septic shock accounts for around half of pediatric septic shock [10, 11]. In-hospital mortality remains around 10%, even in high-income countries [11, 12]. In addition, more than one-third of hospital survivors suffer from a reduced quality of life after hospital discharge [13].
In contrast, data on community-acquired septic shock in children admitted to acute-care hospitals are scarce, even though these hospitals are often the primary caregiver for children with sepsis. PICU-based studies cannot include these children unless they are transferred to PICUs. Thus, there is an important knowledge gap that must be overcome to better understand real-world clinical practice for community-acquired sepsis in children. We therefore used a national inpatient database in Japan to comprehensively describe mortality, its timing, and risk factors in children admitted to acute-care hospitals with community-acquired septic shock.
Methods
Study design and participants
We performed a retrospective cohort study using the Diagnosis Procedure Combination database in Japan. We identified children admitted to acute-care hospitals with community-acquired septic shock from July 2010 to March 2020. Details of the database were described elsewhere [14]; briefly, it includes discharge abstracts and administrative claims data from more than 1200 participating acute care hospitals, which cover approximately eight million inpatient admissions per year, representing more than half of all inpatient admissions to acute care hospitals in Japan. Twenty-four of 27 hospitals with PICUs were registered in the database. The database includes the following data: patient age, sex, body height, weight, Japan Coma Scale score, diagnosis, preadmission comorbidities, post-admission complications, medications, discharge status, and unique identifiers for hospitals. Diagnoses are recorded using the International Classification of Diseases 10th revision (ICD-10) codes. The validity of diagnoses and procedures in the database was established in a previous study; the specificity of the recorded diagnoses exceeded 96%, whereas the sensitivity ranged from 50 to 80%, and the specificity and sensitivity of recorded procedures both exceeded 90% [14]. This study was approved by the Institutional Review Board of the University of Tokyo [approval number: 3501-(5); May 19, 2021] and the procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975. The requirement for informed consent was waived because of the anonymity of the data.
We chose the following inclusion and exclusion criteria in line with previous research [3, 5, 13, 15]. First, we extracted children younger than 20 years of age who were admitted with sepsis-related diagnoses (ICD-10 codes: A02.1, A28.2, A32.7, A39.4, A40.0–A40.9, A41.0–A41.9, A42.7, A54.8, B00.7, B34.9, B37.7, I30.1, I33.0, J02.0, J20.9, L02.9, L08.0, M86.99, P36.0–P36.9, and T81.4) from July 2010 to March 2020. Among them, we included those with: (i) principal or admission diagnoses including the word ‘sepsis’ or ‘septic’ in Japanese; (ii) antibiotics were started within three days of hospitalization and continued for at least four consecutive days with at least one intravenous dosage; and (iii) vasoactive drugs used within three days of hospitalization. The following exclusion criteria were applied: duration of antibiotics shorter than four days; discharge within three days of hospitalization; transport to another hospital within four days of hospitalization; birth admission; hospitalization on the first day of life; admission with exogenous diagnoses (such as trauma, burn, and toxication); or out-of-hospital cardiac arrest. We did not exclude cases if death was the cause of the short duration of hospital stay and antibiotics use (as in previous studies) [16].
Outcomes and patient backgrounds
The primary outcome was in-hospital mortality. The other outcomes included the Japan Coma Scale score at discharge, the activity of daily living at discharge, tracheostomy/gastrostomy during admission, and nasogastric tube feeding/home ventilation/physiotherapy at discharge. Discharge with comorbidities included (i) mechanical ventilation, oxygen therapy, tube feeding, or physiotherapy on the day of discharge to home or the day before discharge to home, (ii) worse Japan Coma Scale score at discharge than on admission, (iii) lower level of activity on the modified Rankin Scale or activities of daily living at discharge than on admission, and (iv) tracheostomy or gastrostomy during admission.
Patient background factors included age, sex, principal and admission diagnoses, underlying conditions (preadmission comorbidities, preadmission activity of daily living, requirement of care at home), clinical characteristics (Japan Coma Scale score on admission, transport from other hospitals, cardiac arrest before hospitalization,), tests (blood culture test and other culture tests), and therapies (antibiotics, vasoactive drugs, corticosteroids, intravenous immunoglobulin, blood product, mechanical ventilation, renal replacement therapy, extracorporeal membrane oxygenation, operations, and resuscitation for in-hospital cardiac arrest). Vasoactive drugs included noradrenaline, dopamine, vasopressin, phenylephrine, adrenaline, dobutamine, and milrinone.
Hospital volume was defined as the number of eligible children in each hospital over the study period and was categorized into tertiles (low, middle, and high). According to the Japanese administrative claims system, accredited intensive care units (ICUs) included PICU, neonatal ICU, general ICU, emergency ICU, and intermediate care unit. We categorized impaired consciousness, as assessed by the Japan Coma Scale, into three groups (severe, moderate, and mild) [17]. This category of ‘severe’, ‘moderate’, and ‘mild’ approximately corresponds to 3–8, 9–13, and 14–15, respectively, on the Glasgow Coma Scale [18, 19]. We categorized underlying conditions according to complex chronic conditions for the ICD-10 code [20]. We defined “care-dependence” according to underlying conditions (e.g., limited level of daily activity, need for daily care, home ventilation, home oxygen therapy, tracheostomy, and tube-feeding).
Statistical analyses
We used a Cox proportional-hazards regression model to analyze the association between study covariates and in-hospital mortality censored on the thirtieth day of hospitalization. The assumption of proportional-hazard was assured based on Schoenfeld residuals and log–log survival plots. We chose the study covariates based on biological and clinical plausibility, and existing literature. The following covariates were included: age, underlying condition (neuromuscular, cardiovascular, respiratory, congenital/genetic, hematological/malignancy/transplant, care-dependence), septic shock as the admission diagnosis, impaired consciousness on admission, transport from other hospitals, admission to accredited ICU within three days of hospitalization, hospital volume, therapies within three days of hospitalization (mechanical ventilation, renal replacement therapy, extracorporeal membrane oxygenation), use of vasoactive drugs on the first day, and use of antibiotics on the first day [2, 5, 10, 21]. All analyses were performed using STATA 17 (StataCorp LLC, College Station, TX, USA).
Results
Patient characteristics and therapies
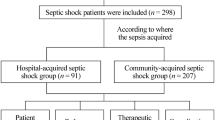
We identified 761 children with community-acquired septic shock (Fig. 1). The median age was 3 (interquartile range (IQR), 0 to 11) years. Infants (29 days to < 1 year of age) accounted for 17.4% of the patients (n = 133), followed by neonates (12.4%; n = 94) and 1-year-old children (10.2%; n = 78) (Fig. 2). Among 761 eligible children, 435 (57.2%) children had one or more underlying conditions. Common underlying conditions included care-dependence in 222 (29.2%), neuromuscular conditions in 106 (13.9%) and cardiovascular conditions in 99 (13.0%) children. A total of 511 (67.1%) children were admitted to accredited ICUs within three days of hospitalization and 294 (32.6%) children were transported from other hospitals (Table 1). The 761 children included in this study were treated in 260 hospitals with a median hospital volume of 4 (IQR, 2 to 11).
Mechanical ventilation, renal replacement therapy, and extracorporeal membrane oxygenation were used in 591 (77.7%), 119 (15.6%), and 15 (2.0%) children within three days of hospitalization. Noradrenaline, dopamine, and adrenaline were commonly used vasoactive drugs (Table 2). Blood products, albumin, and corticosteroids were used in 368 (48.4%), 314 (41.3%), and 417 (54.8%) children. Surgical treatment was performed within three days of hospitalization in 26 (3.4%) children. Blood culture tests were performed within three days of hospitalization in in 666 (79.8%) children.
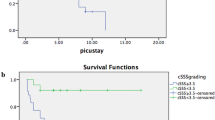
Mortality and timing
Among 761 children, 244 died (in-hospital mortality rate, 32.1%). Among these 244 cases, 77 (31.6%) children died on the first day of hospitalization, and 156 (63.9%) children died within three days of hospitalization.
Risk factors for in-hospital mortality
In a Cox proportional-hazard regression model, the risk of earlier mortality increased with a low hospital volume [hazard ratio (HR), 1.94; 95% confidence interval (CI), 1.36 to 2.76; p < 0.001], age 1–5 years (HR, 1.90; 95% CI 1.33 to 2.70; p < 0.001), severely impaired consciousness (HR, 1.49; 95% CI 1.09 to 2.02; p = 0.01), mechanical ventilation within three days of hospitalization (HR, 3.26; 95% CI 2.00 to 5.30; p < 0.001), extracorporeal membrane oxygenation within three days of hospitalization (HR, 2.22; 95% CI 1.08 to 4.59; p = 0.03), and use of vasoactive drugs on the first day (HR, 1.91; 95% CI 1.37 to 2.68; p < 0.001). On the other hand, the risk decreased with admission to accredited intensive care units (HR, 0.52; 95% CI 0.38 to 0.70; p < 0.001), transport from other hospitals (HR, 0.71; 95% CI 0.53 to 0.97; p = 0.03), care-dependence (HR, 0.57; 95% CI 0.41 to 0.80; p < 0.01), and antibiotics started on the first day (HR, 0.36; 95% CI 0.26 to 0.50; p < 0.001), as described in Table 3.
Comorbidities
Of 761 included children, 43 (5.7%) received tracheostomy, with the median timing being the 27th (IQR, 17th to 53rd) day of hospitalization. Ten (1.3%) children received gastrostomy with the median timing being the 55th (IQR, 49th to 72nd) day of hospitalization.
Among 517 hospital survivors, 178 (34.4%) children were discharged with new comorbidities; requirement for respiratory support in 80 (15.5%), tracheostomy in 31 (6.0%), decreased consciousness in 10 (1.9%), tube-feeding in 70 (13.5%) and physiotherapy-dependence in 75 (14.5%) children.
Discussion
In this analysis of children with community-acquired septic shock in acute-care hospitals, we described in-hospital mortality, early death, and risk factors. The in-hospital mortality rate was 32.1% in this study. Cohort studies from 52 European PICUs and 12 American PICUs in academic hospitals showed in-hospital mortality rates of 10% and 9% in children with community-acquired septic shock [12, 13]. Even in an observational study in nine Japanese PICUs, the in-hospital mortality rate was 18% in 44 children with community-acquired severe sepsis or septic shock [11]. These comparisons could indicate that children with community-acquired septic shock in acute-care hospitals have increased mortality in comparison to those in PICUs. We are not entirely sure of the reasons behind this difference. The difference in mortality may be attributable to multiple factors, such as patient selection, microbiological profiles, and healthcare systems (e.g., types of hospitals caring for children with sepsis and compliance to the guidelines for sepsis) [22, 23]. Our analysis included five times the number of children per year in comparison to the Japanese PICU-based study [11]. Therefore, one potential reason could be that PICU-based studies may have described selected patients given there could be rapidly deteriorating children in acute-care hospitals who did not have a chance to be transported to PICUs, which may have contributed to increased mortality and early death in our study. This hypothesis could be supported by a UK study reporting that 26% of deaths occurred before the PICU admission among children referred to a pediatric inter-hospital transport service with a working diagnosis of sepsis [6]. Moreover, in our study, transport from other hospitals was associated with decreased mortality. This study could suggest that future studies could benefit by including not only children admitted to PICUs but also those in more comprehensive settings, which were acute-care hospitals in this study, to better describe the real-world clinical practice in relation to community-acquired sepsis in children.
On the other hand, our findings regarding the large number of deaths in acute-care hospitals may not be generalizable to other countries or healthcare systems. There is variation among countries in the types of hospitals caring for children with sepsis, thresholds for referring ill children to PICUs, and locally available medical transport services [24, 25]. In addition, microbiological profiles could vary; even the frequency of meningococcal infections in children admitted to acute-care hospitals with community-acquired septic shock has not been well documented, although it has been deemed a common pathogen in children with sepsis who show rapid deterioration [6].
We found that two-thirds of deaths occurred within three days of hospitalization. This was higher than the previously reported rates of early death (30–50%) in children with severe sepsis or septic shock [4,5,6]. Early death was more common in children with septic shock in a North American study, which may explain the high proportion of early death that we observed [5]. This result could emphasize the importance of initial resuscitation for sepsis again. The success of initial resuscitation in local hospitals could reduce mortality in children with sepsis [22]. Moreover, in this study, more than two-thirds of deaths occurred in hospitals in which the hospital volume was less than one case per year. The early deaths that were sporadically distributed to low-volume hospitals could warrant future efforts to enhance the quality of initial resuscitation in these low-volume hospitals [24].
We found that earlier mortality increased with a low hospital volume and in children of 1–5 years of age after adjusting for patient severity and treatments applied, whereas earlier mortality decreased with admission to an accredited ICU and transport from other hospitals. There is some evidence supporting these findings. A North American study showed decreased mortality in high-volume PICUs [5]. Early admission to ICUs might prevent suboptimal resuscitation [23]. Children with community-acquired septic shock could be better treated in accredited ICUs that are well-staffed and which accommodate a large number of critically-ill children. Thus, it is important—from a public health perspective—to ensure a healthcare system in which these critically ill children can be treated in well-staffed ICUs with a high patient volume.
The present study is associated with several limitations. As physiological and laboratory data were limited in the database, we could not describe end-organ dysfunctions according to the International Pediatric Sepsis Consensus Conference definitions [15]. In addition, we could not describe the pathogen, its susceptibility to antibiotics, the timing of recognition of sepsis, or compliance to the guidelines for sepsis, which should be described in future studies to complement our findings. Second, our method of using the ICD-10 codes for sepsis could lead to a narrower cohort with higher mortality in comparison to other coding methods, such as a method extracting data from all children with infection-related diagnoses [26]. However, we considered that including a pure cohort with the diagnosis of sepsis is the safest practically-available approach because it is hardly possible to extract eligible patients from all inpatients with infection-related diagnoses without detailed data on end-organ dysfunctions. Moreover, this approach meant that our study was in line with previous literature [3]. Third, the mortality in this study may have been overestimated because of our inclusion criteria. That is, we only included patients who used antibiotics for four days or more, and thus we may have excluded non-bacterial infections (i.e., viral infections) or milder cases with septic shock. Also, we only included patients who used vasoactive drugs as the surrogate criterion for cardiovascular dysfunction (as in previous studies), and thus we might have excluded milder cases treated with fluid resuscitation alone [15, 27]. Fourth, as for the inclusion criteria, other studies used blood culture results as an inclusion criterion, while we considered that the diagnosis of sepsis was a more specific sign of suspected or confirmed infections [15, 16]. Lastly, as for study covariates associated with mortality, we could not conclude whether these covariates were triggers of deterioration or simply markers of disease severity.
Conclusion
The mortality of children admitted to acute-care hospitals due to community-acquired septic shock was as high as 32% and early death was common, even in a high-income country with national health insurance. The risk factors in this study could warrant future efforts to enhance the quality of initial resuscitation for sepsis, especially in low-volume hospitals, which were associated with mortality, and to ensure a healthcare system in which children with community-acquired septic shock can be treated in accredited intensive care units.
Availability of data and materials
Not applicable.
Abbreviations
- PICU:
-
Pediatric intensive care unit
- ICD-10:
-
International Classification of Diseases 10th revision
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315:775–87.
Schlapbach LJ, Straney L, Alexander J, et al. Mortality related to invasive infections, sepsis, and septic shock in critically ill children in Australia and New Zealand, 2002–13: a multicentre retrospective cohort study. Lancet Infect Dis. 2015;15:46–54.
Born S, Dame C, Schlapbach LJ, et al. Epidemiology of sepsis among children and neonates in Germany: results from an observational study based on nationwide diagnosis-related groups data between 2010 and 2016. Crit Care Med. 2021;14635:1–9.
Weiss SL, Balamuth F, Hensley J, et al. The epidemiology of hospital death following pediatric severe sepsis: when, why, and how children with sepsis die. Pediatr Crit Care Med. 2017;18:823–30.
Johnson KT, Görges M, Murthy S. Characteristics and timing of mortality in children dying with infections in North American PICUs. Pediatr Crit Care Med. 2021;22:365–79.
Cvetkovic M, Lutman D, Ramnarayan P, et al. Timing of death in children referred for intensive care with severe sepsis: implications for interventional studies. Pediatr Crit Care Med. 2015;16:410–7.
Thompson MJ, Ninis N, Perera R, et al. Clinical recognition of meningococcal disease in children and adolescents. Lancet. 2006;367:397–403.
Weiss SL, Peters MJ, Alhazzani W, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med. 2020;46:10–67.
Paoli CJ, Reynolds MA, Sinha M, et al. Epidemiology and costs of sepsis in the United States—an analysis based on timing of diagnosis and severity level. Crit Care Med. 2018;46:1889–97.
Weiss SL, Fitzgerald JC, Pappachan J, et al. Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med. 2015;191:1147–57.
Shime N, Kawasaki T, Saito O, et al. Incidence and risk factors for mortality in paediatric severe sepsis: results from the national paediatric intensive care registry in Japan. Intensive Care Med. 2012;38:1191–7.
Boeddha NP, Schlapbach LJ, Driessen GJ, et al. Mortality and morbidity in community- acquired sepsis in European pediatric intensive care units: a prospective cohort study from the European Childhood Life-threatening Infectious Disease Study (EUCLIDS). Crit Care. 2018;51:1–13.
Zimmerman JJ, Banks R, Berg RA, et al. Trajectory of mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit Care Med. 2020;48:329–37.
Yamana H, Moriwaki M, Horiguchi H, et al. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol. 2017;27:476–82.
Weiss SL, Balamuth F, Chilutti M, et al. Identification of pediatric sepsis for epidemiologic surveillance using electronic clinical data. Pediatr Crit Care Med. 2020;21:113–21.
Rhee C, Dantes R, Epstein L, et al. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009–2014. JAMA. 2017;318:1241–9.
Ohta T, Waga S, Handa W, et al. New grading of level of disordered consiousness (author’s transl). No Shinkei Geka. 1974;2:623–7.
Enomoto Y, Tsutsumi Y, Tsuchiya A, et al. Validation of the Japan Coma Scale for the prediction of mortality in children: analysis of a nationwide trauma database. World J Pediatr Surg. 2022;5:1–6.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–4.
Feudtner C, Feinstein JA, Zhong W, et al. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:1–7.
Xiao C, Wang S, Fang F, et al. Epidemiology of pediatric severe sepsis in main PICU centers in Southwest China. Pediatr Crit Care Med. 2019;20:1118–25.
Oliveira CF, Nogueira De Sá FR, Oliveira DSF, et al. Time- and fluid-sensitive resuscitation for hemodynamic support of children in septic shock: barriers to the implementation of the American college of critical care medicine/pediatric advanced life support guidelines in a pediatric intensive care unit in. Pediatr Emerg Care. 2008;24:810–5.
Inwald DP, Tasker RC, Peters MJ, et al. Emergency management of children with severe sepsis in the united kingdom: the results of the paediatric intensive care society sepsis audit. Arch Dis Child. 2009;94:348–53.
Egi M. The Japanese clinical practice guidelines for management of sepsis and septic shock 2016: methodological considerations and proper use. J Jpn Soc Clin Anesth. 2017;37:805–10.
Odetola FO, Clark SJ, Gurney JG, et al. Factors associated with interhospital transfer of children with respiratory failure from level II to level I pediatric intensive care units. J Crit Care. 2015;30:1080–4.
Balamuth F, Weiss SL, Neuman MI, et al. Pediatric severe sepsis in US children’s hospitals. Pediatr Crit Care Med. 2014;15:798–805.
Hsu HE, Abanyie F, Agus MSD, et al. A national approach to pediatric sepsis surveillance. Pediatrics. 2019. https://doi.org/10.1542/peds.2019-1790.
Acknowledgements
None.
Funding
This study was supported by grants from the Ministry of Health, Labor and Welfare, Japan (21AA2007 and 22AA2003) and the Ministry of Education, Culture, Sports, Science and Technology, Japan (20H03907).
Author information
Authors and Affiliations
Contributions
SM designed the study, planned the analysis and drafted the manuscript. NM gave suggestions for the study design, analyzed data, and revised the manuscript. YH, HM, and KF gave suggestions for the study design and extracted the study dataset from the database. HY gave suggestions for the study design and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the University of Tokyo [approval number: 3501-(5); May 19, 2021] and the procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975. The requirement for informed consent was waived because of the anonymity of the data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Miura, S., Michihata, N., Hashimoto, Y. et al. Descriptive statistics and risk factor analysis of children with community-acquired septic shock. j intensive care 11, 6 (2023). https://doi.org/10.1186/s40560-023-00652-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-023-00652-9