Abstract
Background
The objectives of the present study are to: (i) evaluate the effect of environmental and metabolic heat on heat-related illnesses in outdoor workers; and (ii) evaluate the effect of personal factors, including heat acclimation, on the risk of heat-related illnesses in outdoor workers.
Methods
We identified 47 cases of illnesses from exposure to environmental heat in outdoor workers in Korea from 2010 to 2014, based on review of workers’ compensation data. We also obtained the information on location, time, and work environment of each heat-related illness.
Results
Our major results are that 29 cases (61.7%) occurred during a heat wave. Forty five cases (95.7%) occurred when the maximum estimated WBGT (WBGTmax) was equal to or greater than the case specific threshold value which was determined by acclimatization and metabolic rate. Twenty two cases (46.8%) were not acclimated to the heat. Thirty-seven cases (78.7%) occurred after tropical night (temperature above 25 °C), during which many people may find it hard to sleep.
Conclusion
Personal risk factors such as heat acclimation as well as environmental factors and high metabolic rate during work are the major determinants of heat-related illnesses.
Similar content being viewed by others
Background
Workers who are exposed to extreme heat while engaged in strenuous physical activities outdoors have an increased risk for heat stress [1,2,3]. Exposure to extreme heat can result in several occupational illnesses, including heat stroke, heat exhaustion, heat syncope, heat cramps, heat rashes, and even death [4,5,6,7,8,9,10]. Heat can also increase the risk of injuries, because it may lead to sweaty palms, fogged-up safety glasses, and dizziness, and may also reduce brain function, leading to impaired reasoning ability, and thereby create additional hazards [11, 12].
Heat stress will become an increasing problem for outdoor workers, because global temperatures are expected to rise due to the global climate change [2]. It seem likely that global climate change will increase known heat-exposure hazards for workers, especially their severity, prevalence, and distribution, although this has not yet been definitively established [13, 14]. During sudden or prolonged heat waves in urban areas, there are sudden increases in mortality, especially among older individuals who apparently have reduced physiologic reserves [5, 15, 16]. In prolonged heat waves, the mortality rate is higher in the early phase than in the later phase [15, 16]. Previous studies on heat wave in general population have been focused on meteorological factors such as air temperature, humidity, wind speed and radiation. Recent papers reported that personal factors such as heat acclimation [17,18,19], being older than 60 [20,21,22], experience of a previous heat-related illness [23, 24], use of certain medications [25, 26], presence of certain concurrent diseases [27, 28], severe obesity [15, 20], and dehydration [29, 30] also increase the risk of heat-related illnesses [18]. However, outdoor workers are exposed to heat stress from the meteorological environment, from exertion, and due to the insulation of clothing during work. These workers may also have additional personal risk factors that increase the risk of heat-related illnesses. However, meteorological, metabolic, clothing, and personal factors affecting heat-related diseases in outdoor workers were scarcely studied [31] although heat strokes were reported in soldiers [32,33,34], indoor workers [35], and general population [36,37,38,39,40] in Korea. In particular, the personal factors were not studied in outdoor workers in Korea.
The objectives of the present study are to: (i) evaluate the effect of environmental and metabolic heat on heat-related illnesses; and (ii) evaluate the effect of personal susceptible factors including heat acclimation on heat-related illnesses in Korean outdoor workers, to prevent heat-related illnesses.
Methods
This is a descriptive study on outdoor workers with heat-related illness. We obtained workers’ compensation data for all of Korean workers who were compensated with heat-related illness including heat stroke, heat exhaustion, heat syncope and heat cramps in outdoor workers such as construction workers, or waste disposal workers during previous 5 years prior to the present study (from 2010 to 2014) from Korea Occupational Safety and Health Agency (KOSHA) [41]. We identified 47 cases of illnesses from exposure to environmental heat in outdoor workers. Obtained data include information on age, sex, diagnosis, occupation classified by major, sub-major, and minor categories, and time of employment of workers, the location and time of these events, and the type of work being performed at the time of events. We classified outdoor workers into workers with or without heavy physical work, which is defined by ISO [19], for example, intense arm and trunk work, carrying heavy material, and pushing or pulling heavily loaded carts.
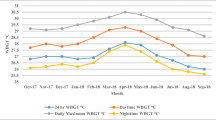
For identification of meteorological factors associated with heat-related diseases, the hourly dry air temperature and relative humidity of the 3 days prior to each heat-related illness were obtained from the closest meteorological sites (Automatic Weather System (AWS) or Automated Synoptic Observing System (ASOS), operated by the Korea Meteorological Administration). A ‘heat wave’ was defined as a period of 2 or more consecutive days with temperatures of 33 °C or higher [42]. A ‘tropical night’ was defined one in which the lowest nighttime temperature was above 25 °C [42]. Wet-bulb globe temperature (WBGT) was estimated using the meteorological data from AWS and ASOS with Park’s formula [43].
Personal factors associated with heat-related diseases identifiable from workers’ compensation data were limited to age and acclimatization. Unacclimatized workers were defined as workers with less than a week of period of time from the first outdoor placement of worker to the time of the onset of heat-related disease [18]. Lack of sleep was presumed when tropical night occurred just 1 day prior to the occurrence of heat-related disease in outdoor workers [44,45,46].
We evaluated 47 workers individually in terms of their exposure to meteorological factors, such as heat wave and tropical night, and personal factor such as acclimatization.
The present study utilized workers’ compensation data, which were formally obtained from KOSHA, and did not include identifiable personal information. This study was exempted from Institutional Review Board review (UUH 2017–04-010).
Results
We identified 47 outdoor workers (43 males and 4 females) who had illnesses following exposure to environmental heat from 2010 to 2014, based on a review of workers’ compensation data (Table 1). Twenty-six workers (55.3%) suffered from heat-related illnesses in 2013, the worst year. Three of the 47 workers were in their 20’s (6.4%), 4 in their 30’s (8.5%), 13 in their 40’s (27.7%), 15 in their 50’s (31.9%), and 10 in their 60’s (21.3%), and 2 in their 70’s (4.2%). Twenty-three individuals (48.9%) were construction workers, 6 were cleaning and janitorial workers, 4 were agroforestry workers, and the others worked in various different fields. The heat-related illnesses were heat stroke (39 cases), heat cramp (1 case), heat exhaustion (5 cases), and heat syncope (2 cases). There were 11 fatalities.
Our evaluation of the 47 compensated cases of occupational heat-related illness in outdoor workers during 2010 ~ 2014 shows that 29 cases (61.7%) occurred during a heat wave. Forty five cases (95.7%) occurred when the maximum estimated WBGT (WBGTmax) was equal to or greater than the case specific threshold value which was determined by acclimatization and metabolic rate [19]. Twenty two cases (46.8%) occurred in workers who were not acclimatized workers, and 37 cases (78.7%) occurred after a tropical night.
Discussion
Heat stress is the net heat load to which a worker is exposed from the combined contributions of environmental factors, metabolic heat, and clothing, all of which increase heat storage in the body [17, 18]. The heat load experienced by a worker provokes a physiological response (heat strain), that increases heat loss from the body in an effort to maintain a stable body temperature. This physiological response is not always successful and, when unsuccessful, may result in heat injury and death [17, 18].
The specific environmental factors causing heat stress are high air temperature, minimal movement of air, high humidity, and radiant heat. Physical work contributes to the total heat stress of a job, because metabolic heat increases in proportion to work intensity [19]. The amount, thermal characteristics, and type of clothing worn are also important, because they alter the rate of heat exchange between the skin and the air [47, 48].
In most situations environmental heat exposure can be assessed by WBGT [3, 49]. The WBGT also considers metabolic heat and insulation from clothing [17, 19]. The metabolic contribution to the heat load of the worker can be estimated based on the extent of physical exertion (light, moderate, or heavy) [19]. Lower WBGT thresholds should be applied to workers when they perform heavy work than light work. WBGT limits assume the person is wearing a conventional one-layer work clothing ensemble, consisting of not more than a long-sleeved work shirt and trousers (or the equivalent) [50]. Thus, a lower WBGT limit should be applied to workers who wear clothes with lower air and vapor permeability or that provide greater insulation than conventional clothing [19, 48, 51,52,53].
In addition to environmental heat, metabolic heat, and clothing insulation, additional personal factors affect the risk of heat-related illness. These include heat acclimation [17,18,19], dehydration [29, 30], unique medical characteristics [23, 24, 26], and overall health status at the time of exposure to heat stress [28, 29].
The present study had several important findings. First, 61.7% of heat-related events occurred during periods when there was a high dry bulb air temperature (heat wave), and 95.7% occurred when the temperature exceeded the WBGT limit. These findings suggest that the WBGT limits can predict heat-related illness better than air temperature [54]. The WBGT-based limit (but not the dry bulb temperature) is based on other environmental factors, such as water vapor pressure, movement of air, and radiant heat, and this limit can be adjusted according to metabolic heat and the type of clothing [49, 55].
Second, 46.8% of the heat-stressed workers in our study were not acclimatized to a high temperature. This finding is compatible with the results of Arbury et al. [56]. They presented 22 cases of heat-related illness or death in a population of workers. In most cases, the employers had no program to prevent heat illness, or the program was deficient. Acclimatization was the most commonly missing program element, and the element most clearly associated with worker death. Appropriate repeated exposure to elevated heat stress causes a series of physiological adaptations -- acclimatization -- in most people, in which the body becomes better able to cope with heat stress. An acclimatized worker can tolerate greater heat stress [25, 57,58,59]. Different exposure limits to heat are applied, depending on the acclimation of each individual. The current National Institute of Occupational Safety and Health (NIOSH) Recommended Alert Limits (RALs) are for unacclimatized workers and the Recommended Exposure Limits (RELs) for acclimatized workers [60, 61]. Occupational Safety and Health Agency (OSHA) defines the WBGT–based limit differently for acclimatized and unacclimatized workers [47], as does the American Conference of Governmental Industrial Hygienists (ACGIH) threshold limit value (TLV) [17], the American Industrial Hygiene Association [62], and the international standard organization [19]. Acclimatization to work in hot, humid environments provides adaptive benefits [25], so an acclimatization plan should be implemented at all workplaces where workers are exposed to heat.
Third, a tropical night on the previous day was associated with 78.7% of heat-related illnesses, but high daytime temperature (heat wave) was associated with 61.7% of heat-related illnesses. The most common consequence of the warm nights on health is their impact on sleep of workers. Heat can cause disturbances and sleep deprivation by thermoregulation processes [44]. Higher than the comfort temperature can influence sleep loss and the reduction of rapid eye movement (REM) and slow-wave sleep (SWS) phases [45, 46]. Sleep disorders occur more frequently, as the risk of death during heat waves, in people with advanced age [44, 63]. During tropical nights, many people may not sleep well, and this lack of sleep may increase the risk for heat-related illness.
Finally, 87.2% of 47 outdoor workers did heavy physical work. This finding showed that metabolic heat is an important factor to increase the risk of heat-related illness in addition to environmental heat. Older outdoor workers were more likely to increase the risk for heat-related illness although they did not perform heavy physical work.
Taken together, personal factors, as well as environmental factors and metabolic heat, are the major determinants of heat-related illnesses. Moreover, many factors other than heat acclimation or lack of sleep may make individuals more susceptible to heat-related illnesses. Recent papers reported that being older than 60 [20,21,22], experience of a previous heat-related illness [23, 24], use of certain medications [25, 26], presence of certain concurrent diseases [27, 28], severe obesity [15, 20], and dehydration [29, 30] also increase the risk of heat-related illnesses [18].
Our research led to a model for the development of heat-related illnesses (Fig. 1). When excessive environmental and/or metabolic heat stress are combined with personal risk factors, physiological responses (heat strain) that promote transfer of heat back into the environment to maintain core body temperature cannot adequately maintain body temperature [64]. This leads to increased core temperature and pulse rate, and decreased body weight due to dehydration [17]. Without early interventions in an individual with early signs of heat-related illness, the heat strain can become harmful and the worker may become a heat casualty [18].
A limitation of the present study is that we only considered two personal risk factors: heat acclimation and lack of sleep. We were not able to obtain information on additional personal factors that affect the risk of heat stress such as dehydration, experience of a previous heat-related illness, use of certain medications, presence of certain concurrent diseases, and overall health status at the time of exposure to heat stress from the data base.
Conclusion
Personal risk factors, environmental factors, and metabolic heat are the major determinants of heat-related illnesses. All workplaces should implement acclimatization plans for workers who are exposed to heat. Managers should also check the status of workers, such as lack of sleep, dehydration, and consumption of alcohol before work.
Abbreviations
- ACGIH:
-
American Conference of Governmental Industrial Hygienists
- ASOS:
-
Automated Synoptic Observing System
- AWS:
-
Automatic Weather System,
- NIOSH:
-
National Institute of Occupational Safety and Health
- OSHA:
-
Occupational Safety and Health Agency
- RAL:
-
Recommended Alert Limit
- REL:
-
Recommended Exposure Limit
- REM:
-
Rapid eye movement
- RH:
-
Relative humidity
- SWS:
-
Slow-wave sleep
- Ta :
-
Air temperature
- TLV:
-
Threshold limit value
- Tw :
-
Wet-bulb temperature
- WBGT:
-
Wet-bulb globe temperature
References
Nichols AW. Heat-related illness in sports and exercise. Curr Rev Musculoskelet Med. 2014;7:355–65.
Lucas RA, Epstein Y, Kjellstrom T. Excessive occupational heat exposure: a significant ergonomic challenge and health risk for current and future workers. Extrem Physiol Med. 2014;3:14.
Garzon-Villalba XP, Mbah A, Wu Y, Hiles M, Moore H, Schwartz SW, et al. Exertional heat illness and acute injury related to ambient wet bulb globe temperature. Am J Ind Med. 2016;59:1169–76.
Minard D, Copman L. Elevation of body temperature in disease. In: Hardy JD, editor. Temperature: its measurement and control in science and industry, vol. 3. New York: Reenhold Co.; 1963.
Leithead CS, Lind AR. Heat stress and heat disorders. London: Cassell; 1964.
Minard D. Physiology of heat stress. In: National Institute for Occupational Safety and Health, United States Public Health Service, Division of Occupational Health, editor. The occupational environment: its evaluation & control. 3rd ed. Washington, DC: U.S. Government Printing Office; 1973.
Lind AR. Human tolerance to hot climates. In: DHK L, Falk HL, Murphy SD, American Physiological Society, editors. Handbook of physiology: a critical, comprehensive presentation of physiological knowledge and concepts. American Physiological Society: Bethesda; 1977.
Dinman BD, Horvath SM. Heat disorders in industry: a reevaluation of diagnostic criteria. J Occup Med. 1984;26:489–95.
Springer K. If you can’t stand the heat. Ohio Monitor. 1985;58:4–9.
CDC. Heat-related deaths among crop workers-United States, 1992–2006, Morbidity and mortality weekly report (MMWR); 2008. p. 649–53.
Ramsey JD, Burford CL, Beshir MY, Jensen RC. Effects of workplace thermal conditions on safe work behavior. J Saf Res. 1983;14:105–14.
Fogleman M, Fakhrzadeh L, Bernard TE. The relationship between outdoor thermal conditions and acute injury in an aluminum smelter. Int J Ind Ergon. 2005;35:47–55.
Schulte PA, Bhattacharya A, Butler CR, Chun HK, Jacklitsch B, Jacobs T, et al. Advancing the framework for considering the effects of climate change on worker safety and health. J Occup Environ Hyg. 2016;13:847–6.
Schulte PA, Chun H. Climate change and occupational safety and health: establishing a preliminary framework. J Occup Environ Hyg. 2009;6:542–54.
Henschel A, Burton LL, Margolies L, Smith JE. An analysis of the heat deaths in St. Louis during July, 1966. Am J Public Health Nations Health. 1969;59:2232–42.
Ellis FP. Mortality from heat illness and heat-aggravated illness in the United States. Environ Res. 1972;5:1–58.
ACGIH. Heat stress and strain, TLVs and BEIs. threshold limit values for chemical substances and physical agents & biological exposure indices. ACGIH: Cincinnati; 2015.
NIOSH. Criteria for a recommended standard. Occupational exposure to heath and hot environments. Cincinnati: DHHS (NIOSH); 2016.
ISO. Estimation of the heat stress on working man, based on the WBGT-index. (Standard no. ISO 7243) 1989.
Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O. Heat stress in older individuals and patients with common chronic diseases. CMAJ. 2010;182:1053–60.
Taylor NAS, Kondo N, Kenny WL. The physiology of acute heat exposure, with implications for human performance in the heat. In: Taylor NAS, Groeller H, editors. Physiological bases of human performance during work and exercise. 1st ed. Edinburgh: Elsevier; 2008.
Wright HE, Larose J, McLellan TM, Hardcastle SG, Boulay P, Kenny GP. Moderate-intensity intermittent work in the heat results in similar low-level dehydration in young and older males. J Occup Environ Hyg. 2014;11:144–53.
Epstein Y, Albukrek D, Kalmovitc B, Moran DS, Shapiro Y. Heat intolerance induced by antidepressants [case report]. Ann N Y Acad Sci. 1997;813:553–8.
Moran DS, Erlich T, Epstein Y. The heat tolerance test: an efficient screening tool for evaluating susceptibility to heat [case report]. J Sport Rehabil. 2007;16:215–21.
DOD. Technical bulletin: heat stress control and heat casualty management, Tb med 507/AFPAM 48–152 (I). Washington, DC: Departments of the U.S. Army, Navy, and Air Force; 2003.
Khagali M, Hayes JSR. Heatstroke and temperature regulation. Sydney: Academic Press; 1983.
Redmond CK, Emes JJ, Mazumdar S, Magee PC, Kamon E. Mortality of steelworkers employed in hot jobs. J Environ Pathol Toxicol. 1979;2:75–96.
Dukes-Dobos FN. Hazards of heat exposure: a review. Scand J Work Environ Health. 1981;7:73–83.
McArdle WD, Katch FI, Katch VI. Exercise at medium and high altitude, Exercise physiology: energy, nutrition, and human performance. 4th ed. Williams & Wilkins: Baltimore; 1996.
Williams WJ, Schneider SM, Stuart CA, Gretebeck RJ, Lane HW, Whitson PA. Effect of dietary sodium and fluid/electrolyte regulation in humans during bed rest. Aviat Space Environ Med. 2003;74:37–46.
Kim SH, Jo SN, Myung HN, Jang JY. The effect of pre-existing medical conditions on heat stroke during hot weather in South Korea. Environ Res. 2014;133:246–52.
Cho WY. Exercise induced heat stroke and acute renal failure. Korean J Med. 2002;62:365–8.
Lee S-H, Yoo T-H, Kim B-H, K-g K. Exertional heat stroke: clinical characteristics and courses of 15 patients. Korean J Med. 2012;62:379–89.
Choi WJ, Jae Wook Lee JW, Lee SW. Exertional heat stroke in a young man with multi-organ dysfunction and fulminant pneumonia. Korean J Emerg Med. 2009;20:458–62.
Park SW, Cho YL, Oh DH, Choe JY, Jun HR. A case of heat stroke in an aluminium utensil plant. Korean J Occup Environ Med. 1999;11:293–303.
Na W, Jang JY, Lee KE, Kim H, Jun B, Kwon J-W, et al. The effects of temperature on heat-related illness according to the characteristics of patients during the summer of 2012 in the Republic of Korea. J Prev Med Public Health. 2013;46:19–27.
Kim H, Ha JS, Park J. High temperature, heat index, and mortality in 6 major cities in South Korea. Arch Environ Occup Health. 2006;61:265–70.
Lee WK, Lee HA, Park H. Modifying effect of heat waves on the relationship between temperature and mortality. J Korean Med Sci. 2016;31:702–8.
Lee S, Kim H, Yi SM. The relationships between temperature changes and mortality in Seoul, Korea. J Environ Health Sci. 2010;36:20–6.
Chung JY, Honda Y, Hong YC, Pan XC, Guo YL, Kim H. Ambient temperature and mortality: an international study in four capital cities of East Asia. Sci Total Environ. 2009;408:390–6.
Korea Occupational Safety and Health Agency. Statistics on workers’ compensation. 2015. Available from http://www.kosha.or.kr/mediaMain.do?menuId=6.
Korea Meteorological Administration Forum on Heat Wave: Still killer, current status and measures. 2015. Available from http://www.kma.go.kr/aboutkma/intro/hiw/heat/heat1.html.
Lee E, Park J, Kim H, Park M. Report on the development of Meterological information in Daily Living Life. Korea Meteorological Administration. 2016.
Buguet A. Sleep under extreme environments: effects of heat and cold exposure, altitude, hyperbaric pressure and microgravity in space. J Neurol Sci. 2007;262:145–52.
Haskell EH, Palca JW, Walker JM, Berger RJ, Heller HC. The effects of high and low ambient temperatures on human sleep stages. Electroencephalogr Clin Neurophysiol. 1981;51:494–501.
Okamoto-Mizuno K, Mizuno K. Effects of thermal environment on sleep and circadian rhythm. J Physiol Anthropol. 2012;31:14.
OSHA. Heat stress. In: OSHA technical manual, section III, 1999. Available from http://www.osha.gov/dts/osta/otm/otm_iii/otm_iii_4.html.
Havenith G. Heat balance when wearing protective clothing. Ann Occup Hyg. 1999;43:289–96.
Bernard TE, Barrow CA. Empirical approach to outdoor WBGT from meteorological data and performance of two different instrument designs. Ind Health. 2013;51:79–85.
ISO. Ergonomics of the thermal environment: estimation of thermal insulation and water vapour resistance of a clothing ensemble, Standard no. ISO 9920. Geneva: ISO; 2007.
Goldman RF. Clothing, its physiological effects, adequacy in extreme thermal environments, and possibility of future improvements. Arch Sci Physiol (Paris). 1973;27:137–47.
McCullough EA, Arpin EJ, Jones B, Konz SA, Rohles FH. Heat transfer characteristics of clothing worn in hot industrial environments. ASHRAE, Journal of the American Society of Heating Refrigerating and Air-Conditioning Engineers. 1982;88:1077–94.
Vogt JJ, Candas V, Libert JP. Graphical determination of heat tolerance limits. Ergonomics. 1982;25:285–94.
Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. American College of Sports Medicine position stand: exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39:556–72.
d'Ambrosio Alfano FR, Malchaire J, Palella BI, Riccio G. WBGT index revisited after 60 years of use. Ann Occup Hyg. 2014;58:955–70.
Arbury S, Jacklitsch B, Farquah O, Hodgson M, Lamson G, Martin H, et al. Heat illness and death among workers: United States, 2012–2013. MMWR Morb Mortal Wkly Rep. 2014;63:661–5.
Navy Environmental Health Center. Prevention and treatment of heat and cold stress injuries, Technical manual NEHC-TM-OEM 6260.6A. Navy Environmental Health Center, Bureau of Medicine and Surgery: Portsmouth; 2007. Available from http://www.public.navy.mil/surfor/Documents/6260_6A_NMCPHC_TM.pdf.
Pandolf KB, Burse RL, Goldman RF. Role of physical fitness in heat acclimatization, decay and reinduction. Ergonomics. 1977;20:399–408.
Yeargin SW, Casa DJ, Armstrong LE, Watson G, Judelson DA, Psathas E, et al. Heat acclimatization and hydration status of American football players during initial summer workouts. J Strength Cond Res. 2006;20:463–70.
NIOSH. Criteria for a recommended standard: occupational exposure to hot environments. Cincinnati: U.S. Department of Health, Education, and Welfare, Health Services and Mental Health Administration, National Institute for Occupational Safety and Health, DHEW (NIOSH) Publication No. HSM 72–10269; 1972.
NIOSH. Criteria for a recommended standard: occupational exposure to hot environments: revised criteria. Cincinnati: U.S. Department of Health and Human Services, Centers for Disease Control, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 86–113; 1986.
AIHA. In: 2nd, editor. The occupational environment: its evaluation, control, and management. Fairfax: AIHA Press; 2003.
Gabriel KMA, Endlicher WR. Urban and rural mortality rates during heat waves in Berlin and Brandenburg, Germany. Environ Pollut. 2011;159:2044–50.
ISO. Ergonomics: evaluation of thermal strain by physiological measurements, Standard no. ISO 9886. Geneva: ISO; 2004.
Acknowledgements
This work was supported by Korea Occupational Safety and Health Agency (Grant number: 2015-OSHRI-1081) and Korea Meteorological Administration (The Study on the Development and Service Improvement of Meteorological Information in Daily Living Life, 2016).
Funding
This work was supported by Korea Occupational Safety and Health Agency (Grant number: 2015-OSHRI-1081) and Korea Meteorological Administration (The Study on the Development and Service Improvement of Meteorological Information in Daily Living Life, 2016). We declare no roles of the funding body in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
Not applicable.
Authors’ contributions
Conception and design of the work: Park J, Kim Y. The acquisition and interpretation of data for the work: Park J, Oh I. Drafting the work; Park J. Revising it critically for important intellectual content; Kim Y. Final approval of the version to be published; Kim Y. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; Kim Y. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Park, J., Kim, Y. & Oh, I. Factors affecting heat-related diseases in outdoor workers exposed to extreme heat. Ann of Occup and Environ Med 29, 30 (2017). https://doi.org/10.1186/s40557-017-0183-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40557-017-0183-y