Abstract
Introduction
The COVID-19 pandemic globally impacted healthcare provision. Prescribing changes in common medications can be used as a marker for new diagnoses. We describe how the prescribing of specific psychotropics was impacted by the pandemic.
Methods
Primary Care Prescribing data for different classes of drugs from March 2017 to February 2022 were considered. To capture the impact during periods of restricted access to health services for new diagnoses/existing conditions, repeat prescriptions/episodic prescribing were included with account taken of historical trends.
The pre-pandemic prescriptions issued each month from March 2018 to February 2020 were linearly extrapolated forward to give an expected annual growth (EAG). The monthly average expected prescriptions for the pandemic period (March 2020–February 2022) were compared.
Results
Physical health medications had lower monthly prescriptions during the pandemic, most markedly for antibiotics − 12.5% (EAG − 1.3%). Bronchodilator prescribing showed a marked increase in the early pandemic months from March 2020 of 5% (EAG 0.1%). Mental health medication prescribing increased above trend for hypnotics/anxiolytics by 0.2% (EAG − 2.3%), while antidepressants fell by − 0.2% (EAG 5.0%), with no net change for antipsychotics (EAG 2.8%), but a temporary increase in antipsychotic prescribing in the early pandemic period. For all the main antidepressants prescribed in England (Sertraline, Mirtazapine, Venlafaxine, Fluoxetine and Citalopram), prescribing actually decreased in the main pandemic period vs historical trend.
Conclusions
The increase in anxiolytic/hypnotic prescribing above trend links to pandemic effects on anxiety/worry. If anything, there was a slight fall in prescribing of the main antidepressants prescribed, which given prevailing circumstances at the time, suggests that access to services may have restricted access to timely assessment.
Similar content being viewed by others
Background
First appearing in late 2019, Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the causative pathogen of Coronavirus disease (COVID-19), and the COVID-19 pandemic [1]. Although the exact origin of COVID-19 is debated, in 2007, Cheng CC et al. forewarned that “the large reservoir of SARS-CoV-like viruses in horseshoe bats, together with the culture of eating exotic mammals in southern China, is a time bomb” [2]. The WHO approximated 14.9 million excess deaths as a result of this global crisis [3]. Although approaches to controlling the virus differed between countries [4], as national lockdowns became widespread worldwide, healthcare provision in relation to both physical and mental healthcare demands was greatly impacted [5, 6], with the effects still being felt globally.
In this study, our aim was to determine how psychotropic prescribing in England in Primary Care was affected by the COVID-19 pandemic, and in addition, compare this to specific other medication groups used to treat physical disorders. Changes in prescribing of commonly used medication can be used as a marker for both diagnoses of new patients and levels of service for existing patients in Primary Care [7, 8].
Although a number of publications have described the consequences of the COVID-19 pandemic in relation to the incidence of depression and other mental health issues [9], the matter of how much the prescribing of specific psychotropic medications was impacted by the pandemic and the tectonic changes in the way that millions of people in developed healthcare systems interacted with their general practices have been less explored.
In relation to this question, we here describe an analysis of prescribing data for all of England in the time before, during and after the main impact period of the COVID-19 pandemic. Making this topic even more relevant is the seeming mental health crisis that was born from this pandemic, whether that be from the direct impact of the virus on mental health itself, or from more indirect and insidious causes, such as the loss of loved ones and feelings of isolation brought on from lockdowns [4]. However, it was reported by Bourmistrova et al., that although SARS-CoV-2 infection was associated with deteriorating mental health in the short term, the long-term prevalence of psychiatric illnesses, including anxiety, depressive disorders, post-traumatic stress disorder (PTSD) and sleep disturbance, is not significantly different to that of the general population [10].
Methods
Prescription Cost Analysis (PCA) is a National Statistic in England, providing details of the total number of items and the Net Ingredient Cost (NIC) of all prescriptions dispensed in the community. Data from 2017 to 2022 (6 years) was downloaded by BNF section. Medications were broken down by the British National Formulary (BNF) into 15 chapters and 105 sections. Chapter 4 central nervous system includes three sections which are taken as psychotropic 4.01 hypnotics and anxiolytics, 4.02 drugs used in psychoses and related disorders and 4.03 Antidepressants [11].
Medications that were on repeat prescriptions and those with episodic patterns were included. The percent change between the start and end year showed how psychotropic medication had performed compared to total medications.
Different classes of medication are growing and falling at different rates and account was taken of this in our analysis, regarding how the trends in prescribing of psychotropic vs physical medication might differ, to capture the impact during periods of restriction of access to health services for new diagnoses/existing conditions.
A selection of physical and mental health medication British National Formulary (BNF) code classes were selected and the number of prescriptions issued each month in Primary Care was downloaded from the English Prescribing data set [12]. Calculation of the monthly rolling total for the previous 12 months was taken to remove short-term fluctuation effects.
The rolling annual total pre-pandemic prescriptions issued each month from March 2018 to Feb 2020, were linearly extrapolated forward to give an expected annual growth (EAG) and then provide estimates over the pandemic period.
From this, the monthly average expected prescriptions for the pandemic period Mar 2020–Feb 2022 were calculated and compared to the actual average.
To evaluate in more detail the impact on anti-depressants, the same evaluation was carried out on the top six prescribed medications.
Ethics approval was not sought as the analysis used publically available aggregated data.
Results
The medication part of Prescription Cost Analysis (PCA) showed in 2022 a total of 1.12 billion prescriptions at net ingredient costs of £8.83 billion were issued within Primary Care in England and these have increased 5.0% in number and 7.5% in costs in the 5 years since 2017. These three psychotropic sections had 112 million prescriptions issued (10.1% of total medication).
Table 1 shows the top 25 BNF classes by number of prescriptions and anti-depressants have increased by 26% to become the most prescribed class in 2022.
Figure 1 shows the rolling monthly trend for major physical health and mental health classes the number reflects the BNF class and the 100% = figure represents the monthly average prescription over the initial 12-month period, i.e., approximates to the number of patients being treated. The coloured sections reflect the periods when social restrictions were enforced during the COVID-19 pandemic—this included access to Primary Care for face-to-face appointments.
Relative development in Primary Care prescribing mental and physical health medication before and over the pandemic. Shows a rolling previous 12 month total prescriptions by medication class for each month, against the linear extrapolation based on the previous 3 years 2017 to 2019. Results are standardised to the values for the year April 2017_March 18. The time intervals of the main England lockdowns are shown
The following prescribing trends for BNF classes are based on the assumption that for long-term conditions patients are receiving one prescription per month;
Antidepressants started with around 5.7 million people on therapy and decreased slightly over the main pandemic period. Drugs for psychoses started with 1 million people on therapy, increased slightly during the social restrictions but have fallen back onto the trend. Hypnotics and Anxiolytics started with 1.2 million on therapy (decreasing EAG), grew slightly during lockdowns and have now returned to the trend. Lipid-regulating drugs started with 6.1 million on therapy, increased slightly over lockdown but have fallen back. Beta blockers started with 3.2 million on therapy increased during the first lockdown and have since then stopped growing. ACEI and ARBs (Hypertension and Heart Failure) with 6 million on therapy increased over the lockdowns and have since then declined. Bronchodilators started with 2.6 million on therapy, increased sharply over the 1st lockdown and then fell sharply in the 2nd lockdown. Antibiotics started with 2.8 million on therapy (falling EAG) due to the ongoing national antibiotic stewardship program to reduce unnecessary prescribing, fell sharply during the pandemic but are now recovering.
Table 2 compares the actual mental and physical health prescribing to the extrapolation of historical trends to show what might have been expected if there had been no pandemic and the difference to the actual average over the 24-month pandemic main period as a % of the expected prescribing.
Compared to declines in physical health prescribing, mental health prescribing of hypnotics/anxiolytics increased by 0.2% above the trend in 2020 and 2021. There was a slight fall in antidepressant prescribing (− 0.2%) in the same period. Antipsychotic prescribing overall kept on-trend.
Physical health medications had lower monthly prescriptions during the pandemic most markedly for antibiotics − 12.5% (EAG − 1.3%). Bronchodilator prescribing showed a marked increase in the early pandemic period from March 2020 of 5% (EAG 0.1%).
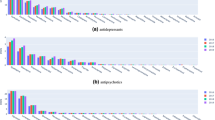
The 6 main antidepressant medications which together take up 88% of total anti-depressant prescriptions were investigated and results are shown in Fig. 2.
The following trends for individual antidepressants are based on the assumption that patients are receiving one prescription per month;
SSRI-Sertraline was used by 1.1 million individuals and was the fastest-growing pre-pandemic. The growth rate reduced during the lockdown and has not recovered to expected levels. Mirtazapine was used by 700,000 people and growth fell during the lockdown but has now recovered back to expected levels. Venlafaxine was used by 350,000 people and the growth rate was reduced during the lockdown and has not recovered to expected levels. Tricyclic Amitriptyline was used by 1.1 million individuals and growth was reduced in lockdown but has now recovered higher than could be expected. SSRI Fluoxetine was used by 550,000 million people and growth was reduced slightly in lockdown but has now recovered higher than could be expected. SSRI Citalopram was used by 1.2 million individuals and was declining before the pandemic fell slightly during lockdown but has now recovered back to higher than could be expected.
Thus for all the main antidepressants prescribed in England (Sertraline, Mirtazapine, Venlafaxine, Fluoxetine and Citalopram), prescribing actually decreased in the main pandemic period vs historical trend.
Net absolute changes for the three main antidepressants over the period analysed were: Sertraline grew by 21% so its share of total anti-depressants increased from 22.7% to 24.6% (+ 8%); Mirtazapine grew by 16% so share increased from 13.0% to 13.6% (+ 5%); Venlafaxine grew by 11% so share stayed at 6.3% (0%).
Discussion
The increase in anxiolytic/hypnotic prescribing above (Table 1 and Fig. 1) may reflect the impact of the COVID-19 pandemic on the levels of anxiety and worry experienced by many individuals. This observation is supported by the findings of Jacob et al. [13] who reported an increase in the number of patients newly diagnosed with anxiety disorder and Estela et al. [8] who described an increasing trend throughout the pandemic in the prescription of anxiolytics, sedatives, and hypnotics. We suggest that this reflects the experience of many people who have lived through the COVID-19 pandemic.
The increased impact of the COVID-19 pandemic on mental health rather than physical health has been well-described [9]. However, there was no increase in antidepressant prescribing above trend (if anything there was a slight fall in prescribing of the main antidepressants prescribed for much of the main pandemic period) (Fig. 2), which given prevailing circumstances at the time, suggests that access to services may have restricted access to assessment [4]. This is supported by Goyal et al., who also reported that instead of being seen by a healthcare professional, patients seeking a consultation for breathlessness were only given automated safety advice [14]. The fall in antibiotic prescribing in addition to the trend, reflects a combination of reduced access to services [15], particularly face-to-face general practice consultations, limited episodic prescribing, and also the wearing of face masks [10] which would have reduced the transmission of respiratory pathogens. Finally, the precipitate increase in bronchodilator prescriptions at the beginning of the COVID-19 pandemic likely reflects the high level of population anxiety re. becoming seriously unwell with acute COVID-19 prevalent at that time [11], in the first of all England lockdowns.
There was an increase in antipsychotic prescribing in the early phase of the pandemic which may relate to the use of antipsychotics to manage behavioural challenges in people with cognitive impairment in residential care home settings [12]. Specifically, the authors of this paper reported that the proportion of patients with dementia who were prescribed antipsychotics through 2020 substantially increased compared to the years immediately prior to 2020, when the proportion of patients with dementia who were prescribed antipsychotics had tended to be constant. This is evidenced by Yan et al., who reported that in the U.S, antipsychotic use increased among nursing home residents, especially those who are of a minority background [16].
The increase in prescriptions of Sertraline and Mirtazapine over time likely reflects the individual preference of general practitioners as there is no specific recommendation for their use vs other agents in BNF/NICE guidance [13]. The antidepressant prescribing practice seen here is not in keeping with NICE Guidelines with respect to the increased use of Venlafaxine—a 3rd line drug in current and previous guidance. The use of Amitriptyline is, of course, most likely to be for chronic pain rather than depression [17]. The popularity of Mirtazapine is surprising given its sedative effects and propensity for weight gain in individuals who take it regularly. However, general practitioners may also prefer mirtazapine when treating patients with psychiatric disturbance and co-morbid insomnia, due to these sedative effects [18].
Going forward, a person and clinician focussed evaluation of the individual experience of the pandemic in relation to how access to general practice has influenced the prescription of antidepressants and anxiolytics may illuminate why we observe these prescribing trends. This is anticipated to be the next step of our work.
Strengths/limitations
We have been able to access national-level aggregated data for this analysis. We accept that this does not take into account differences between individual general practices in relation to access to services, nor does it take into demographic factors in relation to access to care and incident mental health issues during the COVID-19 pandemic. We also accept that our analysis cannot differentiate new from repeat prescriptions.
Conclusions
The increase in anxiolytic/hypnotic prescribing above trend links to pandemic effects on anxiety/worry. If anything there was a slight fall in prescribing of the main antidepressants prescribed, which given prevailing circumstances at the time, suggests that access to services may have restricted access to timely assessment. The increased bronchodilator prescribing in the early pandemic period likely reflects concerns in asthma sufferers regarding the potential effects of COVID-19 infection.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- EAG:
-
Expected annual growth
- COVID-19:
-
SARS-CoV-2
- BNF:
-
British National Formulary
- SSRI:
-
Selective serotonin reuptake inhibitor
- NICE:
-
National Institute for Health and Care Excellence
References
Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–20. https://doi.org/10.1177/0020764020915212.
Sinnott SJ, Smeeth L, Williamson E, Douglas IJ. Trends for prevalence and incidence of resistant hypertension: population based cohort study in the UK 1995–2015. BMJ. 2017;22(358): j3984. https://doi.org/10.1136/bmj.j3984.
Heald AH, Stedman M, Davies M, Livingston M, Taylor D, Gadsby R. Antidepressant prescribing in England: patterns and costs. Prim Care Companion CNS Disord. 2020;22(2):19m02552.
COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–12. https://doi.org/10.1016/S0140-6736(21)02143-7.
OpenPrescribing.net, Bennett Institute for Applied Data Science, University of Oxford.
English Prescribing monthly dataset https://opendata.nhsbsa.net/dataset/english-prescribing-data-epd: accessed 22 July 2022.
Mansfield KE, Mathur R, Tazare J, Henderson AD, Mulick AR, Carreira H, Matthews AA, Bidulka P, Gayle A, Forbes H, Cook S, Wong AYS, Strongman H, Wing K, Warren-Gash C, Cadogan SL, Smeeth L, Hayes JF, Quint JK, McKee M, Langan SM. Indirect acute effects of the COVID-19 pandemic on physical and mental health in the UK: a population-based study. Lancet Digit Health. 2021;3(4):e217–30. https://doi.org/10.1016/S2589-7500(21)00017-0.
Jacob L, Smith L, Koyanagi A, Oh H, Tanislav C, Shin JI, Konrad M, Kostev K. Impact of the coronavirus 2019 (COVID-19) pandemic on anxiety diagnosis in general practices in Germany. J Psychiatr Res. 2021;143:528–33. https://doi.org/10.1016/j.jpsychires.2020.11.029.
Estrela M, Silva TM, Gomes ER, Piñeiro M, Figueiras A, Roque F, Herdeiro MT. Prescription of anxiolytics, sedatives, hypnotics and antidepressants in outpatient, universal care during the COVID-19 pandemic in Portugal: a nationwide, interrupted time-series approach. J Epidemiol Community Health. 2022;76(4):335–40. https://doi.org/10.1136/jech-2021-216732.
Heald AH, Stedman M, Tian Z, Wu P, Fryer AA. Modelling the impact of the mandatory use of face coverings on public transport and in retail outlets in the UK on COVID-19-related infections, hospital admissions and mortality. Int J Clin Pract. 2021;75(3):e13768. https://doi.org/10.1111/ijcp.13768.
Daly M, Robinson E. Depression and anxiety during COVID-19. Lancet. 2022;399(10324):518. https://doi.org/10.1016/S0140-6736(22)00187-8.
Howard R, Burns A, Schneider L. Antipsychotic prescribing to people with dementia during COVID-19. Lancet Neurol. 2020;19(11):892. https://doi.org/10.1016/S1474-4422(20)30370-7.
https://bnf.nice.org.uk/treatment-summaries/antidepressant-drugs: accessed 22 July 2022.
Goyal DK, Mansab F, Naasan AP, Iqbal A, Millar C, Franklin G, Thomas S, McFadden J, Burke D, Lasserson D. Restricted access to the NHS during the COVID-19 pandemic: is it time to move away from the rationed clinical response? Lancet Reg Health Eur. 2021;8: 100201. https://doi.org/10.1016/j.lanepe.2021.100201.
Pujolar G, Oliver-Anglès A, Vargas I, Vázquez ML. Changes in Access to Health Services during the COVID-19 pandemic: a scoping review. Int J Environ Res Public Health. 2022;19(3):1749. https://doi.org/10.3390/ijerph19031749.
Yan D, Temkin-Greener H, Cai S. Did the COVID-19 pandemic affect the use of antipsychotics among nursing home residents with ADRD? Am J Geriatr Psychiatry. 2023;31(2):124–40. https://doi.org/10.1016/j.jagp.2022.09.009.
Umaharan T, Sivayokan S, Sivansuthan S. Amitriptyline dependence and its associations: a case report and literature review. Case Rep Psychiatry. 2021;29(2021):6647952. https://doi.org/10.1155/2021/6647952.
Alam A, Voronovich Z, Carley JA. A review of therapeutic uses of mirtazapine in psychiatric and medical conditions. Prim Care Companion CNS Disord. 2013. https://doi.org/10.4088/PCC.13r01525.
Acknowledgements
There are no specific acknowledgements.
Funding
The authors received no funding from an external source.
Author information
Authors and Affiliations
Contributions
All authors contributed equally and substantially to the co-creation and writing of this paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
No author has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Waheed, U., Stedman, M., Davies, M. et al. Changes in prescribing of psychotropic vs some physical health medication in primary care through the COVID-19 pandemic in England: a national-level survey. J of Pharm Policy and Pract 16, 169 (2023). https://doi.org/10.1186/s40545-023-00655-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40545-023-00655-9