Abstract
Neurodegenerative diseases encompass a heterogeneous group of conditions characterised by the progressive degeneration of the structure and function of the central or peripheral nervous systems. The pathogenic mechanisms underlying these diseases are not fully understood. However, a central feature consists of regional aggregation of proteins in the brain, such as the accumulation of β-amyloid plaques in Alzheimer’s disease (AD), inclusions of hyperphosphorylated microtubule-binding tau in AD and other tauopathies, or inclusions containing α-synuclein in Parkinson’s disease (PD), dementia with Lewy bodies (DLB) and multiple system atrophy (MSA). Various pathogenic mechanisms are thought to contribute to disease, and an increasing number of studies implicate dysfunction of oligodendrocytes (the myelin producing cells of the central nervous system) and myelin loss. Aberrant DNA methylation, the most widely studied epigenetic modification, has been associated with many neurodegenerative diseases, including AD, PD, DLB and MSA, and recent findings highlight aberrant DNA methylation in oligodendrocyte/myelin-related genes. Here we briefly review the evidence showing that changes to oligodendrocytes and myelin are key in neurodegeneration, and explore the relevance of DNA methylation in oligodendrocyte (dys)function. As DNA methylation is reversible, elucidating its involvement in pathogenic mechanisms of neurodegenerative diseases and in dysfunction of specific cell-types such as oligodendrocytes may bring opportunities for therapeutic interventions for these diseases.
Similar content being viewed by others
Introduction
Neurodegenerative diseases form a diverse group of neurological disorders which are characterised by progressive degeneration of the structure and function of the central or peripheral nervous system accompanied by loss of neurons. Despite the extensive accumulation of evidence and proposal of multiple pathogenic mechanisms, there is much to learn about how these disorders develop and progress. Many studies to date have focused on neuronal cells [33, 36]. Less is understood of the involvement of oligodendrocytes (OLGs), which are a major type of glial cells in the central nervous system (CNS). The primary function of OLGs is to produce myelin, and there is growing evidence which implicates myelin changes and OLG dysfunction across several neurodegenerative diseases [7, 14, 25, 77, 79, 87, 102]. In support of these changes not being mere downstream consequences of disease, multiple genome-wide association studies (GWAS) have identified genetic variants in myelin/OLG-related genes such as MOBP as being associated with the risk of multiple neurodegenerative diseases [18, 41, 46, 54, 59, 85, 88]. However, a more holistic view of mechanisms underlying OLG malfunction in neurodegeneration is far from being fully elucidated.
Changes to the epigenome have been consistently associated with neurodegenerative diseases in recent years [4, 73, 91, 99, 118]. By inducing chromatin changes, epigenetic mechanisms can regulate gene expression without changing the underlying genetic sequence. These epigenetic mechanisms include DNA methylation, which is the most widely studied, and histone modifications such as acetylation [73]. Although epigenetic modifications are crucial for the functioning of the cells and are involved in processes such as genomic imprinting and tissue differentiation, they also relate to the development of disease [67, 73]. Of interest to the topic to be discussed in this review, studies highlighting cell-type specific epigenetic changes [91], including in OLGs, started to emerge in the field of neurodegeneration. Although at its infancy, such studies are much needed to fully understand cell-type specific contributions to disease processes.
In this review, we highlight evidence which implicates the (dys)function of OLGs and myelin in neurodegeneration, and discuss how epigenetic modifications such as DNA methylation are crucial for OLG life cycle and myelination and how this could be affected in disease.
The importance of the oligodendrocyte lineage and the myelin in the healthy brain
OLGs are a major glial cell type in the CNS, which constitute around 75% of the CNS glial cell population [80]. OLGs are responsible for the production, stability, and maintenance of myelin [14], the lipid-rich, multilamellar membrane which wraps around axons and enables fast transmission of electrical signals. Structurally, the myelin sheath is an extension of the OLG plasma membrane that wraps around nerve axons in a concentric fashion [102]. The myelin sheath is not continuous along the neuron. Sections of myelinated axon are separated by nodes of Ranvier. These enable saltatory conduction, the ‘hopping’ of electrical impulses along axons, which allows for fast transmission of electrical signals. The importance of the myelin sheath is demonstrated by the consequences of its loss, notably in demyelinating diseases such as multiple sclerosis (MS), where it results in a range of neurological symptoms including visual, motor and sensory problems, with associated disability and reduced life expectancy [20]. OLGs are also involved in homeostasis, trophic support to neurons, provision of lactate to neurons, and the secretion of various growth factors [26].
OLGs arise from oligodendrocyte precursor cells (OPCs), which are characterised by the expression of PDGFR-α (platelet derived growth factor receptor α) and NG2 (neuron-glial antigen 2) [107]. It is known that OPCs, which arise in the ventricular zone during early development [106, 108, 110], proliferate and migrate, and differentiate in stages [56] into myelinating OLGs (Fig. 1). Although most OPCs differentiate to form myelinating OLGs, some OPCs are retained in their proliferative stage. This results in OPCs accounting for 5–10% of all adult brain cells [22]. The main role of adult OPCs is to provide a source of new mature, myelinating OLGs. However, recent studies show they also have other important roles, including their involvement in cell signalling, metabolic regulation and as immune modulators [28, 52, 76]. The maturation of OPCs into OLGs, although relatively well characterised in mice, is not well described in humans given the technical challenges of studying post-mortem brain tissue and/or limitations of current human OLG-like cell lines.
Schematic representation of the stages of OLG lineage differentiation. OPCs (PDGFRαhigh/NG2+) arise from NPCs (A2B5+), before forming mature OLGs (O4+/CNP+/CC1+) and then myelinating OLGs (MOG+/MAG+/MBP+/CC1+/PLP+). NPC Neural progenitor cell, OLG Oligodendrocyte, OPC Oligodendrocyte precursor cell. Figure created with BioRender
A role for myelin and oligodendrocytes in neurodegenerative diseases
The involvement of myelin changes in neurodegeneration
Myelination is a dynamic process that continues throughout life. Most myelination takes place from early childhood through to adolescence, with the major part taking place in the first two years of life. However, myelination does continue into adulthood, followed by an age-related decline in myelination occurring around the sixth decade of life (Fig. 2) [29]. However, decreases in myelin with ageing are not uniform, with regions of the brain that are myelinated earlier in development (such as the primary motor and sensory regions) undergoing white matter decline later [87].
Schematic of the myelin changes throughout life. Shaded areas indicating myelination waves (as defined by de Faria et al. [29]). Also depicted are visualizations of the progression of cortical myelination and the progression of Alzheimer’s disease related destruction. The average age of onset of multiple neurodegenerative diseases is also indicated and coincides with the start of normal ageing-related decline in myelination, which is hypothesized to be accelerated in neurodegeneration. Figure created with BioRender
Although neurodegenerative diseases such as Alzheimer’s disease (AD) are mainly associated with grey matter and neuronal damage, there is evidence for decline and involvement of white matter during disease progression. Disruption of myelin in AD was described at the beginning of the twentieth century by Alois Alzheimer [79]. It has also been noted that the typical age-of-onset of neurodegenerative diseases coincides with the time when age-related decline in myelination is observed (Fig. 2) [29]. Moreover, early evidence of the disruption of myelin in AD suggested those regions of the cortex, such as the temporal and frontal lobes, that are myelinated later in development are more likely to present with AD pathology earlier [13, 79]. This suggests that those regions that myelinate later are more vulnerable to pathogenic mechanisms which result in neurodegeneration. Further evidence of this involvement of myelin comes from the observations of white matter changes in brain imaging studies. For example, white matter hyperintensities (WMHs), which are associated with loss of myelin integrity, have been shown to predict incident AD [15, 16, 77]. Brain imaging data has indicated that β-amyloid deposition may change white matter microstructure in early disease stages [23]. White matter abnormalities and myelin degradation are also described in other neurodegenerative diseases, including multiple system atrophy (MSA) [64], amyotrophic lateral sclerosis (ALS) [121] and progressive supranuclear palsy (PSP) [27, 114].
The involvement of the oligodendrocyte lineage in neurodegeneration
Evidence from pathology
A direct role for OLGs in neurodegenerative disease is exemplified by the pathology of MSA, where glial cytoplasmic inclusions (GCIs) in OLGs are the pathological hallmark of the disease [49]. In MSA, these inclusions consist of aggregates of the synaptic protein α-synuclein. Whether α-synuclein is produced by the OLGs or propagated from neurons is not clear. In MSA, increased number of OPCs is also reported in post-mortem brain tissue [1, 65]. PSP and corticobasal degeneration (CBD) also display clear OLG pathology with disease hallmarks including tau deposits in OLGs, presenting as coiled bodies [24, 53].
Although the precise role of OLGs in AD pathology is less clear, there is evidence from human post-mortem studies that there are alterations in the numbers and morphology of OLG lineage cells in this disease [77]. In post-mortem AD brain tissue, decreases in Olig2 + cells have been reported [8], as well as increased numbers of OPCs in white matter lesions [93]. Morphological changes in OLGs derived from AD post-mortem brains have also been seen, specifically a decrease in nuclear diameter in parahippocampal white matter [34]. A recent study, in apolipoprotein E-ε4 allele (APOE-ε4) carriers, also demonstrated aberrant deposition of cholesterol in OLGs and dysregulated myelination in AD [12].
Evidence from genetics
GWAS have also implicated specific myelin/OLG-related genes in neurodegeneration, including the bridging integrator 1 (BIN1) gene, which is the second strongest genetic risk factor for late onset AD [45, 57, 58] and known to be largely expressed by mature OLGs and localised to white matter tracts [86]. Increased expression of BIN1 is reported in AD [17], although mechanisms behind the association of BIN1 and AD are unclear. Myelin associated oligodendrocyte protein (MOBP) gene has been associated with disease risk in several neurodegenerative diseases, including PSP [19, 41, 88], CBD [54], AD APOE-ε4 carriers [59], ALS [85] and PD [95], and has also been reported to be associated with white matter degradation and increased rates of decline in executive function in behavioural variant frontotemporal dementia [46]. The functional repercussions of such associations remain unclear. However, in human brain tissue, the risk allele T, of the disease-associated single nucleotide polymorphism rs1768208, is also associated with increased expression of the MOBP gene in PSP [2].
Aside from such examples of myelin/OLG relevant genes identified through GWAS, transcriptomic analyses reveal gene expression changes in additional myelin-related genes in a broad range of neurodegenerative diseases, including AD [3], PSP [3], MSA [82], and frontotemporal lobar degeneration (FTLD) [39], further supporting the idea of myelination changes as a common pathway across these diseases. Examples of evidence supporting the importance of OLG/OPC involvement across several neurodegenerative diseases are given in Fig. 3.
Non-exhaustive summary of evidence implicating the oligodendrocyte lineage across neurodegenerative diseases. AD—Alzheimer’s disease, ALS—Amyotrophic lateral sclerosis, BIN1—Bridging Integrator 1, CBD—Corticobasal degeneration, FTD—Frontotemporal dementia, GCI – Glial cytoplasmic inclusion, MSA—Multiple System Atrophy, MOBP—Myelin-associated oligodendrocyte protein, OLG—Oligodendrocyte, OPC—Oligodendrocyte precursor cell, PSP—Progressive supranuclear palsy. Figure created with BioRender
A role for DNA methylation in the dysfunction of oligodendrocytes and myelin in neurodegenerative diseases
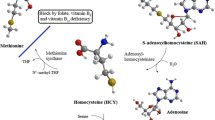
Epigenetic modifications are those which, without altering the underlying DNA sequence, bring around changes in gene expression. DNA methylation, the most widely studied epigenetic modification, involves the transfer of a methyl group to a cytosine nucleotide to form 5-methylcytosine (5mC) [66] (Fig. 4a). This transfer is catalysed by a family of enzymes called DNA methyltransferases. The effect DNA methylation on gene expression regulation is largely dependent upon genomic location [37, 66]. For example, methylation within the gene body, i.e. protein coding exons and introns, more often results in increased gene expression, whereas methylation in the promoter region frequently leads to decreased gene expression [60, 78, 109]. DNA methylation, along with other epigenetic modifications, allow the intricate spatiotemporal control of gene expression and is crucial both during development and adult life. DNA methylation has been implicated in many processes relevant for the brain, including in brain development, learning, memory, and brain cell-type specification [48]. DNA hydroxymethylation (5hmC), an oxidative derivative of DNA methylation (Fig. 4a), is also important. Having originally been presumed to be an intermediate mark before demethylation [38], evidence now supports a functional role for 5hmC [103]. Interestingly, the distribution of different methylation states varies in a tissue dependent manner, with 5hmC known to be enriched tenfold in human brain compared to peripheral tissues [35]. Distribution of 5mC and 5hmC between brain cell-types has also been reported to be variable, with studies indicating that 5hmC may be enriched in neuronal cells compared to OLGs [55, 72]. Notwithstanding, Fig. 5 shows 5mC and 5hmC immunopositive glial nuclei, including OLG nuclei, in human post-mortem white matter tissue.
Schematic representation of the DNA modifications cycle, including factors responsible for the transitions between states. a Overall DNA modifications cycle; b Diagram summarising the known involvement of DNMTs and TET enzymes in OLG differentiation, developmental myelination, and in remyelination in response to injury. Evidence shows an age dependent role for DNMT1 and DNMT3A, with the former suggested to be more important in developmental myelination, and the latter in the remyelination involving differentiation of adult OPCs [68, 71]. Whilst it has been suggested that all three TET enzymes are involved in oligodendrocyte differentiation [120], TET1 has been reported to be more important for myelination and remyelination after injury [38, 69]. DNMT1/3A/3B—DNA methyltransferase 1/3A/3B, TET—ten-eleven translocation enzymes, TDG—thymine DNA glycosylase. Figure created with BioRender
Immunohistochemical analysis of global DNA (hydroxyl)methylation in human post-mortem cerebellar white matter tissue. Positive staining in nuclei of glial cells, including oligodendrocytes, is shown in brown (scale bar 100 µm). a 5‐Methylcytosine (5mC) immunohistochemical staining; b 5‐Hydroxymethylcytosine (5hmC) immunohistochemical staining
Studies using immunodetection of 5mC or 5hmC have often failed to lead to consensus regarding the occurrence of global DNA methylation/hydroxymethylation changes in neurodegenerative diseases, possibly reflecting limitations of such techniques [5, 73, 113]. However, technological advances that allowed querying throughout the genome at specific sites, have empowered investigations of relevant candidate genes and epigenome-wide association studies (EWAS) to identify DNA methylation alterations in neurodegenerative diseases at the single nucleotide resolution. In AD, EWAS studies utilising bulk brain tissue have identified multiple genes with DNA methylation changes associated with the disease and its pathological burden [47, 61, 98, 111], and meta-analyses have identified significant changes across multiple brain regions [91, 96, 99, 118]. Differentially methylated genes have also been identified in bulk brain tissue EWAS in other neurodegenerative diseases such as PD [51, 63], PSP [112], MSA [10], FTLD [31] and Huntington’s disease [43, 100]. DNA methylation changes in AD and movement disorders (including PD, HD, PSP and MSA) have been reviewed by Smith et al. [96] and Murthy et al. [73], respectively.
Whilst most DNA methylation studies employ ‘bulk’ tissue analysis, more recent studies exploring DNA methylation changes in neurodegeneration have investigated cell-specific alterations. Shireby and co-workers investigated AD-related DNA methylation signatures in purified brain nuclei and found that many AD-related DNA methylation changes that had previously been detected in ‘bulk’ tissue were indeed driven by changes in non-neuronal cells, including in OLGs [91]. This finding highlights the need of a deeper understanding of DNA methylation changes in OLGs which may also occur in other neurodegenerative diseases. Below, we discuss several lines of evidence that support DNA methylation having a role in the dysfunction of OLGs and myelin in neurodegenerative diseases. These are summarised in Fig. 6.
Potential roles for DNA methylation in the dysfunction of oligodendrocytes and myelin in neurodegenerative diseases. Panels illustrate different lines of evidence that implicate DNA methylation changes affecting OLGs/OLG-related genes and their relevance to neurodegeneration. BIN1—Bridging interactor 1, MOBP—Myelin associated oligodendrocyte protein, OPC—Oligodendrocyte precursor cell, OLG—Oligodendrocyte, ROS—Reactive oxygen species. Figure created with BioRender
DNA methylation plays a crucial role in determining the fate of OPCs in health and neurodegenerative diseases
Gene expression changes determined by DNA methylation play an important role in the process of lineage specification from OPCs to mature OLGs [68, 105]. Although most studies investigating the OLG life cycle have been conducted in animal models, there is significant evidence to suggest that DNA methyltransferases and DNA methylation are dynamic in the processes of OPC specification, survival, proliferation, differentiation, and myelination [68, 70, 83, 104, 105]. Proliferation of OPCs occurs in response to exogenous signals such as growth factors, and epigenetic modifications are important players in this regulation. In mice, ablation of DNA methyltransferases has been shown to result in a hypomyelinating phenotype through reduction in the OPC progenitor pool due to impaired OPC proliferation [70]. During differentiation of OPCs to OLGs in mice, lower DNA methylation levels in myelin genes and increased methylation levels in cell cycle and neuronal genes were reported [70]. Given that the majority of the DNA methylation sites (CpGs) investigated in these studies were in promoter regions, and given the association of promoter region DNA hypermethylation with decreased gene expression, this supports an important role for DNA methylation in silencing cell cycle and proliferation genes and in activating myelin genes, thus enabling OPCs to leave their proliferative state and differentiate into myelinating OLGs. DNA methylation of specific genes involved in OPC differentiation has also been described. The DNA-binding protein inhibitors Id2 and Id4 showed decreased expression during OPC differentiation in mice, which was correlated with hypermethylation of their promoter regions, suggesting a role for DNA methylation in the silencing of these genes to allow the expression of myelin genes during differentiation [104]. As described in MSA and AD brain tissue, the increased number of OPCs observed [26, 65, 93] could be reflective of an inability of the OPCs to mature and differentiate into myelinating OLGs, possibly in part due to defective DNA methylation. However, further investigations are required to shed light on such effects. It is also worth noting that DNA methyltransferases DNMT1, DNMT3a and DNMT3b have been shown to have distinct roles in various aspect of the OLG lineage cell cycle, myelination, and in remyelination after injury (Fig. 4b) [68, 70, 71, 83, 105].
DNA hydroxymethylation is also dynamic during the OLG life cycle, and TET1 is one of the enzymes involved in this process (Fig. 4). Slower cell cycle progression of OPCs was found in Tet1 knock-out mice, an effect that appeared to be largely specific to the OLG lineage compared to neurons and astrocytes [119]. TET1 was also found to be implicated in processes of myelin repair through the regulation of genes important for the axon-myelin interface [69]. Interestingly, there is increased hydroxymethylation in adult OPCs compared to neonatal OPCs in mice, and evidence suggests that TET1 is essential for myelin repair after damage [69]. As with DNMTs, there is evidence for distinct and complex roles of the TET enzyme family in different aspects of the OLG lineage cell life cycle (Fig. 4b) [69, 119, 120]. Overall, these studies indicate that DNA modifications undergo dynamic changes between neonatal and adult OPCs and are relevant for the decrease in myelinating capacity that is observed in ageing OPCs [87].
More research is needed to elucidate further the importance of 5mC and 5hmC in OLGs, and to understand the complex roles of DNMTs and the TET family of enzymes. This should include investigation of changes in their catalytic activities, during OLG differentiation, in myelination, and in remyelination after injury.
Oligodendrocyte-related genes are differentially methylated in neurodegenerative diseases
As discussed above, OLG-related genes (e.g. MOBP and BIN1) have been associated in GWAS with the risk of developing neurodegenerative diseases. In addition, MOBP was shown to present aberrant DNA methylation in an EWAS of post-mortem MSA white matter tissue [10]. Specifically, hypermethylation (i.e. increased methylation levels) of the promoter region of the gene was detected in MSA compared to controls. DNA methylation changes in MOBP were found even in brain regions very mildly affected by MSA pathology (e.g. occipital lobe), indicating that these may reflect early changes and contribute to disease pathogenesis. The methylation status of MOBP in MSA is linked to changes in MOBP expression levels [11], and the observed downregulation of this gene is likely driven by the hypermethylation of its promoter region. As MOBP protein is involved in the morphological differentiation of OLGs [90], changes in its expression levels due to aberrant methylation during OLG differentiation likely lead to functional impairment of these cells. As another example, BIN1 is the second strongest genetic risk factor for late onset AD [45, 57, 58] and associations between AD neuropathology and the level of methylation at the BIN1 locus have also been reported [47, 116], with BIN1 transcript levels being associated with β-amyloid load [116]. Given this, and that BIN1 has been shown to be predominantly localised to white matter in the brain and expressed primarily in mature OLGs [86], it is reasonable to hypothesise that the involvement of BIN1 gene in disease processes may be mediated through DNA methylation changes affecting OLGs.
Oligodendrocyte cell types and epigenetic age acceleration
DNA methylation changes are known to occur during ageing, which is the major risk factor for neurodegeneration, with accelerated epigenetic ageing, as measured using epigenetic clocks, being reported in neurodegenerative diseases [42,43,44, 81]. Epigenetic clocks allow to infer the difference between the biological age, estimated using the DNA methylome, and the actual chronological age (i.e. epigenetic age acceleration). Age-related changes have been described in OLGs, notably the decrease in myelinating capacity with increased age [87], but it has also been suggested that there is a loss of epigenetic memory in these cells [92]. It has been proposed that intrinsic changes observed in ageing OLGs could be a result of changes on gene expression brought around by an altered epigenomic profile [92]. Indeed, a recent study investigating DNA methylation-based measures of accelerated ageing in post-mortem tissue from different brain regions in MSA and controls found that the relative frequency of OLGs in brain tissue is positively correlated with epigenetic age acceleration [75]. This relationship between OLG proportions and epigenetic age acceleration has also been found in some forms of FTLD [74]. These findings support a role for OLGs in pushing towards increased epigenetic/biological age, suggesting that this cell lineage ages faster than other brain cell types.
Vulnerability of oligodendrocyte lineage cells to reactive oxygen species via epigenetic modifications
A further role of OLGs (aside from myelination) is their involvement in iron equilibrium in the CNS. Iron is key for normal CNS function [94], and OLGs are important in maintaining brain iron homeostasis [84]. Dysregulation, and, specifically, increased iron levels in the brain are associated with neurodegenerative diseases such as AD, PD, and MSA [117]. Proposed mechanisms for the role of iron in neurodegeneration include increased oxidative stress, possibly due to enhanced generation of reactive oxygen species (ROS) associated with increased protein aggregation [26, 117]. Given that OLGs are the principal iron-containing cells of the brain [21], it is reasonable to hypothesise that aberrant OLG function could contribute to neurodegeneration via dysregulation of brain iron levels. Indeed, investigations into brain gene expression in the context of neurodegeneration with brain iron accumulation (NBIA), and in mouse models of increased brain iron loading, implicate OLGs and myelin-related genes [9, 40]. This may well be relevant for other neurodegenerative diseases. OPCs and OLGs are thought to be more vulnerable to oxidative stress than other brain cell types due to factors which include lower levels of antioxidant enzymes and free radical scavengers [6, 30], as well as their high metabolic requirements [7, 87]. Excessive oxidative stress can lead to OLG malfunction through the impairment of effective OLG differentiation [32], with such effects having been reported in neurodegenerative diseases [101]. Interestingly, a link between DNA methylation changes and presence of ROS has been suggested with the finding that increased ROS leads to oxidation of 5mC into 5hmC [62], likely leading to changes in gene expression regulation. Although speculative, it could be hypothesised that this proposed increase in susceptibility of OPCs to ROS-induced damage compared to other brain cell types could, at least in part, be driven by ROS induced alterations in DNA methylation in these cells [6, 30, 32]. However, causal relationships between neurodegenerative processes, OPC dysfunction, DNA methylation and ROS are still unclear and require further investigations.
Concluding remarks
There is an increasing understanding of the importance of myelin and OLGs in the pathogenesis of various neurodegenerative diseases, both in those with or without obvious OLG pathology. There is mounting evidence showing that the efficient development, proliferation, differentiation, and maintenance of the OLG lineage cells may be disrupted in disease, and that aberrant DNA methylation is implicated (Fig. 6). Whether such disease associated disruption leads to death of the OLG lineage cells and consequent demyelination, a decrease in their ability to provide trophic support to neurons, or another unknown ‘effect’ is still unclear. Thus, a better understanding of how human OLG lineage cells function in health and disease is needed. Currently, most studies of the role of epigenetic mechanisms in OLG function, including proliferation, have been carried out in animal models, with only limited studies in human OPCs/OLGs. It is also worth noting that other factors affecting gene expression, not within the scope of this review, including histone modifications and RNA methylation, may also be important in the life cycle of OLG lineage cells [83, 105, 115], and it is likely that combined effects from such factors contribute to OLG function both in health and disease.
Although EWAS have uncovered several aberrantly methylated genes across multiple neurodegenerative diseases, most of these studies utilised bulk tissue, limiting cell-type specific inferences. However, exciting recent advances in cell-type deconvolution algorithms and techniques allowing characterisation of DNA methylation changes in purified cell types or even in single cells will no doubt enhance the discovery of cell-type specific disease-associated DNA methylation signatures.
The study of DNA methylation in neurodegenerative diseases is an exciting avenue. On one hand, elucidating pathogenic mechanisms in disease could provide targets for therapeutic intervention. On the other hand, given that DNA methylation is potentially modifiable, and novel techniques to edit DNA methylation in specific genomic sites are emerging [50, 73, 89, 97], this reinforces the importance of knowing where in genome and in which cell-types disease-related changes occur, and could open new avenues for therapies targeting DNA methylation.
References
Ahmed Z, Asi YT, Lees AJ, Revesz T, Holton JL (2013) Identification and quantification of oligodendrocyte precursor cells in multiple system atrophy, progressive supranuclear palsy and parkinson’s disease. Brain Pathol 23:263. https://doi.org/10.1111/J.1750-3639.2012.00637.X
Allen M, Burgess JD, Ballard T, Serie D, Wang X, Younkin CS, Sun Z, Kouri N, Baheti S, Wang C, Carrasquillo MM, Nguyen T, Lincoln S, Malphrus K, Murray M, Golde TE, Price ND, Younkin SG, Schellenberg GD, Asmann Y, Ordog T, Crook J, Dickson D, Ertekin-Taner N (2016) Gene expression, methylation and neuropathology correlations at progressive supranuclear palsy risk loci. Acta Neuropathol 132:197. https://doi.org/10.1007/S00401-016-1576-7
Allen M, Wang X, Burgess JD, Watzlawik J, Serie DJ, Younkin CS, Nguyen T, Malphrus KG, Lincoln S, Carrasquillo MM, Ho C, Chakrabarty P, Strickland S, Murray ME, Swarup V, Geschwind DH, Seyfried NT, Dammer EB, Lah JJ, Levey AI, Golde TE, Funk C, Li H, Price ND, Petersen RC, Graff-Radford NR, Younkin SG, Dickson DW, Crook JR, Asmann YW, Ertekin-Taner N (2018) Conserved brain myelination networks are altered in Alzheimer’s and other neurodegenerative diseases. Alzheimer’s Dementia 14:352–366. https://doi.org/10.1016/J.JALZ.2017.09.012
Al-Mahdawi S, Anjomani Virmouni S, Pook MA (2016) DNA methylation in neurodegenerative diseases. Epigenet Biomark Diagnost. https://doi.org/10.1016/B978-0-12-801899-6.00020-6
Appleby-Mallinder C, Schaber E, Kirby J, Shaw PJ, Cooper-Knock J, Heath PR, Highley JR (2021) TDP43 proteinopathy is associated with aberrant DNA methylation in human amyotrophic lateral sclerosis. Neuropathol Appl Neurobiol 47:61–72. https://doi.org/10.1111/NAN.12625
Back SA, Gan X, Li Y, Rosenberg PA, Volpe JJ (1998) Maturation-dependent vulnerability of oligodendrocytes to oxidative stress-induced death caused by glutathione depletion. J Neurosci 18:6241–6253. https://doi.org/10.1523/JNEUROSCI.18-16-06241.1998
Bartzokis G (2004) Age-related myelin breakdown: a developmental model of cognitive decline and Alzheimer’s disease. Neurobiol Aging 25:5–18. https://doi.org/10.1016/J.NEUROBIOLAGING.2003.03.001
Behrendt G, Baer K, Buffo A, Curtis MA, Faull RL, Rees MI, Götz M, Dimou L (2013) Dynamic changes in myelin aberrations and oligodendrocyte generation in chronic amyloidosis in mice and men. Glia 61:273–286. https://doi.org/10.1002/GLIA.22432
Bettencourt C, Forabosco P, Wiethoff S, Heidari M, Johnstone DM, Botía JA, Collingwood JF, Hardy J, Milward EA, Ryten M, Houlden H, for the UK Brain Expression Consortium (UKBEC) (2016) Gene co-expression networks shed light into diseases of brain iron accumulation. Neurobiol Dis 87:59. https://doi.org/10.1016/J.NBD.2015.12.004
Bettencourt C, Foti SC, Miki Y, Botia J, Chatterjee A, Warner TT, Revesz T, Lashley T, Balazs R, Viré E, Holton JL (2020) White matter DNA methylation profiling reveals deregulation of HIP1, LMAN2, MOBP, and other loci in multiple system atrophy. Acta Neuropathol 139:135. https://doi.org/10.1007/S00401-019-02074-0
Bettencourt C, Miki Y, Piras IS, de Silva R, Foti SC, Talboom JS, Revesz T, Lashley T, Balazs R, Viré E, Warner TT, Huentelman MJ, Holton JL (2021) MOBP and HIP1 in multiple system atrophy: New α-synuclein partners in glial cytoplasmic inclusions implicated in the disease pathogenesis. Neuropathol Appl Neurobiol 47:640. https://doi.org/10.1111/NAN.12688
Blanchard JW, Akay LA, Davila-Velderrain J, von Maydell D, Mathys H, Davidson SM, Effenberger A, Chen C-Y, Maner-Smith K, Hajjar I, Ortlund EA, Bula M, Agbas E, Ng A, Jiang X, Kahn M, Blanco-Duque C, Lavoie N, Liu L, Reyes R, Lin Y-T, Ko T, R’Bibo L, Ralvenius WT, Bennett DA, Cam HP, Kellis M, Tsai L-H (2022) APOE4 impairs myelination via cholesterol dysregulation in oligodendrocytes. Nature 2022:1–11. https://doi.org/10.1038/s41586-022-05439-w
Braak H, Braak E (1996) Development of Alzheimer-related neurofibrillary changes in the neocortex inversely recapitulates cortical myelogenesis. Acta Neuropathologica 92:197–201. https://doi.org/10.1007/S004010050508
Bradl M, Lassmann H Oligodendrocytes: biology and pathology. https://doi.org/10.1007/s00401-009-0601-5
Brickman AM (2013) Contemplating Alzheimer’s disease and the contribution of white matter hyperintensities. Curr Neurol Neurosci Rep 13:1–9. https://doi.org/10.1007/S11910-013-0415-7/FIGURES/2
Brickman AM, Provenzano FA, Muraskin J, Manly JJ, Blum S, Apa Z, Stern Y, Brown TR, Luchsinger JA, Mayeux R (2012) Regional White matter hyperintensity volume, not hippocampal atrophy, predicts incident alzheimer disease in the community. Arch Neurol 69:1621–1627. https://doi.org/10.1001/ARCHNEUROL.2012.1527
Chapuis J, Hansmannel F, Gistelinck M, Mounier A, Cauwenberghe V, Kolen K, v, Geller F, Sottejeau Y, Harold D, Dourlen P, Grenier-Boley B, Kamatani Y, Delepine B, Demiautte F, Zelenika D, Zommer N, Hamdane M, Bellenguez C, Dartigues J-F, Hauw J-J, Letronne F, Ayral A-M, Sleegers K, Schellens A, Broeck L v, Callaerts P, Mann D, Williams J, Bué L, Dewachter I, Broeckhoven V, Amouyel P, Moechars D, Dermaut B, Lambert J-C, (2013) Increased expression of BIN1 mediates Alzheimer genetic risk by modulating tau pathology. Mol Psychiatry 16:1225–1234. https://doi.org/10.1038/mp.2013.1
Chen JA, Chen Z, Won H, Huang AY, Lowe JK, Wojta K, Yokoyama JS, Bensimon G, Leigh PN, Payan C, Shatunov A, Jones AR, Lewis CM, Deloukas P, Amouyel P, Tzourio C, Dartigues JF, Ludolph A, Boxer AL, Bronstein JM, Al-Chalabi A, Geschwind DH, Coppola G (2018) Joint genome-wide association study of progressive supranuclear palsy identifies novel susceptibility loci and genetic correlation to neurodegenerative diseases. Mol Neurodegener 13:1–11. https://doi.org/10.1186/S13024-018-0270-8/FIGURES/3
Chen JA, Chen Z, Won H, Huang AY, Lowe JK, Wojta K, Yokoyama JS, Bensimon G, Leigh PN, Payan C, Shatunov A, Jones AR, Lewis CM, Deloukas P, Amouyel P, Tzourio C, Dartigues JF, Ludolph A, Boxer AL, Bronstein JM, Al-Chalabi A, Geschwind DH, Coppola G (2018) Joint genome-wide association study of progressive supranuclear palsy identifies novel susceptibility loci and genetic correlation to neurodegenerative diseases. Mol Neurodegener. https://doi.org/10.1186/S13024-018-0270-8
Compston A, Coles A (2008) Multiple sclerosis. The Lancet 372:1502–1517. https://doi.org/10.1016/S0140-6736(08)61620-7
Connor JR, Menzies SL (1996) Relationship of iron to oligodendrocytes and myelination
Dawson MRL, Polito A, Levine JM, Reynolds R (2003) NG2-expressing glial progenitor cells: an abundant and widespread population of cycling cells in the adult rat CNS. Mol Cell Neurosci 24:476–488. https://doi.org/10.1016/S1044-7431(03)00210-0
Dean DC, Hurley SA, Kecskemeti SR, O’Grady JP, Canda C, Davenport-Sis NJ, Carlsson CM, Zetterberg H, Blennow K, Asthana S, Sager MA, Johnson SC, Alexander AL, Bendlin BB (2017) Association of amyloid pathology with myelin alteration in preclinical alzheimer disease. JAMA Neurol 74:41–49. https://doi.org/10.1001/JAMANEUROL.2016.3232
Dickson DW, Ahmed Z, Algom AA, Tsuboi Y, Josephs KA (2010) Neuropathology of variants of progressive supranuclear palsy. Curr Opin Neurol 23:394–400. https://doi.org/10.1097/WCO.0B013E32833BE924
Ettle B, Schlachetzki JCM, Winkler J (2015) Oligodendroglia and Myelin in neurodegenerative diseases: more than just bystanders? Mol Neurobiol 53:3046–3062. https://doi.org/10.1007/S12035-015-9205-3
Ettle B, Schlachetzki JCM, Winkler J (2035) Oligodendroglia and myelin in neurodegenerative diseases: more than just bystanders? Mol Neurobiol https://doi.org/10.1007/s12035-015-9205-3
F C, F A, M J-L, I P, A M, VS K, M F, (2018) Progression of white matter damage in progressive supranuclear palsy with predominant parkinsonism. Parkinsonism Relat Disord 49:95–99. https://doi.org/10.1016/J.PARKRELDIS.2018.01.001
Falcão AM, van Bruggen D, Marques S, Meijer M, Jäkel S, Agirre E, Samudyata Floriddia EM, Vanichkina DP, ffrench-Constant C, Williams A, Guerreiro-Cacais AO, Castelo-Branco G, (2018) Disease-specific oligodendrocyte lineage cells arise in multiple sclerosis. Nat Med 24:1837–1844. https://doi.org/10.1038/s41591-018-0236-y
de Faria O, Pivonkova H, Varga B, Timmler S, Evans KA, Káradóttir RT (2021) Periods of synchronized myelin changes shape brain function and plasticity. Nat Neurosci 24:1508–1521. https://doi.org/10.1038/s41593-021-00917-2
Fern R, Möller T (2000) Rapid ischemic cell death in immature oligodendrocytes: a fatal glutamate release feedback loop. J Neurosci 20:34–42. https://doi.org/10.1523/JNEUROSCI.20-01-00034.2000
Fodder K, Murthy M, Rizzu P, Toomey CE, Hasan R (2023) Humphrey · Jack, Raj T, Lunnon K, Mill J, Heutink · Peter, Lashley T, Conceição Bettencourt · (2023) Brain DNA methylomic analysis of frontotemporal lobar degeneration reveals OTUD4 in shared dysregulated signatures across pathological subtypes. Acta Neuropathol 1:1–19. https://doi.org/10.1007/S00401-023-02583-Z
French HM, Reid M, Mamontov P, Simmons RA, Grinspan JB (2009) Oxidative stress disrupts oligodendrocyte maturation. J Neurosci Res 87:3076–3087. https://doi.org/10.1002/JNR.22139
Fu H, Hardy J, Duff KE (2018) Selective vulnerability in neurodegenerative diseases. Nat Neurosci 21:1350–1358. https://doi.org/10.1038/s41593-018-0221-2
Gagyi E, Kormos B, Castellanos KJ, Valyi-Nagy K, Korneff D, Lopresti P, Woltjer R, Valyi-Nagy T (2012) Decreased oligodendrocyte nuclear diameter in alzheimer’s disease and lewy body dementia. Brain Pathol 22:803. https://doi.org/10.1111/J.1750-3639.2012.00595.X
Globisch D, Münzel M, Müller M, Michalakis S, Wagner M, Koch S, Brückl T, Biel M, Carell T (2010) Tissue distribution of 5-hydroxymethylcytosine and search for active demethylation intermediates. PLoS ONE 5:15367. https://doi.org/10.1371/JOURNAL.PONE.0015367
Gorman AM (2008) Neuronal cell death in neurodegenerative diseases: recurring themes around protein handling. J Cell Mol Med 12:2263. https://doi.org/10.1111/J.1582-4934.2008.00402.X
Greenberg MVC, Bourc’his D, (2019) The diverse roles of DNA methylation in mammalian development and disease. Nat Rev Mol Cell Biol 20:590–607. https://doi.org/10.1038/s41580-019-0159-6
Guo JU, Su Y, Zhong C, Ming GL, Song H (2011) Hydroxylation of 5-methylcytosine by TET1 promotes active DNA demethylation in the adult brain. Cell 145:423–434. https://doi.org/10.1016/J.CELL.2011.03.022
Hasan R, Humphrey J, Bettencourt C, Newcombe J, Lashley T, Fratta P, Raj T (2022) Transcriptomic analysis of frontotemporal lobar degeneration with TDP-43 pathology reveals cellular alterations across multiple brain regions. Acta Neuropathol. https://doi.org/10.1007/S00401-021-02399-9
Heidari M, Johnstone DM, Bassett B, Graham RM, Chua A, House MJ, Collingwood JF, Bettencourt C, Houlden H, Ryten M (2016) Brain iron accumulation affects myelin-related molecular systems implicated in a rare neurogenetic disease family with neuropsychiatric features. Mol Psychiatry 21:1599–1607. https://doi.org/10.1038/mp.2015.192
Höglinger GU, Melhem NM, Dickson DW, A Sleiman PM, Wang L-S, Klei L, Rademakers R, de Silva R, Litvan I, Riley DE, van Swieten JC, Heutink P, Wszolek ZK, Uitti RJ, Vandrovcova J, Hurtig HI, Gross RG, Maetzler W, Goldwurm S, Tolosa E, Borroni B, Pastor P, Cantwell LB, Ryung Han M, Dillman A, van der Brug MP, Raphael Gibbs J, Cookson MR, Hernandez DG, Singleton AB, Farrer MJ, Yu C-E, Golbe LI, Revesz T, Hardy J, Lees AJ, Devlin B, Hakonarson H, Müller U, Schellenberg GD (2011) Identification of common variants influencing risk of the tauopathy progressive supranuclear palsy. https://doi.org/10.1038/ng.859
Horvath S (2013) DNA methylation age of human tissues and cell types. Genome Biol 14:1–20. https://doi.org/10.1186/GB-2013-14-10-R115/COMMENTS
Horvath S, Langfelder P, Kwak S, Aaronson J, Rosinski J, Vogt TF, Eszes M, Faull RLM, Curtis MA, Waldvogel HJ, Choi OW, Tung S, Vinters HV, Coppola G, Yang XW (2016) Huntington’s disease accelerates epigenetic aging of human brain and disrupts DNA methylation levels. Aging 8:1485–1512. https://doi.org/10.18632/AGING.101005
Horvath S, Ritz BR (2015) Increased epigenetic age and granulocyte counts in the blood of Parkinson’s disease patients. Aging 7:1130–1142. https://doi.org/10.18632/AGING.100859
Hu X, Pickering E, Liu YC, Hall S, Fournier H, Katz E, Dechairo B, John S, van Eerdewegh P, Soares H (2011) Meta-analysis for genome-wide association study identifies multiple variants at the BIN1 locus associated with late-onset Alzheimer’s disease. PLoS One. https://doi.org/10.1371/journal.pone.0016616
Irwin DJ, McMillan CT, Suh E, Powers J, Rascovsky K, Wood EM, Toledo JB, Arnold SE, Lee VM-Y, Van DVM, Trojanowski JQ, Grossman M (2014) Myelin oligodendrocyte basic protein and prognosis in behavioral-variant frontotemporal dementia. Neurology 83:502. https://doi.org/10.1212/WNL.0000000000000668
De Jager PL, Srivastava G, Lunnon K, Burgess J, Schalkwyk LC, Yu L, Eaton ML, Keenan BT, Ernst J, McCabe C, Tang A, Raj T, Replogle J, Brodeur W, Gabriel S, Chai HS, Younkin C, Younkin SG, Zou F, Szyf M, Epstein CB, Schneider JA, Bernstein BE, Meissner A, Ertekin-Taner N, Chibnik LB, Kellis M, Mill J, Bennett DA (2014) Alzheimer’s disease: early alterations in brain DNA methylation at ANK1, BIN1, RHBDF2 and other loci. Nat Neurosci 17:1156–1163. https://doi.org/10.1038/nn.3786
Jeong H, Mendizabal I, Berto S, Chatterjee P, Layman T, Usui N, Toriumi K, Douglas C, Singh D, Huh I, Preuss TM, Konopka G, Yi S, v. (2021) Evolution of DNA methylation in the human brain. Nat Commun. https://doi.org/10.1038/S41467-021-21917-7
Kaji S, Maki T, Ishimoto T, Yamakado H, Takahashi R (2020) Insights into the pathogenesis of multiple system atrophy: focus on glial cytoplasmic inclusions. Transl Neurodegen 9:1–15. https://doi.org/10.1186/S40035-020-0185-5
Kantor B, Tagliafierro L, Gu J, Zamora ME, Ilich E, Grenier C, Huang ZY, Murphy S, Chiba-Falek O (2018) Downregulation of SNCA expression by targeted editing of DNA methylation: a potential strategy for precision therapy in PD. Mol Ther 26:2638. https://doi.org/10.1016/J.YMTHE.2018.08.019
Kaut O, Schmitt I, Wüllner U (2012) Genome-scale methylation analysis of Parkinson’s disease patients’ brains reveals DNA hypomethylation and increased mRNA expression of cytochrome P450 2E1. Neurogenetics 13:87–91. https://doi.org/10.1007/S10048-011-0308-3
Kirby L, Castelo-Branco G (2021) Crossing boundaries: Interplay between the immune system and oligodendrocyte lineage cells. Semin Cell Dev Biol 116:45–52. https://doi.org/10.1016/J.SEMCDB.2020.10.013
Komori T (1999) Tau-positive dial inclusions in progressive supranuclear palsy, corticobasal degeneration and Pick’s disease. Brain Pathol 9:663. https://doi.org/10.1111/J.1750-3639.1999.TB00549.X
Kouri N, Ross OA, Dombroski B, Younkin CS, Serie DJ, Soto-Ortolaza A, Baker M, Finch NCA, Yoon H, Kim J, Fujioka S, Mclean CA, Ghetti B, Spina S, Cantwell LB, Farlow MR, Grafman J, Huey ED, Ryung Han M, Beecher S, Geller ET, Kretzschmar HA, Roeber S, Gearing M, Juncos JL, Vonsattel JPG, van Deerlin VM, Grossman M, Hurtig HI, Gross RG, Arnold SE, Trojanowski JQ, Lee VM, Wenning GK, White CL, Höglinger GU, Müller U, Devlin B, Golbe LI, Crook J, Parisi JE, Boeve BF, Josephs KA, Wszolek ZK, Uitti RJ, Graff-Radford NR, Litvan I, Younkin SG, Wang LS, Ertekin-Taner N, Rademakers R, Hakonarsen H, Schellenberg GD, Dickson DW (2015) Genome-wide association study of corticobasal degeneration identifies risk variants shared with progressive supranuclear palsy. Nat Commun. https://doi.org/10.1038/NCOMMS8247
Kozlenkov A, Li J, Apontes P, Hurd YL, Byne WM, Koonin EV, Wegner M, Mukamel EA, Dracheva S (2018) A unique role for DNA (hydroxy)methylation in epigenetic regulation of human inhibitory neurons. Sci Adv. https://doi.org/10.1126/SCIADV.AAU6190/SUPPL_FILE/AAU6190_TABLE_S4.XLSX
Kuhn S, Gritti L, Crooks D, Dombrowski Y (2019) Oligodendrocytes in development, myelin generation and beyond. Cells. https://doi.org/10.3390/CELLS8111424
Kunkle BW, Grenier-Boley B, Sims R, Bis JC, Damotte V, Naj AC, Boland A, Vronskaya M, van der Lee SJ, Amlie-Wolf A, Bellenguez C, Frizatti A, Chouraki V, Martin ER, Sleegers K, Badarinarayan N, Jakobsdottir J, Hamilton-Nelson KL, Moreno-Grau S, Olaso R, Raybould R, Chen Y, Kuzma AB, Hiltunen M, Morgan T, Ahmad S, Vardarajan BN, Epelbaum J, Hoffmann P, Boada M, Beecham GW, Garnier JG, Harold D, Fitzpatrick AL, Valladares O, Moutet ML, Gerrish A, Smith A v., Qu L, Bacq D, Denning N, Jian X, Zhao Y, del Zompo M, Fox NC, Choi SH, Mateo I, Hughes JT, Adams HH, Malamon J, Sanchez-Garcia F, Patel Y, Brody JA, Dombroski BA, Naranjo MCD, Daniilidou M, Eiriksdottir G, Mukherjee S, Wallon D, Uphill J, Aspelund T, Cantwell LB, Garzia F, Galimberti D, Hofer E, Butkiewicz M, Fin B, Scarpini E, Sarnowski C, Bush WS, Meslage S, Kornhuber J, White CC, Song Y, Barber RC, Engelborghs S, Sordon S, Voijnovic D, Adams PM, Vandenberghe R, Mayhaus M, Cupples LA, Albert MS, de Deyn PP, Gu W, Himali JJ, Beekly D, Squassina A, Hartmann AM, Orellana A, Blacker D, Rodriguez-Rodriguez E, Lovestone S, Garcia ME, Doody RS, Munoz-Fernadez C, Sussams R, Lin H, Fairchild TJ, Benito YA, Holmes C, Karamujić-Čomić H, Frosch MP, Thonberg H, Maier W, Roschupkin G, Ghetti B, Giedraitis V, Kawalia A, Li S, Huebinger RM, Kilander L, Moebus S, Hernández I, Kamboh MI, Brundin RM, Turton J, Yang Q, Katz MJ, Concari L, Lord J, Beiser AS, Keene CD, Helisalmi S, Kloszewska I, Kukull WA, Koivisto AM, Lynch A, Tarraga L, Larson EB, Haapasalo A, Lawlor B, Mosley TH, Lipton RB, Solfrizzi V, Gill M, Longstreth WT, Montine TJ, Frisardi V, Diez-Fairen M, Rivadeneira F, Petersen RC, Deramecourt V, Alvarez I, Salani F, Ciaramella A, Boerwinkle E, Reiman EM, Fievet N, Rotter JI, Reisch JS, Hanon O, Cupidi C, Andre Uitterlinden AG, Royall DR, Dufouil C, Maletta RG, de Rojas I, Sano M, Brice A, Cecchetti R, George-Hyslop PS, Ritchie K, Tsolaki M, Tsuang DW, Dubois B, Craig D, Wu CK, Soininen H, Avramidou D, Albin RL, Fratiglioni L, Germanou A, Apostolova LG, Keller L, Koutroumani M, Arnold SE, Panza F, Gkatzima O, Asthana S, Hannequin D, Whitehead P, Atwood CS, Caffarra P, Hampel H, Quintela I, Carracedo Á, Lannfelt L, Rubinsztein DC, Barnes LL, Pasquier F, Frölich L, Barral S, McGuinness B, Beach TG, Johnston JA, Becker JT, Passmore P, Bigio EH, Schott JM, Bird TD, Warren JD, Boeve BF, Lupton MK, Bowen JD, Proitsi P, Boxer A, Powell JF, Burke JR, Kauwe JSK, Burns JM, Mancuso M, Buxbaum JD, Bonuccelli U, Cairns NJ, McQuillin A, Cao C, Livingston G, Carlson CS, Bass NJ, Carlsson CM, Hardy J, Carney RM, Bras J, Carrasquillo MM, Guerreiro R, Allen M, Chui HC, Fisher E, Masullo C, Crocco EA, DeCarli C, Bisceglio G, Dick M, Ma L, Duara R, Graff-Radford NR, Evans DA, Hodges A, Faber KM, Scherer M, Fallon KB, Riemenschneider M, Fardo DW, Heun R, Farlow MR, Kölsch H, Ferris S, Leber M, Foroud TM, Heuser I, Galasko DR, Giegling I, Gearing M, Hüll M, Geschwind DH, Gilbert JR, Morris JC, Green RC, Mayo K, Growdon JH, Feulner T, Hamilton RL, Harrell LE, Drichel D, Honig LS, Cushion TD, Huentelman MJ, Hollingworth P, Hulette CM, Hyman BT, Marshall R, Jarvik GP, Meggy A, Abner E, Menzies GE, Jin LW, Leonenko G, Real LM, Jun GR, Baldwin CT, Grozeva D, Karydas A, Russo G, Kaye JA, Kim R, Jessen F, Kowall NW, Vellas B, Kramer JH, Vardy E, LaFerla FM, Jöckel KH, Lah JJ, Dichgans M, Leverenz JB, Mann D, Levey AI, Pickering-Brown S, Lieberman AP, Klopp N, Lunetta KL, Wichmann HE, Lyketsos CG, Morgan K, Marson DC, Brown K, Martiniuk F, Medway C, Mash DC, Nöthen MM, Masliah E, Hooper NM, McCormick WC, Daniele A, McCurry SM, Bayer A, McDavid AN, Gallacher J, McKee AC, van den Bussche H, Mesulam M, Brayne C, Miller BL, Riedel-Heller S, Miller CA, Miller JW, Al-Chalabi A, Shaw CE, Myers AJ, Wiltfang J, O’Bryant S, Olichney JM, Alvarez V, Parisi JE, Singleton AB, Paulson HL, Collinge J, Perry WR, Mead S, Peskind E, Cribbs DH, Rossor M, Pierce A, Ryan NS, Poon WW, Nacmias B, Potter H, Sorbi S, Quinn JF, Sacchinelli E, Raj A, Spalletta G, Raskind M, Caltagirone C, Bossù P, Orfei MD, Reisberg B, Clarke R, Reitz C, Smith AD, Ringman JM, Warden D, Roberson ED, Wilcock G, Rogaeva E, Bruni AC, Rosen HJ, Gallo M, Rosenberg RN, Ben-Shlomo Y, Sager MA, Mecocci P, Saykin AJ, Pastor P, Cuccaro ML, Vance JM, Schneider JA, Schneider LS, Slifer S, Seeley WW, Smith AG, Sonnen JA, Spina S, Stern RA, Swerdlow RH, Tang M, Tanzi RE, Trojanowski JQ, Troncoso JC, van Deerlin VM, van Eldik LJ, Vinters H v., Vonsattel JP, Weintraub S, Welsh-Bohmer KA, Wilhelmsen KC, Williamson J, Wingo TS, Woltjer RL, Wright CB, Yu CE, Yu L, Saba Y, Pilotto A, Bullido MJ, Peters O, Crane PK, Bennett D, Bosco P, Coto E, Boccardi V, de Jager PL, Lleo A, Warner N, Lopez OL, Ingelsson M, Deloukas P, Cruchaga C, Graff C, Gwilliam R, Fornage M, Goate AM, Sanchez-Juan P, Kehoe PG, Amin N, Ertekin-Taner N, Berr C, Debette S, Love S, Launer LJ, Younkin SG, Dartigues JF, Corcoran C, Ikram MA, Dickson DW, Nicolas G, Campion D, Tschanz JA, Schmidt H, Hakonarson H, Clarimon J, Munger R, Schmidt R, Farrer LA, van Broeckhoven C, C. O’Donovan M, DeStefano AL, Jones L, Haines JL, Deleuze JF, Owen MJ, Gudnason V, Mayeux R, Escott-Price V, Psaty BM, Ramirez A, Wang LS, Ruiz A, van Duijn CM, Holmans PA, Seshadri S, Williams J, Amouyel P, Schellenberg GD, Lambert JC, Pericak-Vance MA (2019) Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat Genet 51:414–430. https://doi.org/10.1038/s41588-019-0358-2
Lambert JC, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C, Jun G, DeStefano AL, Bis JC, Beecham GW, Grenier-Boley B, Russo G, Thornton-Wells TA, Jones N, Smith A v., Chouraki V, Thomas C, Ikram MA, Zelenika D, Vardarajan BN, Kamatani Y, Lin CF, Gerrish A, Schmidt H, Kunkle B, Fiévet N, Amouyel P, Pasquier F, Deramecourt V, de Bruijn RFAG, Amin N, Hofman A, van Duijn CM, Dunstan ML, Hollingworth P, Owen MJ, O’Donovan MC, Jones L, Holmans PA, Moskvina V, Williams J, Baldwin C, Farrer LA, Choi SH, Lunetta KL, Fitzpatrick AL, Harris TB, Psaty BM, Gilbert JR, Hamilton-Nelson KL, Martin ER, Pericak-Vance MA, Haines JL, Gudnason V, Jonsson P v., Eiriksdottir G, Bihoreau MT, Lathrop M, Valladares O, Cantwell LB, Wang LS, Schellenberg GD, Ruiz A, Boada M, Reitz C, Mayeux R, Ramirez A, Maier W, Hanon O, Kukull WA, Buxbaum JD, Campion D, Wallon D, Hannequin D, Crane PK, Larson EB, Becker T, Cruchaga C, Goate AM, Craig D, Johnston JA, Mc-Guinness B, Todd S, Passmore P, Berr C, Ritchie K, Lopez OL, de Jager PL, Evans D, Lovestone S, Proitsi P, Powell JF, Letenneur L, Barberger-Gateau P, Dufouil C, Dartigues JF, Morón FJ, Rubinsztein DC, st. George-Hyslop P, Sleegers K, Bettens K, van Broeckhoven C, Huentelman MJ, Gill M, Brown K, Morgan K, Kamboh MI, Keller L, Fratiglioni L, Green R, Myers AJ, Love S, Rogaeva E, Gallacher J, Bayer A, Clarimon J, Lleo A, Tsuang DW, Yu L, Bennett DA, Tsolaki M, Bossù P, Spalletta G, Collinge J, Mead S, Sorbi S, Nacmias B, Sanchez-Garcia F, Deniz Naranjo MC, Fox NC, Hardy J, Bosco P, Clarke R, Brayne C, Galimberti D, Mancuso M, Matthews F, Moebus S, Mecocci P, del Zompo M, Hampel H, Pilotto A, Bullido M, Panza F, Caffarra P, Mayhaus M, Pichler S, Gu W, Riemenschneider M, Lannfelt L, Ingelsson M, Hakonarson H, Carrasquillo MM, Zou F, Younkin SG, Beekly D, Alvarez V, Coto E, Razquin C, Pastor P, Mateo I, Combarros O, Faber KM, Foroud TM, Soininen H, Hiltunen M, Blacker D, Mosley TH, Graff C, Holmes C, Montine TJ, Rotter JI, Brice A, Nalls MA, Kauwe JSK, Boerwinkle E, Schmidt R, Rujescu D, Tzourio C, Nöthen MM, Launer LJ, Seshadri S (2013) Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat Genet 45:1452–1458. doi: https://doi.org/10.1038/NG.2802
Liu QY, Yu JT, Miao D, Ma XY, Wang HF, Wang W, Tan L (2013) An exploratory study on STX6, MOBP, MAPT, and EIF2AK3 and late-onset Alzheimer’s disease. Neurobiol Aging 34:1519.e13-1519.e17. https://doi.org/10.1016/J.NEUROBIOLAGING.2012.10.004
Lou S, Lee HM, Qin H, Li JW, Gao Z, Liu X, Chan LL, Lam VKL, So WY, Wang Y, Lok S, Wang J, Ma RCW, Tsui SKW, Chan JCN, Chan TF, Yip KY (2014) Whole-genome bisulfite sequencing of multiple individuals reveals complementary roles of promoter and gene body methylation in transcriptional regulation. Genome Biol 15:1–21. https://doi.org/10.1186/S13059-014-0408-0/FIGURES/11
Lunnon K, Smith R, Hannon E, De Jager PL, Srivastava G, Volta M, Troakes C, Al-Sarraj S, Burrage J, Macdonald R, Condliffe D, Harries LW, Katsel P, Haroutunian V, Kaminsky Z, Joachim C, Powell J, Lovestone S, Bennett DA, Schalkwyk LC, Mill J (2014) Methylomic profiling implicates cortical deregulation of ANK1 in Alzheimer’s disease. Nat Neurosci 17:1164–1170. https://doi.org/10.1038/NN.3782
Madugundu GS, Cadet J, Wagner JR (2014) Hydroxyl-radical-induced oxidation of 5-methylcytosine in isolated and cellular DNA. Nucleic Acids Res 42:7450–7460. https://doi.org/10.1093/NAR/GKU334
Masliah E, Dumaop W, Galasko D, Desplats P (2013) Distinctive patterns of DNA methylation associated with Parkinson disease: Identification of concordant epigenetic changes in brain and peripheral blood leukocytes. Epigenetics 8:1030–1038. https://doi.org/10.4161/EPI.25865/SUPPL_FILE/KEPI_A_10925865_SM0001.ZIP
Matsuo A, Akiguchi I, Lee GC, McGeer EG, McGeer PL, Kimura J (1998) Myelin degeneration in multiple system atrophy detected by unique antibodies. Am J Pathol 153:735. https://doi.org/10.1016/S0002-9440(10)65617-9
May VEL, Ettle B, Poehler AM, Nuber S, Ubhi K, Rockenstein E, Winner B, Wegner M, Masliah E, Winkler J (2014) α-Synuclein impairs oligodendrocyte progenitor maturation in multiple system atrophy. Neurobiol Aging 35:2357–2368. https://doi.org/10.1016/J.NEUROBIOLAGING.2014.02.028
Moore LD, Le T, Fan G (2012) DNA Methylation and Its Basic Function. Neuropsychopharmacology 2013 38:1 38:23–38. doi: https://doi.org/10.1038/npp.2012.112
Moosavi A, Ardekani AM (2016) Role of epigenetics in biology and human diseases. Iran Biomed J 20:246. https://doi.org/10.22045/IBJ.2016.01
Moyon S, Casaccia P (2017) DNA methylation in oligodendroglial cells during developmental myelination and in disease. Neurogenesis. https://doi.org/10.1080/23262133.2016.1270381
Moyon S, Frawley R, Marshall-Phelps KL, Kegel L, Bøstrand SM, Sadowski B, Huang D, Jiang Y-H, Lyons D, Möbius W, Casaccia P (2019) TET1-mediated DNA hydroxy-methylation regulates adult remyelination. bioRxiv. https://doi.org/10.1101/819995
Moyon S, Huynh JL, Dutta D, Zhang F, Ma D, Yoo S, Lawrence R, Wegner M, John GR, Emery B, Lubetzki C, Franklin RJM, Fan G, Zhu J, Dupree JL, Casaccia P (2016) Functional characterization of DNA methylation in the oligodendrocyte lineage. Cell Rep 15:748. https://doi.org/10.1016/J.CELREP.2016.03.060
Moyon S, Ma D, Huynh JL, Coutts DJC, Zhao C, Casaccia P, Franklin RJM (2017) Efficient remyelination requires DNA methylation. eNeuro. https://doi.org/10.1523/ENEURO.0336-16.2017
Münzel M, Globisch D, Brückl T, Wagner M, Welzmiller V, Michalakis S, Müller M, Biel M, Carell T (2010) Quantification of the sixth DNA base hydroxymethylcytosine in the brain. Angew Chem Int Ed 49:5375–5377. https://doi.org/10.1002/ANIE.201002033
Murthy M, Cheng YY, Holton JL, Bettencourt C (2021) Neurodegenerative movement disorders: an epigenetics perspective and promise for the future. Neuropathol Appl Neurobiol 47:897–909. https://doi.org/10.1111/NAN.12757
Murthy M, Rizzu P, Heutink P, Mill J, Lashley T, Bettencourt C (2023) Epigenetic age acceleration in frontotemporal lobar degeneration: a comprehensive analysis in the blood and brain. bioRxiv. https://doi.org/10.1101/2023.05.19.541419
Murthy M, Shireby G, Miki Y, Viré E, Lashley T, Warner TT, Mill J, Bettencourt C (2023) Epigenetic age acceleration is associated with oligodendrocyte proportions in MSA and control brain tissue. Neuropathol Appl Neurobiol. https://doi.org/10.1111/NAN.12872
Narine M, Colognato H (2022) Current insights into oligodendrocyte metabolism and its power to sculpt the myelin landscape. Front Cell Neurosci. https://doi.org/10.3389/FNCEL.2022.892968
Nasrabady SE, Rizvi B, Goldman JE, Brickman AM (2018) White matter changes in Alzheimer’s disease: a focus on myelin and oligodendrocytes. Acta Neuropathol Commun 6:22. https://doi.org/10.1186/S40478-018-0515-3
Pai AA, Bell JT, Marioni JC, Pritchard JK, Gilad Y (2011) A genome-wide study of DNA methylation patterns and gene expression levels in multiple human and chimpanzee tissues. PLoS Genet 7:1001316. https://doi.org/10.1371/journal.pgen.1001316
Papuc E, Rejdak K (2020) The role of myelin damage in Alzheimer’s disease pathology. Arch Med Sci 16:345–351. https://doi.org/10.5114/AOMS.2018.76863
Pelvig DP, Pakkenberg H, Stark AK, Pakkenberg B (2008) Neocortical glial cell numbers in human brains. Neurobiol Aging 29:1754–1762. https://doi.org/10.1016/J.NEUROBIOLAGING.2007.04.013
Picillo M, Lizarraga KJ, Friesen EL, Chau H, Zhang M, Sato C, Rooke G, Munhoz RP, Rogaeva E, Fraser PE, Kalia SK, Kalia LV (2018) Parkinsonism due to A53E α-synuclein gene mutation: clinical, genetic, epigenetic, and biochemical features. Mov Disord 33:1950–1955. https://doi.org/10.1002/MDS.27506
Piras IS, Bleul C, Schrauwen I, Schrauwen I, Talboom J, Llaci L, Llaci L, de Both MD, Naymik MA, Halliday G, Bettencourt C, Holton JL, Serrano GE, Sue LI, Beach TG, Stefanova N, Huentelman MJ (2020) Transcriptional profiling of multiple system atrophy cerebellar tissue highlights differences between the parkinsonian and cerebellar sub-types of the disease. Acta Neuropathol Commun. https://doi.org/10.1186/S40478-020-00950-5
Pruvost M, Moyon S (2021) Oligodendroglial epigenetics, from lineage specification to activity-dependent myelination. Life 11:62. https://doi.org/10.3390/LIFE11010062
Qing H, Xu H, Xie J, Wang Y, Song N, Wang J, Jiang H (2018) New progress on the role of glia in iron metabolism and iron-induced degeneration of dopamine neurons in Parkinson’s disease. https://doi.org/10.3389/fnmol.2017.00455
van Rheenen W, Shatunov A, Dekker AM, McLaughlin RL, Diekstra FP, Pulit SL, van der Spek A, RA, Võsa U, de Jong S, Robinson MR, Yang J, Fogh I, van Doormaal PT, P Tazelaar GH, Koppers M, Blokhuis AM, Sproviero W, Jones AR, Kenna KP, van Eijk KR, Harschnitz O, Schellevis RD, Brands WJ, Medic J, Menelaou A, Vajda A, Ticozzi N, Lin K, Rogelj B, Vrabec K, Ravnik-Glavač M, Koritnik B, Zidar J, Leonardis L, Dolenc Grošelj L, Millecamps S, Salachas F, Meininger V, de Carvalho M, Pinto S, Mora JS, Rojas-García R, Polak M, Chandran S, Colville S, Swingler R, Morrison KE, Shaw PJ, Hardy J, Orrell RW, Pittman A, Sidle K, Fratta P, Malaspina A, Topp S, Petri S, Abdulla S, Drepper C, Sendtner M, Meyer T, Ophoff RA, Staats KA, Wiedau-Pazos M, Lomen-Hoerth C, van Deerlin VM, Trojanowski JQ, Elman L, McCluskey L, Nazli Basak A, Tunca C, Hamzeiy H, Parman Y, Meitinger T, Lichtner P, Radivojkov-Blagojevic M, Andres CR, Maurel C, Bensimon G, Landwehrmeyer B, Brice A, M Payan CA, Saker-Delye S, Dürr A, Wood NW, Tittmann L, Lieb W, Franke A, Rietschel M, Cichon S, Nöthen MM, Amouyel P, Tzourio C, Dartigues J-F, Uitterlinden AG, Rivadeneira F, Estrada K, Hofman A, Curtis C, Blauw HM, van der Kooi AJ, de Visser M, Goris A, Weber M, Shaw CE, Smith BN, Pansarasa O, Cereda C, del Bo R, Comi GP, Bertolin C, Sorarù G, Mazzini L, Pensato V, Gellera C, Tiloca C, Ratti A, Calvo A, Moglia C, Brunetti M, Arcuti S, Capozzo R, Zecca C, Lunetta C, Penco S, Riva N, Padovani A, Filosto M, Muller B, Jan Stuit R, Blair I, Zhang K, McCann EP, Fifita JA, Nicholson GA, Rowe DB, Pamphlett R, Kiernan MC, Grosskreutz J, Witte OW, Ringer T, Prell T, Stubendorff B, Kurth I, Hübner CA, Nigel Leigh P, Casale F, Chio A, Beghi E, Pupillo E, Tortelli R, Logroscino G, Powell J, Ludolph AC, Weishaupt JH, Robberecht W, van Damme P, Franke L, Pers TH, Brown RH, Glass JD, Landers JE, Hardiman O, Andersen PM, Corcia P, Vourc P, Silani V, Wray NR, Visscher PM, W de Bakker PI, van Es MA, Jeroen Pasterkamp R, Lewis CM, Breen G, Al-Chalabi A, van den Berg LH, Veldink JH, (2016) Genome-wide association analyses identify new risk variants and the genetic architecture of amyotrophic lateral sclerosis. Nat Publ Group. https://doi.org/10.1038/ng.3622
De Rossi P, Buggia-Prévot V, Clayton BLL, Vasquez JB, Van Sanford C, Andrew RJ, Lesnick R, Botté A, Deyts C, Salem S, Rao E, Rice RC, Parent A, Kar S, Popko B, Pytel P, Estus S, Thinakaran G (2016) Predominant expression of Alzheimer’s disease-associated BIN1 in mature oligodendrocytes and localization to white matter tracts. Mol Neurodegener 11:1–21. https://doi.org/10.1186/S13024-016-0124-1/TABLES/2
Sams EC (2021) Oligodendrocytes in the aging brain. Neuronal Signal. https://doi.org/10.1042/NS20210008
Sanchez-Contreras MY, Kouri N, Cook CN, Serie DJ, Heckman MG, Finch NA, Caselli RJ, Uitti RJ, Wszolek ZK, Graff-Radford N, Petrucelli L, Wang LS, Schellenberg GD, Dickson DW, Rademakers R, Ross OA (2018) Replication of progressive supranuclear palsy genome-wide association study identifies SLCO1A2 and DUSP10 as new susceptibility loci. Mol Neurodegener 13:1–10. https://doi.org/10.1186/S13024-018-0267-3/TABLES/4
Sapozhnikov DM, Szyf M (2021) Unraveling the functional role of DNA demethylation at specific promoters by targeted steric blockage of DNA methyltransferase with CRISPR/dCas9. Nat Commun 12:1–26. https://doi.org/10.1038/s41467-021-25991-9
Schäfer I, Müller C, Luhmann HJ, White R (2016) MOBP levels are regulated by Fyn kinase and affect the morphological differentiation of oligodendrocytes. J Cell Sci 129:930–942. https://doi.org/10.1242/JCS.172148
Shireby G, Dempster EL, Policicchio S, Smith RG, Pishva E, Chioza B, Davies JP, Burrage J, Lunnon K, Seiler Vellame D, Love S, Thomas A, Brookes K, Morgan K, Francis P, Hannon E, Mill J (2022) DNA methylation signatures of Alzheimer’s disease neuropathology in the cortex are primarily driven by variation in non-neuronal cell-types. Nat Commun 13:1–14. https://doi.org/10.1038/s41467-022-33394-7
Siming S, Aixiao L, Jiadong L, Candy W, Patrizia C-B (2008) Epigenetic memory loss in aging oligodendrocytes in the corpus callosum. Neurobiol Aging 29:452. https://doi.org/10.1016/J.NEUROBIOLAGING.2006.10.026
Simpson JE, Fernando MS, Clark L, Ince PG, Matthews F, Forster G, O’Brien JT, Barber R, Kalaria RN, Brayne C, Shaw PJ, Lewis CE, Wharton SB (2007) White matter lesions in an unselected cohort of the elderly: astrocytic, microglial and oligodendrocyte precursor cell responses. Neuropathol Appl Neurobiol 33:410–419. https://doi.org/10.1111/J.1365-2990.2007.00828.X
Singh N, Haldar S, Tripathi AK, Horback K, Wong J, Sharma D, Beserra A, Suda S, Anbalagan C, Dev S, Mukhopadhyay CK, Singh a comprehensive invited review brain iron homeostasis: from molecular mechanisms to clinical significance and therapeutic opportunities. https://doi.org/10.1089/ars.2012.4931
Siokas V, Aloizou AM, Liampas I, Bakirtzis C, Tsouris Z, Sgantzos M, Liakos P, Bogdanos DP, Hadjigeorgiou GM, Dardiotis E (2022) Myelin-associated oligodendrocyte basic protein rs616147 polymorphism as a risk factor for Parkinson’s disease. Acta Neurol Scand 145:223–228. https://doi.org/10.1111/ANE.13538
Smith AR, Wheildon G, Lunnon K (2020) Invited Review - A 5-year update on epigenome-wide association studies of DNA modifications in Alzheimer’s disease: progress, practicalities and promise. Neuropathol Appl Neurobiol 46:641–653. https://doi.org/10.1111/NAN.12650
Smith J, Banerjee R, Waly R, Urbano A, Gimenez G, Day R, Eccles MR, Weeks RJ, Chatterjee A (2021) Locus-specific DNA methylation editing in melanoma cell lines using a CRISPR-based system. Cancers (Basel). https://doi.org/10.3390/CANCERS13215433
Smith RG, Hannon E, De JPL, Chibnik L, Lott SJ, Condliffe D, Smith AR, Haroutunian V, Troakes C, Al-Sarraj S, Bennett DA, Powell J, Lovestone S, Schalkwyk L, Mill J, Lunnon K (2018) Elevated DNA methylation across a 48-kb region spanning the HOXA gene cluster is associated with Alzheimer’s disease neuropathology. Alzheimer’s & Dementia 14:1580–1588. https://doi.org/10.1016/J.JALZ.2018.01.017
Smith RG, Pishva E, Shireby G, Smith AR, Roubroeks JAY, Hannon E, Wheildon G, Mastroeni D, Gasparoni G, Riemenschneider M, Giese A, Sharp AJ, Schalkwyk L, Haroutunian V, Viechtbauer W, van den Hove DLA, Weedon M, Brokaw D, Francis PT, Thomas AJ, Love S, Morgan K, Walter J, Coleman PD, Bennett DA, De Jager PL, Mill J, Lunnon K (2021) A meta-analysis of epigenome-wide association studies in Alzheimer’s disease highlights novel differentially methylated loci across cortex. Nat Commun 12:1–13. https://doi.org/10.1038/s41467-021-23243-4
De Souza RAG, Islam SA, McEwen LM, Mathelier A, Hill A, Mah SM, Wasserman WW, Kobor MS, Leavitt BR (2016) DNA methylation profiling in human Huntington’s disease brain. Hum Mol Genet 25:2013–2030. https://doi.org/10.1093/HMG/DDW076
Spaas J, van Veggel L, Schepers M, Tiane A, van Horssen J, Wilson DM, Moya PR, Piccart E, Hellings N, Eijnde BO, Derave W, Schreiber R, Vanmierlo T (2021) Oxidative stress and impaired oligodendrocyte precursor cell differentiation in neurological disorders. Cell Mol Life Sci 78:4615–4637. https://doi.org/10.1007/S00018-021-03802-0
Stadelmann C, Timmler S, Barrantes-Freer A, Simons M (2019) Myelin in the central nervous system: structure, function, and pathology. Physiol Rev 99:1381–1431. https://doi.org/10.1152/PHYSREV.00031.2018/ASSET/IMAGES/LARGE/Z9J0031929070008.JPEG
Sun W, Zang L, Shu Q, Li X (2014) From development to diseases: the role of 5hmC in brain. Genomics 104:347–351. https://doi.org/10.1016/J.YGENO.2014.08.021
Tiane A, Schepers M, Riemens R, Rombaut B, Vandormael P, Somers V, Prickaerts J, Hellings N, van den Hove D, Vanmierlo T (2021) DNA methylation regulates the expression of the negative transcriptional regulators ID2 and ID4 during OPC differentiation. Cell Mol Life Sci 78:6631–6644. https://doi.org/10.1007/S00018-021-03927-2
Tiane A, Schepers M, Rombaut B, Hupperts R, Prickaerts J, Hellings N, van den Hove D, Vanmierlo T (2019) From OPC to oligodendrocyte: an epigenetic journey. Cells. https://doi.org/10.3390/CELLS8101236
Timsit S, Martinez S, Allinquant B, Peyron F, Puelles L, Zalc B (1995) Oligodendrocytes originate in a restricted zone of the embryonic ventral neural tube defined by DM-20 mRNA expression. J Neurosci 15:1012–1024. https://doi.org/10.1523/JNEUROSCI.15-02-01012.1995
Valério-Gomes B, Guimarães DM, Szczupak D, Lent R (2018) The absolute number of oligodendrocytes in the adult mouse brain. Front Neuroanat 12:90. https://doi.org/10.3389/FNANA.2018.00090/BIBTEX
Vallstedt A, Klos JM, Ericson J (2005) Multiple dorsoventral origins of oligodendrocyte generation in the spinal cord and hindbrain. Neuron 45:55–67. https://doi.org/10.1016/J.NEURON.2004.12.026
Vanderkraats ND, Hiken JF, Decker KF, Edwards JR (2013) Discovering high-resolution patterns of differential DNA methylation that correlate with gene expression changes. Nucleic Acids Res 41:6816–6827. https://doi.org/10.1093/NAR/GKT482
Warf BC, Fok-Seang J, Miller RH (1991) Evidence for the ventral origin of oligodendrocyte precursors in the rat spinal cord. J Neurosci 11:2477–2488. https://doi.org/10.1523/JNEUROSCI.11-08-02477.1991
Watson CT, Roussos P, Garg P, Ho DJ, Azam N, Katsel PL, Haroutunian V, Sharp AJ (2016) Genome-wide DNA methylation profiling in the superior temporal gyrus reveals epigenetic signatures associated with Alzheimer’s disease. Genome Med. https://doi.org/10.1186/S13073-015-0258-8
Weber A, Schwarz SC, Tost J, Trümbach D, Winter P, Busato F, Tacik P, Windhorst AC, Fagny M, Arzberger T, McLean C, van Swieten JC, Schwarz J, Vogt Weisenhorn D, Wurst W, Adhikary T, Dickson DW, Höglinger GU, Müller U (2018) Epigenome-wide DNA methylation profiling in progressive supranuclear palsy reveals major changes at DLX1. Nat Commun. https://doi.org/10.1038/s41467-018-05325-y
Wen KX, Milic J, El-Khodor B, Dhana K, Nano J, Pulido T, Kraja B, Zaciragic A, Bramer WM, Troup J, Chowdhury R, Arfam Ikram M, Dehghan A, Muka T, Franco OH (2016) The role of DNA methylation and histone modifications in neurodegenerative diseases: a systematic review. PLoS One 11:e0167201. https://doi.org/10.1371/JOURNAL.PONE.0167201
Whitwell JL, Master AV, Avula R, Kantarci K, Eggers SD, Edmonson HA, Jack CR, Josephs KA (2011) Clinical correlates of white matter tract degeneration in progressive supranuclear palsy. Arch Neurol 68:753–760. https://doi.org/10.1001/ARCHNEUROL.2011.107
Xu H, Dzhashiashvili Y, Shah A, Kunjamma RB, Weng Y, lan, Elbaz B, Fei Q, Jones JS, Li YI, Zhuang X, Ming G li, He C, Popko B, (2020) m6A mRNA methylation is essential for oligodendrocyte maturation and CNS myelination. Neuron 105:293-309.e5. https://doi.org/10.1016/J.NEURON.2019.12.013
Yu L, Chibnik LB, Srivastava GP, Pochet N, Yang J, Xu J, Kozubek J, Obholzer N, Leurgans SE, Schneider JA, Meissner A, de Jager PL, Bennett DA (2015) Association of brain DNA methylation in SORL1, ABCA7, HLA-DRB5, SLC24A4, and BIN1 with pathological diagnosis of Alzheimer disease. JAMA Neurol 72:15–24. https://doi.org/10.1001/JAMANEUROL.2014.3049
Zecca L, Youdim MBH, Riederer P, Connor JR, Crichton RR (2004) Iron, brain ageing and neurodegenerative disorders. Nat Rev Neurosci 5:863–873. https://doi.org/10.1038/nrn1537
Zhang L, Silva TC, Young JI, Gomez L, Schmidt MA, Hamilton-Nelson KL, Kunkle BW, Chen X, Martin ER, Wang L (2020) Epigenome-wide meta-analysis of DNA methylation differences in prefrontal cortex implicates the immune processes in Alzheimer’s disease. Nat Commun 11:1–13. https://doi.org/10.1038/s41467-020-19791-w
Zhang M, Wang J, Zhang K, Lu G, Liu Y, Ren K, Wang W, Xin D, Xu L, Mao H, Xing J, Gao X, Jin W, Berry K, Mikoshiba K, Wu S, Lu QR, Zhao X (2021) Ten-eleven translocation 1 mediated-DNA hydroxymethylation is required for myelination and remyelination in the mouse brain. Nat Commun 12:1–21. https://doi.org/10.1038/s41467-021-25353-5
Zhao X, Dai J, Ma Y, Mi Y, Cui D, Ju G, Macklin WB, Jin W (2014) Dynamics of ten-eleven translocation hydroxylase family proteins and 5-hydroxymethylcytosine in oligodendrocyte differentiation. Glia 62:914–926. https://doi.org/10.1002/GLIA.22649
Zhou T, Ahmad TK, Gozda K, Truong J, Kong J, Namaka M (2017) Implications of white matter damage in amyotrophic lateral sclerosis. Mol Med Rep 16:4379. https://doi.org/10.3892/MMR.2017.7186
Acknowledgements
We would like to thank Professor Janice Holton and Dr Sandrine Foti for kindly providing the 5mC and 5hmC immunostaining images.
Funding
KF is supported by the Medical Research Council (MR/N013867/1). RdS is supported by CurePSP, Karin & Sten Mortstedt CBD Solutions and the Reta Lila Weston Trust. TTW is supported by the Reta Lila Weston Trust and the MRC (N013255/1). CB is supported by Alzheimer’s Research UK (ARUK-RF2019B-005) and the Multiple System Atrophy Trust.
Author information
Authors and Affiliations
Contributions
KF drafted the manuscript. RdS, TTW and CB critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fodder, K., de Silva, R., Warner, T.T. et al. The contribution of DNA methylation to the (dys)function of oligodendroglia in neurodegeneration. acta neuropathol commun 11, 106 (2023). https://doi.org/10.1186/s40478-023-01607-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-023-01607-9