Abstract
Pediatric high grade gliomas (pHGG), including diffuse intrinsic pontine gliomas (DIPGs), are aggressive tumors with a dismal outcome. Radiotherapy (RT) is part of the standard of care of these tumors; however, radiotherapy only leads to a transient clinical improvement. Delta-24-RGD is a genetically engineered tumor-selective adenovirus that has shown safety and clinical efficacy in adults with recurrent gliomas. In this work, we evaluated the feasibility, safety and therapeutic efficacy of Delta-24-RGD in combination with radiotherapy in pHGGs and DIPGs models. Our results showed that the combination of Delta-24-RGD with radiotherapy was feasible and resulted in a synergistic anti-glioma effect in vitro and in vivo in pHGG and DIPG models. Interestingly, Delta-24-RGD treatment led to the downregulation of relevant DNA damage repair proteins, further sensitizing tumors cells to the effect of radiotherapy. Additionally, Delta-24-RGD/radiotherapy treatment significantly increased the trafficking of immune cells (CD3, CD4+ and CD8+) to the tumor niche compared with single treatments.
In summary, administration of the Delta-24-RGD/radiotherapy combination to pHGG and DIPG models is safe and significantly increases the overall survival of mice bearing these tumors. Our data offer a rationale for the combination Delta-24-RGD/radiotherapy as a therapeutic option for children with these tumors.
Significance
Delta-24-RGD/radiotherapy administration is safe and significantly increases the survival of treated mice. These positive data underscore the urge to translate this approach to the clinical treatment of children with pHGG and DIPGs.
Similar content being viewed by others
Introduction
Pediatric high grade gliomas (pHGG) and diffuse intrinsic pontine gliomas (DIPGs) are malignant tumors present with an aggressive behavior [7]. Integrated molecular profiling has contributed to renew the classification of these tumors by considering the mutations encoding histone H3 variants that determine localization, age of presentation, clinical outcome or even radiological features [18, 25, 30, 41].
The current standard therapy for pHGG consists of maximal surgical resection followed by temozolomide/radiotherapy (RT) [35]. In the case of DIPGs, effective therapeutic options are limited, and the standard of care is RT. RT offers a temporal decrease of clinical symptoms and an increase in the overall survival; however, it is not curative [12] . Despite combined efforts to develop new therapies for these aggressive tumors, over the last decade, the overall survival is 15 months for pHGG patients and approximately 9 to 11 months for DIPGs [16].
RT induces DNA damage [24], resulting in the triggering of either cell death programs or cell survival mechanisms, such as apoptosis, necrosis or autophagy, among others [6]. Radiation-induced cell responses mediated by DNA damage cause tumor antigens release, generation of ROS species or production of cytokines, which awake the immune system [31]. Recent studies demonstrate that RT also induces an immunogenic cell death that promotes the recruitment of different immune populations to the tumor bed. In some instances, RT triggers an abscopal effect which results in an effective immunity against the tumor [9]. However, the RT mediated abscopal effect is seen in few patients and many times is hampered by the tolerance and an immunosuppressive tumor microenvironment [28].
In this study, we evaluated whether the combination of the oncolytic adenovirus, Delta-24-RGD (DNX-2401) [36], genetically engineered to destroy cancer cells, in combination with RT would result in a superior antitumor effect in pHGG and DIPGs when compared to either agent alone. Delta-24-RGD administration has been demonstrated to be safe and therapeutically effective in a subset of adult patients with recurrent glioblastoma [22]. Moreover, clinical and preclinical studies with Delta-24-RGD have shown that part of the antitumor effect is due to the capacity of the virus to boost or awake the patient’s immune system [15]. We have previously shown that administration of Delta-24-RGD alone resulted in a robust antitumor effect in vitro and in vivo in pHGGs and DIPGs models (Martinez-Velez et al., 2019, nature communication, in press). Moreover, our group and others have shown that adenoviral infection inhibits the cellular DNA repair machinery to increase its replication potency [34]. We hypothesized that DNA repair inhibition by viral administration could sensitize tumor cells to irradiation, increasing the therapeutic effect [29]. Furthermore, RT/Delta-24-RGD administration will increase the release of tumor antigens overcoming the “cold” status of pHGG and DIPG tumors and triggering a stronger immune response that could translate into a synergistic antitumor effect and an increase of the overall survival in these patients.
Material and methods
Cell lines and culture conditions
Pediatric glioma CHLA-03-AA (H3 WT) was obtained from the America Type Culture Collection (ATCC, Manassas, VA). PBT-24 pediatric glioma cell line was developed from a biopsy (H3 WT) obtained at the University Clinic of Navarra from a 13-year-old boy. Tumor samples were obtained with a signed-informed consent. Tumors were cut into smaller pieces, and cells were dissociated enzymatically. Cell obtained from dissociation were cultured with RPMI medium supplemented with 10% FBS and 1% antibiotic. Cell lines obtained from ATCC or Chilren Oncology Group (COG) were cultured following manufacturer specifications. The DIPG cell line TP54 (H3.3K27M) was kindly provided by Drs. Marie-Pierre Junier and Hervé Cheneiwess (INSERM Institute, Paris, France), and the SU-DIPG IV (H3.1K27M) cell line was a kind gift from Michelle Monje (Stanford University, CA). The DIPG cell line was maintained as neurospheres cultured in a specialized serum-free basal medium complemented with a human neural stem cell proliferation supplement (NeuroCult™ NS-A Proliferation Kit, #05751, STEMCELL Technologies) supplemented with basic fibroblast growth factor and epidermal growth factor (20 ng/mL Sigma-Aldrich, St Louis, MO). All cells were maintained in a humidified atmosphere containing 5% CO2 at 37 °C. All of the cell lines were tested and authenticated at the CIMA Genomic Core Facility (Pamplona, Spain) using short tandem repeats DNA profiling.
The murine DIPG cell lines NP53 and XFM were provided by Dr. Becher (Northwestern University, Chicago, IL). Cell lines were generated from DIPG tumors arisen in genetically modified mice. The NP53 cell line was generated from tumors that arose in a DIPG mouse model induced by PDGF-B signaling, p53 loss, and ectopic H3.3-K27 M [10]. The XFM cell line was generated from tumors developed in a mouse model driven by PDGF-B signaling and Ink4a and ARF loss [3].
Adenovirus construction and infection
Construction of Delta-24-RGD and viral infection have been previously described [26, 40].
Viral replication assays
pHGG and DIPG cells were seeded at a density of 2 × 105 cells/well in 6-well plates and infected with 10 MOI of Delta-24-RGD, and 4 h after infection, these cells were irradiated with three different doses (3, 6 and 12 Gy). Three days later, cells were collected, and the final amount of virus was determined by means of a method based on anti-hexon staining in HEK293 cells [4].
Cell viability assay
Cells were seeded at a density of 2 × 105 cells per well in 6-well plates, and the next day, cells were infected with 10 MOIs of Delta-24-RGD. In addition, cells were irradiated at doses of 3, 6 and 12 Gy. Cell viability was assessed 5 days later using trypan blue. Dose–response curves were analyzed using GraphPad software. Quantification of viability was measured in triplicate, and each experiment was performed three times. After fitting the combined dose-response curve from a single representative experiment to a Chou–Talalay line, Chou–Talalay combination indices (CIs) were calculated with Calcusyn software (Biosoft, Cambridge, UK). Levels of interaction are defined as follows: CI > 1.1 indicates antagonism, CI between 0.9 and 1.1 indicates additive effect, and CI < 0.9 indicates synergy [5]. A mean CI was calculated from data points with the fraction affected (FA) > 0.5. The FA range used to calculate the average CI values in the combination experiments did not include CI values of FA < 0.5, which was not considered a relevant growth inhibition because one aims to achieve the maximal effect of the combination tested on cancer cells.
Immunoblotting
For immunoblotting assays, samples were subjected to SDS-Tris-glycine gel electrophoresis. Membranes were incubated with the following antibodies: E1A, (Santa Cruz Biotechnology, Santa Cruz, CA), fiber (NeoMarkers, Fremont, CA), Mre-11, Rad 50, Rad 51, pH2Ax, MPG (Cell Signaling, Danvers, MA) and GRB-2 (Sigma-Aldrich). The membranes were developed according to Amersham’s enhanced chemiluminescence protocol.
Animal studies
Ethical approval for animal studies was granted by the Animal Ethical Committee of the University of Navarra (CEEA; Comité Etico de Experimentación Animal under the protocol number CEEA/069–13). All animal studies were performed in the veterinary facilities of the Center for Applied Medical Research in accordance with institutional, regional, and national laws and ethical guidelines for experimental animal care. For the orthotopic supratentorial model, CHLA-03-AA cells (5 × 105) were engrafted by injection into the caudate nucleus of athymic mice. TP54 cells (5 × 105) developed DIPG tumors by injection of those cells into the pons of athymic mice in both models, we have utilized a guide-screw system. (Taconic Farms, Inc.). NP53 cells (5 × 105) were implanted in transgenic mice, kindly provided by Dr. Oren Becher. Cells were administered in 3–4 μl of PBS. Animals were randomized to 2 or 4 groups (controls without treatment, Delta-24-RGD, irradiated, and combination of radiation and Delta-24-RGD). Delta-24-RGD (107 pfu/animal) was administered intracranially once in 3–4 μl 3 days after cell implantation. A week later, brain tumors were irradiated (4 Gy) using the bolt as a guide to administer irradiation to that area.
Tumor establishment procedure
Under aseptic conditions and with all materials sterilized according to standard techniques, mice of 4 weeks of age were anesthetized by intraperitoneal injection with ketamine and xilacyne solution. The animal heads were supported by a couple of rolled gauzes so that when the screw was inserted, pressure applied over neck and head structures was better tolerated by the animal.
We prepared mice head skin with povidone iodine solution prior to make a 5 mm-long lineal skin incision with 23-size scalpel and expose skull sutures. We first made a small mark according to the coordinates with a small 15-gauge needle which was subsequently widened with a hand-controlled twist drill which penetrates the skull. Next, we introduced the screw with its specific screwdriver by applying slight pressure throughout the previous twist hole. The coordinates for generation of DIPG tumors are 1.0 mm right to lambda and just posterior (0.8 mm) to lambdoid suture, while coordinates for pHGG tumors are from bregma (intersection between coronal and sagittal suture) 1 mm anterior and 2.5 mm to the right. Thereafter the needle of Hamilton syringe is slowly introduced into the hole by applying gentle pressure until the sleeve/cuff from the syringe reaches the screw surface. The desired depth to reach brainstem is 6.5 mm and depth for hemispheric tumors (pHGG) is 3.5 mm. Cell suspension was carefully injected using an infusion pump (Harvard Apparatus) over 20 min.
Comet assay
Cell lines were irradiated with ascending doses (ranging from 3 to 12 Gy) and infected with Delta-24-RGD at 10 MOIs; 72 h later, cells were recollected. Cells were prepared following the manufacturer protocol provided by CometAssay® kit (Trevigen, Inc., Gaithersburg, MD).
Immunohistochemical analysis
The paraffin-embedded sections of the mice brains were immunostained for antibodies specific for adenoviral mouse-hexon (Chemicon International, Inc., Temecula, CA), adenovirus rabbit-E1A, (Santa Cruz Biotechnology, Santa Cruz, CA), pH2Ax (Cell Signaling, Danvers, MA), CD3 (NeoMarkers, Fremont, CA), CD4 (Abcam, Cambridge, MA) CD8a (Cell Signaling, Danvers, MA), FoxP3 (eBiosciences, Thermo Fisher, Waltham, MA) and vimentin clone V9 (IS30, Dako Denmark A/S, Glostrup, Denmark), following manufacturer procedures. For immunohistochemical staining, Vectastain ABC kits (Vector Laboratories Inc., Burlingame, CA) were used according the manufacturer’s instructions.
Statistical analysis
For the in vitro experiments, data are expressed as the mean ± SD, and comparisons were evaluated by the two-tailed Student’s t test or ANOVA. The effect of Delta-24-RGD and RT, alone or in combination, and pHGG and DIPG xenografts was assessed by plotting survival curves according to the Kaplan-Meier method. Survival in different treatment groups was compared using the log-rank test. The program GraphPad Prism 5 (Statistical Software for Sciences) was used for the statistical analysis.
Results
Combination of Delta-24-RGD with RT exerts a synergistic antitumor effect in pHGG and DIPG in vitro and in vivo
First, to evaluate whether irradiation would interfere with viral replication, we infected pHGG and DIPG cells with Delta-24-RGD (10 MOIs) followed by increasing doses of RT: 3 , 6 and 12 Gy. After the combined treatment, we observed a robust expression of the viral late protein fiber regardless of the RT dosage used (Fig. 1a and Additional file 1: Figure S1A). This result suggested that RT does not interfere with the viral cycle. To support this notion, we quantified the viral progeny present in cells after irradiation with increasing Gys. We found that Delta-24-RGD replication was not hindered by any of the irradiation doses evaluated (Fig. 1b and Additional file 1: Figure S1B). These data confirmed the feasibility of combining RT with the Delta-24-RGD virus. Next, we evaluated the anticancer effect of this combination in a panel of the pHGG and DIPG cell lines. Our results showed that RT alone, at the highest dose used of 12 Gy, induced only a modest increment of cell death, 30–40%, in the pHGG (CHLA-03-AA and PBT-24) and DIPG cell lines (TP54 and SU-DIPG IV) (Fig. 1c, Additional file 1: Figure S1C and Table 1). The TP54 DIPG cell line was more susceptible to RT, with a 70% cell death at the 12 Gy dose (Fig. 1c and Additional file 1: Figure S2A).
Radiotherapy is amenable to combine with Delta-24- in vitro and in vivo in the DIPG and pHGG models. a Evaluation by western blotting of the expression of viral proteins after Delta-24-RGD (10 MOIs) infection and subsequent irradiation (3 , 6 and 12 Gy) in TP54 and CHLA-03-AA. b Quantification of Delta-24-RGD replication in the indicated cell lines irradiated with different Gy doses. The viral titers were determined 3 days after infection at an MOI of 10 by an anti-hexon staining-based method in 293 cells and expressed as plaque-forming units (pfu) per milliliter. Data are shown as the mean ± SD of three independent experiments and analyzed with two-tailed Student-t test, not significant differences were found. c Cell viability analyses of irradiated cells at the indicated Gy doses alone (Mock; control with a mock infection) or in combination with Delta-24-RGD. Cell viability was assessed 5 days after irradiation and viral infection using an automatic cell counter that measures cell viability (life, death and total cells) with the standard trypan blue reaction. Data are shown as the percentage (the mean ± SD) of viability after treatments and relative to control cells (neither infected nor irradiated). Statistical significance were calculated using two-tailed Student-t test, ns, not significative; *, P < 0.05; **, P < 0.01; ***, P < 0.001. d Kaplan-Meier survival curves of nude mice bearing orthotopic DIPGs (TP54) or pHGG (CHLA-03-AA) tumors that were treated with either Delta-24-RGD (107 pfu), irradiation (4 Gys) or combined treatment. Log-rank test were used for statistical analyses
Combination of RT with Delta-24-RGD induced an increase in the cytotoxicity with a viability decrease of approximately 20–40% when compared with the single treatment (Fig. 1c and Table 1) (P < 0.001). Evaluation of the combinatory index (CI) showed that RT plus Delta-24-RGD had a synergistic antiglioma effect in all doses tested in the PBT-24 and TP54 cell line. In the CHLA-03-AA and SU-DIPG IV cell lines, combination treatment presented a synergistic effect (CI = 0.17–0.76) at the highest irradiation doses (6 and 12 Gy); meanwhile, at the lowest irradiation dose (3 Gy), an additive effect with Delta-24-RGD resulted (CI = 0.9–1.1) (Table 1).
Next, we wanted to assess whether in vivo combination of Delta-24-RGD with RT would show the same synergistic effect that we observed in vitro in the pHGG and DIPG cell lines to determine the optimal dose to the mice pons. The results showed that any of tested doses evaluated presented toxicity (Additional file 1: Table S1). Next, we evaluated which dose accurately reproduced the clinical behavior presented in patients. We established that 4 Gy irradiation produces a transient delay in tumor growth similar to that in patients but with no curative effect.
We used the CHLA-03-AA (pHGG) and TP54 (DIPG) cell lines to assess the in vivo combination efficacy. A single dose (107 pfu) of Delta-24-RGD was injected intratumorally at day 3 followed by RT (4 Gy) at day 4. Animals were monitored during the experiment, and they were sacrificed when they presented signals of physical deterioration derived from high tumor burden presence.
Survival analyses showed that RT increased the median survival of mice in 6 days in the TP54 model (P = 0.39) (Fig. 1d and Table 2) and in 7 days in the CHLA-03-AA model (P = 0.003) (Fig. 1d). Combination of virus/RT compared with single RT significantly increased the survival in both models (P = 0.009 and P < 0.006, respectively). Importantly, combination treatment of mice bearing the CHLA-03-AA resulted in 3 long-term survivors free of disease (N = 3) (P < 0.0001). Mice bearing the TP54 orthotopic DIPG model also benefitted from the RT/virus combination with a significant increase of 20 days (P = 0.01) in the overall survival.
These data suggest that combination of virus and RT could be synergistic not only in vitro but also importantly in vivo, allowing a reduction in the RT doses to achieve the same effect.
In summary, the combination of irradiation and Delta-24-RGD is a feasible therapeutic strategy that increases the antitumor effect in vitro and increases the overall survival when compared with single treatment (RT or Delta-24-RGD) administration in pHGG and DIPG models.
Delta-24-RGD inhibits important proteins involved in the DNA damage cellular response
RT induces DNA damage in cancer cells, and hence, if left unrepaired, the cells die [24]. Of importance, our group and others [14, 17, 20, 34] have shown that adenoviral proteins are able to inhibit different components of the cell DNA damage repair machinery to facilitate their replication in the host. Interestingly, viral inhibition of the DNA damage repair protein could contribute to sensitizing tumor cells to agents that cause DNA damage. Therefore, we evaluated the expression of several proteins involved in DNA damage to understand whether the inhibition of the DNA damage repair machinery could be underlying the synergistic effect of treatment combination.
We observed that Delta-24-RGD infection resulted in the inhibition of cellular machinery, involving Rad50 and Mre11 proteins; both proteins are part of the MRN complex [21, 33] which is involved in the repair of double strand breaks (DSB) (Fig. 2a and Additional file 1: Figure S3A); Rad 51 is also inhibited, a protein with a major role in the homologous recombination repair (HRR [13, 27]). MPG protein is able to initiate the base excision repair (BER) mechanism that repairs alkylating bases [1, 39, 42] (Fig. 2a and Additional file 1: Figure S3A). The expression of these proteins is altered in refractory cancer cells as machinery of resistance to chemotherapy or radiotherapy [2, 44] .Interestingly, pH2Ax protein is also inhibited when tumor cells are infected, even after higher doses of irradiation (Fig. 2a and Additional file 1: Figure S3A). Phosphorylation of H2Ax marks a double strand break; therefore, pH2Ax inhibition could represent an advantage for the therapy. DNA repair machinery of infected tumor cells is unable to detect DNA damage caused by RT (Fig. 2b, c and Additional file 1: Figure S3B and S3C) and not repair it, increasing DNA damage that prompts in cell death.
Delta-24-RGD downregulation of the cellular DNA damage repair machinery in the DIPG and pHGG cell lines. a Expression analyses by western blotting of the relevant proteins involved in the DNA damage response to RT in the DIPG and pHGG cell lines after the indicated treatments. The proteins levels were evaluated 72 h after cells were treated. b Evaluation of DNA damage upon treatment with Delta-24-RGD and/or RT by the comet assay. TP54 cells were administered the indicated treatments, and 72 h later, the induction of comets was assessed. Representative photomicrographs of comets shown by the cells after the indicated treatment (magnification, × 200). c Quantification of positive cells showing comets after the indicated treatment. Data are shown as the percentage of comet tails found per treatment percentage (n = 500 cells per treatment); bars represent means ± SD. All experiments were performed in triplicate and analyzed using two-way ANOVA and corrected for multiple comparision with Bonferroni posttest; **, P < 0.01 and ***, P < 0.001. d Hexon immune-staining representative images (scale bar =100um) after the indicated treatments. The above images images show differences in hexon protein expression in CHLA-03-AA tumors while below images show hexon staining in TP54 tumors
Histological analyses showed that Delta-24-RGD combined with RT is able to replicate in pHGG and DIPG in vivo. Positive immuno-staining against viral proteins are found in tumors after irradiation in vivo (Fig. 2d).
Our results suggest that the synergistic antitumor effect that we observed in combination adenovirus/RT could be explained, at least in part, by the inhibition that the adenovirus exerts on the cell DNA damage repair machinery and the subsequent increase in DNA damage.
Delta-24-RGD combined with RT enhanced the antitumor effect in murine DIPG cell lines
In addition, we wanted to elucidate how the immune response contributed to the synergistic effect of this combination.
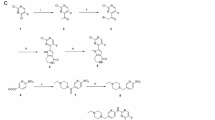
To this end, we evaluated the combination of Delta-24-RGD plus RT in the XFM and NP53 murine DIPG cell lines [3, 10]. Previously, we showed that these cell lines were semipermissive to Delta-24-RGD (Martinez-Velez et al., 2019 in review); therefore, these cell lines constitute a good model to analyze immune response to the viral infection. We observed that fiber protein, a late protein that is part of the adenoviral capsid, is robustly expressed after the highest dose of RT (Fig. 3a). At the functional level, we did not observe variations between viral titers obtained in non-irradiated versus irradiated infected cells (Fig. 3b). Importantly, treatment of these cell lines with RT alone was not capable of decreasing the viability more than 50% at the highest dose used (12 Gy), given that NP53 is the most sensitive cell line. The addition of Delta-24-RGD resulted in a significant decrease in cell viability, between 40 and 70%, compared with the single treatment (Fig. 3c).
Combination of Delta-24-RGD/radiotherapy exerts a potent oncolytic effect in the NP53 and XFM murine DIPG cell lines. a Analyses of the expression of viral late protein fiber in murine cell lines 42 h after the indicated treatments by western blotting. b Quantification of Delta-24-RGD replication in the indicated cell lines. Viral titers were determined 3 days after infection with Delta-24-RGD (100 MOIs) and irradiation with either 3, 6 or 12 Gy. The viral titers were quantified using the anti-hexon staining-based method in 293 cells and expressed as plaque-forming units (pfu) per milliliter. The data are shown as the mean ± SD of three independent experiments. c Cell viability analyses of the combination treatment in DIPG murine cell lines. Cell viability was assessed 5 days after irradiation and/or viral infection using an automatic cell counter that measures cell viability (life, death and total cells) with the standard trypan blue reaction. Data are shown as the percentage (mean ± SD) of viability after irradiation at the indicated doses alone or also infected with Delta-24-RGD and analyzed with Two-tailed Student t-test
Therefore, we can conclude that the combination of Delta-24-RGD/RT increases the cytotoxicity of a single treatment in DIPG murine cell lines in vitro.
Delta-24-RGD /RT treatment triggers a potent immune response in a murine DIPG model
Since it has been described that anti-tumor immune effect mediated by local RT is more prominent after a previous immune activation [8, 32] we analyzed whether combined Delta-24-RGD/RT treatment resulted in a heightened immune response.
Mice bearing NP53 DIPG tumors were administered a single injection of Delta-24-RGD followed 1 day later by RT. Histopathology examination of mice tumors treated with the combination showed an increase in tumor immune CD3 infiltration when compared with the single treatment. Moreover, we observed perivascular cuffing in mice brain treated with RT/Delta-24-RGD, indicating an immune cell recruitment triggered by the combination, mainly CD4+ and CD8+ (Figs. 4a, b, c and Additional file 1: Figure S4).
Administration of Delta-24-RGD in combination with radiotherapy heightens the immune infiltration in DIPG murine tumors. a Representative images of immune infiltration, such as perivascular cuffing, after Delta-24-RGD/RT treatment. The mouse brain stained against CD3 (a), CD4 (b) and CD8 (c). d Quantification of positive CD3+, e CD4+, and f CD8+ cell infiltration per mm2 of DIPG tumors. Graph showing the quantification of positive cells infiltrating the brain 15 days after the indicated treatments per mm2 (PBS, RT, Delta-24-RGD and Delta-24-RGD/RT; n = 2–3). Comparisons were analyzed with One-way ANOVA. g Quantification of Granzyme B, IFN gamma, CD8a and CD4 mRNA expression. The data shown represent mRNA expression in tumors treated with Delta-24-RGD, RT, and Delta-24-RGD/RT normalized to the average of PBS-tumors mRNA expression (n = 2). Data were analyzed with One-way ANOVA
Quantification of CD3, CD4 and CD8 positive cells (Figs. 3d, e and f) showed a modest increase in lymphocyte infiltration in irradiated tumors (2.02, 3.06 and 3.08-fold, respectively); this infiltration was higher in tumors treated with Delta-24-RGD alone (2.46, 4.6 and 5.35-fold, respectively). Tumors treated with both agents showed a significant increase in the recruitment of immune populations (7.83, 6.2 and 8.89-fold) (CD3+, CD4+ and CD8+) (P = 0.032, P = 0.318 and P = 0.065), respectively. Evaluation of pro-inflammatory cytokines expression levels, such as Granzyme B (P = 0.19) and IFNg (P = 0.13), in addition to CD4 (P = 0.57) and CD8a (P = 0.16) expression levels, presented an increased trend in tumors treated with Delta-24-RGD and irradiation compared with single treatments (Fig. 3g), indicating that the combination stimulates the immune response in DIPG tumors. All together, these results demonstrate that combination of RT and Delta-24-RGD in vivo triggers a potent immune response that increases the immune recruitment at the tumor bed and the production of inflammatory cytokines that could mediate an antitumor immune response.
Discussion
Previous works demonstrated that the oncolytic adenovirus Delta-24-RGD exerts a potent antitumor effect in pHGG and DIPG preclinical models. pHGG and specifically, DIPGs, are the most aggressive brain tumors with dismal outcomes and ineffective therapeutic options [38]. Clinical trials testing single agents as unique treatments have resulted in limited efficacy. The standard treatment for unresectable tumors is hypo fractionated RT [11], which improves the quality of life of these children transitorily, but in a few months, the tumors will relapse. Therefore, the valuation of the therapeutic benefit of the Delta-24-RGD/RT combination is extremely timely.
One of our findings was that the increase in cytotoxicity of Delta-24-RGD/RT in vitro and in vivo in pHGG and DIPG models could be mediated by the inhibition of the cellular DNA repair mechanisms resulting in an increase in DNA damage. Delta-24-RGD administration has been described to inhibit proteins involved in DNA repair to allow viral replication [29]. We observed the inhibition of proteins that play a main role in double strand break repair, such as Rad51, MPG and proteins that are part of the MRN complex, in pediatric glioma cells infected with Delta-24-RGD. The inhibition of the host cellular DNA repair machinery is sustained after irradiation, resulting in cellular machinery incapable of repairing the DNA damage and thus sensitizing cells to irradiation-induced cell death. Inhibition of Rad51 and MPG has been described to sensitize glioma cells to other agents [43], such as TMZ [2], a drug that is commonly used to treat brain tumors, opening new therapeutic combination options.
Recent evidence has shown that in addition to tumor growth delay mediated by DNA damage-induced cell death, RT also performs an immunostimulatory effect that is triggered by the activation of immune cells or by the modification of the tumor bed [8, 31]. The antitumor systemic effect found after local irradiation is defined as the abscopal effect and induces tumor recognition by immune cells [19]. Delta-24-RGD has been shown to unleash an immune response in a clinical trial phase I/II performed in recurrent adult gliomas [22].
We observed that Delta-24-RGD/RT increased the lymphocyte infiltration in DIPG tumors (including CD4+ and CD8+ cells), and the mRNA evaluation showed an increase in the expression of several cytokines. Viral administration stimulates immune infiltration, which that overcomes the immune “cold” status of these tumors [23]. It has been hypothesized that RT fails to develop an abscopal effect because of the active immunosuppression sustained by the tumor microenvironment. The immune system boost induced by Delta-24-RGD administration offers the immune activation that is necessary to stimulate the trafficking of immune specific effector cells into the tumor niche that RT needs to trigger the abscopal effect.
Therefore, Delta-24-RGD/RT administration could represent a promising therapeutic combination, considering the awakening of the immune system, which could increase the probability of developing a specific immune response against tumor cells that would translate to an effective antitumor effect.
Our results have supported the opening of a new clinical trial phase I/II in our institution to evaluate the safety and efficacy of Delta-24-RGD administration followed by RT in patients with newly diagnosed DIPG [37].
Conclusion
In conclusion, Delta-24-RGD alone or in combination with RT is a promising therapy for DIPG and pHGG patients, and additional studies to understand the virus-induced immune response in patients could improve immune-virotherapy approaches to fight against these aggressive tumors.
References
Adhikari S, Üren A, Roy R (2009) Excised damaged base determines the turnover of human N-methylpurine-DNA glycosylase. DNA Repair (Amst) 8(10):1201–1206. https://doi.org/10.1016/j.dnarep.2009.06.005
Agnihotri S, Gajadhar AS, Ternamian C et al (2012) Alkylpurine-DNA-N-glycosylase confers resistance to temozolomide in xenograft models of glioblastoma multiforme and is associated with poor survival in patients. J Clin Invest 122(1):253–266. https://doi.org/10.1172/JCI59334
Barton KL, Misuraca K, Cordero F et al (2013) PD-0332991, a CDK4/6 inhibitor, significantly prolongs survival in a genetically engineered mouse model of brainstem glioma. PLoS One 8(10). https://doi.org/10.1371/journal.pone.0077639
Cascallo M, Gros A, Bayo N, Serrano T, Capella G, Alemany R (2006) Deletion of VAI and VAII RNA genes in the design of oncolytic adenoviruses. Hum Gene Ther 17(9):929–940. doi. https://doi.org/10.1089/hum.2006.17.929
Chou TC, Talalay P (1984) Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv Enzym Regul 22(C):27–55. https://doi.org/10.1016/0065-2571(84)90007-4
Deloch L, Derer A, Hartmann J, Frey B, Fietkau R, Gaipl US (2016) Modern radiotherapy concepts and the impact of radiation on immune activation. Front Oncol 6. https://doi.org/10.3389/fonc.2016.00141
Fangusaro J (2009) Pediatric high-grade gliomas and diffuse intrinsic pontine gliomas. J Child Neurol 24:1409–1417. https://doi.org/10.1177/0883073809338960
Frey B, Rubner Y, Wunderlich R et al (2012) Induction of Abscopal anti-tumor immunity and immunogenic tumor cell death by ionizing irradiation - implications for Cancer therapies. Curr Med Chem 19(12):1751–1764. https://doi.org/10.2174/092986712800099811
Golden EB, Apetoh L (2015) Radiotherapy and immunogenic cell death. Semin Radiat Oncol 25(1):11–17. https://doi.org/10.1016/j.semradonc.2014.07.005
Halvorson KG, Barton KL, Schroeder K et al (2015) A high-throughput in vitro drug screen in a genetically engineered mouse model of diffuse intrinsic pontine glioma identifies BMS-754807 as a promising therapeutic agent. PLoS One 10(3):e0118926. doi. https://doi.org/10.1371/journal.pone.0118926
Hankinson TC, Patibandla MR, Green A et al (2016) Hypofractionated radiotherapy for children with diffuse intrinsic pontine gliomas. Pediatr Blood Cancer 63(4):716–718. https://doi.org/10.1002/pbc.25836
Janssens GORJ, Gidding CEM, Van Lindert EJ et al (2009) The role of Hypofractionation radiotherapy for diffuse intrinsic brainstem glioma in children: a pilot study. Int J Radiat Oncol Biol Phys 73(3):722–726. https://doi.org/10.1016/j.ijrobp.2008.05.030
Jenkins SS, Mukherjee S, Heyer W-D (2016) DNA repair by homologous recombination. Encycl Cell Biol. https://doi.org/10.1016/B978-0-12-394447-4.10048-3
Jiang H, Alonso MM, Gomez-Manzano C, Piao Y, Fueyo J (2006) Oncolytic viruses and DNA-repair machinery: overcoming chemoresistance of gliomas. Expert Rev Anticancer Ther 6(11):1585–1592. https://doi.org/10.1586/14737140.6.11.1585
Jiang H, Clise-Dwyer K, Ruisaard KE et al (2014) Delta-24-RGD oncolytic adenovirus elicits anti-glioma immunity in an immunocompetent mouse model. PLoS One 9(5):e97407. doi. https://doi.org/10.1371/journal.pone.0097407
Jones C, Karajannis MA, Jones DTW et al (2017) Pediatric high-grade glioma: biologically and clinically in need of new thinking. Neuro-Oncology 19(2):153–161. https://doi.org/10.1093/neuonc/now101
Kanai R, Rabkin SD, Yip S et al (2012) Oncolytic virus-mediated manipulation of DNA damage responses: synergy with chemotherapy in killing glioblastoma stem cells. J Natl Cancer Inst 104(1):42–55. doi. https://doi.org/10.1093/jnci/djr509
Korshunov A, Ryzhova M, Hovestadt V et al (2015) Integrated analysis of pediatric glioblastoma reveals a subset of biologically favorable tumors with associated molecular prognostic markers. Acta Neuropathol 129(5):669–678. https://doi.org/10.1007/s00401-015-1405-4
Kroemer G, Galluzzi L, Kepp O, Zitvogel L (2013) Immunogenic cell death in Cancer therapy ICD: immunogenic cell death. Annu Rev Immunol 31(March):51–72. https://doi.org/10.1146/annurev-immunol-032712-100008
Kuroda S, Fujiwara T, Shirakawa Y et al (2010) Telomerase-dependent oncolytic adenovirus sensitizes human cancer cells to ionizing radiation via inhibition of DNA repair machinery. Cancer Res 70(22):9339–9348. https://doi.org/10.1158/0008-5472.CAN-10-2333
Lamarche BJ, Orazio NI, Weitzman MD (2010) The MRN complex in double-strand break repair and telomere maintenance. FEBS Lett 584(17):3682–3695. https://doi.org/10.1016/j.febslet.2010.07.029
Lang FF, Conrad C, Gomez-Manzano C et al (2018:JCO2017.75.821) Phase I study of DNX-2401 (Delta-24-RGD) oncolytic adenovirus: replication and immunotherapeutic effects in recurrent malignant glioma. J Clin Oncol. https://doi.org/10.1200/JCO.2017.75.8219
Lin GL, Nagaraja S, Filbin MG, Suvà ML, Vogel H, Monje M (2018) Non-inflammatory tumor microenvironment of diffuse intrinsic pontine glioma. Acta Neuropathol Commun 6(1):51. https://doi.org/10.1186/s40478-018-0553-x
Lomax ME, Folkes LK, O’Neill P (2013) Biological consequences of radiation-induced DNA damage: relevance to radiotherapy. Clin Oncol 25(10):578–585. https://doi.org/10.1016/j.clon.2013.06.007
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131(6):803–820. doi. https://doi.org/10.1007/s00401-016-1545-1
Manzano FRG, Fuller C, Khan G, Conrad A, Liu C, Jiang T-J, Lemoine H, Suzuki M, Sawaya K, Curiel R, David Y, Alfred Lang WK, Frederick JA (2003) Preclinical characterization of the antiglioma activity of a tropism-enhanced adenovirus targeted to the retinoblastoma pathway. J Natl Cancer Inst 95(9):652–660. https://doi.org/10.1093/jnci/95.9.652
Martin JS, Winkelmann N, Petalcorin MIR, McIlwraith MJ, Boulton SJ (2005) RAD-51-dependent and -independent roles of a Caenorhabditis elegans BRCA2-related protein during DNA double-strand break repair. Mol Cell Biol 25(8):3127–3139. https://doi.org/10.1128/MCB.25.8.3127-3139.2005
Ngwa W, Irabor OC, Schoenfeld J, Hesser J, Demaria S, Formenti SC (2017;in press) Boosting the Abscopal effect of local radiotherapy. Nat Rev Cancer. https://doi.org/10.1038/nrc.2018.6
O’Cathail SM, Pokrovska TD, Maughan TS, Fisher KD, Seymour LW, Hawkins MA (2017) Combining oncolytic adenovirus with radiation—a paradigm for the future of Radiosensitization. Front Oncol 7. https://doi.org/10.3389/fonc.2017.00153
Paugh BS, Qu C, Jones C et al (2010) Integrated molecular genetic profiling of pediatric high-grade gliomas reveals key differences with the adult disease. J Clin Oncol 28(18):3061–3068. https://doi.org/10.1200/JCO.2009.26.7252
Rödel F, Frey B, Multhoff G, Gaipl U (2015) Contribution of the immune system to bystander and non-targeted effects of ionizing radiation. Cancer Lett 356(1):105–113. https://doi.org/10.1016/j.canlet.2013.09.015
Rubner Y, Wunderlich R, Rühle P-F et al (2012) How does ionizing irradiation contribute to the induction of anti-tumor immunity? Front Oncol 2. https://doi.org/10.3389/fonc.2012.00075
Rupnik A, Grenon M, Lowndes N (2008) The MRN complex. Curr Biol 18(11). https://doi.org/10.1016/j.cub.2008.03.040
Schwartz RA, Palacios JA, Cassell GD, Adam S, Giacca M, Weitzman MD (2007) The Mre11/Rad50/Nbs1 complex limits adeno-associated virus transduction and replication. J Virol 81(23):12936–12945. https://doi.org/10.1128/JVI.01523-07
Stupp R, Hegi ME, Mason WP et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10(5):459–466. https://doi.org/10.1016/S1470-2045(09)70025-7 [doi]
Suzuki K, Fueyo J, Krasnykh V, Reynolds PN, Curiel DT, Alemany R (2001) A conditionally replicative adenovirus with enhanced infectivity shows improved oncolytic potency. Clin Cancer Res 7(1):120–126
Tejada S, Alonso M, Patiño A, Fueyo J, Gomez-Manzano C, Diez-Valle R (2017) Phase I trial of DNX-2401 for diffuse intrinsic pontine glioma newly diagnosed in pediatric patients. Neurosurgery. https://doi.org/10.1093/neuros/nyx507
Vanan MI, Eisenstat DD (2015) DIPG in children – what can we learn from the past? Front Oncol 5. https://doi.org/10.3389/fonc.2015.00237
Wallace SS, Murphy DL, Sweasy JB (2012) Base excision repair and cancer. Cancer Lett 327(1–2):73–89. https://doi.org/10.1016/j.canlet.2011.12.038
Witlox AM, Van Beusechem VW, Molenaar B et al (2004) Conditionally replicative adenovirus with tropism expanded towards integrins inhibits osteosarcoma tumor growth in vitro and in vivo. Clin Cancer Res 10(1 Pt 1):61–67. https://doi.org/10.1158/1078-0432.CCR-0609-03
Wu G, Broniscer A, McEachron TA et al (2012) Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nat Genet 44(3):251–253. https://doi.org/10.1038/ng.1102
Xia L, Zheng L, Lee HW et al (2005) Human 3-methyladenine-DNA glycosylase: effect of sequence context on excision, association with PCNA, and stimulation by AP endonuclease. J Mol Biol 346(5):1259–1274. https://doi.org/10.1016/j.jmb.2005.01.014
Xipell E, Aragón T, Martínez-Velez N et al (2016) Endoplasmic reticulum stress-inducing drugs sensitize glioma cells to temozolomide through downregulation of MGMT, MPG, and Rad51. Neuro-Oncology 18(8):1109–1119. https://doi.org/10.1093/neuonc/now022
Yamamori T, Meike S, Nagane M, Yasui H, Inanami O (2013) ER stress suppresses DNA double-strand break repair and sensitizes tumor cells to ionizing radiation by stimulating proteasomal degradation of Rad51. FEBS Lett 587(20):3348–3353. https://doi.org/10.1016/j.febslet.2013.08.030
Acknowledgements
Not applicable.
Funding
This work was supported by the European Union (Marie Curie IRG270459; to M.M. Alonso), the Instituto de Salud Carlos III y los Fondos Feder Europeos (PI13/125; PI16/0066 to M.M. Alonso), the Spanish Ministry of Science and Innovation (Ramón y Cajal contract RYC-2009–05571 and IEDI-2015-00638 to M.M. Alonso), the Department of Health of the Government of Navarra (to M.M. Alonso), the Basque Foundation for Health Research (BIOEF, BIO13/CI/005), Fundación Caja Navarra (Convocatoria de Ayudas 2011 to A. Patiño), Foundation M Torres (JJA, MMA), Foundation LA CAIXA-Caja Navarra (A-PG, MMA), Foundation “El sueño de Vicky”, Asociation Pablo Ugarte-Fuerza Julen (A-PG,MMA), and DOD team science award (MMA, JF, and CG-M). 2018 AACR-AstraZeneca Immuno-oncology Research Fellowship, Grant number 18–40-12-MART (NMV). European Research Council (ERC) under the European Union´s Horizon 2020 research and innovation programme, grant agreement No. 817884; ViroPedTher, (MMA).
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Author information
Authors and Affiliations
Contributions
Conception and design: JJA, LIR, JF, CG-M, AP-G, and MMA. Development of methodology: NM-V, MM, MG-H, MG-M, ST-S, RD-V, and MMA. Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): All authors. Analysis and interpretation of the data (e.g., statistical analysis, biostatistics, and computational analysis): NM-V, JJA, LIR, and MMA. Writing, review, and/or revision of the manuscript: All authors. Administrative, technical, or material support (i.e., reporting or organizing data and constructing databases): NM-V, OB, AP-G, and MMA. Study supervision: AP-G, CM, JF and MMA. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval for animal studies was granted by the Animal Ethical Committee of the University of Navarra (CEEA; Comité Etico de Experimentación Animal under the protocol number CEEA/069–13). All animal studies were performed in the veterinary facilities of the Center for Applied Medical Research in accordance with institutional, regional, and national laws and ethical guidelines for experimental animal care.
Consent for publication
Not applicable.
Competing interests
C. Gomez-Manzano and Juan Fueyo report ownership interest (including patents) in and are consultants for DNATrix. M. M. Alonso has a research grant from DNATrix (not related with this manuscript). The remaining authors do not have potential conflicts of interest to disclose.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Figure S1. Combination of radiotherapy with the oncolytic virus Delta-24-RGD results in a potent oncolytic effect in the DIPG and pHGG cell lines. Figure S2. Delta-24-RGD in combination with radiotherapy shows a synergistic cytotoxic effect in the DIPG and pHGG cell lines in vitro. Figure S3. Delta-24-RGD downregulation of the cellular DNA damage repair machinery in the DIPG and pHGG cell lines. Figure S4. Administration of Delta-24-RGD in combination with radiotherapy heightens the immune infiltration in DIPG murine tumors. Table S1. Evaluation of dose-escalation RT administration to the mice pons. (PDF 1150 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Martinez-Velez, N., Marigil, M., García-Moure, M. et al. Delta-24-RGD combined with radiotherapy exerts a potent antitumor effect in diffuse intrinsic pontine glioma and pediatric high grade glioma models. acta neuropathol commun 7, 64 (2019). https://doi.org/10.1186/s40478-019-0714-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-019-0714-6