Abstract
Background
Parkinson's disease (PD) is the most prevalent neurodegenerative motor disorder. The neuropathology is characterized by intraneuronal protein aggregates of α-synuclein and progressive degeneration of dopaminergic neurons within the substantia nigra. Previous studies have shown that extracellular α-synuclein aggregates can activate microglial cells, induce inflammation and contribute to the neurodegenerative process in PD. However, the signaling pathways involved in α-synuclein-mediated microglia activation are poorly understood. Galectin-3 is a member of a carbohydrate-binding protein family involved in cell activation and inflammation. Therefore, we investigated whether galectin-3 is involved in the microglia activation triggered by α-synuclein.
Results
We cultured microglial (BV2) cells and induced cell activation by addition of exogenous α-synuclein monomers or aggregates to the cell culture medium. This treatment induced a significant increase in the levels of proinflammatory mediators including the inducible Nitric Oxide Synthase (iNOS), interleukin 1 Beta (IL-1β) and Interleukin-12 (IL-12). We then reduced the levels of galectin-3 expression using siRNA or pharmacologically targeting galectin-3 activity using bis-(3-deoxy-3-(3-fluorophenyl-1H-1,2,3-triazol-1-yl)-β-D-galactopyranosyl)-sulfane. Both approaches led to a significant reduction in the observed inflammatory response induced by α-synuclein. We confirmed these findings using primary microglial cells obtained from wild-type and galectin-3 null mutant mice. Finally, we performed injections of α-synuclein in the olfactory bulb of wild type mice and observed that some of the α-synuclein was taken up by activated microglia that were immunopositive for galectin-3.
Conclusions
We show that α-synuclein aggregates induce microglial activation and demonstrate for the first time that galectin-3 plays a significant role in microglia activation induced by α-synuclein. These results suggest that genetic down-regulation or pharmacological inhibition of galectin-3 might constitute a novel therapeutic target in PD and other synucleinopathies.
Similar content being viewed by others
Introduction
Parkinson's disease (PD) is a progressive neurodegenerative disorder clinically typified by bradykinesia, rigidity, postural instability and tremor, as well as a wide range of non-motor symptoms including constipation, bladder dysfunction and cognitive impairment [1]. Pathologically, PD is characterized by the formation of α-synuclein aggregates commonly known as Lewy bodies and Lewy neurites [2], glial activation, brain inflammation and progressive dopaminergic cell degeneration [3]. While the majority of cases of PD appear to be sporadic, genetic mutations or multiplications of the α-synuclein gene (SNCA) lead to the onset of familial PD [4],[5].
α-synuclein is a soluble protein composed of 140 amino acids found predominantly in presynaptic terminals where it is thought to play a role in development and plasticity [6]-[9]. In addition, α-synuclein is highly expressed in immune cells, including T-cells, B-cells, natural killer cells and monocytes [10]. Recent studies suggest that α-synuclein can transfer from one cell to another and promote the self-aggregation and thus possibly contributing to disease propagation [7],[11]-[14].
While microglial activation has been suggested to play major role in the neurodegenerative process in PD [15],[16], the signaling pathways that mediate this process are still poorly understood. For instance, Codolo and colleagues have recently demonstrated that α-synuclein monomers and fibrils induce Interleukin 1β (IL-1β) release from monocytes [17] via the Toll-like receptor 2 (TLR2). Moreover, Kim and colleagues have suggested that oligomeric forms of α-synuclein specifically activate TLR2 [18]. However, the TLR4 has also been implicated in α-synuclein-induced inflammation [19]. Moreover, it has been shown that the effects on cell activation and the subsequent inflammatory response can vary with the source/species of α-synuclein (mammalian cell-derived vs recombinant) and/or the type of protein used (wild type or mutant) [20]. Moreover, the molecular state of the protein used (monomeric, oligomeric or fibrillar) can also play a role in the magnitude of the inflammatory response [18]. Indeed, depending on the microenvironment/insult, activated microglia cells can adopt one of two well-characterized profiles, namely a classical (pro-inflammatory, M1) or an alternative (anti-inflammatory, M2) profile [21],[22]. In these two different states, activated microglia release different factors and express different surface proteins that allow them to sense the microenvironment and coordinate the inflammatory response. In the pro-inflammatory (M1) profile, microglial cells release different pro-inflammatory molecules, e.g. Tumor Necrosis Factor-α (TNF-α), IL-1β, Interleukin-12 (IL-12), Interferon-γ (IFN-γ) or Nitric oxide (NO), which decrease neuronal survival [23],[24]. The alternative profile, however, is characterized by release of anti-inflammatory factors (e.g. Interleukin-4 (IL-4), Interleukin-13 (IL-13) or Transforming Growth factor-β (TGF-β)) which reduce microglial activation [25]. While different pathways have been suggested to be involved in α-synuclein-mediated activation including the ERK 1/2, p38 MAPK, inflammasome or the NF-κβ pathway [17],[26], the involvement of galectin-3 and microglial activation remains to be elucidated. Galectin-3, which is identical to the commonly used macrophage marker Mac-2, is an inflammatory mediator known to be highly expressed in some activated inflammatory cells, including microglia. Galectin-3 levels are increased in several conditions including encephalomyelitis, traumatic brain injury, experimental allergic encephalitis (EAE) and ischemic brain injury [27],[28]. However, a possible role for α-synuclein induced galectin-3 activation during the inflammatory process in PD has yet to be elucidated.
Galectin-3 is a member of the β-galactoside-binding lectin family defined by their typical carbohydrate recognition domains (CRDs) [29],[30]. Galectin-3 plays a role in different biological activities, including cell adhesion, proliferation, clearance, apoptosis, cell activation, cell migration, phagocytosis and inflammatory regulation [27],[31]-[37]. Galectin-3 is found both intra- (in cytoplasm and nucleus) and extracellularly in different cell types and is suggested to play both pro-inflammatory and anti-inflammatory roles which depend on the cell type and insult provided [31],[36],[38],[39]. In this study, we investigated whether galectin-3 is involved in microglial activation induced by α-synuclein proteins. Therefore, we exposed BV2 and primary microglia cells to monomeric and aggregated forms of recombinant α-synuclein and specifically studied the inflammatory response. We then determined the effects of microglial activation following down-regulation of galectin-3 using a specific pharmacological inhibitor or genetic down regulation using siRNA. We then monitored the effects of different forms of α-synuclein on galectin-3-null mice primary microglial cultures. Finally, we determined whether α-synuclein injections into the olfactory bulb of wild type mice result in microglia activation and galectin-3 protein expression.
Materials and methods
Animals
For primary microglial cultures, galectin-3 null mice [40] with a pure C57BL/6 background were obtained from Dr. K. Sävman from Gothenburg University. For intracerebral injections, 3-month-old female mice C57BL/6J were purchased from Charles River Laboratories and housed them under a 12 h light/12 h dark cycle with access to food and water and libitum at Lund university (Sweden). All procedures were carried in accordance with the international guidelines and were approved by the Malmö-Lund Ethical Committee for Animal Research in Sweden (M479-12).
Genotyping
The genotype of gal3-/- and gal3+/+ mice was determined by an integrated extraction and amplification kit (Extract-N-Amp™, Sigma-Aldrich). The PCR consisted of 94°C for 5 min, then 40 cycles with denaturation at 94°C for 45 sec, annealing at 55°C for 30 sec, and elongation at 72°C for 1.5 min. The primers (CyberGene, Solna, Sweden) used were as follows: galectin-3 common 5-CAC GAA CGT CTT TTG CTC TCT GG-3'), gal3-/- 5-GCT TTT CTG GAT TCA TCG ACT GTG G-3' (single band of 384 bp) and gal3+/+ 5-TGA AAT ACT TAC CGA AAA GCT GTC TGC-3' (single band of 300 bp) [41]. We separated the PCR products by gel electrophoresis labeled with ethidium bromide and visualized in a CCD camera (SONY, Tokyo, Japan).
Cell cultures and treatment
We cultured murine microglial cells (BV2 cell line) in Dulbecco's modified Eagle's medium (DMEM) containing 10% Fetal Bovine Serum (Invitrogen) with 100 U/ml Penicillin and 100 U/ml Streptomycin (Invitrogen) in 5% CO2 atmosphere at 37°C in T75 flasks (Nunc, Thermo Scientific) and passaged at confluency. BV2 cells were seeded at a concentration of 2×105 cells/well in 24 wells plate (Nunc, Thermo Scientific) then treated with α-synuclein monomers or aggregates at different concentrations (5, 10 and 20 μM) or LPS (Sigma-Aldrich) at 1 μg/ml. All treatments were conducted for 12 h.
Primary cell cultures
Primary microglia cultures from wild-type (WT) (C57BL/6) or galectin-3 knockout (KO) mice, cells were prepared from postnatal day 1-3 and cultured as previously described [42]. Briefly, the cerebral cortex were dissociated in ice cold Hank's Balance Salt Solution without bivalent ions (HBSS, Invitrogen), Trypsin (0.1%) (Invitrogen) and DNase (0.05%) (Sigma-Aldrich). The cells were then plated in T75 flask with 10 ml/flask of Dulbecco's modified Eagle's medium (DMEM, Invitrogen) containing 10% Fetal Bovine Serum (Invitrogen) with 100 U/ml Penicillin and 100 U/ml Streptomycin (Invitrogen) in 5% CO2 atmosphere at 37°C. After 14 days, cells were harvested in the medium by smacking the flask 10-20 times and plated in 96 wells plates at a density of 2×104 cells/well. The primary cultures were then treated with α-synuclein aggregates at different concentrations (50 nM, 200 nM, 1, 5, and 20 μM).
α-synuclein aggregate generation
Briefly, human α-synuclein was purified using the heat treatment, ion exchange, and gel filtration chromatography as previously described [43]. α-synuclein monomers were placed on an orbital shaker at 250 rpm, shaking the monomers for 5 days at 37°C in sterile PBS. After 5 days of incubation, the protein aggregates were sonicated using a Branson Sonifier 250 (All-Spec, Willington, US) with the following conditions: 3/9 output and 30/100 Duty Cycle. We tested the composition of our aggregates and monomers using Western Blot analysis and transmission electron microscopy (TEM) (FEI, Einhofen Holland). We performed negative stain of monomeric and sonicated aggregated forms of α-synuclein by using 2% uranyl acetate in water. The concentration of endotoxin was measured in our protein preparations using the Limulus amebocyte lysate assay (Chromogenic Endotoxin Quantification Kit, Thermo Scientific, US). We detected very low levels of endotoxin (0.14 ng of LPS/ml) that was unable to influence on the microglial activation (data not shown).
Galectin-inhibitor
We used a small inhibitory molecule for galectin-3 activity, bis-(3-deoxy-3-(3-fluorophenyl-1H-1,2,3-triazol-1-yl)-β-D-galactopyranosyl)-sulfane (Kd = 14 nM) [44]-[46] as pre-treatment 30 minutes (5, 25, 50 and 100 μm) before cells were treated with α-synuclein (monomers or aggregates) or for 12 h along with α-synuclein (monomers or aggregates) at 100 μm.
Transfection conditions
Transfection of BV2 cells was carried out using Lipofectamine 2000 following the manufacturer's recommendation (Life Technologies). Non-targeting control and galectin-3 siRNAs were obtained from Dharmacon. (SMART pool) siRNA sequence used: siLGal3S3(1) J-041097-09 GAGAGAUACCCAUCGCUUU, siLGal3S3(2) J-041097-10 ACUUCAAGGUUGCGGUCAA, siLGal3S3(3) J-041097-11 ACAGUGAAACCCAACGCAA, siLGal3S3(4) J-041097-12 GGAUGAAGAACCUCCGGGA.
Western blot analysis
Briefly, proteins were loaded on 4-20% Mini-Protean TGX Precast Gels (Bio-Rad) then transferred to Nitrocellulose membranes (Bio-Rad) using Trans-Blot Turbo System (Bio-Rad). Membranes were then blocked with 10% Casein (Sigma-Aldrich) diluted in PBS (tablets, Sigma-Aldrich). After blocking, we incubated membranes, with primary antibodies at 4°C over night. We then incubated membranes with peroxidase secondary antibody (Vector Labs) and blots were developed using Clarity Western ECL Substrate (Bio-Rad) and protein levels were normalized to actin.
Antibodies
Antibodies used for this study; anti-rabbit iNOS primary Antibody (1:5000, Santa Cruz), Anti-rat Galectin-3 Antibody (1:3000, M38 clone from Hakon Leffler's lab), Anti-mouse Actin antibody 1:8000 (Sigma-Aldrich), Anti-human Synuclein antibody 1:3000 (Life Technologies).
Cytokines analysis
We measured the cytokine levels from BV2 conditioned medium and primary microglial cells after 12 h treatment. We used the ultrasensitive Th1/Th2 cytokine multiplex plate to measure IFN-γ, IL-1β, IL-2, IL-4, IL-5, IL-8, IL-10, IL-12, IL-6 and TNF-α (Meso Scale Discovery, Rockville, USA) according to the manufacturer's recommendations. The plates were analyzed using with the plate reader SECTOR Imager 6000 (Meso Scale Discovery, Rockville, USA). The conditioned medium was snap frozen on dry ice and kept in -80°C freezer prior analysis.
Viability assay
Cell viability was performed by measuring mitochondrial activity (mitochondrial dehydrogenase) in living cells using XTT (2,3-Bis-(2-methoxy-4-nitro-5-sulfophenyl]-2H-tetrazolium-5-carboxyanilide salt) (Sigma-Aldrich). The assay was performed following manufacturer's protocol on a 96-well plate (Biochrom Asys Expert 96 micro plate reader, Cambridge, UK).
Olfactory bulb recombinant α-synuclein injections
We analyzed brain sections from mice injected into the olfactory bulb with different α-synuclein species (monomeric, oligomeric and fibrillar α-synuclein) as previously described [47]. Briefly, α-synuclein was produced in Escherichia coli and purified and filtered as described previously [47],[48]. Oligomers were obtained by incubating soluble α-synuclein at 4 degrees for 7 days without shaking, in 50 mM Tris hCl, and then separated from monomers by size exclusion chromatography. Fibrils were obtained from incubation of monomers under continuous shaking at 37°C, and samples were assessed by electron microscopy. α-synuclein was then tagged with ATTO-550 as described previously [47]. We injected α-synuclein monomers, oligomer and fibrils (1 mg/mL; 0.8 uL) stereotactically into the olfactory bulb of mice (coordinates AP: +5.4 mm, L: -0.75 mm, DV: -1 mm relative to bregma and dural surface). After injection, 12 h and 72 h, we perfused the mice transcardially with saline solution, followed by 4% paraformaldehyde (PFA) in phosphate buffer. We dissected the brains and post-fixed them for 2 h in PFA 4% followed by saturation in 30% sucrose solution. We then cut brains into 30 μm free-floating coronal sections, as shown previously [47].
Immunofluorescence on mouse brain tissue
We stained free-floating coronal sections of the olfactory bulb from injected mice with primary antibodies: anti-rat Galectin-3 (1:300) and anti-rabbit Iba-1 (1:500, Wako/Nordic labs) with appropriate secondary antibodies Alexa-488 anti-rat, Alexa-647 anti-rabbit (raised in goat, 1:400, Invitrogen). We then analyzed these sections with a confocal laser microscope ZEISS LSM 510 (Switzerland), equipped with Ar and HeNe Lasers.
Phagocytic Assay
We measured the microglial phagocytosis using a phagocytosis assay kit (Cayman Chem, USA) according to the protocol provided by the manufacturer. We plated 5 × 104 cells/well in 96 well plates for 12 h before treating the cells with α-synuclein (20 μm) for additional 12 h. Thereafter, IgG-FITC beads were added with or without galectin-3 inhibitor for 12 h and the phagocytic ability was then analyzed (FluoStar Optima, BMG, LabTech, Sweden).
Statistical analysis
The differences between experimental groups were analyzed (unless otherwise stated) with one-way ANOVA with Tukey's post hoc test, two-way ANOVA Dunnett's post hoc test or t-test as indicated in the figure legends. P < 0.05 was considered as statistically significant. We used the statistical software GraphPad PRISM 6.0 (San Diego, CA, USA). Data is represented as mean ± S.E.M. A minimum of 3 different independent experiments were performed for all the in vitro experiments.
Results
Exogenous α-synuclein proteins promote microglial activation
To assess whether α-synuclein can activate microglial cells in vitro, we first generated recombinant α-synuclein and induced protein aggregates as previously reported [43]. We then characterized the α-synuclein species by Western blot and electron microscopy analysis (Additional file 1: Figure S1A-C). Our data demonstrate that α-synuclein in the aggregated state is composed of a mixture of monomers, oligomers and to a lesser extent, fibrillar α-synuclein species (Additional file 1: Figure S1D). We then assessed the inflammatory response by exposing microglial cells to different concentrations of monomeric or aggregated forms of α-synuclein (5, 10 and 20 μm) for 12 h, the time period at which the temporal iNOS expression response following LPS treatment is the highest [49]. Using these conditions, we identified a concentration-dependent up-regulation of iNOS expression following both monomeric and aggregated forms of α-synuclein (Figure 1A and B, respectively). At the highest concentration used however (20 μm), α-synuclein aggregates induced a 3-fold higher iNOS expression compared to monomeric α-synuclein (Figure 1A and B). These results indicate that our α-synuclein proteins successfully induce microglial activation [17].
Microglial activation by α-synuclein and inhibition by galectin-3 inhibitor. We measured iNOS expression by western blot in microglial cells after 12 h incubation with α-synuclein monomers (A) and α-synuclein aggregates (B) using different concentrations, 5 μm, 10 μm and 20 μm. iNOS was significantly up regulated with both protein preparations of α-synuclein. α-synuclein aggregates (B) induced a 3-fold higher activation compared to monomers (A). To determine the role of galectin-3 we used a pre-treatment, incubating the galectin-3 inhibitor for 30 min and then we incubated for 12 h the cells with α-synuclein, monomers or aggregates, using the highest concentration, 20 μm. The lower iNOS expression induced by α-synuclein monomers was not significantly inhibited by pharmacological inhibition of galectin-3 (C). iNOS expression induced by α-synuclein aggregates (D) was inhibited by more than 50% using 100 μm of the inhibitor. We use the highest iNOS response in each experiment as an internal control to evaluate the response to the other concentrations. Western blot analysis displays iNOS and β-actin protein levels. One-way ANOVA, *P < 0.05, **P < 0.01, n = 3, mean ± S.E.M.
Pro-inflammatory cytokine levels increase after α-synuclein treatment
Following α-synuclein treatment, we observed a concentration dependent up-regulation of cytokine secretion that includes TNF-α, IL-2 and IL-12 (Figure 2A-C). These results suggest that microglial activation induced by α-synuclein aggregates promote a pro-inflammatory cascade similar to that observed in PD [24],[50].
Increased cytokine levels in BV2 microglia culture medium after α-synuclein activation. Cytokine levels in BV2 microglia culture medium after 12 h incubation with α-synuclein aggregates at concentrations of 5, 10 and 20 μm. α-synuclein aggregates induced a significant increase in cytokine levels of the proinflammatory cytokines TNF-α (A), IL-12 (B) and IL-2 (C). One-way ANOVA, *P < 0.05, **P < 0.01, n = 3, mean ± S.E.M.
Inhibition of galectin-3 prevents iNOS expression and reduce pro-inflammatory cytokines release in BV2 microglial cells
First, we assessed the effect of pharmacological inhibition of galectin-3 prior to α-synuclein-induced microglial activation. To this end, microglial cells were pre-treated with a galectin-3 inhibitor for 30 minutes (5, 25, 50 and 100 μm) then washed and exposed to monomeric or α-synuclein aggregates (20 μm) then we assessed the levels of iNOS expression. After pharmacological inhibition of galectin-3, we observed a significant inhibition of α-synuclein-induced microglial activation (as shown by the lack of iNOS expression) in a concentration-dependent manner with more than 50% iNOS down-regulation following 50 and 100 μm treatment, a result that was specific to α-synuclein aggregates (Figure 1C and D). Next, we assessed the effect of pharmacological inhibition of galectin-3 for 12 h along with the α-synuclein aggregates. Pharmacological inhibition of galectin-3 for 12 h resulted in a higher inhibition (85%) of α-synuclein-induced microglial activation (iNOS expression, Figure 3A). We then measured the cytokine levels in the medium after galectin-3 inhibition and α-synuclein treatment for 12 h and observe a clear reduction in the pro-inflammatory cytokines IL-12, IL-6 and TNF-α (Figure 3B).
Inhibition of microglial activation by galectin-3 inhibitor. To determine the role of galectin-3 we used a treatment, incubating the galectin-3 inhibitor along with α-synuclein aggregates for 12 h at 20 μm. We determine by western blot the iNOS expression induced by α-synuclein aggregates. iNOS expression was inhibited by more than 80% using 100 μm of the inhibitor (A). The cytokines levels were measure and TNF-α, IL-12 and IL-6 were down regulated when using the inhibitor for 12 along with α-synuclein aggregates (B). We use the highest iNOS response in each experiment as an internal control to evaluate the response to the other concentrations. Western blot analysis displays iNOS and β-actin protein levels. One-way ANOVA, *P < 0,05, **P < 0.01,****P < 0,0001) n = 3, mean ± S.E.M.
Galectin-inhibition does not impair cell viability
As shown in figure S2, inhibition of galectin-3 does not affect cell viability when cells are treated alone or in combination with α-synuclein aggregates for 12 h. Interestingly, α-synuclein treatment of microglial cells increased mitochondrial activity with or without the inhibitor, suggesting an increased metabolic need that may be triggered by α-synuclein aggregates.
Galectin-3 knockdown in BV2 microglial cells down-regulates iNOS expression and pro-inflammatory cytokine release
To further test the role of galectin-3 in microglial activation, we genetically down-regulated galectin-3 expression in BV2 cells using small interfering RNA (siRNA) (Figure 4A). We then treated the cells with α-synuclein aggregates and analyzed the iNOS expression levels using Western blot analysis (Figure 3B). As expected, down-regulation of galectin-3 significantly reduced iNOS protein expression levels (Figure 4B). Next, we measured the cytokine levels in BV2 cells genetically down regulated with small interfering RNA (siRNA) targeting galectin-3 and treated with α-synuclein aggregates. Genetic down-regulation of galactin-3 also showed a reduction in TNF-α and IL-10 compared to cells treated with control siRNA (Figure 4C). Taken together these results demonstrate that down-regulation of galectin-3 reduces α-synuclein induced microglial activation and significantly lowers iNOS protein expression and cytokine up-regulation.
Galectin-3 siRNA reduces microglial activation induced by α-synuclein aggregates. BV2 microglia activated by 20 μm of α-synuclein aggregates for 12 h show a robust iNOS down regulation by 80% when galectin-3 is knocked down by siRNA (B). Knock down efficiency of galectin-3 siRNA (A). The cytokines levels from BV2 cells treated medium was measured after 12 h incubation with α-synuclein aggregates and we found significant reduction in TNF-α and IL-10 (C). Western blot analysis showing iNOS and β-actin protein levels. t-test, One-Way ANOVA. *P < 0.05, **P < 0,01 n = 3, mean ± S.E.M.
Pharmacological intervention of galectin-reduces the microglial phagocytic activity
To test the implications on the phagocytic ability of microglial cells in our α-synuclein activation model, we treated BV2 cells with the galectin-3 inhibitor for either 30 minutes or 12h together with α-synuclein aggregates. As expected, activated microglial cells show a higher phagocytic activity whereas no differences were observed in the phagocytic ability using the inhibitor as a pre-treatment (data not shown). As shown in Figure 5, the phagocytic ability of microglia was reduced to control levels during the experiment when cells are treated with the inhibitor for 12 h. As expected, treating the cells with recombinant galectin-3 proteins up-regulates microglial phagocytic activity to levels similar to cells treated with α-synuclein aggregates (Figure 5). Importantly, we did not detect any synergic effect when cells were treated with galectin-3 and α-synuclein aggregates. These results suggest that induction of phagocytosis is an important aspect of microglial activation by α-synuclein aggregates and that galectin-3 plays an important role in cell activation and phagocytosis. These results are in in line with previous studies showing that phagocytosis is a central part in α-synuclein induced inflammation [17].
BV2 microglial cells treated with the galectin-3 inhibitor show reduced phagocytic ability. Phagocytic ability of microglia was robustly increased after 12 h of treatment with α-synuclein aggregates (20 μm). Adding galectin-3 inhibitor (100 μm) to microglial cultures treated with α-synuclein aggregates for the same 12 h time period robustly reduced the phagocytosis down to baseline levels. Adding galectin-3 protein we could recover the phagocytic ability even when using the inhibitor at the same time. Phagocytosis was measured by the cellular uptake up of fluorescent beads. One-way ANOVA, *P < 0.05; **P < 0.01, n = 3, mean ± S.E.M.
Microglia from galectin-knockout mice display iNOS down-regulation following α-synuclein activation
Next we examined the iNOS levels in primary microglial cells, we analyzed the conditioned medium after cells been treated with α-synuclein aggregates for 12h. In line with our BV2 iNOS cytokine data (Figure 1), we identified a robust up-regulation iNOS following α-synuclein challenge (Figure 6A). Importantly, galectin-3 knockout microglial cells showed a complete abrogation of iNOS protein expression (Figure 6B). This data clearly demonstrated that iNOS regulation maybe dependent on galectin-3.
Abrogation of iNOS proteins level and pro-inflammatory cytokines reduction in primary microglial cells from galectin-3 knockout mice after activation with α-synuclein. Primary microglial culture from wild-type mice shows robust iNOS expression following exposure of 20 μm α-synuclein aggregates, or LPS (100 ng/ml), for 12 h (A). Lower concentrations of α-synuclein aggregates, 5 μm and below, failed to induce iNOS expression in wild- type microglia (A). Primary microglia from galectin-3 knockout mice completely lack iNOS up regulation following exposure of 20 μm α-synuclein aggregates for 12 h (B). Cytokine levels in culture medium from primary microglial cells were measured after 12 h incubation with α-synuclein aggregates. Treatment of wild-type microglia with 5 and 20 μm α-synuclein aggregates for 12 h induced increased levels of IL-1β, IL-12, IFN-γ and IL-4 (C). Treatment of galectin-3 knockout microglia for 12 h reduced levels of IL-1β IL-12 using 20 μm α-synuclein aggregates. Cytokine levels of IFN-γ and IL-4 did not change in galectin-3 knockout compared to wild-type microglia. Two-way ANOVA, *P < 0.05, **P < 0.01, n = 5, mean ± S.E.M.
Microglia from galectin-knockout mice show a down-regulation of pro-inflammatory cytokines following α-synuclein activation
To examine the cytokine levels in primary microglial cells, we analyzed the conditioned medium after cells were treated with α-synuclein aggregates. In line with our BV2 cytokine data (Figure 2), we identified a robust up-regulation of pro-inflammatory cytokines that included IL-12 and IL-1β and IFN-γ as well as the anti-inflammatory cytokine IL-4 (Figure 6C). Importantly, galectin-3 KO microglial cells showed a significant reduction in IL-1β (55%) and IL-12 (75%) cytokine release when compared to wild type microglia (Figure 6C). However, no differences were observed in IFN-γ or the anti-inflammatory cytokine IL-4. Taken together, our results indicate that galectin-3 is involved in the pro-inflammatory activation of specific inflammatory pathways that involve the IL-1β and IL-12 cytokines.
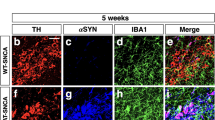
Olfactory bulb injections of recombinant α-synuclein
To confirm the expression of galectin-3 in microglial cells following activation with α-synuclein in vivo, we injected α-synuclein tagged with ATTO-550 in a monomeric, oligomeric or fibrillar state within the olfactory bulb of wild type mice. We then performed immunofluorescence analysis and identified activated microglial cells (Iba-1) that were positive for galectin-3 following α-synuclein injections (Figure 7). While microglial cells were able to take up all three different forms of α-synuclein injected, differences in the molecular species taken up by microglia cells were shown to vary with time. Indeed, at 12 h post injection, we identified activated microglial cells containing monomers and oligomers with up-regulated galectin-3 expression (Figure 7A). In contrast, limited galectin-3 expression was observed upon fibrillar α-synuclein (Figure 7A). These results may be due to the limited uptake of the fibrillar forms of α-synuclein [47], or the time required to phagocyte the fibrillar α-synuclein species. Interestingly, at 72 h post injection, monomeric α-synuclein did not induce galectin-3 expression, whereas oligomers and fibrils showed a clear galectin-3 up-regulation (Figure 7B). Taken together, our data demonstrate that microglial cells take up α-synuclein in vivo and display a microglia phenotype that is galectin-3 positive.
Intracerebral injection of α-synuclein is taken up by microglia and induces galectin-3 expression. Injections of fluorescent labeled α-synuclein (tagged with ATTO-550) into the olfactory bulbs were performed to study if α-synuclein can be taken up by microglia and induce microglial activation with galectin-3 expression. α-synuclein in the form of monomers, oligomers and fibrils were injected. Sections were stained for galectin-3 and Iba-1 (microglial markers). At 12 h post-injection, monomers and oligomers of α-synuclein were taken up by microglia and showed low expression of galectin-3 (A). No microglia with galectin-3 expression was detected at 12 h after injection of fibrils. At 72 h post-injection, galectin-3 expression was clearly detected after injection of oligomers and fibrils, but had disappeared for monomers (B) (n = 3).
Discussion
We demonstrate for the first time that galectin-3; a carbohydrate-binding protein is an immune modulator that plays an important role in the α-synuclein-induced activation of microglia. We identified a profound inflammatory inhibition of microglia cells by genetic down-regulation or pharmacological inhibition of galectin-3 or by using galectin-3 knockout primary microglia following activation by α-synuclein aggregates. In agreement with these results, prior work suggests that α-synuclein oligomers are neurotoxic and induce a strong inflammatory response in microglia cells, exceeding that seen after exposure to α-synuclein monomers [18]. Interestingly, Tokuda and colleagues have identified elevated levels of α-synuclein oligomers and an increased oligomers/total-α-synuclein ratio in the cerebrospinal fluid in PD patients, suggesting that α-synuclein oligomers may contribute to the progression of PD [51].
Recent discoveries have also demonstrated that α-synuclein can transfer from one cell to another and seed endogenous protein aggregation within the recipient cell in a prion-like fashion [13]. Besides spreading from neuron to neuron, α-synuclein can also spread from neurons to glial cells as shown previously in vitro and in vivo[52]. Due to the presence of α-synuclein in the extracellular milieu, several novel treatment strategies focusing on reducing the α-synuclein levels have been proposed including immunotherapy [53],[54], delivery of α-synuclein degrading enzymes [55] or altering microglial activity [56]. Indeed, microglial activation has been linked to several neurodegenerative disorders [57] and therefore, a pharmacological intervention on the inflammatory response exerted by microglia may be a promising therapeutic target. In attempts to reduce microglial activity, several different inflammatory pathways have been targeted in earlier studies. For example peroxiredoxin 2, which inhibits the mitogen-activated protein kinase and the transcription factor nuclear factor-κB (NF-kB), have shown to be effective [58]. Additionally, minocycline, one of the most used inhibitors for microglia activation has also been suggested to specifically inhibit the M1 phenotype [59]. Moreover, inhibition of NADPH oxidase 2 (Nox2) has also been shown to reduce microglial activation in α-synuclein-induced inflammation model [60].
In this study, we used a small molecule inhibitor targeting galectin-3 and found that it inhibited microglial activation following challenge with aggregated α-synuclein. Galectin-3 inhibitor has been successfully tested in other pathological conditions with evidence for a rate-limiting role of galectin-3 [46]. For example, in a mouse model of hepatitis, the galectin-3 inhibitor attenuated liver damage and proinflammatory T cell-mediated cytokine release (IFN-γ- and IL-17- and IL-4 producing CD4+ T cells). The same inhibitor also increased the number of T cells producing the anti-inflammatory IL-10 while promoting activation of M2 phenotype in macrophages [45]. Recently, the inhibitor was shown to support the survival of pancreatic beta cells in an apoptotic model induced by proinflammatory cytokines TNF-α + IFN-γ + IL-1β [44]. In our current model system, we observed an up-regulation of both pro and anti-inflammatory cytokines released from primary and BV2 microglial cells. After analysis, we detected a significant up regulation of pro-inflammatory cytokines TNF-α, IL-2 and IL-12. Using either, the galectin-3 inhibitor for 12 h or genetic down-regulation using siRNA we found a significant down-regulation in different pro-inflammatory molecules that include iNOS and TNF-α, molecules involved in the nuclear factor-kappa Beta (NF-κβ) pathway [61]. Using primary microglial cells derived from galectin-3 knockout mice, we identified a significant reduction in IL-12 and IL-1β release compared to wild type microglia. Interestingly, the absence of galectin-3 did not significantly affect the levels of IFN-γ or cytokines related to alternative activation pathway (e.g. IL-4) suggesting that, in response to α-synuclein, galectin-3 plays a specific inflammatory role in microglial activation. Such selective role for galectin-3 is noteworthy as galectin-3 regulates traffic of specific membrane glycoproteins (e.g. receptors) [62]. While the regulatory roles of galectins vary between different cell types, this variation is likely due to the galectin type and/or the type of glycans expressed in a particular cell [63]. Our findings support the notion that the inflammatory modulation exerted by galectin-3 is related to specific inflammatory pathways.
We have identified a robust reduction of IL-12 cytokine level in the primary galectin-3 KO microglia when compared to wild type microglial cells. The IL-12 production is regulated through multiple pathways that include: NF-κβ, p38 mitogen-activated protein (MAP) kinase, cyclic adenosine monophosphate (cyclic AMP)-modulating molecules and nitric oxide (NO) [64]. In line with our findings, several studies have shown a relationship between iNOS inhibition and a down-regulation of IL-12 expression [65]. Our results demonstrate a profound iNOS expression and a pro-inflammatory cytokines reduction upon galectin-3 knockdown, gene deletion or pharmacological inhibition, suggesting that the NF-κβ pathway may indeed be the effector pathway for galectin-3. Moreover, the inflammasome, which generates mature IL-1β by activating caspase-1, has also been shown to be associated with microglial activation [66]-[69]. Indeed, recent findings suggest that this inflammatory signaling pathway is activated by the phagocytosis of α-synuclein [17],[70]. For instance, Freeman and colleagues described a specific interaction between galectin-3 and the phagosomes/lysosomes containing α-synuclein [70]. We observed a remarkable 80% inhibition of α-synuclein-induced phagocytosis by pharmacological inhibition of galectin-3. This suggests that galectin-3 regulates α-synuclein-induced activation of microglia. On the other hand, increased phagocytosis of α-synuclein by microglia within the substantia nigra could potentially reduce the load of toxic α-synuclein species [71].
Indeed, we found galectin-3 immunoreactive microglia 12 h following injection of monomeric or oligomeric α-synuclein proteins. However, we did not detected galectin-3 immunoreactive cells after fibril injections at the same time points suggesting different up-take dynamics or intracellular processing [47]. At later time point however, α-synuclein fibrils and oligomers induced a robust galectin-3 immunoreactivity whereas monomers failed to induce a similar response indicating that monomers may be processed intracellular within 72 h without galectin-3 activation.
Conclusions
We have demonstrated that galectin-3 is an important molecule that contributes to full-blown microglial activity upon exposure to α-synuclein aggregates. Genetic ablation, down-regulating galectin-3, or pharmacologically inhibition of galectin-3, resulted in a profound down-regulation of microglial activation (i.e. reduced levels of iNOS, TNF-α, IL-12, IL-1β and the phagocytic ability of microglia). Following injections of α-synuclein species in the olfactory bulb, we observe an up-regulation of galectin-3 in microglial cells that had taken up the injected α-synuclein, providing further support for the importance of galectin-3 in vivo.
Additional files
Abbreviations
- PD:
-
Parkinson disease
- KO:
-
Knockout
- WT:
-
Wild-type
- iNOS:
-
Inducible nitric oxide synthase
- TLR:
-
Toll like receptor
- IFN-γ:
-
Interferon gamma
- TNF-α:
-
Tumor necrosis factor alpha
- IL:
-
Interleukin
- MAPK:
-
Mitogen-activated protein kinases
- ERK:
-
Extracellular signal-regulated kinases
- NF-κβ:
-
Nuclear factor kappa-light-chain-enhancer of activated B cells
References
Chaudhuri KR, Schapira AH: Non-motor symptoms of Parkinson's disease: dopaminergic pathophysiology and treatment. Lancet Neurol 2009, 8: 464–474. 10.1016/S1474-4422(09)70068-7
Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M: Alpha-synuclein in Lewy bodies. Nature 1997, 388: 839–840. 10.1038/42166
Qiao S, Luo JH, Jin JH: Role of microglial activation induced by alpha-synuclein in pathogenesis of Parkinson's disease. Zhejiang Da Xue Xue Bao Yi Xue Ban 2012, 41: 210–214.
Ross OA, Braithwaite AT, Skipper LM, Kachergus J, Hulihan MM, Middleton FA, Nishioka K, Fuchs J, Gasser T, Maraganore DM, Adler CH, Larvor L, Chartier-Harlin MC, Nilsson C, Langston JW, Gwinn K, Hattori N, Farrer MJ: Genomic investigation of alpha-synuclein multiplication and parkinsonism. Ann Neurol 2008, 63: 743–750. 10.1002/ana.21380
Kruger R, Kuhn W, Muller T, Woitalla D, Graeber M, Kosel S, Przuntek H, Epplen JT, Schols L, Riess O: Ala30Pro mutation in the gene encoding alpha-synuclein in Parkinson's disease. Nat Genet 1998, 18: 106–108. 10.1038/ng0298-106
George JM, Jin H, Woods WS, Clayton DF: Characterization of a novel protein regulated during the critical period for song learning in the zebra finch. Neuron 1995, 15: 361–372. 10.1016/0896-6273(95)90040-3
Stefanis L: alpha-Synuclein in Parkinson's disease. Cold Spring Harbor Perspect Med 2012, 2: a009399. 10.1101/cshperspect.a009399
Kholodilov NG, Neystat M, Oo TF, Lo SE, Larsen KE, Sulzer D, Burke RE: Increased expression of rat synuclein in the substantia nigra pars compacta identified by mRNA differential display in a model of developmental target injury. J Neurochem 1999, 73: 2586–2599. 10.1046/j.1471-4159.1999.0732586.x
Bendor JT, Logan TP, Edwards RH: The function of alpha-synuclein. Neuron 2013, 79: 1044–1066. 10.1016/j.neuron.2013.09.004
Shin EC, Cho SE, Lee DK, Hur MW, Paik SR, Park JH, Kim J: Expression patterns of alpha-synuclein in human hematopoietic cells and in Drosophila at different developmental stages. Mol Cells 2000, 10: 65–70. 10.1007/s10059-000-0065-x
Lee HJ, Bae EJ, Lee SJ: Extracellular alpha-synuclein-a novel and crucial factor in Lewy body diseases. Nat Rev Neurol 2014, 10: 92–98. 10.1038/nrneurol.2013.275
George S, Rey NL, Reichenbach N, Steiner JA, Brundin P: alpha-Synuclein: the long distance runner. Brain Pathol 2013, 23: 350–357. 10.1111/bpa.12046
Olanow CW, Brundin P: Parkinson's disease and alpha synuclein: is Parkinson's disease a prion-like disorder? Mov Disord 2013, 28: 31–40. 10.1002/mds.25373
Dunning CJ, George S, Brundin P: What's to like about the prion-like hypothesis for the spreading of aggregated alpha-synuclein in Parkinson disease? Prion 2013, 7: 92–97. 10.4161/pri.23806
Villar-Cheda B, Dominguez-Meijide A, Joglar B, Rodriguez-Perez AI, Guerra MJ, Labandeira-Garcia JL: Involvement of microglial RhoA/Rho-kinase pathway activation in the dopaminergic neuron death. Role of angiotensin via angiotensin type 1 receptors. Neurobiol Dis 2012, 47: 268–279. 10.1016/j.nbd.2012.04.010
Tomas-Camardiel M, Rite I, Herrera AJ, de Pablos RM, Cano J, Machado A, Venero JL: Minocycline reduces the lipopolysaccharide-induced inflammatory reaction, peroxynitrite-mediated nitration of proteins, disruption of the blood-brain barrier, and damage in the nigral dopaminergic system. Neurobiol Dis 2004, 16: 190–201. 10.1016/j.nbd.2004.01.010
Codolo G, Plotegher N, Pozzobon T, Brucale M, Tessari I, Bubacco L, de Bernard M: Triggering of inflammasome by aggregated alpha-synuclein, an inflammatory response in synucleinopathies. PLoS One 2013, 8: e55375. 10.1371/journal.pone.0055375
Kim C, Ho DH, Suk JE, You S, Michael S, Kang J, Joong Lee S, Masliah E, Hwang D, Lee HJ, Lee SJ: Neuron-released oligomeric alpha-synuclein is an endogenous agonist of TLR2 for paracrine activation of microglia. Nat Commun 2013, 4: 1562. 10.1038/ncomms2534
Fellner L, Irschick R, Schanda K, Reindl M, Klimaschewski L, Poewe W, Wenning GK, Stefanova N: Toll-like receptor 4 is required for alpha-synuclein dependent activation of microglia and astroglia. Glia 2013, 61: 349–360. 10.1002/glia.22437
Rojanathammanee L, Murphy EJ, Combs CK: Expression of mutant alpha-synuclein modulates microglial phenotype in vitro. J Neuroinflammation 2011, 8: 44. 10.1186/1742-2094-8-44
Gordon S, Pluddemann A: Tissue macrophage heterogeneity: issues and prospects. Semin Immunopathol 2013, 35: 533–540. 10.1007/s00281-013-0386-4
Roodveldt C, Labrador-Garrido A, Gonzalez-Rey E, Lachaud CC, Guilliams T, Fernandez-Montesinos R, Benitez-Rondan A, Robledo G, Hmadcha A, Delgado M, Pozo D: Preconditioning of microglia by alpha-synuclein strongly affects the response induced by toll-like receptor (TLR) stimulation. PloS one 2013, 8: e79160. 10.1371/journal.pone.0079160
De Pablos RM, Herrera AJ, Villaran RF, Cano J, Machado A: Dopamine-dependent neurotoxicity of lipopolysaccharide in substantia nigra. FASEB J 2005, 19: 407–409.
Zindler E, Zipp F: Neuronal injury in chronic CNS inflammation. Best Pract Res Clin Anaesthesiol 2010, 24: 551–562. 10.1016/j.bpa.2010.11.001
Stirling DP, Cummins K, Mishra M, Teo W, Yong VW, Stys P: Toll-like receptor 2-mediated alternative activation of microglia is protective after spinal cord injury. Brain 2013, 137: 707–723. 10.1093/brain/awt341
Venero JL, Burguillos MA, Brundin P, Joseph B: The executioners sing a new song: killer caspases activate microglia. Cell Death Differ 2011, 18: 1679–1691. 10.1038/cdd.2011.107
Jiang HR, Al Rasebi Z, Mensah-Brown E, Shahin A, Xu D, Goodyear CS, Fukada SY, Liu FT, Liew FY, Lukic ML: Galectin-3 deficiency reduces the severity of experimental autoimmune encephalomyelitis. J Immunol 2009, 182: 1167–1173. 10.4049/jimmunol.182.2.1167
Pajoohesh-Ganji A, Knoblach SM, Faden AI, Byrnes KR: Characterization of inflammatory gene expression and galectin-3 function after spinal cord injury in mice. Brain Res 2012, 1475: 96–105. 10.1016/j.brainres.2012.07.058
Seetharaman J, Kanigsberg A, Slaaby R, Leffler H, Barondes SH, Rini JM: X-ray crystal structure of the human galectin-3 carbohydrate recognition domain at 2.1-A resolution. J Biol Chem 1998, 273: 13047–13052. 10.1074/jbc.273.21.13047
Leffler H, Carlsson S, Hedlund M, Qian Y, Poirier F: Introduction to galectins. Glycoconj J 2004, 19: 433–440. 10.1023/B:GLYC.0000014072.34840.04
Shin T: The pleiotropic effects of galectin-3 in neuroinflammation: a review. Acta Histochem 2013, 115: 407–411. 10.1016/j.acthis.2012.11.010
Jeon SB, Yoon HJ, Chang CY, Koh HS, Jeon SH, Park EJ: Galectin-3 exerts cytokine-like regulatory actions through the JAK-STAT pathway. J Immunol 2010, 185: 7037–7046. 10.4049/jimmunol.1000154
Karlsson A, Christenson K, Matlak M, Bjorstad A, Brown KL, Telemo E, Salomonsson E, Leffler H, Bylund J: Galectin-3 functions as an opsonin and enhances the macrophage clearance of apoptotic neutrophils. Glycobiology 2009, 19: 16–20. 10.1093/glycob/cwn104
Lalancette-Hebert M, Swarup V, Beaulieu JM, Bohacek I, Abdelhamid E, Weng YC, Sato S, Kriz J: Galectin-3 is required for resident microglia activation and proliferation in response to ischemic injury. J Neurosci 2012, 32: 10383–10395. 10.1523/JNEUROSCI.1498-12.2012
Lepur A, Carlsson MC, Novak R, Dumic J, Nilsson UJ, Leffler H: Galectin-3 endocytosis by carbohydrate independent and dependent pathways in different macrophage like cell types. Biochim Biophys Acta 1820, 2012: 804–818.
Liu FT, Rabinovich GA: Galectins: regulators of acute and chronic inflammation. Ann N Y Acad Sci 2010, 1183: 158–182. 10.1111/j.1749-6632.2009.05131.x
Sano H, Hsu DK, Apgar JR, Yu L, Sharma BB, Kuwabara I, Izui S, Liu FT: Critical role of galectin-3 in phagocytosis by macrophages. J Clin Invest 2003, 112: 389–397. 10.1172/JCI200317592
Lee HJ, Suk JE, Bae EJ, Lee SJ: Clearance and deposition of extracellular alpha-synuclein aggregates in microglia. Biochem Biophys Res Commun 2008, 372: 423–428. 10.1016/j.bbrc.2008.05.045
Yang RY, Hsu DK, Liu FT: Expression of galectin-3 modulates T-cell growth and apoptosis. Proc Natl Acad Sci U S A 1996, 93: 6737–6742. 10.1073/pnas.93.13.6737
Colnot C, Ripoche MA, Milon G, Montagutelli X, Crocker PR, Poirier F: Maintenance of granulocyte numbers during acute peritonitis is defective in galectin-3-null mutant mice. Immunology 1998, 94: 290–296. 10.1046/j.1365-2567.1998.00517.x
Doverhag C, Hedtjarn M, Poirier F, Mallard C, Hagberg H, Karlsson A, Savman K: Galectin-3 contributes to neonatal hypoxic-ischemic brain injury. Neurobiol Dis 2010, 38: 36–46. 10.1016/j.nbd.2009.12.024
Deierborg T: Preparation of primary microglia cultures from postnatal mouse and rat brains. Methods Mol Biol 2013, 1041: 25–31. 10.1007/978-1-62703-520-0_4
Grey M, Linse S, Nilsson H, Brundin P, Sparr E: Membrane interaction of alpha-synuclein in different aggregation states. J Parkinsons Dis 2011, 1: 359–371.
Saksida T, Nikolic I, Vujicic M, Nilsson UJ, Leffler H, Lukic ML, Stojanovic I, Stosic-Grujicic S: Galectin-3 deficiency protects pancreatic islet cells from cytokine-triggered apoptosis in vitro. J Cell Physiol 2013, 228: 1568–1576. 10.1002/jcp.24318
Volarevic V, Milovanovic M, Ljujic B, Pejnovic N, Arsenijevic N, Nilsson U, Leffler H, Lukic ML: Galectin-3 deficiency prevents concanavalin A-induced hepatitis in mice. Hepatology 2012, 55: 1954–1964. 10.1002/hep.25542
Mackinnon AC, Gibbons MA, Farnworth SL, Leffler H, Nilsson UJ, Delaine T, Simpson AJ, Forbes SJ, Hirani N, Gauldie J, Sethi T: Regulation of transforming growth factor-beta1-driven lung fibrosis by galectin-3. Am J Respir Crit Care Med 2012, 185: 537–546. 10.1164/rccm.201106-0965OC
Rey NL, Petit GH, Bousset L, Melki R, Brundin P: Transfer of human alpha-synuclein from the olfactory bulb to interconnected brain regions in mice. Acta Neuropathol 2013, 126: 555–573. 10.1007/s00401-013-1160-3
Ghee M, Melki R, Michot N, Mallet J: PA700, the regulatory complex of the 26S proteasome, interferes with alpha-synuclein assembly. FEBS J 2005, 272: 4023–4033. 10.1111/j.1742-4658.2005.04776.x
Henn A, Lund S, Hedtjarn M, Schrattenholz A, Porzgen P, Leist M: The suitability of BV2 cells as alternative model system for primary microglia cultures or for animal experiments examining brain inflammation. Altex 2009, 26: 83–94.
Blandini F: Neural and immune mechanisms in the pathogenesis of Parkinson's disease. J Neuroimmune Pharmacol 2013, 8: 189–201. 10.1007/s11481-013-9435-y
Tokuda T, Qureshi MM, Ardah MT, Varghese S, Shehab SA, Kasai T, Ishigami N, Tamaoka A, Nakagawa M, El-Agnaf OM: Detection of elevated levels of alpha-synuclein oligomers in CSF from patients with Parkinson disease. Neurology 2010, 75: 1766–1772. 10.1212/WNL.0b013e3181fd613b
Reyes JF, Rey NL, Bousset L, Melki R, Brundin P, Angot E: Alpha-synuclein transfers from neurons to oligodendrocytes. Glia 2014, 62: 387–398. 10.1002/glia.22611
Bae EJ, Lee HJ, Rockenstein E, Ho DH, Park EB, Yang NY, Desplats P, Masliah E, Lee SJ: Antibody-aided clearance of extracellular alpha-synuclein prevents cell-to-cell aggregate transmission. J Neurosci 2012, 32: 13454–13469. 10.1523/JNEUROSCI.1292-12.2012
Roodveldt C, Labrador-Garrido A, Gonzalez-Rey E, Fernandez-Montesinos R, Caro M, Lachaud CC, Waudby CA, Delgado M, Dobson CM, Pozo D: Glial innate immunity generated by non-aggregated alpha-synuclein in mouse: differences between wild-type and Parkinson's disease-linked mutants. PloS one 2010, 5: e13481. 10.1371/journal.pone.0013481
Spencer B, Michael S, Shen J, Kosberg K, Rockenstein E, Patrick C, Adame A, Masliah E: Lentivirus mediated delivery of neurosin promotes clearance of wild-type alpha-synuclein and reduces the pathology in an alpha-synuclein model of LBD. Mol Ther 2013, 21: 31–41. 10.1038/mt.2012.66
Sanchez-Guajardo V, Barnum CJ, Tansey MG, Romero-Ramos M: Neuroimmunological processes in Parkinson's disease and their relation to alpha-synuclein: microglia as the referee between neuronal processes and peripheral immunity. ASN Neuro 2013, 5: 113–139. 10.1042/AN20120066
Schwartz M, Kipnis J, Rivest S, Prat A: How do immune cells support and shape the brain in health, disease, and aging? J Neurosci 2013, 33: 17587–17596. 10.1523/JNEUROSCI.3241-13.2013
Suk K, Ock J: Chemical genetics of neuroinflammation: natural and synthetic compounds as microglial inhibitors. Inflammopharmacology 2012, 20: 151–158. 10.1007/s10787-011-0108-2
Kobayashi K, Imagama S, Ohgomori T, Hirano K, Uchimura K, Sakamoto K, Hirakawa A, Takeuchi H, Suzumura A, Ishiguro N, Kadomatsu K: Minocycline selectively inhibits M1 polarization of microglia. Cell Death Dis 2013, 4: e525. 10.1038/cddis.2013.54
Surace MJ, Block ML: Targeting microglia-mediated neurotoxicity: the potential of NOX2 inhibitors. Cell Mol Life Sci 2012, 69: 2409–2427. 10.1007/s00018-012-1015-4
Vafeiadou K, Vauzour D, Spencer JP: Neuroinflammation and its modulation by flavonoids. Endocr Metab Immune Disord Drug Targets 2007, 7: 211–224. 10.2174/187153007781662521
Delacour D, Koch A, Jacob R: The role of galectins in protein trafficking. Traffic 2009, 10: 1405–1413. 10.1111/j.1600-0854.2009.00960.x
Carlsson S, Carlsson MC, Leffler H: Intracellular sorting of galectin-8 based on carbohydrate fine specificity. Glycobiology 2007, 17: 906–912. 10.1093/glycob/cwm059
Kang BY, Kim E, Kim TS: Regulatory mechanisms and their therapeutic implications of interleukin-12 production in immune cells. Cell Signal 2005, 17: 665–673. 10.1016/j.cellsig.2004.12.010
Rothe H, Hartmann B, Geerlings P, Kolb H: Interleukin-12 gene-expression of macrophages is regulated by nitric oxide. Biochem Biophys Res Commun 1996, 224: 159–163. 10.1006/bbrc.1996.1000
Latz E, Xiao TS, Stutz A: Activation and regulation of the inflammasomes. Nat Rev Immunol 2013, 13: 397–411. 10.1038/nri3452
Strowig T, Henao-Mejia J, Elinav E, Flavell R: Inflammasomes in health and disease. Nature 2012, 481: 278–286. 10.1038/nature10759
Lee HM, Kang J, Lee SJ, Jo EK: Microglial activation of the NLRP3 inflammasome by the priming signals derived from macrophages infected with mycobacteria. Glia 2013, 61: 441–452. 10.1002/glia.22448
Hafner-Bratkovic I, Bencina M, Fitzgerald KA, Golenbock D, Jerala R: NLRP3 inflammasome activation in macrophage cell lines by prion protein fibrils as the source of IL-1beta and neuronal toxicity. Cell Mol Life Sci 2012, 69: 4215–4228. 10.1007/s00018-012-1140-0
Freeman D, Cedillos R, Choyke S, Lukic Z, McGuire K, Marvin S, Burrage AM, Sudholt S, Rana A, O°Connor C, Wiethoff CM, Campbell EM: Alpha-synuclein induces lysosomal rupture and cathepsin dependent reactive oxygen species following endocytosis. PLoS One 2013, 8: e62143. 10.1371/journal.pone.0062143
Sokolowski JD, Mandell JW: Phagocytic clearance in neurodegeneration. Am J Pathol 2011, 178: 1416–1428. 10.1016/j.ajpath.2010.12.051
Acknowledgements
We thank Dr. Sara Linse from Lund University for providing the α-synuclein plasmid construct. This work was supported by grants from the Swedish Research Council (2012-2229, 2012-4100), A.E. Berger, Gyllenstiernska Krapperup), the Royal Physiographic Society, Crafoord, Wiberg, G&J Kock, Stohnes foundation, by Swedish governmental agency for innovation systems, VINNOVA, grant No. 2009-00236. By the European Research Council Advanced Award (PRISTINE-PD) to P.B., the Swedish Parkinson Foundation (Sweden), the Swedish Brain Foundation, the Human Frontier Science Program. Grant from Spanish Ministerio de Economia y Competitividad (SAF2012-39029). A.B.-S., J.F.R., N.L.R., P.B. and T.D. are active in Bagadilico (Linné consortium sponsored by the Swedish Research Council) and the Strong Research Environment Multipark (Multidisciplinary research in Parkinson's disease at Lund University).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
H.L. and U.N. hold stocks/options in Galecto Biotech AB, Sweden, a company developing galectin-3-targeting molecules.
Authors' contributions
ABS performed all the experiments except as otherwise noted. JFR prepared α-synuclein monomers and aggregates. TD took the pictures using Transmission Electron Micrograph (T.E.M) and JFR performed the α-synuclein characterization using Western Blot. NR performed intracerebral injections and analyzed microglial galectin-3 immunoreactivity. MAB performed BV2 cells knockdown and measure iNOS levels. ABS, TD, JFR, MAB and JLV designed the study, analyzed and interpreted the data. All authors discussed the results and commented on or edited the manuscript. The first draft of the paper was written by ABS and then TD, JFR, PB, MBS and JLV discussed the results and commented on or edited the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
40478_2014_156_MOESM1_ESM.pdf
Additional file 1: Figure S1: Characterization of α-synuclein monomers and α-synuclein aggregates. We analyzed our α-synuclein preparations using Transmission Electron Micrograph (TEM) (A-C) and western blot (D). Images from TEM showed small molecules in the preparation of monomers (B) and larger molecule arrangements in our aggregated preparations (C), suggested monomeric and oligomeric/fibril proteins structures, respectively. Western Blot analysis confirmed monomeric protein in our monomer protein preparations. In our protein aggregate preparation we found oligomers and monomers and a small fraction of fibrils (>250 kDa). D1, normal exposure time; D2, long exposure time. (PDF 1 MB)
40478_2014_156_MOESM2_ESM.pdf
Additional file 2: Figure S2: Survival assay showed no impairment in microglia viability after treatment with α-synuclein and/or galectin-3 inhibitor. BV2 cell viability was used to study the effect of α-synuclein aggregates and the galectin-3 inhibitor, alone or in combination after 12 h culturing. α-synuclein aggregates did not negatively affect the cell viability. In fact, α-synuclein aggregates (with or together without inhibitor) showed increased mitochondrial activity. XTT Cell Viability Assay Kit was used. One-way ANOVA, *P < 0.05, n = 4, mean ± S.E.M. (PDF 46 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Boza-Serrano, A., Reyes, J.F., Rey, N.L. et al. The role of Galectin-3 in α-synuclein-induced microglial activation. acta neuropathol commun 2, 156 (2014). https://doi.org/10.1186/s40478-014-0156-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-014-0156-0