Abstract
Background
Snoring is a main concern in patients who consult an otolaryngologist (ENT physicians) and patients who have cardiovascular comorbidities or excessive daytime sleepiness who usually consult with other specialists. The aim of this study was to describe the clinical differences in patients with obstructive sleep apnea (OSA) referred from ENT or other specialists.
Methods
A prospective study was carried out between June 2015 and July 2018 in a tertiary center. We included patients with suspected OSA referred by the Home Sleep Apnea Test (HSAT) from different specialties such as ENT or other specialties. The main outcome measures of our study were demographic characteristics, clinical characteristics, sleep questionnaire results and HSAT results between OSA patients referred from ENT or other specialists. We used a t-test and chi-squared test for analysis. The diagnostic accuracy of the sleep questionnaires was achieved using receiver operating characteristic (ROC) curve and the area under the curve (AUC).
Results
A total of 481 patients were included. OSA was occurred in 82.4% of the subjects (90 in ENT and 306 in other specialties). Patients with OSA referred from other specialists were older than ENT patients (55 ± 13 vs 44 ± 12; p < 0.001), there was more obesity (IMC 31 ± 5.0 vs 28.7 ± 3.8; p < 0,001), a larger neck circumference (42.2 cm ± 3.7 vs 40.6 cm ± 3.0; p < 0.001) and more reported comorbidities (p < 0.001). ENT patients reported mild OSA (46% vs 31%, p = 0.015) and more positional apnea (62% vs 39%, p = 0.002). In this group, the STOP-BANG questionnaire showed an AUC 0.695 vs AUC 0.804, and for sensitivity, the best cutoff was 4 points.
Patients referred from otorhinolaryngology are different from those referred from other specialties. Clinical evaluation and screening of OSA should be patient-centered according to these clinical findings.
Similar content being viewed by others
Background
Obstructive sleep apnea (OSA) is a common condition with an estimated prevalence of 20% in the adult population worldwide [1,2,3]. In Chile, according to data from the national health survey in Chile, the population at risk for OSA is 31.2% and the risk of moderate/severe OSA is 8.9% [4]. OSA is linked with an increased risk of hypertension [5], traffic accidents [6, 7], metabolic disorders such as Type 2 diabetes mellitus, insulin resistance and dyslipidemia [8], and a greater number of both fatal and nonfatal cardiovascular events [9, 10]. Due to its complexity, it requires multidisciplinary management including both physicians and nonphysician practitioners from different specialties. Overall, therapeutic options are weight loss, postural therapy, myofunctional therapy, a mandibular advancement device, nasal surgery, multilevel surgery and continuous positive airway pressure devices (CPAP) that are chosen depending on different factors such as the severity of the disease, comorbidities, symptoms and anthropometric variables [3, 11, 12]. However, patients tend to consult specialist physicians who are often not associated with a sleep center and ignore their diagnosis based on their symptoms, personal experiences and recommendation of their acquaintances [13]. We believe people will consult an otolaryngologist (ENT physician) if snoring is their main concern or another specialist if their main problem is cardiovascular comorbidities or excessive daytime sleepiness. This may mean that patients who consult ENT specialists have different clinical characteristics than patients who are evaluated by other specialists (pulmonary physician, neurologists, and internal medicine specialists). The objective of this study was to describe the clinical and anthropometric characteristics, home sleep apnea test (HSAT) scores, and the accuracy of different diagnostic questionnaires in patients with sleep apnea according to the specialty of the doctor who referred them to the study (ENT or other specialties).
Methods
Participants
We performed an observational, prospective study between June 2015 and July 2018 in which all adult patients who were referred to a sleep study performed an ambulatory HSAT because of clinical suspicion of OSA (snoring symptoms, apneas observed by bed partner or excessive daytime sleepiness) in a sleep unit located in a tertiary center placed in Santiago, Chile. Our unit received referrals from both ENT and other medical specialists. Before to sleep study, patients were evaluated using a symptom standardized questionnaire with the purpose of evaluating their sleep schedule, degree of daytime sleepiness, snoring, apnea observed by a bed partner, insomnia, episodes of nocturnal suffocation, nycturia, morning headache, dry mouth upon awakening, memory loss and cognitive deterioration. Sociodemographic data, habits, comorbidities and anthropometric data (such as weight, mallampati score, height and neck, abdominal and waist circumferences) were recorded. The following data were collected: demographic, anthropometric, and comorbidity characteristics, different variables of the HSAT, the apnea-hypopnea index (AHI), mean and minimum oxygen saturation, the oxygen desaturation index (ODI), total sleep time with oxyhemoglobin saturation below 90% (TST-90%), and total time of recording. In addition, the Epworth sleepiness scale [14], modified Thornton scale [15], STOP-BANG questionnaire [16], Beck depression inventory [17], nasal obstruction symptom evaluation (NOSE) scale [18] and the Flemons predictive model score (adjusted neck circumference) [19] were calculated. The presence of OSA was defined as AHI ≥ 5 ev/hr. according to current recommendations [20], and the patients were classified according to the specialty of the referring doctor for subjects referred by ENT specialists and those referred by other specialists (pulmonary physicians, neurologists, and internal medicine specialists).
Home sleep apnea test (HSAT)
To carry out the HSAT, Embletta MPR equipment ([Embla Systems Natus sleep products, USA) was used following the current recommendations and requirements of scientific societies for level III studies [20, 21]. The studies were conducted by the patients at their homes after previous instruction in the laboratory for installation by the patient or their families. They were given a printed user’s manual with iconographic information regarding the installation procedure. All recordings were downloaded the next day. The recordings had to meet the standards required by the American Academy of Sleep Medicine (AASM) for diagnostic studies; otherwise, it had to be repeated. The HSAT analysis was performed manually, according to the AASM guidelines [21], by a respiratory disease specialist with extensive experience in the diagnosis of sleep-disordered breathing (author J.J) who did not know the clinical history, the precedence, and the results of the sleep questionnaires analysis. The following definitions were used according to current recommendations. Apnea was defined as the absence of air flow for more than 10 s; obstructive apnea was defined as the absence of oronasal flow in the presence of abdominal thoracic movements; central apnea was defined as the absence of oronasal flow and abdominal thoracic movements; mixed apnea was defined as the absence of oronasal flow that begins with a central component and ends as obstruction; and hypopnea was defined as discernible airflow reduction (more than 30% and less than 90%) for a period greater than 10 s. To calculate the total number of respiratory events, we used the AHI, dividing the total events (apneas + hypopnea)/total time of recording in hours. A diagnosis of OSA was achieved when the AHI was greater than or equal to five events per hour.
Statistical analysis
The results were expressed as the mean value ± standard deviation for the variables measured in numerical scales, as the median plus interquartile range 25–75 for the ordinal variables and the number and percentage for the ones measured in a nominal scale. The qualitative variables were compared using a Chi squared test, the ordinal variables were analyzed with a Mann-Whitney U test, and the continuous variables were assessed with Student’s t-test. The results of the HSAT were used as the gold standard. The ability of the different surveys (STOP-BANG, Thornton, and Epworth, Flemons predictive model and neck circumference) were used to discriminate patients with and without sleep apnea (AHI ≥ 5). Receiver operating characteristic (ROC) curves and degree or measure of separability was evaluated trough area under the curve (AUC) that was considered > 0.7 as good indicator of separability. The one with the highest amount of sensitivity and specificity for each of the questionnaires was established as the best cutoff point using the Youden Index. Data analysis and recording were performed using Excel 2016 software and SPSS 15.0 software (SPSS Inc., Chicago). A value of p ≤ 0.05 was considered as statistically significant.
Results
General characteristic and reason for referral between groups
A total of 481 adult subjects with clinical suspicion of OSA were evaluated consecutively with the HSAT. A total of 124 patients were derived by ENT compared to 357 by other specialists (pulmonology: 67.2%, cardiology: 13.72%, primary care: 4.0%, internal medicine: 4.88%, neurology: 3.31%, geriatrics: 1.29% and others: 5.6%). Reason for referral in the ENT group was: (Frequent snoring (≥ 1 times/week): 94.36%; usual snoring (≥ 5 times/week) 31.66%; bothered snoring (family group): 62.19%. and excessive daytime sleepiness (49%). Meanwhile in other specialties, reason for referral was: refractory hypertension or non- dipper hypertension (67.28%); snoring and observed apnea (65.90%); snorers with cardiovascular risk factors (8%) and regular snorer in subjects with metabolic disease (8%). The average age was 51.1 ± 14.7 years old, 81% of the patients were men, average neck circumference (NC) was 41.3 ± 3.9 cm, and the body mass index (BMI) was 29.8 ± 4.9 kg/m2. Of all subjects (396/481), 82.4% had OSA (AHI ≥ 5 ev/hr), 34.3% were mild, 34.1% were moderate, and 31.6% were severe. Table 1 describes the clinical characteristics and HSAT of patients with OSA derived by ENT and other specialties.
Differences in patients with OSA derived by ENT and other specialties
A total of 90 patients with OSA were included in ENT group and 306 patients with OSA were included in other specialties group. When analyzing the differences between groups, the following were observed:
-
a)
Symptoms: There were no differences in the presence of symptoms, such as habitual snoring, apneas observed by bed partners, unrefreshing sleep or morning headache. No differences were observed regarding the depression symptoms or the use of hypnotics or antidepressants (Table 2).
-
b)
Anthropometric variables: patients referred by ENT specialists were younger (44.6 ± 12.4 vs 55.4 ± 13.4, p < 0.001), thinner (BMI 28.7 kg/m2 ± 3.8 vs 31.0 kg/m2 ± 5.0, p < 0.001) and had a smaller neck circumference (40.6 cm ± 3.0 vs 42.2 cm ± 3.7, p < 0.001) (Table 2).
-
c)
Comorbidities: Patients referred by ENT specialists had fewer comorbidities (hypertension, dyslipidemia, diabetes, coronary heart disease and gastroesophageal reflux), and there were fewer smokers in this group. No differences were observed regarding the prevalence of respiratory diseases, such asthma or chronic obstructive pulmonary disease or allergic rhinitis or nasal obstruction measured on the NOSE scale. Table 3 shows the associated comorbidities of the patients according to the referring physician.
-
d)
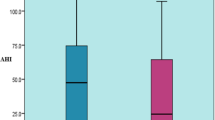
HSAT: Subjects with OSA referred by ENT specialists tended to present milder cases (46% v/s 31%, p = 0.015) and presented more episodes of strict positional apneas (62% v/s 39%, p = 0.002). In addition, they presented with fewer altered oximetric parameters (average saturation, minimum saturation and saturation time under 90%). Table 4 shows the main characteristics of HSAT for patients according to their referring doctor.
-
e)
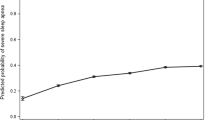
Questionnaires: There was a difference in the predictive ability of the questionnaires to identify patients with OSA (Epworth, STOP-BANG, Thornton, Flemons predictive model and neck circumference) were different. Flemons predictive model achieved the best discrimination for OSA in patients referred by ENT specialists (AUC 0.744, p < 0.001) (Fig. 1a). STOP-BANG had the best discrimination for OSA in patients referred by other professionals (AUC 0.800, CI 0.766–0.882 versus AUC 0.702, CI 0.594–0.796, p = 0.001) (Fig. 1b). According to Youden index, the cutoff point that best discriminated OSA (AHI ≥ 5 ev/hr) in the ENT group was lower than in patients referred by other specialists, obtaining the best sensitivity and specificity for STOP-BANG with 4 and 5 points, for the Flemons predictive model with 45 and 47 points and for neck circumference with 41 and 42 cm, respectively (Table 5).
Discussion
The main results of this study were a) patients who consulted different specialists had different clinical characteristics; b) patients referred by ENT specialists were younger, thinner, had thinner necks, and they also had fewer comorbidities; however, they had the same symptoms of intensity of drowsiness and snoring; c) patients referred by ENT specialists had milder diseases and greater positional predominance; and d) regarding predictive models that achieved the best discrimination in patients with OSA, the predictive model of Flemons was the best for patients referred by ENT specialists, while STOP-BANG was the best for patients referred by other medical specialists.
To the best of our knowledge, this is the first study that evaluated the differences in the profiles of groups of patients studied for suspected sleep apnea referred by otolaryngology and other specialties. This is important because it can change how we appraise past and future studies on the OSA population. We demonstrate that patients who have OSA are different populations depending on which specialist they see for their issues and previous and future studies need to be re-evaluated for possible selection bias depending on which specialty published the data (physicians practicing sleep medicine or surgery). The decision that a patient initially consults an ENT doctor or other specialist depends on a number of sociocultural factors, personal or family experiences, and information in the media, among others. Patients could be expected to consult an ENT specialist if snoring is their main problem or other specialist if either cardiovascular comorbidities or excessive daytime sleepiness is their most relevant problems. However, in the present study, there were no differences in the reporting of habitual snoring, apneas observed by a bed partner, unrefreshing sleep, morning headache, excessive daytime sleepiness measured with the Epworth sleepiness scale or repercussions of snoring measured with the Thornton scale. Although the clinical history was similar, patients with OSA who consulted otolaryngologists were significantly younger and thinner. There were less smokers in that group, and there were fewer associated medical comorbidities commonly associated with OSA (hypertension, dyslipidemia, diabetes, coronary heart disease and gastroesophageal reflux) [8].
In addition, patients who consulted ENT specialists had a higher prevalence of mild disease (46% v/s 31%, p = 0.015), had more strict positional apnea episodes (62% v/s 39%, p = 0.002), and their oximetric parameters were less altered (average saturation, minimum saturation and TST- 90%). This is relevant when evaluating patients and the different perceptions that different specialists have regarding a patient with possible sleep apnea. Thus, despite the fact that the subjects presented with similar symptoms, they consulted different specialists, perhaps due to a perception of severity of the minor picture and the expectation of surgical resolution. According to previous publications, this is a novel finding; however, this finding is interesting because the initial approach of a patient who consults the ENT specialist compared to the approach of a patient who consults another specialist may be different and it might explain why different specialists present different perceptions of the same disease. This is relevant in order to define a potential “phenotype” of patients. Moreover, the performance on the different questionnaires is also different, with the Flemons predictive model achieving the best discrimination for OSA in patients referred by ENT specialists, while the STOP-BANG was the one that had the best discrimination for those referred by other professionals. In the ENT referred group, the best cut-off point to predict significant risk of sleep apnea using STOP-BANG as a screening method was 4 points versus 5 points in patients referred by other specialists. For the Flemons predictive model, the best were 45 and 47 points, and for neck circumference, the best were 41 and 42 cm, respectively. We showed that patients derived by ENT reported lowest neck circumference, age, neck circumference, and hypertension, (all variables included in both questionnaires). These variations can affect the ability of both STOP-BANG and Flemons questionnaires underestimating the predictive value in ENT group compared to other specialties.
These data are very relevant because the different models of clinical prediction have been evaluated in the general population in Chile [3, 22] and have not considered the potential selection bias created by the referral source or specialty performing the study. We did not use the Berlin questionnaire due to poor performance in our population [23]. This was a prospective study of consecutive patients with high n-value (481) and there was complete characterization of their diseases, major limitations, and possible bias that referring physicians held when carrying out an evaluation in a multidisciplinary center with established study programs. Finally, we used a HSAT or type III study as a reference standard; however, full polysomnography is better than HSAT for OSA diagnosis [24]. We decided to use HSAT due to recent publications showing that full polysomnography is not necessary for the management of patients with suspected OSA. Moreover, this approach is associated with potentially wasteful healthcare resources [3, 24].
Conclusions
In conclusion, the patients with sleep apnea from different health teams were different. The subjects who consulted otolaryngologists were younger, thinner, with less comorbidities, but equally symptomatic. Therefore, the research strategies must be different and oriented to the requirements of the patients.
Availability of data and materials
All data will be available by personal communication with corresponding author.
Abbreviations
- AASM):
-
American Academy of Sleep Medicine
- AHI):
-
Apnea-hypopnea index
- AUC):
-
area under the curve
- BMI):
-
Body mass index
- CPAP):
-
Continuous Positive Airway Pressure
- ENT):
-
Otolaryngology
- HSAT):
-
Home Sleep Apnea Test
- NC):
-
neck circumference
- NOSE):
-
nasal obstruction symptom evaluation
- ODI):
-
oxygen desaturation index
- OSA):
-
Obstructive sleep apnea
- ROC):
-
Receiver operating curves
- TST-90%):
-
Total sleep time with oxyhemoglobin saturation below 90%
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–5.
Duran J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001;163(3 Pt 1):685–9.
Saldias PF, Jorquera AJ, Diaz PO. Predictive value of clinical features and nocturnal oximetry for the detection of obstructive sleep apnea syndrome. Rev Med Chil. 2010;138(8):941–50.
J. Carrillo CV, A. Cisternas, P. Olivares-Tirado. Obstructive sleep apnea: findings from the Chilean National Health Survey 2010. 49 Congreso Chileno de Enfermedades Respiratorias 2016.
Duran-Cantolla J, Aizpuru F, Martinez-Null C, Barbe-Illa F. Obstructive sleep apnea/hypopnea and systemic hypertension. Sleep Med Rev. 2009;13(5):323–31.
Young T, Blustein J, Finn L, Palta M. Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults. Sleep. 1997;20(8):608–13.
Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. Cooperative group Burgos-Santander. N Engl J Med. 1999;340(11):847–51.
Labarca G, Cruz NR, Descalzi F. Multisystemic involvement in obstructive sleep apnea. Rev Med Chil. 2014;142(6):748–57.
Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, Nieto FJ, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071–8.
Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–53.
Lloberes P, Duran-Cantolla J, Martinez-Garcia MA, Marin JM, Ferrer A, Corral J, et al. Diagnosis and treatment of sleep apnea-hypopnea syndrome. Spanish Society of Pulmonology and Thoracic Surgery. Arch Bronconeumol. 2011;47(3):143–56.
Qaseem A, Holty JE, Owens DK, Dallas P, Starkey M, Shekelle P. Management of Obstructive Sleep Apnea in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2013.
Phillipson EA. Sleep apnea--a major public health problem. N Engl J Med. 1993;328(17):1271–3.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5.
Richard W, Kox D, den Herder C, Laman M, van Tinteren H, de Vries N. The role of sleep position in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2006;263(10):946–50.
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812–21.
Wang YP, Gorenstein C. Assessment of depression in medical patients: a systematic review of the utility of the Beck depression inventory-II. Clinics (Sao Paulo). 2013;68(9):1274–87.
Larrosa F, Roura J, Dura MJ, Guirao M, Alberti A, Alobid I. Adaptation and validation of the Spanish version of the nasal obstruction symptom evaluation (NOSE) scale. Rhinology. 2015;53(2):176–80.
Flemons WW. Clinical practice. Obstructive sleep apnea. N Engl J Med. 2002;347(7):498–504.
Qaseem A, Dallas P, Owens DK, Starkey M, Holty JE, Shekelle P, et al. Diagnosis of obstructive sleep apnea in adults: a clinical practice guideline from theAmerican College of Physicians. Ann Intern Med. 2014;161(3):210–20.
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504.
Saldías F, Gassmann J, Canelo A, Uribe J, Díaz Patiño O. Accuracy of sleep questionnaires for obstructive sleep apnea syndrome screening. Rev Med Chile 2018; 146: 1123–1134. 2018;146:1123–34.
Jorquera J, Freire M, Munoz P, F S. Utilidad de los indices clinicos y oximetricos en el diagnostico de apnea obstructiva del sueno moderada a severa. XXXV Congreso Chileno de Enfermedades Respiratorias; Valdivia: Rev. Chil. Enferm respir.; 2002.
Corral J, Sanchez-Quiroga MA, Carmona-Bernal C, Sanchez-Armengol A, Sanchez-de-la-Torre A, Duran-Cantolla J, et al. Conventional Polysomnography is not necessary for the Management of Most Patients with suspected obstructive sleep apnea. Am J Respir Crit Care Med. 2017.
Acknowledgments
We will recognize the support of Clinica Las Condes, Santiago. Chile.
Funding
Authors declare no funding regarding this article.
Author information
Authors and Affiliations
Contributions
JJ: Principal investigator, data extraction, data analysis, manuscript redaction and final approval. CS, JD, AC, GN: Data extraction, data synthesis, manuscript redaction and final approval. CA, RC and GL: Data conception, critical analysis, manuscript redaction and final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Institution (Institutional Review Board, Clinica Las condes) and the patients signed the informed consent document prior to their incorporation.
Consent for publication
All authors confirm this final version and consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Salas, C., Dreyse, J., Contreras, A. et al. Differences in patients derived from otolaryngology and other specialties with sleep apnea. J of Otolaryngol - Head & Neck Surg 48, 53 (2019). https://doi.org/10.1186/s40463-019-0373-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40463-019-0373-4