Abstract
Background
The risk of delayed autoimmunity occurring months or years after discontinuation of immunotherapy is frequently asserted in the literature. However, specific cases were rarely described until 2018, when a wave of reports surfaced. With expanding I-O indications in the adjuvant/neoadjuvant curative setting, growing numbers of patients will receive limited courses of immunotherapy before entering routine surveillance. In this context, under-recognition of DIRE could pose a growing clinical hazard.
Methods
The aim of this study was to characterize DIRE through identification of existing reports of delayed post-treatment irAE in cancer patients treated with immunotherapy. We performed a PubMed literature review from 2008 through 2018 to determine the median data safety reporting window from existing I-O clinical trials, which we then applied to define the DIRE cutoff, and collated all qualifying reports over the same time span. DIRE was defined as new immune-related adverse events (irAE) manifesting ≥90 days after discontinuation of immunotherapy.
Results
Median duration of I-O clinical trials data safety reporting was 90 days (82% ≤ 90 days). DIRE cutoff was thus set as ≥90 days post-immunotherapy. We identified 23 qualifying cases; 21 by literature review and 2 from our institution. Median off-treatment interval to DIRE was 6 months (range: 3 to 28). Median cumulative immunotherapy exposure was 4 doses (range: 3 to 42). Involvement included endocrine, neurologic, GI, pulmonary, cardiac, rheumatologic and dermatologic irAE.
Conclusions
As immunotherapy indications expand into the curative setting, often with brief exposure and potentially sequenced with multimodality treatments, it will be necessary to recognize an emerging diagnostic complex, which we have termed delayed immune-related events (DIRE). Clinical vigilance has the potential to reduce morbidity from diagnostic delay, as irAE are generally manageable with prompt initiation of treatment – or from misdiagnosis - as misattribution can lead to unnecessary or harmful interventions as we describe. DIRE should therefore figure prominently in the differential diagnosis of patients presenting with illnesses of unclear etiology, irrespective of intervening treatments or interval post-immunotherapy, both of which can confound diagnosis. Increased recognition will rest on delineation of DIRE as a clinical diagnostic entity.
Similar content being viewed by others
Background
Two recent cases of severe autoimmune illness in patients treated by our institution’s Head and Neck Oncology Department were the impetus for this study (Additional file 1: Institutional Case Series). Both cases were diagnosed months to years after brief exposure to immunotherapy in previous neoadjuvant surgical window trials. In Case No. 1, the relapsing remitting course of neurologic deficits roughly two years after a one week course of immunotherapy (anti-OX40 agonist mAb), led to diagnostic disputes among consulting specialists and resulted in the placement of an Ommaya reservoir based on an erroneous diagnosis of leptomeningeal carcinomatosis, ultimately requiring transfer through three hospital systems to arrive at a conclusive diagnosis of neurosarcoidosis. We found a prevailing assertion in the literature that new autoimmune illness, presenting months to years after discontinuation of immunotherapy, has been well-described. And yet, on tracing the citation trail from 39 review articles, we were able to identify only a single case report (cited by several reviews), describing a patient with delayed dermatologic hypersensitivity reaction (swelling and >erythema of the upper extremities with pruritus) diagnosed 76 days after the last dose of ipilimumab [1]. This prompted us to ask, to what extent are post-immunotherapy immune-related adverse events (irAE) being reported in the literature, what barriers exist to recognition, and to what extent have the hazards of misdiagnosis been described.
Methods
The aim of this study was to characterize DIRE through identification of existing reports of delayed post-treatment irAE in cancer patients treated with immunotherapy. Literature review was conducted in two phases. In the first phase, we queried existing clinical trials to determine a temporal cutoff by which to define DIRE. In the second phase, we applied this cutoff to identify relevant case reports over the same period, and included 2 cases from our institution.
Defining temporal cutoff for DIRE
PubMed search of English language reports from Jan 1, 2008 to Dec 31, 2018 was conducted using first-pass Boolean filtering followed by automated titles keyword filtering (Additional file 2: Supplementary Methods). Entries were then divided into two groups: 1) I-O clinical trials, or 2) irAE or toxicity-related case reports. The text, supplement and on-line protocol (when available) for each confirmed I-O clinical trial was manually reviewed to identify the duration of serious adverse event (SAE) reporting. The median SAE reporting duration, thus determined, was taken as the temporal cutoff to define DIRE.
Literature search for clinical cases
We next performed full text keyword search of all identified entries (trials and case reports), using: “after,” “delay,” “time,” “onset,” “days,” “week,” and “month.” Articles that described irAE after immunotherapy discontinuation were manually reviewed, including recursive bibliography search for any additional reports. Identified DIRE cases were confirmed by consensus reading of at least two investigators. Cases in which an irAE had been previously diagnosed (e.g. colitis first noted on-treatment, then recurring post-treatment), were considered recrudescent and excluded.
Results
Determining a temporal cutoff for DIRE (Fig. 1)
PubMed Boolean filter and sequential automated titles keyword filter resulted in 3600 and 1489 entries, respectively (Fig. 1a). Of these, 194 were I-O clinical trials, of which 127 specified a discrete duration of SAE reporting in the report or via on-line protocol (Fig. 1b). The duration of SAE reporting following the last dose of immunotherapy was 90 days or less in 82% of I-O clinical trials (range 28 to 100 days). Extension of the SAE reporting window to 90 or 100 days appears to be a more recent trend, accounting for only 7% (1/15) of pre-2015 trials identified. The median I-O trials SAE reporting window (90 days), thus determined, was taken as the temporal cutoff to define DIRE cases the literature search which followed.
Literature search for DIRE cases (Fig. 2)
Literature search identified 367 case reports, case series and review articles in which the title suggested relevance to irAE or I-O toxicity. These were combined with the 194 I-O clinical trials identified by preceding search, for full-text keyword screening of n = 561 reports (Fig. 2a). We identified 21 cases of DIRE using a definition of autoimmune sequelae newly diagnosed ≥90 days following discontinuation of immunotherapy [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19]. Only one case could be confirmed from an I-O trial, reflecting the lack of granularity inherent to conventional SAE reporting (eg. timing of SAE onset relative to first or last treatment dose) [15]. Notably, over half the cases came from 2018 (11 of 21). Two local cases are described in this report, bringing the total to 23 DIRE cases (Table 1). Literature search additionally identified 16 suspected DIRE cases, primarily from I-O clinical trials (14/16), which could not be confirmed or excluded due to lack of sufficient detail and are included in the online supplement (Additional file 3: Table S1).
Characteristics of DIRE cases (Table 1)
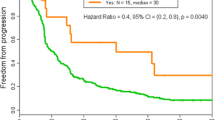
The median interval to DIRE diagnosis was 6 months post-immunotherapy (range 3 to 28 months). Target organ system involvement (Fig. 2b) included: endocrine (7 patients), cutaneous (5), neurologic (5), pulmonary (3), cardiac (3), gastrointestinal (2), rheumatologic (1) and ophthalmologic (1). Interestingly, over half of the DIRE cases occurred following a brief immunotherapy course of ≤4 doses (Fig. 2c: median 4 doses, range 3 to 42). Immunotherapy exposure included pembrolizumab, nivolumab, ipilimumab, tremelimumab plus PF-3512676 (TLR9 agonist) and MEDI6469 (anti-OX40 mAb agonist). In 5 cases, patients received both anti-PD1 and anti-CTLA-4, sequentially or concurrently. Three patients experienced 2 or more DIRE, while a distinctly separate group of patients, roughly 50% (12/23), experienced prior on-treatment irAEs - frequently the proximal cause of immunotherapy discontinuation (9/12) - of which most were managed with corticosteroids (7/12), with the addition of infliximab for cases of colitis (3/12).
Melanoma predominated (15 cases), followed by non-small cell lung cancer (NSCLC) (4), HPV-associated head and neck squamous cell carcinoma (HNSCC) (2), cutaneous squamous cell carcinoma (1) and not specified (1; likely melanoma, clinical trial) [15]. The majority of DIRE cases occurred in the recurrent/metastatic setting (18/23), but three cases were reported following adjuvant melanoma treatment; we identified two cases following neoadjuvant surgical window I-O trials in HNSCC. Subsequent treatment following immunotherapy included: BRAF inhibitor for a melanoma patient (to which Guillain-Barré syndrome was erroneously attributed), and multimodality standard of care (surgery followed by risk-adapted radiation +/− chemotherapy) for the two HNSCC patients, both of which developed protracted neurologic DIRE, with adrenal crisis included in the DIRE complex in case No. 2 (Table 1; Additional file 1: Institutional Case Series).
Suspected DIRE cases – incomplete reports
There were 16 additional suspected DIRE cases identified by literature search, which although likely representing bona fide examples, could not be included due to insufficient reported details [20,21,22,23,24,25,26]. (Additional file 4: Clinical Trial AEs Suspicious for DIRE) Target organ system involvement included endocrine (6 patients), cutaneous (6), gastrointestinal (3), genitourinary (1), hematologic (1), rheumatologic (1) and ophthalmologic (1). Immunotherapy exposure included pembrolizumab, nivolumab, ipilimumab and gp100. Melanoma predominated (15 cases) of which 20% were adjuvant (3/15); the sixteenth case was metastatic NSCLC.
Discussion
The variable temporality of on-treatment irAE is well-characterized [27,28,29,30,31,32,33,34,35,36,37]. However, off-treatment autoimmune illness, manifesting months to years after discontinuation of immunotherapy, have occasionally been alluded to in the literature, but probably represent an under-recognized phenomenon [38,39,40,41,42]. In 2013, the first such report involving a case of vitiligo manifesting 9 months after discontinuation of pembrolizumab appeared in abstract form in Deutschen Dermatologischen Gesellschaft (case No. 9, Table 1) [8]. Through 2017, a handful of reports described cases of post-immunotherapy autoimmune illness, but focused primarily on target organ manifestations, rather than the fact of delayed onset following an extended interval off-treatment and the diagnostic challenges this most likely posed [3, 13, 16,17,18,19]. By the close of 2018, however, a wave of new reports had surfaced, some explicitly emphasizing the significance of newly manifest irAE emerging long after discontinuation of immunotherapy, a clinical diagnostic complex we have termed DIRE (delayed immune-related events).
To our knowledge, this is the first study to collate existing scattered reports of substantially delayed irAE, manifesting at prolonged intervals after discontinuation of immunotherapy. Over half of all cases occurred following short courses of immunotherapy of ≤4 doses, and the majority of cases were reported in 2018 (Table 1). There is sound mechanistic plausibility to support these observations. For instance, PD-1 receptor occupancy on T cells plateaus at approximately 80% up to 90 days after a single dose of nivolumab, despite a serum half-life of only 12–20 days. After three doses, occupancy remains at 40% for more than 8 months after the last dose [43]. Just as durable clinical responses following immunotherapy appear to be independent of dose and duration of treatment, so too, immune-mediated toxicity would be expected to display variable onset relative to treatment.
Obstacles to assessment of the true frequency and extent of DIRE are inherent in current I-O clinical trials reporting convention. Issues such as limited follow up periods and incompleteness of irAE reporting were previously described by Chen et al. in a systematic review of I-O clinical trials [44]. Some trial protocols explicitly excluded reporting of adverse events occurring > 30 days after last dose, or reporting of any adverse events after initiation of another cancer treatment [45,46,47,48,49]. Importantly, irAE are routinely reported relative to the start of treatment, without any related information regarding the end of treatment [21, 50,51,52,53,54]. We were only able to confirm a single case of DIRE in an I-O clinical trial, despite rather simple criteria we proposed, and a careful manual review of all published trials reports. This was a case of grade 2 uveitis occurring 157 days after end of study treatment (TLR9 + tremelimumab), which was couched in a DLT table that caught our eye on manual reading of the report (case No. 16, Table 1), and actually not within the searchable text [15].
The fact that our literature search was able to identify cases dating back to 2013 suggests that DIRE is not a new phenomenon. Indeed, we identified 39 review articles that posited the existence of delayed irAE post discontinuation of treatment [29, 31, 34, 38,39,40,41,42, 44, 55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84]; however, only two of these reviews provided specific citations, both to the same report describing a case of delayed dermatologic hypersensitivity reaction starting 76 days following final dose of ipilimumab [34, 66]. This particular example would not have posed a substantial diagnostic challenge, nor qualified as DIRE based on a ≥ 90 day cutoff. It may be that clinical anecdotes were in circulation as a basis for the widespread assertions we encountered in the literature, but the lack of citations to any extant reports suggest an under-reporting effect, likely deriving from clinical reluctance to recognize autoimmunity at a distance, in favor of misattribution to more proximal events or treatments.
Two recent cases of severe and substantially delayed post-treatment irAE occurring in patients treated by our institution’s Head and Neck Oncology Department are described in this report. These serve as among the first detailed examples of DIRE following neoadjuvant immunotherapy, and describe the diagnostic uncertainty posed by otherwise healthy individuals being followed for surveillance, months to years following remote (and brief) immunotherapy exposure in the neoadjuvant clinical trials context. We were unable to find analogous reports in the literature, indicating a diagnostic hazard which is predicted to increase with new I-O approvals in the curative setting (adjuvant/neoadjuvant treatment) [21, 85,86,87,88,89,90,91,92]. Current diagnostic challenges are reminiscent of early experience in allogeneic bone marrow transplantation, prior to delineation of graft versus host disease (GVHD) as a clinical diagnostic complex. Diagnostic misattribution to the effects of intercurrent chemotherapy, radiation, disease recurrence or sepsis, were reported as common confounding factors [93, 94]. Clinical awareness, therefore has the potential to avert morbidity/mortality from misdiagnosis, by preventing unnecessary and potentially harmful interventions, (as in the neurosarcoidosis case we describe of Ommaya reservoir placement on the basis of an erroneous leptomeningeal carcinomatosis diagnosis) – and from diagnostic delay, given that these conditions are generally manageable with prompt initiation of immune suppressive therapy.
As contemporary examples of diagnostic hazard, our literature search identified two reports, one of immune-related colitis manifesting 23 months after completion of pembrolizumab, in which the patient was initially treated with neostigmine based on an erroneous diagnosis of Ogilvie’s syndrome, failed to respond, and then underwent right-sided colectomy, which unfortunately revealed correct diagnosis (Case No. 6, Table 1) [5]. A case of Guillain-Barré syndrome (GBS) manifesting 3 months post-pembrolizumab, was erroneously attributed to subsequent treatment with dabrafenib (case No. 22, Table 1) [18]. Only one other case of GBS has been associated with dabrafenib, in a 2015 abstract, again post-pembrolizumab [95], whereas the association of checkpoint blockade with GBS is well-recognized [96, 97]. Clinical confounding, akin to experience prior to categorization of GVHD, attests to the need for characterization of DIRE as a clinical diagnostic entity. These cases illustrate several hazards of diagnostic misattribution, including unnecessary/invasive procedures, delay in the proper management of an autoimmune illness, and abandonment of an otherwise beneficial therapy (eg…BRAF inhibitors).
We would highlight three important limitations to this study. First, it is impossible to prove direct causality between immunotherapy and delayed autoimmunity, particularly from case reports. With rare exception, autoimmune sequelae of immunotherapy remain diagnoses-of-exclusion in clinical practice. The lack of a temporal association or dose-dependent relationship, which might otherwise enhance credulity, lends to a cautious skepticism which only further empiric observation will dispel or reinforce. Second, there is a heterogeneous level of detail regarding diagnosis and clinical management in the case reports thus far available. As clinical awareness increases, we anticipate that a growing emphasis will be placed on diagnostic algorithms, management strategies, and possibly unique DIRE associations to specific drugs. Third, we cannot accurately begin to gauge the frequency or true extent of DIRE given clinical trial reporting conventions which favor attribution of irAE to the most temporally proximal treatment/process and reporting irAE relative only to start of treatment but not end of treatment.
Conclusions
With expanding I-O indications in the curative disease setting, either as adjuvant/neoadjuvant therapy, or in combination with multimodality approaches, growing numbers of patients will be exposed to immunotherapy before transitioning to routine clinical surveillance. In this context, it will be necessary to recognize an emerging clinical diagnostic complex, which we have termed DIRE (delayed immune-related events), manifesting months to years after discontinuation of immunotherapy and representing a substantive diagnostic hazard. In our experience, diagnostic misattribution is clinically reinforced by several confounding factors: 1) a brief and remote immunotherapy exposure; 2) intervening treatments with overlapping toxicities; 3) a protracted diagnosis-by-exclusion process; 4) reduced vigilance in the post-treatment setting. DIRE syndrome should therefore figure prominently in the differential diagnosis of patients presenting with unexplained illnesses, irrespective of post-immunotherapy interval. The clinical hazards of diagnostic misattribution include inappropriate invasive procedures (unnecessary colectomy or Ommaya reservoir placement, as in cases described) and delay to start of treatment for autoimmune conditions that are often readily managed with prompt initiation of immune suppressive therapy. Changes to I-O clinical trial reporting convention could unmask the true incidence of DIRE, and include: the standardization of irAE reporting duration; collection of safety data regardless of whether a new cancer therapy is started; publication of irAE that emerge after the formal study period; and reporting of time-to-onset of irAE in relation to both treatment start and end.
Availability of data and materials
The data and references supporting the conclusions of this article are included within the main text and additional files.
Abbreviations
- DIRE:
-
Delayed-immune related events
- DLT:
-
Dose-limiting toxicity
- GBS:
-
Guillain-Barré syndrome
- GVHD:
-
Graft versus host disease
- HNSCC:
-
Head and neck squamous cell carcinoma
- I-O:
-
Immuno-oncology
- irAE:
-
Immune-related adverse event
- mAb:
-
Monoclonal antibody
- NSCLC:
-
Non-small cell lung cancer
- SAE:
-
Serious adverse event
References
Ludlow SP, Kay N. Delayed dermatologic hypersensitivity reaction secondary to ipilimumab. J Immunother Hagerstown Md 1997. 2015;38:165–6.
Mandalà M, Merelli B, Indriolo A, Tondini C. Late-occurring toxicity induced by an immune checkpoint blockade in adjuvant treatment of a stage III melanoma patient. Eur J Cancer Oxf Engl 1990. 2018;95:130–2.
Diamantopoulos PT, Gaggadi M, Kassi E, Benopoulou O, Anastasopoulou A, Gogas H. Late-onset nivolumab-mediated pneumonitis in a patient with melanoma and multiple immune-related adverse events. Melanoma Res. 2017;27:391–5.
Garcia CA, El-Ali A, Rath TJ, Contis LC, Gorantla V, Drappatz J, et al. Neurologic immune-related adverse events associated with adjuvant ipilimumab: report of two cases. J Immunother Cancer. 2018;6:83.
Sarofim M, Winn R. Rare case of delayed onset colitis due to immunotherapy for malignant melanoma. ANZ J Surg. 2018;0. https://doi.org/10.1111/ans.14768.
Boudjemaa A, Rousseau-Bussac G, Monnet I. Late-onset adrenal insufficiency more than 1 year after stopping Pembrolizumab. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2018;13:e39–40.
Tan I, Malinzak M, Salama AKS. Delayed onset of neurosarcoidosis after concurrent ipilimumab/nivolumab therapy. J Immunother Cancer. 2018;6. https://doi.org/10.1186/s40425-018-0390-2.
Hanrahan P, Van Der Westhuizen A, Collins S, Owens D, Hersey P. Delayed autoimmune effects in patients treated with antibodies against the checkpoint inhibitor PD1. J Dtsch Dermatol Ges. 2013;11:16.
Parakh S, Cebon J, Klein O. Delayed autoimmune toxicity occurring several months after cessation of anti-PD-1 therapy. Oncologist. 2018;23:849–51.
Shrotriya S, Rai MP, Alratroot A, Sarzynski E. Delayed presentation of isolated Adrenocorticotropin insufficiency after Nivolumab therapy for advanced non-small-cell lung carcinoma (NSCLC). BMJ Case Rep. 2018;2018:bcr-2018-225048.
Otsubo K, Nakatomi K, Furukawa R, Ashida K, Yoneshima Y, Nakanishi Y, et al. Two cases of late-onset secondary adrenal insufficiency after discontinuation of nivolumab. Ann Oncol. 2017;28:3106–7.
Wang LL, Patel G, Chiesa-Fuxench ZC, McGettigan S, Schuchter L, Mitchell TC, et al. Timing of onset of adverse cutaneous reactions associated with programmed cell death protein 1 inhibitor therapy. JAMA Dermatol. 2018;154:1057–61.
Zarbo A, Belum VR, Sibaud V, Oudard S, Postow MA, Hsieh JJ, et al. Immune-related alopecia (areata and universalis-type) in cancer patients receiving immune checkpoint inhibitors. Br J Dermatol. 2017;176:1649–52.
Dasanu CA, Jen T, Skulski R. Late-onset pericardial tamponade, bilateral pleural effusions and recurrent immune monoarthritis induced by ipilimumab use for metastatic melanoma. J Oncol Pharm Pract Off Publ Int Soc Oncol Pharm Pract. 2017;23:231–4.
Millward M, Underhill C, Lobb S, McBurnie J, Meech SJ, Gomez-Navarro J, et al. Phase I study of tremelimumab (CP-675 206) plus PF-3512676 (CPG 7909) in patients with melanoma or advanced solid tumours. Br J Cancer. 2013;108:1998–2004.
Roth ME, Muluneh B, Jensen BC, Madamanchi C, Lee CB. Left ventricular dysfunction after treatment with Ipilimumab for metastatic melanoma. Am J Ther. 2016;23:e1925–8.
Khoja L, Maurice C, Chappell M, MacMillan L, Al-Habeeb AS, Al-Faraidy N, et al. Eosinophilic fasciitis and acute encephalopathy toxicity from Pembrolizumab treatment of a patient with metastatic melanoma. Cancer Immunol Res. 2016;4:175–8.
Khoja L, Butler MO, Chappell MA, Hogg D, Joshua AM. Increased treatment-related toxicity subsequent to an anti-PD-1 agent. Curr Oncol Tor Ont. 2015;22:e320–2.
Yun S, Vincelette ND, Mansour I, Hariri D, Motamed S. Late onset Ipilimumab-induced pericarditis and pericardial effusion: a rare but life threatening complication. Case Rep Oncol Med. 2015;2015:794842.
Luu Q, Major G. Unleashing the tiger – iatrogenic autoimmunity from cancer immunotherapy drugs. JRSM Open. 2018;9. https://doi.org/10.1177/2054270417746905.
Weber J, Mandala M, Del Vecchio M, Gogas HJ, Arance AM, Cowey CL, et al. Adjuvant Nivolumab versus Ipilimumab in resected stage III or IV melanoma. N Engl J Med. 2017;377:1824–35.
Wolchok JD, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob J-J, Cowey CL, et al. Overall survival with combined Nivolumab and Ipilimumab in advanced melanoma. N Engl J Med. 2017;377:1345–56.
Ricciuti B, Metro G, Baglivo S, Colabrese D, Chiari R, Bennati C, et al. Long-lasting response to Nivolumab and immune-related adverse events in a nonsquamous metastatic non-small cell lung cancer patient. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2017;12:e51–5.
Yamazaki N, Kiyohara Y, Uhara H, Fukushima S, Uchi H, Shibagaki N, et al. Phase II study of ipilimumab monotherapy in Japanese patients with advanced melanoma. Cancer Chemother Pharmacol. 2015;76:997–1004.
Robert C, Thomas L, Bondarenko I, O’Day S, Weber J, Garbe C, et al. Ipilimumab plus Dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–26.
McDermott D, Haanen J, Chen T-T, Lorigan P, O’Day S, For the MDX010-20 investigators. Efficacy and safety of ipilimumab in metastatic melanoma patients surviving more than 2 years following treatment in a phase III trial (MDX010-20). Ann Oncol. 2013;24:2694–8.
Abdel-Rahman O, ElHalawani H, Fouad M. Risk of cutaneous toxicities in patients with solid tumors treated with immune checkpoint inhibitors: a meta-analysis. Future Oncol Lond Engl. 2015;11:2471–84.
Akturk HK, Michels AW. Adverse events associated with immune checkpoint blockade. N Engl J Med. 2018;378:1163–4.
Brahmer JR, Lacchetti C, Schneider BJ, Atkins MB, Brassil KJ, Caterino JM, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol Off J Am Soc Clin Oncol. 2018;36:1714–68.
Costa R, Carneiro BA, Agulnik M, Rademaker AW, Pai SG, Villaflor VM, et al. Toxicity profile of approved anti-PD-1 monoclonal antibodies in solid tumors: a systematic review and meta-analysis of randomized clinical trials. Oncotarget. 2017;8:8910–20.
Michot JM, Bigenwald C, Champiat S, Collins M, Carbonnel F, Postel-Vinay S, et al. Immune-related adverse events with immune checkpoint blockade: a comprehensive review. Eur J Cancer Oxf Engl 1990. 2016;54:139–48.
Naidoo J, Page DB, Li BT, Connell LC, Schindler K, Lacouture ME, et al. Toxicities of the anti-PD-1 and anti-PD-L1 immune checkpoint antibodies. Ann Oncol Off J Eur Soc Med Oncol. 2015;26:2375–91.
Nishino M, Sholl LM, Hodi FS, Hatabu H, Ramaiya NH. Anti-PD-1-related pneumonitis during cancer immunotherapy. N Engl J Med. 2015;373:288–90.
Spain L, Diem S, Larkin J. Management of toxicities of immune checkpoint inhibitors. Cancer Treat Rev. 2016;44:51–60.
Topalian SL, Sznol M, McDermott DF, Kluger HM, Carvajal RD, Sharfman WH, et al. Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J Clin Oncol Off J Am Soc Clin Oncol. 2014;32:1020–30.
Wang P-F, Chen Y, Song S-Y, Wang T-J, Ji W-J, Li S-W, et al. Immune-related adverse events associated with anti-PD-1/PD-L1 treatment for malignancies: a meta-analysis. Front Pharmacol. 2017;8:730.
Weber JS, Hodi FS, Wolchok JD, Topalian SL, Schadendorf D, Larkin J, et al. Safety profile of Nivolumab monotherapy: a pooled analysis of patients with advanced melanoma. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35:785–92.
Champiat S, Lambotte O, Barreau E, Belkhir R, Berdelou A, Carbonnel F, et al. Management of immune checkpoint blockade dysimmune toxicities: a collaborative position paper. Ann Oncol Off J Eur Soc Med Oncol. 2016;27:559–74.
Haanen JBAG, Carbonnel F, Robert C, Kerr KM, Peters S, Larkin J, et al. Management of toxicities from immunotherapy: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol Off J Eur Soc Med Oncol. 2017;28(suppl_4):iv119–42.
Luke JJ, Ott PA. PD-1 pathway inhibitors: the next generation of immunotherapy for advanced melanoma. Oncotarget. 2015;6:3479–92.
Puzanov I, Diab A, Abdallah K, Bingham CO, Brogdon C, Dadu R, et al. Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) toxicity management working group. J Immunother Cancer. 2017;5:95.
Tarhini A. Immune-mediated adverse events associated with ipilimumab ctla-4 blockade therapy: the underlying mechanisms and clinical management. Scientifica. 2013;2013:857519.
Brahmer JR, Drake CG, Wollner I, Powderly JD, Picus J, Sharfman WH, et al. Phase I study of single-agent anti–programmed Death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol. 2010;28:3167–75.
Chen TW, Razak AR, Bedard PL, Siu LL, Hansen AR. A systematic review of immune-related adverse event reporting in clinical trials of immune checkpoint inhibitors. Ann Oncol Off J Eur Soc Med Oncol. 2015;26:1824–9.
Weber JS, Gibney G, Sullivan RJ, Sosman JA, Slingluff CL, Lawrence DP, et al. Sequential administration of nivolumab and ipilimumab with a planned switch in patients with advanced melanoma (CheckMate 064): an open-label, randomised, phase 2 trial. Lancet Oncol. 2016;17:943–55.
Fang W, Yang Y, Ma Y, Hong S, Lin L, He X, et al. Camrelizumab (SHR-1210) alone or in combination with gemcitabine plus cisplatin for nasopharyngeal carcinoma: results from two single-arm, phase 1 trials. Lancet Oncol. 2018;19:1338–50.
Kaufman HL, Russell J, Hamid O, Bhatia S, Terheyden P, D’Angelo SP, et al. Avelumab in patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial. Lancet Oncol. 2016;17:1374–85.
Emens LA, Cruz C, Eder J, et al. Long-term clinical outcomes and biomarker analyses of atezolizumab therapy for patients with metastatic triple-negative breast cancer: a phase 1 study. JAMA Oncol. 2019;5:74–82.
Lukas RV, Rodon J, Becker K, Wong ET, Shih K, Touat M, et al. Clinical activity and safety of atezolizumab in patients with recurrent glioblastoma. J Neuro-Oncol. 2018;140:317–28.
Horn L, Gettinger SN, Gordon MS, Herbst RS, Gandhi L, Felip E, et al. Safety and clinical activity of atezolizumab monotherapy in metastatic non-small-cell lung cancer: final results from a phase I study. Eur J Cancer Oxf Engl 1990. 2018;101:201–9.
Vokes EE, Ready N, Felip E, Horn L, Burgio MA, Antonia SJ, et al. Nivolumab versus docetaxel in previously treated advanced non-small-cell lung cancer (CheckMate 017 and CheckMate 057): 3-year update and outcomes in patients with liver metastases. Ann Oncol. 2018;29:959–65.
Hodi FS, Chiarion-Sileni V, Gonzalez R, Grob J-J, Rutkowski P, Cowey CL, et al. Nivolumab plus ipilimumab or nivolumab alone versus ipilimumab alone in advanced melanoma (CheckMate 067): 4-year outcomes of a multicentre, randomised, phase 3 trial. Lancet Oncol. 2018;19:1480–92.
Schachter J, Ribas A, Long GV, Arance A, Grob J-J, Mortier L, et al. Pembrolizumab versus ipilimumab for advanced melanoma: final overall survival results of a multicentre, randomised, open-label phase 3 study (KEYNOTE-006). Lancet Lond Engl. 2017;390:1853–62.
Schadendorf D, Wolchok JD, Hodi FS, Chiarion-Sileni V, Gonzalez R, Rutkowski P, et al. Efficacy and safety outcomes in patients with advanced melanoma who discontinued treatment with Nivolumab and Ipilimumab because of adverse events: a pooled analysis of randomized phase II and III trials. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35:3807–14.
Andrews S, Holden R. Characteristics and management of immunerelated adverse effects associated with ipilimumab, a new immunotherapy for metastatic melanoma. Cancer Manag Res. 2012;4:299–307.
Astaras C, de Micheli R, Moura B, Hundsberger T, Hottinger AF. Neurological adverse events associated with immune checkpoint inhibitors: diagnosis and management. Curr Neurol Neurosci Rep. 2018;18:3.
Brahmer JR. Identifying and addressing the toxicity of checkpoint inhibitors in lung cancer. Clin Adv Hematol Oncol HO. 2016;14:165–7.
Camacho LH. CTLA-4 blockade with ipilimumab: biology, safety, efficacy, and future considerations. Cancer Med. 2015;4:661–72.
Cappelli LC, Shah AA, Bingham CO. Immune-related adverse effects of cancer immunotherapy- implications for rheumatology. Rheum Dis Clin N Am. 2017;43:65–78.
Ciccarese C, Iacovelli R, Bria E, Modena A, Massari F, Brunelli M, et al. The incidence and relative risk of pulmonary toxicity in patients treated with anti-PD1/PD-L1 therapy for solid tumors: a meta-analysis of current studies. Immunotherapy. 2017;9:579–87.
Economopoulou P, Psyrri A. Overview and management of toxicities of immune checkpoint-blocking drugs. Forum Clin Oncol. 2016;7:28–37.
Fecher LA, Agarwala SS, Hodi FS, Weber JS. Ipilimumab and its toxicities: a multidisciplinary approach. Oncologist. 2013;18:733–43.
Feng S, Coward J, McCaffrey E, Coucher J, Kalokerinos P, O’Byrne K. Pembrolizumab-induced encephalopathy: a review of neurological toxicities with immune checkpoint inhibitors. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer. 2017;12:1626–35.
Helissey C, Vicier C, Champiat S. The development of immunotherapy in older adults: new treatments, new toxicities? J Geriatr Oncol. 2016;7:325–33.
Hwang SJE, Carlos G, Chou S, Wakade D, Carlino MS, Fernandez-Penas P. Bullous pemphigoid, an autoantibody-mediated disease, is a novel immune-related adverse event in patients treated with anti-programmed cell death 1 antibodies. Melanoma Res. 2016;26:413–6.
Hansen ED, Wang X, Case AA, Puzanov I, Smith T. Immune checkpoint inhibitor toxicity review for the palliative care clinician. J Pain Symptom Manage. 2018;56:460–72.
Linardou H, Gogas H. Toxicity management of immunotherapy for patients with metastatic melanoma. Ann Transl Med. 2016;4:272.
Lopez AT, Geskin L. A case of Nivolumab-induced bullous pemphigoid: review of dermatologic toxicity associated with programmed cell death Protein-1/programmed death Ligand-1 inhibitors and recommendations for diagnosis and management. Oncologist. 2018;23:1119–26.
Mathias C. Current standard in monitoring of immunotherapy-related toxicity. J Thorac Oncol. 2017;12:S1658–9.
Messmer M, Upreti S, Tarabishy Y, Mazumder N, Chowdhury R, Yarchoan M, et al. Ipilimumab-induced enteritis without colitis: a new challenge. Case Rep Oncol. 2016;9:705–13.
Miranda Poma J, Ostios Garcia L, Villamayor Sanchez J, D’errico G. What do we know about cancer immunotherapy? Long-term survival and immune-related adverse events. Allergol Immunopathol (Madr). 2018;47:303–8.
Nagai H, Muto M. Optimal management of immune-related adverse events resulting from treatment with immune checkpoint inhibitors: a review and update. Int J Clin Oncol. 2018;23:410–20.
Overman MJ, Ernstoff MS, Morse MA. Where we stand with immunotherapy in colorectal cancer: Deficient mismatch repair, proficient mismatch repair, and toxicity management. Am Soc Clin Oncol Educ Book. 2018;38:239–47.
Remon J, Mezquita L, Corral J, Vilariño N, Reguart N. Immune-related adverse events with immune checkpoint inhibitors in thoracic malignancies: focusing on non-small cell lung cancer patients. J Thorac Dis. 2018;10(Suppl 13):S1516–33.
Rudzki JD. Management of adverse events related to checkpoint inhibition therapy. Memo. 2018;11:132–7.
Shah M, Tayar JH, Abdel-Wahab N, Suarez-Almazor ME. Myositis as an adverse event of immune checkpoint blockade for cancer therapy. Semin Arthritis Rheum. 2018;48:736-40.
Simmons D, Lang E. The Most recent oncologic emergency: what emergency physicians need to know about the potential complications of immune checkpoint inhibitors. Cureus. 9. https://doi.org/10.7759/cureus.1774.
Sosa A, Lopez Cadena E, Simon Olive C, Karachaliou N, Rosell R. Clinical assessment of immune-related adverse events. Ther Adv Med Oncol. 2018;10. https://doi.org/10.1177/1758835918764628.
Sznol M, Postow MA, Davies MJ, Pavlick AC, Plimack ER, Shaheen M, et al. Endocrine-related adverse events associated with immune checkpoint blockade and expert insights on their management. Cancer Treat Rev. 2017;58:70–6.
Thompson JA. New NCCN guidelines: recognition and management of immunotherapy-related toxicity. J Natl Compr Cancer Netw JNCCN. 2018;16:594–6.
Touat M, Talmasov D, Ricard D, Psimaras D. Neurological toxicities associated with immune-checkpoint inhibitors. Curr Opin Neurol. 2017;30:659–68.
Bertrand A, Kostine M, Barnetche T, Truchetet M-E, Schaeverbeke T. Immune related adverse events associated with anti-CTLA-4 antibodies: systematic review and meta-analysis. BMC Med. 2015;13:211.
Gupta A, De Felice KM, Loftus EVJ, Khanna S. Systematic review: colitis associated with anti-CTLA-4 therapy. Aliment Pharmacol Ther. 2015;42:406–17.
June CH, Warshauer JT, Bluestone JA. Is autoimmunity the Achilles’ heel of cancer immunotherapy? Nat Med. 2017;23:540.
Forde PM, Chaft JE, Smith KN, Anagnostou V, Cottrell TR, Hellmann MD, et al. Neoadjuvant PD-1 blockade in resectable lung cancer. N Engl J Med. 2018;378:1976–86.
Uppaluri R, Zolkind P, Lin T, Nussenbaum B, Jackson RS, Rich J, et al. Neoadjuvant pembrolizumab in surgically resectable, locally advanced HPV negative head and neck squamous cell carcinoma (HNSCC). J Clin Oncol. 2017;35(15_suppl):6012.
Ferris RL, Gonçalves A, Baxi SS, Martens UM, Gauthier H, Langenberg M, et al. LBA46An open-label, multicohort, phase 1/2 study in patients with virus-associated cancers (CheckMate 358): Safety and efficacy of neoadjuvant nivolumab in squamous cell carcinoma of the head and neck (SCCHN). Ann Oncol. 2017;28(suppl_5):mdx440.041.
Necchi A, Briganti A, Bianchi M, Raggi D, Giannatempo P, Lucianó R, et al. Preoperative pembrolizumab (pembro) before radical cystectomy (RC) for muscle-invasive urothelial bladder carcinoma (MIUC): Interim clinical and biomarker findings from the phase 2 PURE-01 study. J Clin Oncol. 2018;36(15_suppl):4507.
Powles T, Rodriguez-Vida A, Duran I, Crabb SJ, Van Der Heijden MS, Font Pous A, et al. A phase II study investigating the safety and efficacy of neoadjuvant atezolizumab in muscle invasive bladder cancer (ABACUS). J Clin Oncol. 2018;36(15_suppl):4506.
Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, et al. Durvalumab after Chemoradiotherapy in stage III non–small-cell lung cancer. N Engl J Med. 2017;377:1919–29.
FDA grants regular approval to nivolumab for adjuvant treatment of melanoma. U.S. Food & Drug Administration. Updated December 21, 2017. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm590004.htm. Accessed 19 Feb 2019.
FDA Approves Merck’s KEYTRUDA® (pembrolizumab) for the Adjuvant Treatment of Patients with Melanoma with Involvement of Lymph Node(s) Following Complete Resection. Merck. Published February 19, 2019. https://bit.ly/2S89NmN. Accessed 19 Feb 2019.
Krüger GR, Berard CW, DeLellis RA, Graw RG, Yankee RA, Leventhal BG, et al. Graft-versus-host disease. Morphologic variation and differential diagnosis in 8 cases of HL-A matched bone marrow transplantation. Am J Pathol. 1971;63:179–202.
Ferrara JLM, Deeg HJ. Graft-versus-host disease. N Engl J Med. 1991;324:667–74.
Maurice C, Marcus B, Mason W. Guillain-barre syndrome after treatment with dabrafenib for metastatic recurrent melaloma. (P4.232). Neurology. 2015;84:14 Supplement http://n.neurology.org/content/84/14_Supplement/P4.232.abstract.
Garcia CR, Cox JN, Villano JL. Myasthenia gravis and Guillain-barré syndrome adverse events with immune checkpoint inhibitors. J Clin Oncol. 2018;36(5_suppl):37.
Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with Ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23.
Acknowledgements
Not applicable.
Funding
Research support provided by Providence Portland Medical Foundation.
Author information
Authors and Affiliations
Contributions
MAC and RSL collected and interpreted the data and were major contributors to writing the manuscript. RBB, AAP, MCR, MRC, BDC, WJU contributed patient data and contributed to manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted under institutional review board approval at Providence Portland Medical Center, Oregon. Waiver of consent was obtained for retrospective chart review.
Consent for publication
No personal identifying information was included in the manuscript, and therefore no consent was required.
Competing interests
RBB receives research funding from the Oral and Maxillofacial Surgery Foundation, BMS, Abbvie, Safeway Foundation, Providence Portland Medical Center Foundation, receives institutional support from BMS, MedImmune, Prometheus, Merck, and is a member of the speakers bureaus for Merck and BMS, MRC receives institutional research support from Nanobiotix, Jounce, Celldex, Mavupharma and BMS, BDC receives institutional research support from MedImmune/AstraZeneca, BMS, Viralytics, and Gallectin Therapeutics, and serves as consultant to BMS, Eisai, Alligator, and Iovance, WJU has received renumeration from MedImmune and Leidos Biomedical Research, serves on the board of directors for Leidos, and serves on the advisory board for Bionical EMAS, RSL receives institutional research support from Bristol Myers Squibb and Medimmune/AstraZeneca, and serves as a consultant to Merck and Regeneron.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Institutional Case Series. Detailed descriptions of two DIRE cases identified from our institution. (DOCX 23 kb)
Additional file 2:
Supplementary Methods. Boolean search strategy and keywords for titles screen (DOCX 17 kb)
Additional file 3:
Table S1. Table of suspected DIRE cases that could not be confirmed due to lack of supporting information (PDF 23 kb)
Additional file 4:
Clinical Trial AEs Suspicious for DIRE. Descriptions of suspected DIRE cases from clinical trials that could not be confirmed due to lack of supporting information (DOCX 18 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Couey, M.A., Bell, R.B., Patel, A.A. et al. Delayed immune-related events (DIRE) after discontinuation of immunotherapy: diagnostic hazard of autoimmunity at a distance. j. immunotherapy cancer 7, 165 (2019). https://doi.org/10.1186/s40425-019-0645-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40425-019-0645-6