Abstract
Background
Diffuse large B-cell lymphoma (DLBCL) is the most common form of non-Hodgkin lymphoma. Rhabdomyosarcoma, the most common soft tissue sarcoma of childhood. makes up less than 1% of solid malignancies in adults with around 400 new cases each year in the United States. They have not previously been reported concurrently.
Case presentation
A 37 year old woman presented with painful enlarging leg mass. Biopsy of the mass was consistent with embryonal rhabdomyosarcoma. Staging imaging revealed a PET avid anterior mediastinal lymph node. Excisional biopsy of this mass was consistent with diffuse large B-cell lymphoma. Hybridization capture-based next-generation DNA sequencing did not reveal shared somatic tumor mutations. Germline analysis did not show identifiable aberrations of TP53 or other heritable cancer susceptibility genes. She was treated with a personalized chemotherapy regimen combining features of R-CHOP and Children’s Oncology Group ARST 0331.
Conclusions
This case illustrates a unique clinical entity successfully treated with a personalized chemotherapeutic regimen.
Similar content being viewed by others
Background
Rhabdomyosarcoma (RMS), the most common soft tissue sarcoma of childhood, is subdivided into three histopathologically distinct groups: embryonal, alveolar, and pleomorphic [1]. Embryonal RMS (ERMS) is the most common subtype. Alveolar RMS is characterized by the presence of a pathognomonic FOXO1 gene rearrangement with PAX3 or PAX7. Pleomorphic rhabdomyosarcoma is exceedingly rare in children and seen almost exclusively in adults. RMS makes up less than 1% of solid malignancies in adults with around 400 new cases each year in the United States [1, 2]. Therapy for patients with RMS is stratified based upon site-modified TNM staging and the extent of up-front surgical resection and typically involves multi-agent chemotherapy, and some combination of surgery with or without radiation therapy for local control.
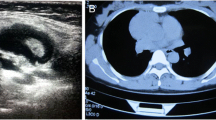
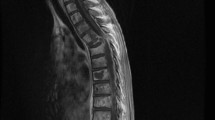
Key imaging and pathology results from the Rhabdomyosarcoma and Diffuse large B-cell lymphoma. a Axial view of the left thigh rhabdomyosarcoma demonstrating the lesion was FDG-avid on PET scan. b Morphology of rhabdomyosarcoma showing spindle cells in intersecting fascicles. (H&E, 200x) c Immunohistochemical stain for Desmin showing diffuse positivity supporting the diagnosis of rhabdomyosarcoma. d Axial view of the mediastinal diffuse large B-cell lymphoma demonstrating FDG-avidity on PET scan. e Morphology of lymph node showing involvement by diffuse large B-cell lymphoma. (H&E, 200x) f Higher power image of the lymphoma showing large lymphoid cells in sheets. (H&E, 400x)
While usually sporadic in appearance, RMS has been seen in patients with cancer-predisposition syndromes such as Li-Fraumeni syndrome, neurofibromatosis type I, Costello syndrome, Noonan syndrome, and Beckwith-Wiedemann syndrome [3]. There is also an increased risk of RMS in children with constitutional DICER1 mutations [4]. Additionally, due to multimodal therapy with alkylating agents and radiation based therapy, these patients are also at risk of developing secondary malignancies. The last Childhood Cancer Survivor Study reported that 20% of patients with secondary malignancies were survivors of soft tissue sarcomas [5].
Diffuse large B-cell lymphoma (DLBCL) is the most common form of non-Hodgkin lymphoma. Heterogeneous in presentation and molecular pathology, it is characterized by aberrant proliferation of mature B-cells in nodal or extranodal sites [6]. Therapy is based on extent of disease and presence or absence of ‘B symptoms’ and includes a multi-agent chemotherapy with targeted therapy including anti-CD20 antibodies. Genome wide association studies have shown independent single-nucleotide polymorphisms (SNPs) correlate with an increased risk of DLBCL [7, 8]. We report a woman with no significant prior medical history who was diagnosed with simultaneous ERMS and DLBCL. To our knowledge, the synchronous occurrence of these two tumors has not previously been reported in the medical literature. Next generation sequencing did not reveal a pervasive somatic or germline mutation that might link these tumors. Testing for a germline mutation consistent with a cancer predisposition syndrome failed to reveal identifiable abnormality of TP53 or any of the other genes associated with an increased risk of soft tissue sarcomas, in general, or rhabdomyosarcoma in particular.
Case presentation
A 37-year old woman with no pertinent past medical history presented with a firm non-tender lump in her left proximal thigh. The mass was mildly painful and enlarged over one year. This patient had a family tree consisting of 2 generations above and 1 generation below compiled during her visit with the Clinical Genetics team. The family cancer history was notable for a paternal grandfather with prostate cancer at age 80, a maternal uncle with prostate cancer at age 72, and a maternal grandmother with melanoma at age 60. There were no cancers at an early age, sarcomas, leukemias, lymphomas, nor malignancies pathognomonic for inherited predisposition syndromes.). Approximately one month prior to diagnosis, she was hospitalized for management of pneumonia; imaging studies were not performed and she was treated with antibiotics and a weeklong pulse of glucocorticosteroids. Following ultrasound-guided fine needle aspiration showing a spindle cell neoplasm, a MRI demonstrated an enhancing intra-muscular mass measuring 4.9 cm in maximal diameter. She underwent en bloc resection of the mass with pathology consistent with high-grade spindle cell rhabdomyosarcoma with high mitotic rate, negative margins, and negative local lymph nodes. During staging imaging, she was found to have a hypermetabolic 1.4 cm left anterior mediastinal perivascular thoracic lymph node on baseline PET scan (SUV = 6.6). As the presence of a distant metastasis would increase her stage from Stage 2 to Stage 4, with a resultant significant change in both her therapy and prognosis, she underwent excision of this mediastinal mass which revealed a distinct primary tumor, DLBCL. Given the simultaneous occurrence of two rare and pathophysiologically distinct malignancies, each tumor was sequenced using MSK-IMPACT, a hybridization capture-based next-generation DNA sequencing assay of exons of 410 genes recurrently mutated in solid tumors [9] (Fig. 1). Her rhabdomyosarcoma was negative for FOXO1 gene rearrangement and found to have a somatic alteration in NF1. Her DLBCL had multiple somatic mutations including ATM, B2M, FAT1, HGF, MYCN, PIM1, various mutations in the same allele of exon 2 of SOCS1, and SOX17 (Table 1). MSK-IMPACT testing did not reveal any germline mutations in the targeted gene panel. No copy number alterations were identified. Although the ERMS was of sufficient tumor purity, the DLBCL had low tumor content. Mean overall coverage (sequencing depth) in the ERMS, DLBCL, and germline samples were 606X, 623X, and 261X, respectively. Given the consequences of missing a Li-Fraumeni syndrome diagnosis, additional testing was performed on the TP53 coding sequence (exons 2–11), including bidirectional splice junction sequencing, as well as deletion and duplication analysis to evaluate for larger chromosomal rearrangements were negative for any germline aberrations.
Based on the absence of distant metastases and the favorable histology of her tumor, her RMS was classified as “low-risk” (Stage 2, Group I) and her mediastinal DLBCL was classified as Stage 1. Consequently, she was treated with an individualized regimen that incorporated the basic design of the Children’s Oncology Group (COG) low-risk rhabdomyosarcoma study, ARST 0331, with R-CHOP. The low risk arm of ARST 0331 is composed of 24 weeks of chemotherapy with vincristine, dactinomycin, and cyclophosphamide plus/minus radiation. R-CHOP consists of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone. The patients individualized regimen is detailed in Table 2. Because severe neuropathy in adults tends to limit the tolerability of intensively-dosed vincristine as typically given on pediatric chemotherapeutic regimens, her individualized regimen was modified to replace 6 vincristine doses with 2 additional cyclophosphamide doses. Four doses of dactinomycin were substituted with doxorubicin to achieve the desired anthracycline dose for R-CHOP. She received pulses of prednisone every 5 days and 6 total doses of Rituximab. Her treatment course was complicated by severe constipation and jaw pain secondary to vincristine, granulocyte colony stimulating factor associated bone pain, and mild mucositis during her expected periods of neutropenia. These toxicities did not lead to any delays in treatment. She is currently more than a year and a half off therapy in complete remission from both primary cancers, undergoing close monitoring for both malignancies.
Discussion and Conclusions
We report an adult woman with no prior medical history nor familial cancer history who was diagnosed with synchronous RMS and DLBCL. Genomic analyses did not identify unifying somatic nor predisposing germline mutations. Although there is a prior report of a 64 year old man with concurrent RMS and Hodgkin lymphoma, to our knowledge this is the first case of RMS and any non-Hodgkin lymphoma [10].
Two distinct primary tumors without prior chemotherapy or radiation exposures or known underlying cancer predisposition is a rare entity that is poorly described. The simultaneous existence of two primary tumors presents a major therapeutic challenge, requiring the tailoring of a customized regimen that provides adequate therapy directed at each tumor without incurring intolerable toxicities. Cyclophosphamide, doxorubicin, vincristine, and prednisone are active against both RMS and DLBCL [11, 12]. It is likely that this overlapping chemotherapeutic sensitivity allowed the patient to tolerate the combined regimens of the COG RMS protocol with standard DLBCL therapy, R-CHOP.
The patient received a week pulse of steroids for pneumonia one month before she was diagnosed with RMS. This may have partially treated her DLBCL, causing her mediastinal mass to be less extensive than if untreated. A week-long steroid pre-phase is routinely utilized in the treatment of elderly patients with low performance status as a means of reducing initial treatment toxicities [13].
Despite genomic analyses, no unifying molecular aberration was identified in both of our patient’s two cancers. Archer et al. argued that the SEER-9 database provides population based evidence that subgroups of patients with rhabdomyosarcoma have constitutional cancer predisposition [14]. At this point, further studies are required to delineate whether our patient had the unfortunate coincidence of two unrelated synchronous tumors or indeed represents part of a yet to be fully characterized cohort of patients with constitutional or inherited risk for rhabdomyosarcoma and other cancers.
Abbreviations
- COG:
-
Children’s oncology group
- DLBCL:
-
Diffuse large B-cell lymphoma
- ERMS:
-
Embryonal RMS
- RMS:
-
Rhabdomyosarcoma
- SNPs:
-
single-nucleotide polymorphisms
References
Ruiz-Mesa C, Goldberg JM, Coronado Munoz AJ, Dumont SN, Trent JC. Rhabdomyosarcoma in adults: new perspectives on therapy. Curr Treat Options Oncol. 2015;16:27.
Sun X, Guo W, Shen JK, Mankin HJ, Hornicek FJ, Duan Z. Rhabdomyosarcoma: advances in molecular and cellular biology. Sarcoma. 2015;2015:232010.
Li FP, Fraumeni Jr JF. Rhabdomyosarcoma in children: epidemiologic study and identification of a familial cancer syndrome. J Natl Cancer Inst. 1969;43:1365–73.
Doros L, Yang J, Dehner L, Rossi CT, Skiver K, Jarzembowski JA, Messinger Y, Schultz KA, Williams G, Andre N, Hill DA. DICER1 mutations in embryonal rhabdomyosarcomas from children with and without familial PPB-tumor predisposition syndrome. Pediatr Blood Cancer. 2012;59:558–60.
Meadows AT, Friedman DL, Neglia JP, Mertens AC, Donaldson SS, Stovall M, Hammond S, Yasui Y, Inskip PD. Second neoplasms in survivors of childhood cancer: findings from the childhood cancer survivor study cohort. J Clin Oncol. 2009;27:2356–62.
Vitolo U, Seymour JF, Martelli M, Illerhaus G, Illidge T, Zucca E, Campo E, Ladetto M, Committee EG: Extranodal diffuse large B-cell lymphoma (DLBCL) and primary mediastinal B-cell lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v91-v102.
Cerhan JR, Berndt SI, Vijai J, Ghesquieres H, McKay J, Wang SS, Wang Z, Yeager M, Conde L, de Bakker PI, et al. Genome-wide association study identifies multiple susceptibility loci for diffuse large B cell lymphoma. Nat Genet. 2014;46:1233–8.
Bassig BA, Cerhan JR, Au WY, Kim HN, Sangrajrang S, Hu W, Tse J, Berndt S, Zheng T, Zhang H, et al. Genetic susceptibility to diffuse large B-cell lymphoma in a pooled study of three Eastern Asian populations. Eur J Haematol. 2015;95:442–8.
Cheng DT, Mitchell TN, Zehir A, Shah RH, Benayed R, Syed A, Chandramohan R, Liu ZY, Won HH, Scott SN, et al. Memorial Sloan Kettering-integrated mutation profiling of actionable cancer targets (MSK-IMPACT): a hybridization capture-based next-generation sequencing clinical assay for solid tumor molecular oncology. J Mol Diagn. 2015;17:251–64.
Dergan J, Sirsi S, Asarian A, Guevara E, Xiao P. Rhabdomyosarcoma masquerading as lymphadenopathy in a patient with newly diagnosed Hodgkin’s lymphoma. World J Surg Oncol. 2016;14:101.
Arndt CA, Nascimento AG, Schroeder G, Schomberg PJ, Neglia JP, Sencer SF, Silberman TL, Moertel CL, Tillisch JK, Miser JS. Treatment of intermediate risk rhabdomyosarcoma and undifferentiated sarcoma with alternating cycles of vincristine/doxorubicin/cyclophosphamide and etoposide/ifosfamide. Eur J Cancer. 1998;34:1224–9.
Kubuschok B, Held G, Pfreundschuh M. Management of diffuse large B-cell lymphoma (DLBCL). Cancer Treat Res. 2015;165:271–88.
Pfreundschuh M. How I treat elderly patients with diffuse large B-cell lymphoma. Blood. 2010;116:5103–10.
Archer NM, Amorim RP, Naves R, Hettmer S, Diller LR, Ribeiro KB, Rodriguez-1rhabdomyosarcoma: population-based evidence for a cancer predisposition syndrome? Pediatr Blood Cancer. 2016;63:196–201.
Acknowledgements
The authors would like to thank Dr. Narasimhan Agaram for providing the pathologic images shown in Figure 1.
Funding
This work was supported in part by the National Cancer Institute (NCI) Grant NIH T32 CA062948, the St. Baldricks Foundation Scholar who fund the salary of MM during the collection of data for this analysis and writing of the manuscript. All authors are partially funded by the MSK Cancer Center Support Grant/Core Grant P30 CA008748.
Author contributions
MM and MO had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. MM, MO, and LW were responsible for study concept and design. MM, MO, and LW drafted the manuscript. All authors helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare they have no competing interests.
Consent for publication
The patient and family gave consent to publish this form and signed our institutional form of consent.
Ethics approval and consent to participate
The patient and family gave assent and informed consent to all parts of this study and informed consent for publication.
Data deposition and access
Data Sharing not applicable to this article as no datasets were generated or analyzed during the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. D. Mathias and M.V. Ortiz are co-first authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mathias, M.D., Ortiz, M.V., Magnan, H. et al. A case report of concurrent embryonal rhabdomyosarcoma and diffuse large B-cell lymphoma in an adult without identifiable cancer predisposition. Biomark Res 5, 7 (2017). https://doi.org/10.1186/s40364-017-0086-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40364-017-0086-7