Abstract
Background
Experiences of potentially morally injurious events (PMIEs) have been found to negatively impact the mental health of US personnel/veterans, yet little is known about the effect of PMIEs on the mental health of the UK Armed Forces (AF). This cross-sectional study aimed to examine the association between PMIEs and the mental health outcomes of UK AF veterans.
Method
Assessments of PMIE exposure and self-report measures of common mental disorders were administered using an online questionnaire to 204 UK veterans. Subjects were classified as having experienced a morally injurious event (n = 66), a non-morally injurious traumatic event (n = 57), a ‘mixed’ event (n = 31), or no event (n = 50).
Results
Potentially morally injurious experiences were associated with adverse mental health outcomes, including likely anxiety disorders and suicidal ideation, compared to those who reported no event exposure. The likelihood of meeting criteria for probable PTSD was greatest in those who had experienced a non-morally injurious trauma. No statistically significant association between alcohol misuse and experiencing a PMIE or traumatic event was observed.
Conclusions
The results provide preliminary evidence that potentially morally injurious experiences are associated with adverse mental health outcomes in UK AF veterans. Further work is needed to better understand the interplay between morally injurious events and threat-based trauma in order to design effective pathways for prevention and intervention for people exposed to highly challenging events.
Similar content being viewed by others
Background
Military service can involve exposure to potentially morally injurious events (PMIEs), which are experiences that violate one’s moral or ethical code [1, 2]. PMIEs are understood to generally include acts of commission, omission or betrayal by trusted others [3]. More recent evidence suggests moral injury can follow ‘mixed’ events which combine ethically challenging and more routine traumatic events, involving threatened or actual death, serious injury or sexual assault, which are otherwise consistent with criterion A for DSM-5 posttraumatic stress disorder (PTSD) [2, 4,5,6]. PMIEs in a military context are not uncommon; for example, 24% of US Marines reported engaging in at least one morally transgressive act and 28% experienced a betrayal event during deployment [7].
While moral injury is not currently considered a mental disorder, experiences of PMIEs can lead to negative attributions about the self (e.g. ‘I am an awful person’) and others, as well as profound feelings of guilt, anger, worthlessness and shame [8]. This in turn can lead to the development of formal psychological difficulties. Moral injury has been found to be significantly associated with PTSD, depression and suicidal ideation [9, 10]. Furthermore, patients who seek treatment for PTSD often report PMIEs as the most distressing event for them [5].
The majority of evidence relating to the impact of moral injury on wellbeing stems from studies carried out in US military or veteran populations [11, 12]. However, US and UK militaries often differ in terms of demographics (e.g. US troops are frequently younger, larger proportion of National Guards/reserves [13]), have distinct deployment experiences (e.g. US troops often deploy for longer) and there are differences in the rules of engagement which may affect exposure to PMIEs. Similarly, once personnel have left service, veterans in the UK and US may face a number of distinct challenges, including different experiences in accessing healthcare (e.g. National Health Service (NHS) versus Department of Veterans Affairs). Qualitative studies of UK veterans have shown that they experience intense psychological distress following a PMIE, which can significantly disrupt their daily functioning [2, 14]. However, the association between PMIE exposure and mental health outcomes in a UK veteran population has not yet been explored. Previous US military and veteran studies have shown a significant association between experiences of moral injury and likely mental disorders, including PTSD, anxiety and depression [3, 15, 16]. Whether the same occurs in a UK context is unknown.
To address this gap, the primary aim of this study was to examine the association between potentially morally injurious experiences and the mental health outcomes of UK Armed Forces (AF) veterans. We hypothesised that those exposed to morally injurious events or traumatic events would be more likely to report poor mental health outcomes, including PTSD, alcohol misuse, suicidality, depression and anxiety, than those who did not report exposure to a challenging event during the course of their military service.
Methods
This study received ethical approval from King’s College London Research Ethics Committee (RESCM-17/18-4002).
Participants
Between November 2018 and April 2019, eligible veterans (defined as serving personnel who had left the UK AF) were recruited to the study. Eligibility required veterans to be aged 18 years and above, English speaking, and to be willing to self-report their experiences during military service. No limitations on eligibility according to demographic characteristics (e.g. gender, age, rank, years of service) were imposed. Further, we did not restrict participation by deployment location or AF service branch.
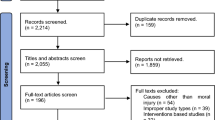
We used opportunity sampling and recruited participants by circulation of the study information posted on social media, online platforms, veteran affiliated charities, veteran specific newsletters, and military-affiliated magazines. The sampling method of snowballing was also utilised with participants asked to share study information with other potentially eligible individuals. Individuals were screened for eligibility in line with study inclusion/exclusion criteria using self-report questions, with written informed consent obtained.
Assessments
The online questionnaire was distributed via the internet using a secure server. The anonymity of subjects was protected as they were not asked to provide any personally identifying information in order to participate (e.g. name, home address). Prior to distribution, the questionnaire was piloted with UK AF veterans (n = 4, not included in the final sample) with questions and formatting adjusted accordingly. Basic demographic information (e.g. age, service branch, sex, etc.) was collected from participants.
To determine whether a participant had experienced a moral injury, all participants were asked whether or not they had experienced a challenging event during military service (i.e. “during your military service, did you ever experience an event that was a serious challenge to your sense of who you are, your sense of the world, or your sense of right and wrong?”). Veterans were asked to write a brief description of the event which was later classified by two independent researchers as a moral injury, a non-morally injurious trauma, or a ‘mixed’ event. This classification process is described in-depth by Williamson et al., (2020). Any UK AF veterans who self-reported having not experienced a challenging military event were classified as ‘no event’. The inclusion of veterans who did and did not self-report having exposure to events which challenged their ethical or moral code allowed for comparisons between groups.
Psychological assessment measures
Probable PTSD was assessed via the PCL-5 (cut off score = 33) [17], probable depression via the PHQ-9 (cut off score = 15) [18], probable anxiety disorder via the GAD-7 (cut off score = 8) [19], probable alcohol misuse via the AUDIT (cut off score = 16) [20], and probable suicidal ideation via the SBQ-R (cut off score = 7) [21]. Combat exposure was assessed via the Combat Exposure Scale [22] with a score between 17 and 41 indicative of moderate-high combat exposure. All measures have been widely used in military samples and found to have good reliability and validity [3, 23,24,25,26].
Data analysis
Descriptive analyses were conducted to provide an overview of the sample characteristics (Table 1). Prior to the main analysis, data were screened for inaccuracies in data entry, missing values and the presence of outliers. Where more than 50% of data was missing, the participant was excluded from the analysis. This resulted in three subjects being excluded from the analysis. Consistent with previous studies [23], for the remaining participants, we replaced missing values in the psychometric scales with the lowest possible value if 25% or fewer items were missing. If more than 25% of items were missing, the response was counted as missing. Common Mental Disorders (CMD) reflects participants who met case criteria on the GAD, PHQ-9 and/or PCL-5. Chi2 and Fishers’ Exact tests (where the sample size was limited) were used to determine whether statistically significant differences between groups existed, with p values < 0.05 used to indicate statistical significance. Where appropriate, odds ratios (OR) or adjusted odds ratios (AOR) and 95% confidence intervals (CI) were calculated using logistic regression. AOR were adjusted for sex and age. The reference category was reporting no exposure to a challenging event during military service. Effect sizes were considered statistically significant if the 95% CI did not include 1.
Results
Demographic information
Participant demographic information can be found in Tables 1 and 2. Overall, the 204 veterans had served between 18 months to 42 years in the AF (mean = 17.3 years, SD 9.61). The majority were White British (n = 200, 98.2%) and 88.6% were male (n = 177). In terms of event exposure, 66 (33.4%) veterans self-reported exposure to an event that was classified as morally injurious, 57 (27.9%;) veterans reported exposure to non-morally injurious trauma (e.g. being under enemy fire, exposure to an explosion), 31 (15.2%) veterans reported a ‘mixed’ event, and 50 (24.5%) veterans did not report exposure to a challenging event during military service. As seen in Table 1, a substantial proportion of veterans across the sample met case criteria for probable PTSD, alcohol misuse, depression and anxiety disorders. High rates of suicidal ideation were also found. It should be noted that these are not prevalence rates or representative of mental disorder prevalence in the AF and may reflect the purposive sampling strategy used.
No statistically significant differences were found between exposure groups in terms of socio-demographic or military-related characteristics (see Tables 1 and 2). Many veterans across the sample reported a high level of education attainment and a considerable proportion were officers or non-commissioned officers (n = 123, 57.7%). No significant differences were found between deployment location, extent of combat exposure or number of deployments and exposure to morally injurious, traumatic or ‘mixed’ events (Table 2).
Relationship between type of event exposure and mental health
Only adjusted analysis will be discussed. Exposure to specific types of challenging events in military service was found to be associated with a range of adverse mental health outcomes. Compared to veterans who did not report exposure to a challenging event during military service, veterans who experienced a morally injurious event (AOR 3.98; 95% CI 1.75–9.05) were significantly more likely to meet case criteria for probable PTSD (see Table 3), anxiety (AOR 3.91; 95% CI 1.69–9.04) and suicidal ideation (AOR 2.60; 95% CI 1.20–5.66) compared to those who did not report a challenging event during military service. Compared to those who reported no challenging event during military service, veterans who were classified as having experienced a ‘mixed’ event were also more likely to meet criteria for likely PTSD (AOR 5.21; 95% CI 1.93–14.06; Table 3), depression (AOR 3.36; 95% CI 1.25–9.01), anxiety (AOR 6.75; 95% CI 2.44–18.72), and suicidal ideation (AOR 3.89; 95% CI 1.48–10.21). Veterans who reported exposure to a traumatic, non-morally injurious event were more likely to meet case criteria for probable PTSD (AOR 6.67; 95% CI 2.77–16.07), depression (AOR 3.38; 95% CI 1.41–8.05), anxiety (AOR 6.29; 95% CI 2.59–15.25) and suicidal ideation (AOR 3.33; 95% CI 1.47–7.58) compared to those who did not report a challenging event during military service.
Notably, veterans who reported a moral injurious, a ‘mixed’ or a traumatic, non-morally injurious event were not more likely to report alcohol misuse compared to those who reported no event exposure (see Table 3). Moreover, the likelihood of meeting case criteria for a probable anxiety disorder and suicidal ideation was greatest in the ‘mixed’ group, compared to those who reported morally injurious or non-morally injurious traumatic events (Table 3). The likelihood of meeting case criteria for probable PTSD and depression was greatest in those who had experienced a non-morally injurious trauma. Nonetheless, overlapping confidence intervals indicate these differences between exposure groups are not statistically significant but may indicate an upward trend.
Discussion
This study aimed to investigate the impact of exposure to morally injurious events on the mental health of UK AF veterans. Three key findings were observed. First, experiences of moral injury were associated with adverse mental health outcomes, with veterans exposed to ‘mixed’ events having a greater likelihood of meeting criteria for probable anxiety and suicidal ideation. Secondly, the likelihood of meeting criteria for probable PTSD was greatest in those who had experienced a non-morally injurious trauma, although overlapping confidence intervals suggest these differences are not statistically significant. Thirdly, there was no statistically significant association between alcohol misuse and experiencing a PMIE or traumatic event.
The results of this study indicate that, as with incidents meeting the DSM-5 definition of a traumatic event [4], experiences of moral injury, trauma and ‘mixed’ events are significantly associated with poor mental health outcomes in the UK AF. The results are consistent with previous studies in the US militaries where experiences of morally injurious events are significantly associated with adverse mental health outcomes, including PTSD, anxiety and suicidal ideation [11, 12]. A meta-analysis highlighted the lack of non-US research into the impact of moral injury on mental health [9]. The present study addresses this gap by providing preliminary evidence of the detrimental effect of traumatic events, including PMIEs, on the mental health of UK veterans.
It is notable that the likelihood of meeting case criteria for probable anxiety and suicidal ideation was greatest in the ‘mixed’ group compared to those who reported moral injurious or non-morally injurious traumatic events. While this difference was not statistically significant (potentially due to the small sample size), this finding could indicate that those who experience events which are both traumatic and morally injurious may be at particular risk of suicidality which is consistent with previous qualitative studies [2, 5]. It is possible that the combined impact of both a traumatic and PMIE may act as a ‘double stressor’. These events could potentially complicate treatment as clinicians may be more likely to focus on the traumatic aspects of the event—rather than the morally injurious features—which are well addressed by conventional models of PTSD care. Therefore, these results tentatively contribute towards the conceptual clarification of moral injury in a UK context as well as having a practical application in that it is clear that clinicians taking a trauma history from veterans should specifically ask about potentially morally injurious aspects related to traumatic incidents. Where ‘mixed’ events are identified, our results suggest that particular attention should be paid to risk assessment for suicidality. As suggested by previous studies [27], standard exposure-based treatments for PTSD may not adequately address the needs of those who are suffering after potentially morally injurious or ‘mixed’ events. Other approaches, such as Adaptive Disclosure or Acceptance and Commitment Therapy [28, 29], could potentially be more suitable in such cases to address patient’s maladaptive psychological responses of guilt and shame.
This study also found that the likelihood of meeting criteria for probable PTSD was somewhat greater in those who had experienced a non-morally injurious traumatic event. However, this finding was not significantly different to the lower rates found after ‘mixed’ and morally injurious incidents. Although, this differential profile of distress is consistent with previous research that participants who experience traumatic events which elicit fear (rather than moral crisis) report higher levels of hyperarousal/hypervigilance symptoms relative to those who report non-life threat traumas [30]. It is possible that the lack of statistically significant differences between PMIE and trauma exposed groups could reflect the opportunity sampling approach used, in that individuals who took part in the study may have been especially motivated to share their experience, causing a ceiling effect.
Interestingly, this study did not find an association between experiences of moral injury and/or trauma and alcohol misuse, which is inconsistent with some previous studies of war-related PMIEs [31]. This is a surprising finding as alcohol misuse has been found to be an avoidant coping strategy often used post-trauma [32]. However, it may be that heavier drinking is an endemic problem for the AF and such behaviours may mask drinking as an avoidance coping strategy. Future large-scale studies are needed to further examine the prevalence of mental health difficulties following PMIEs in UK veterans to better understand their occurrence, with direct comparisons made between the UK and other AF to advance our understanding of the psychological impact of moral injury.
This study has several strengths and weaknesses. Among the strengths is that participation was anonymous and confidential, which may have facilitated disclosure of veteran experiences and associated distress. That no veterans were excluded on the basis of demographic or military characteristics (e.g. AF branch, length of service or deployment location, etc.) is also a strength. Nonetheless, the cross-sectional design of this study prevents causal inferences and the convenience sampling strategy used may reduce the generalisability of the present findings. Another limitation of the study is that the details of military service and trauma exposure provided by subjects were not verified from official records, so we cannot be sure of their accuracy. The sample also was not representative of UK AF given the high percentage of officers and non-commissioned officers (NCOs) who took part in the study. There may be biases associated with a population that responds to advertisements and participant invitations in social media and military charities rather than by random selection. Additionally, the assignment of participants to moral injury, ‘mixed’ or trauma groups was determined by independent researcher ratings and future studies should use a screening measure once a validated tool for detecting moral injury is developed for use in the UK AF. Efforts are currently underway, both in the UK and internationally [33, 34], to develop a validated measure of moral injury exposure that may improve not only improve the identification of those suffering following moral injury but reduce bias in future studies. Finally, the presence of probable mental health problems was assessed via self-report questionnaire rather than clinical interview which is considered the gold-standard for mental disorder assessment.
Conclusions
The current study provides the first preliminary evidence that experiences of moral injury are associated with adverse mental health outcomes in UK AF veterans. The findings also expand on the limited available research into the specific psychological impact of experiencing ‘mixed’ events that are simultaneously morally injurious and traumatic/threatening – a distinction that has not been clearly made before in the existing literature. That ‘mixed’ events may be associated with particular mental health difficulties, such as anxiety and suicidal ideation, stresses the importance of comprehensive trauma history taking in clinical settings. Finally, this research underscores the pressing need for a validated measure for moral injury appropriate for the UK AF to not only better understand the impact of moral injury on veteran wellbeing, but also to ensure that appropriate treatment can be provided to those identified as suffering post-trauma.
Availability of data and materials
No additional data are available.
Abbreviations
- PTSD:
-
Posttraumatic stress disorder
- PMIE:
-
Potentially morally injurious events
- AF:
-
Armed Forces
- NHS:
-
National Health Service
References
Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695–706.
Williamson V, Murphy D, Stevelink SAM, Allen S, Jones E, Greenberg N. The impact of trauma exposure and moral injury on UK military veterans: a qualitative study. Eur J Psychotraumatol. 2020;11(1):1704554.
Bryan CJ, Bryan AO, Anestis MD, Anestis JC, Green BA, Etienne N, et al. Measuring moral injury: psychometric properties of the moral injury events scale in two military samples. Assessment. 2016;23(5):557–70. https://doi.org/10.1177/1073191115590855.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). American Journal of Psychiatry. 2013. 991 p
Stein NRT, Mills MA, Arditte K, Mendoza C, Borah AM, et al. A Scheme for categorizing traumatic military events. Behav Modif. 2012;36(6):787–807.
Jones E. Moral injury in a context of trauma. 2020. https://icd.who.int/browse11/l-m/en
Jordan AH, Eisen E, Bolton E, Nash WP, Litz BT. Distinguishing war-related PTSD resulting from perpetration-and betrayal-based morally injurious events. Psychol Trauma Theory Res Pract Policy. 2017;9(6):627–34.
Farnsworth JK, Drescher KD, Evans W, Walser RD. A functional approach to understanding and treating military-related moral injury. J Context Behav Sci. 2017;6:391–7.
Williamson V, Stevelink SAM, Greenberg N. Occupational moral injury and mental health: systematic review and meta-analysis. Br J Psychiatry. 2018;212(06):339–46.
Battles AR, Bravo AJ, Kelley ML, White TD, Braitman AL, Hamrick HC. Moral injury and PTSD as mediators of the associations between morally injurious experiences and mental health and substance use. Traumatology (Tallahass Fla). 2018;24(4):246–54.
Griffin BJ, Purcell N, Burkman K, Litz BT, Bryan CJ, Schmitz M, et al. Moral injury: an integrative review. J Trauma Stress. 2019. https://doi.org/10.1002/jts.22362.
Frankfurt S, Frazier P. A review of research on moral injury in combat veterans. Mil Psychol. 2016;28(5):318–30. https://doi.org/10.1037/mil0000132.
Sundin J, Herrell RK, Hoge CW, Fear NT, Adler AB, Greenberg N, et al. Mental health outcomes in US and UK military personnel returning from Iraq. Br J Psychiatry. 2014. http://bjp.rcpsych.org/content/early/2014/01/02/bjp.bp.113.129569.short
Williamson V, Greenberg N, Murphy D. Impact of moral injury on the lives of UK military veterans: a pilot study. J R Army Med Corps. 2019
Bryan AO, Bryan CJ, Morrow CE, Etienne N, Ray-Sannerud B. Moral injury, suicidal ideation, and suicide attempts in a military sample. Traumatology (Tallahass Fla). 2014;20(3):154–60. https://doi.org/10.1037/h0099852.
Currier JM, Holland JM, Malott J. Moral injury, meaning making, and mental health in returning veterans. J Clin Psychol. 2015;71(3):229–40. https://doi.org/10.1002/jclp.22134.
Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–98. https://doi.org/10.1002/jts.22059.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Spitzer, Kroenke, Williams L. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test guidelines for use in primary care. In: World Health Organization. 2001.
Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The suicidal behaviors questionnaire-revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment. 2001;8(4):443–54. https://doi.org/10.1177/107319110100800409.
Keane T, Zimering R, Caddell J. A behavioral formulation of posttraumatic stress disorder in Vietnam veterans. Behav Ther. 1985;8:9–12.
Fear NT, Jones M, Murphy D, Hull L, Iversen AC, Coker B, et al. What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. Lancet. 2010;375(9728):1783–97.
Hotopf M, Hull L, Fear NT, Browne T, Horn O, Iversen A, et al. The health of UK military personnel who deployed to the 2003 Iraq war: a cohort study. Lancet. 2006;367(9524):1731–41.
Iversen AC, Fear NT, Simonoff E, Hull L, Horn O, Greenberg N, et al. Influence of childhood adversity on health among male UK military personnel. Br J Psychiatry. 2007
Stevelink SAM, Jones M, Hull L, Pernet D, MacCrimmon S, Goodwin L, et al. Mental health outcomes at the end of the British involvement in the Iraq and Afghanistan conflicts: a cohort study. Br J Psychiatry. 2018;213(6):690–7.
Maguen S, Burkman K. Combat-related killing: expanding evidence-based treatments for PTSD. Cogn Behav Pract. 2013;20(4):476–9.
Steinmetz S, Gray M. Treatment for distress associated with accurate appraisals of self-blame for moral transgressions. Curr Psychiatry Rev. 2015;11(3):207–19.
Litz BT, Lebowitz L, Gray MJ, Nash WP. Adaptive disclosure : a new treatment for military trauma, loss, and moral injury. New York: The Guildford Press; 2017.
Litz BT, Contractor AA, Rhodes C, Dondanville KA, Jordan AH, Resick PA, et al. Distinct trauma types in military service members seeking treatment for posttraumatic stress disorder. J Trauma Stress. 2018;31(2):286–95. https://doi.org/10.1002/jts.22276.
Robbins AT. Association Between Combat, Morally Injurious Experiences, Spiritual Injury, and Alcohol Use Among Active Duty Military Personnel and Veterans Recommended Citation. 2016.
Lee J, Possemato K, Ouimette PC. Longitudinal changes in combat-related posttraumatic stress disorder among operation enduring freedom/operation iraqi freedom/operation new dawn veterans with hazardous alcohol use. J Nerv Ment Dis. 2017;205(10):805–8.
Yeterian J, Berke D, Carney J, McIntyre-Smith A, St. Cyr K, King L, et al. Development of a Moral Injury Outcomes Scale: Rationale, Study Design, and Preliminary Findings. J Trauma Stress.
Williamson V, Murphy D, Stevelink SA, Jones E, Greenberg N. Experiences of moral injury in UK military veterans. London; 2020
Acknowledgements
Not applicable.
Funding
This research was funded by the Forces in Mind Trust. This paper represents independent research part-funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London (SAMS). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. The funders did not have a role in the study design, the collection, analysis or interpretation of data, and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Authors (VW, DM, SAMS, EJ, NG) contributed towards the design of the study. Authors (VW, SA, SAMS) collected and analysed the data. Author (VW) drafted the manuscript. All authors (VW, DM, SAMS, SA, EJ, NG) contributed towards reviewing the manuscript and approved the manuscript before submission. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
King’s College London Research Ethics Committee (RESCM-17/18-4002). Written consent was obtained for participation.
Consent for publication
Not applicable.
Competing interests
Authors had financial support from a Forces in Mind Trust grant (FiMT17/0920E) for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Williamson, V., Murphy, D., Stevelink, S.A.M. et al. The impact of moral injury on the wellbeing of UK military veterans. BMC Psychol 9, 73 (2021). https://doi.org/10.1186/s40359-021-00578-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40359-021-00578-7