Abstract
Background
Lithium is well recognized as the first-line maintenance treatment for bipolar disorder (BD). However, besides therapeutic benefits attributed to lithium therapy, the associated side effects including endocrinological and renal disorders constitute important parameters in prescribing patterns and patient adherence. The objectives of this study is to (i) determine whether long-term lithium therapy is associated with a decrease in renal function, hyperparathyroidism and hypercalcemia and (ii) identify risk factors for lithium-induced chronic kidney disease (CKD).
Methods
We conducted a single-centered cohort study of adult patients (≥ 18 years) treated with lithium, who were enrolled at Rennes University Hospital in France between January 1, 2018 and June 1, 2020. Required data were collected from the patient’s medical records: demographics characteristics (age, sex, body mass index), biologic parameters (GFR, lithium blood level, PTH and calcium), medical comorbidities (hypertension and diabetes), lithium treatment duration and dosage, and length of hospitalization.
Results
A total of 248 patients were included (mean age: 60.2 ± 16.5 years). Duration of lithium treatment correlated with (i) deterioration of renal function estimated at − 2.9 mL/min/year (p < 0.0001) and (ii) the development of hyperparathyroidism (p < 0.01) and hypercalcemia (p < 0.01). We also noted that patients with lithium blood level > 0.8 mEq/mL had significantly lower GFR than patients with lithium blood level < 0.8 mEq/mL (61.8 mL/min versus 77.6 mL/min, respectively, p = 0.0134). Neither diabetes mellitus nor hypertension was associated with more rapid deterioration of renal function.
Conclusion
This study suggests that the duration of lithium treatment contribute to the deterioration of renal function, raising the question of reducing dosages in patients with a GFR < 60 mL/min. Overdoses has been identified as a risk factor for CKD, emphasizing the importance of regular re-evaluation of the lithium dose regimen. Also, long-term lithium therapy was associated with hyperparathyroidism and hypercalcemia. Particular vigilance is required on these points in order to limit the occurrence of endocrinological and renal lithium adverse effects.
Similar content being viewed by others
Introduction
Lithium is well recognized as the first-line maintenance treatment for bipolar disorder (BD) in all international clinical practice guidelines since it is effective in preventing relapses of mood episodes and in reducing risk of suicide (Geddes and Miklowitz 2013), (Goodwin et al. 2016; Yatham et al. 2018). Others therapeutic indications of lithium therapy include schizophrenia (Leucht et al. 2015), major depression (Vázquez et al. 2021), alcoholism and cluster headaches (Timmer and Sands 1999). Besides therapeutic benefits attributed to lithium therapy, the associated side effects constitute important parameters in prescribing patterns and patient adherence.
Among the endocrinological effects, lithium-induced hypercalcemia and hyperparathyroidism are well known in the literature and appear to result from both acute and chronic effects. The acute, potentially reversible effects are related to the action of lithium on the calcium-sensing receptor and glycogen synthase kinase 3 pathway, resulting in a biochemical picture similar to that seen in familial hypocalciuric hypercalcemia (Ballehaninna et al. 2011; Mifsud et al. 2020; Szalat et al. 2009). Chronic effects are thought to be related to permanent changes in the parathyroid glands, either by unmasking hyperparathyroidism in patients with subclinical parathyroid adenoma or by triggering multiglandular hyperparathyroidism (McHenry and Lee 1996; Mifsud et al. 2020; Nordenström et al. 1992).
Among nephrotoxic effect, lithium is well known to cause nephrogenic diabetes insipidus (NDI) with an incidence that might be as high as 85% (Bockenhauer and Bichet 2015; Hetmar et al. 1986; Rej et al. 2012). Discontinuation of lithium therapy may resolve the symptoms of NDI, but this approach is not a reasonable treatment option in most cases, as the beneficial effects of lithium on psychiatric disorders overcome the negative impact of polyuric complications on quality of life. Even if the exact mechanism of this lithium toxicity is not known, robust data suggest that lithium exerts its effects after entering the principal cell through epithelial sodium channels (ENaCs), which have high permeability for lithium (Kortenoeven and Fenton 2014). This mechanism notably allows for the proposal of ENaC blockers such as amiloride, to increase urine osmolality and improve polyuria in lithium-induced NDI (Batlle et al. 1985; Bedford et al. 2008; Kortenoeven et al. 2009).
Beside lithium-induced NDI, its ability to cause chronic kidney disease (CKD) is a much more debated issue in the literature, with various studies suggesting both a positive and negative relationship (Azab et al. 2015; Clos et al. 2015; Gitlin 2016) (Gupta and Khastgir 2017). Despite these conflicting data, the predominant view seems to be that lithium has the capacity to cause chronic tubulointerstitial nephritis leading to progressive CKD over several years and end stage renal disease (ESRD) in about 1.5% of long-term lithium users (Fogo et al. 2017). To go further, the definition of risk factors for the development of CKD on lithium remains to date very poorly documented. Answering this question is all the more difficult because the progression of CKD on lithium may be irreversible. This makes it particularly difficult to observe an improvement in renal function when a suspected risk factor is removed. In contrast to NDIs, the question of the benefit-risk balance in the face of a patient with CKD with a high risk of relapse of BD if treatment is stopped is thus more challenging and currently constitutes an obstacle to the development of detailed recommendations on the subject (Ng et al. 2009).
Hence, the objectives of this study is to (i) determine whether long-term lithium therapy is associated with a decrease in renal function and hyperparathyroidism (ii) identify risk factors for lithium-induced nephrotoxicity.
Materials and methods
Study design and setting
This study was designed as a single-centered. We conducted a cohort study of adult patients (≥ 18 years) on lithium, who were hospitalized for any cause more than 24 h in Rennes University Hospital in France between January 1, 2018 and June 1, 2020. No specific ethical approval was sought. All information used within the study was anonymized and not traceable to a single individual.
Data sources
We collected the required data from the patient’s medical records: demographics characteristics [age, sex, body mass index (BMI)], biologic parameters (glomerular filtration rate (GFR), lithium blood level, parathormone (PTH) and calcium), medical comorbidities (hypertension and diabetes), lithium treatment duration and dosage. Only biological parameters at entry were considered. For lithium blood level assessment, blood samples from patients on once-daily lithium therapy were collected 24 h after the last dose, while blood samples from patients on twice-daily lithium therapy were collected 12 h after the last dose. GFR were estimated by CKD-EPI equations. Common nephrotoxic drugs at admission and discharge considered in this study (and listed according to the literature) are displayed in Table 1 (Kwiatkowska et al. 2021; Mody et al. 2020; Perazella 2018; Perazella and Rosner 2022).
Statistical analysis
The significance of intergroup differences [expressed as the mean ± standard error of the mean (SEM)] was determined using an unpaired t-test. A chi-squared test was used to compare percentages. Linear regression analysis was used to assess the relationship between biological variables (GFR, lithium blood level, PTH and calcium) and time of lithium exposure. Multiple regression analysis were used to adjust GFR for age, sex, number of nephrotoxic medications, hypertension, diabetes and of time of lithium exposure. All analyses were performed using Prism software (version 8.0, GraphPad Software, La Jolla, CA, USA). The threshold for statistical significance was set to p < 0.05 in all cases.
Results
Sample description
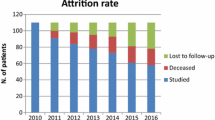
A total of 248 patients were included. Table 2 summarizes the clinical characteristics and demographics of patients. In the cohort, 59% (n = 146) of patients were women, mean age 60.2 ± 16.5 years. The majority of patients, 71% (n = 176) were on lithium for bipolarity. Co-occurring hypertension and diabetes mellitus were found in 80 patients (32%) and 34 patients (14%), respectively. Twenty-one patients (8.5%) presented both hypertension and diabetes mellitus.
Mean lithium therapy duration was 10.6 ± 10.9 years corresponding to an estimated cumulative lithium dose of 2221 ± 2570 g per patient. The mean CKD-EPI was 77.5 ± 31.9 mL/min per 1.73 m2 and 70 patients (28.8%) developed CKD stage 3 or more severe (CDK < 60 mL/min/1.73 m2). Eight patients reached ESRD at median age of 59 (± 11.3) years.
Mean lithium serum levels was 0.9 ± 0.8 mEq/L. Slightly more than 31% of the patients had a lithium blood level within the norms (i.e. between 0.5 and 0.8 mEq/L) while 37% were overdosed and 31% underdosed. More than half of patients [n = 133 (53.6%)] had no lithium blood level checked during their hospitalization. Regarding the distribution of the lithium dose, more than 86% of psychiatrists prescribe it in a single daily dose, 12% in 2 daily doses and only 2% in 3 daily doses. Lastly, the median age of the extended-release lithium group was significantly lower than the immediate-release lithium group (60 years old versus 66 years old, respectively, p = 0.0068).
Co-medication
Table 3 reports the nephrotoxic drugs most frequently found on prescriptions at admission and discharge. The number of nephrotoxic drugs per patient at admission tended to be higher in the GFR > 60 ml/min group compared to the < 60 ml/min group although not significant (0.45 ± 0.04 versus 0.37 ± 0.01, respectively).
Interestingly, decreased in renal function was non-significantly associated with a decrease in the average number of nephrotoxic drugs per patient (Table 4).
Relation between lithium therapy and renal functional impairment
Estimated creatinine clearance inversely correlated with the length of lithium therapy (Fig. 1A) (p < 0.0001) and estimated cumulative dose of lithium (Fig. 1B) (p < 0.0001). Deterioration of renal function was estimated at − 2.9 ml/min/year and median time to develop CKD Stage 3 from starting lithium therapy was 15.2 ± 9.6 years. Lastly, we noted that patients with lithium blood level > 0.8 mEq/ml had significantly lower renal function than patients with lithium blood level < 0.8 mEq/ml (61.8 ml/min versus 77.6 ml/min, respectively, p = 0.0134).
Biological parameter
A serum calcium concentration was determinated in 170 patients (2.34 ± 0.21 mmol/L) and 30 (17.6%) patients had hypercalcemia (> 2.5 mmol/L). Parathyroid hormone (PTH) level was measured in 37 patients (51.5 ± 49.0 pg/mL). We found correlation between the number of years on lithium therapy and the increase in calcium (p = 0. 0049) and PTH (p = 0.0063) (Fig. 2A–B). A non-significant trend of increasing blood lithium levels as a function of treatment time was observed (Fig. 2C).
Co-morbidities
Using multiple regression analysis we investigated whether patient co-morbidities and characteristics (namely age, sex, diabetes mellitus, hypertension, time of lithium exposure and number of nephrotoxic medications) were associated with renal function impairment. We found that age and time of exposure to lithium (but not diabetes mellitus or hypertension) emerged as risk factors for decreased renal function (p < 0.0001) (Table 5).
Discussion
In this study, we showed that (i) long-term lithium therapy is associated with a decrease in renal function, hyperparathyroidism and hypercalcemia and that (ii) the risk factors identified for renal toxicity should lead to close monitoring of renal function in these patients.
First, the decrease in renal function under lithium therapy was estimated at − 2.9 mL/min/year, which is consistent with previous studies among which this effect was estimated at − 2.3 mL/min/year (Presne et al. 2003; Shine et al. 2015). Multiple regression analysis revealed that time of lithium exposure was a risk factor for decreased renal function after adjusting for age, sex, diabetes, hypertension, and number of nephrotoxic medications (Table 5). The deterioration of renal function is thus 2 to 3 times more rapid compared to the general population where mean annual GFR loss is estimated at approximately 1 mL/min/1.73 m2 (Glassock and Rule 2016; Nankivell 2001; Schmitt and Melk 2017). Also, the median time to develop chronic kidney disease stage 3 (< 60 mL/min) from starting lithium therapy was 15.2 years, compared to 21.7 years in previous study (Pahwa et al. 2021). Going further, we highlighted that patients treated with high doses of lithium for a long period of time were likely to be at greater risk of developing chronic kidney disease, and raising the question of dose reduction in patients with a GFR < 60 mL/min. Since we have no data regarding the evolution of lithium dosages over the lifetime of patients, interpretation of cumulative dose data is particularly difficult. Also, a history of acute lithium intoxication is thought to constitute a risk factor for developing lithium-induced chronic renal failure (Gupta and Khastgir 2017). Because of this renal toxicity, a reassessment of the benefit-risk of lithium treatment may be necessary in some patients, although it may not be possible to discontinue it for psychiatric reasons. According to guidelines, patients with GFR < 60 mL/min/1.73 m2 require more intensive monitoring, even if the fibrous renal lesions are sometimes irreversible with progression of the deterioration even with the discontinuation of lithium (Kripalani et al. 2009; Morriss and Benjamin 2008).
Second, from a biochemical point of view, we showed that lithium treatment was associated with an increase in blood PTH and calcium concentrations (Fig. 2A, B). Lithium hyperparathyroidism is associated with increased morbidity such as nephrolithiasis and/or reduced bone mineral density, especially in chronically treated patients (Mifsud et al. 2020). For these reasons, regular monitoring of calcium levels in these patients is of utmost importance, as early recognition of lithium-associated hyperparathyroidism may improve outcomes. Also, the literature reports that hypercalcemia and hyperparathyroidism may occur more frequently in the elderly, prompting psychiatrists to be more vigilant both prior to starting treatment and at least annually thereafter (Lehmann and Lee 2013). In addition to the risk of nephrolithiasis, hypercalcemia can worsen nephrogenic diabetes insipidus, leading to dehydration and thus lithium intoxication, which can then deteriorate renal function (Khairallah et al. 2007).
Third, the increase in lithium blood level was not associated with time of lithium exposure in this study (Fig. 2C), despite the associated lower GFR observed for patients with lithium blood level > 0.8 mEq/ml. These results might suggest regular reassessment of renal function and lithium levels in a majority of patients, leading to subsequent adjustment of lithium dosages as the GFR decrease. As a therapeutic range around 1.2 mEq/mL can be targeted in manic episodes, this probably leads to a slight overestimation of the proportion the overdosed patients. This could also explain why the baseline lithium levels are relatively high.
Surprisingly, the presence of comorbidities (namely diabetes and hypertension) were not associated with a more rapid deterioration of renal function (Table 5). In the literature, Pahwa et al. (2021) reported that diabetes mellitus was associated with more rapid deterioration in function, with a population size equal to that of our population (n = 34) (Pahwa et al. 2021). Because of the trend toward accelerated deterioration of renal function observed in the diabetic and hypertensive patients in our study, it is likely that a larger number of patients included would have made a significant difference.
Lastly, it is known that there are several medications which can interfere both with serum lithium levels and renal function whose use needs to be closely monitored. Amongst these include the use of non-steroidal anti-inflammatory drugs, angiotensin-converting enzyme inhibitors, and thiazide diuretics while loop and potassium-sparing diuretics are generally considered to cause less disruption to serum lithium levels (Ng et al. 2009). In our study, the trend toward lower number of nephrotoxic drugs in patients with a GFR < 60 mL/min compared with patients with a GFR > 60 mL/min might suggest a withdrawal of nephrotoxic drugs by clinicians as the GFR decreases. Therefore, the impact of the presence of nephrotoxic drugs on renal function could not be assessed.
This study has several limitations. First, the limited number of patients may have limited the observation of a risk factor for renal toxicity, especially for comorbidities and comedications and a prospective study would be important to perform in this context. Second, the fact that the sample is that of hospitalized patients might indicate that this is a more ill cohort than an outpatient sample. Third, only a minority of the patients were evaluated regarding PTH, which may suggest confounding by indication, leading to caution in interpreting the data. Four, in the age group of the study population the use of D-vitamin and calcium supplement would be likely, which may have slightly overestimated the increases in calcemia found in this study.
Overall, precautions to be taken in case of lithium treatment include:
-
Screening for diabetic insipidus
-
Regular monitoring of blood lithium levels (we propose every 3 months for the first year, then every 6 months [except high risk groups such as elderly, taking interacting meds, renal or thyroid impairment, poor symptoms control or adherence, last lithium level over 0.8 mmol/L] as suggested by National Health Service guidelines [Tees Esk and Wear Valley NHS Foundation Trust 2021)].
-
Biological monitoring (TSH, PTH, ionogram, creatinine at least once a year), associated with education of the patient regarding co-medications or the procedure to follow in case of signs of overdose or dehydratation.
Conclusion
Lithium therapy result in increased risk of CKD overtime, raising the question of reducing dosages in patients with a GFR < 60 mL/min. Overdoses has been identified as a risk factor for CKD, emphasizing the importance of regular re-evaluation of the lithium dose regimen. Although difficult to implement, a prospective study would be interesting in order to identify more easily the impact of comorbidities and comedications on the evolution of renal function, which did not emerge in our study.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Azab AN, Shnaider A, Osher Y, Wang D, Bersudsky Y, Belmaker RH. Lithium nephrotoxicity. Int J Bipolar Disord. 2015;3(1):13.
Ballehaninna UK, Nguyen SM, Chamberlain RS. Lithium associated hyperparathyroidism: an evidence based surgical approach. SS. 2011;02(10):468–75.
Batlle DC, von Riotte AB, Gaviria M, Grupp M. Amelioration of polyuria by amiloride in patients receiving long-term lithium therapy. N Engl J Med. 1985;312(7):408–14.
Bedford JJ, Weggery S, Ellis G, McDonald FJ, Joyce PR, Leader JP, et al. Lithium-induced nephrogenic diabetes insipidus: renal effects of amiloride. CJASN. 2008;3(5):1324–31.
Bockenhauer D, Bichet DG. Pathophysiology, diagnosis and management of nephrogenic diabetes insipidus. Nat Rev Nephrol. 2015;11(10):576–88.
Clos S, Rauchhaus P, Severn A, Cochrane L, Donnan PT. Long-term effect of lithium maintenance therapy on estimated glomerular filtration rate in patients with affective disorders: a population-based cohort study. Lancet Psychiatry. 2015;2(12):1075–83.
Fogo AB, Lusco MA, Andeen NK, Najafian B, Alpers CE. AJKD atlas of renal pathology: lithium nephrotoxicity. Am J Kidney Dis. 2017;69(1):e1-2.
Geddes JR, Miklowitz DJ. Treatment of bipolar disorder. Lancet. 2013;381(9878):1672–82.
Gitlin M. Lithium side effects and toxicity: prevalence and management strategies. Int J Bipolar Disord. 2016;4(1):27.
Glassock RJ, Rule AD. Aging and the kidneys: anatomy, physiology and consequences for defining chronic kidney disease. Nephron. 2016;134(1):25–9.
Goodwin G, Haddad P, Ferrier I, Aronson J, Barnes T, Cipriani A, et al. Evidence based guidelines for treating bipolar disorder: revised third edition recommendations from the British association for psychopharmacology. J Psychopharmacol. 2016;30(6):495–553.
Gupta S, Khastgir U. Drug information update. lithium and chronic kidney disease: debates and dilemmas. BJPsych Bull. 2017;41(4):216–20.
Hetmar O, Bolwig TG, Brun C, Ladefoged J, Larsen S, Rafaelsen OJ. Lithium: long-term effects on the kidney I. renal function in retrospect. Acta Psychiatr Scand. 1986;73(5):574–81.
Khairallah W, Fawaz A, Brown EM, El-Hajj FG. Hypercalcemia and diabetes insipidus in a patient previously treated with lithium. Nat Rev Nephrol. 2007;3(7):397–404.
Kortenoeven MLA, Fenton RA. Renal aquaporins and water balance disorders. Biochim Biophys Acta. 2014;1840(5):1533–49.
Kortenoeven MLA, Li Y, Shaw S, Gaeggeler H-P, Rossier BC, Wetzels JFM, et al. Amiloride blocks lithium entry through the sodium channel thereby attenuating the resultant nephrogenic diabetes insipidus. Kidney Int. 2009;76(1):44–53.
Kripalani M, Shawcross J, Reilly J, Main J. Lithium and chronic kidney disease. BMJ. 2009;339(jul03 1):b2452–b2452.
Kwiatkowska E, Domański L, Dziedziejko V, Kajdy A, Stefańska K, Kwiatkowski S. The mechanism of drug nephrotoxicity and the methods for preventing kidney damage. IJMS. 2021;22(11):6109.
Lehmann SW, Lee J. Lithium-associated hypercalcemia and hyperparathyroidism in the elderly: what do we know? J Affect Disord. 2013;146(2):151–7.
Leucht S, Helfer B, Dold M, Kissling W, McGrath JJ. Lithium for schizophrenia. cochrane schizophrenia group, editor. Cochrane Database Syst Rev. 2015;2015:10. https://doi.org/10.1002/14651858.CD003834.pub3.
McHenry CR, Lee K. Lithium therapy and disorders of the parathyroid glands. Endocr Pract. 1996;2(2):103–9.
Mifsud S, Cilia K, Mifsud EL, Gruppetta M. Lithium-associated hyperparathyroidism. Br J Hosp Med. 2020;81(11):1–9.
Mody H, Ramakrishnan V, Chaar M, Lezeau J, Rump A, Taha K, et al. A review on drug-induced nephrotoxicity: pathophysiological mechanisms, drug classes, clinical management, and recent advances in mathematical modeling and simulation approaches. Clin Pharmacol Drug Dev. 2020;9(8):896–909.
Morriss R, Benjamin B. Lithium and eGFR: a new routinely available tool for the prevention of chronic kidney disease. Br J Psychiatry. 2008;193(2):93–5.
Nankivell BJ. Abnormal laboratory results: creatinine clearance and the assessment of renal function. Aust Prescr. 2001;24(1):15–7.
Ng F, Mammen OK, Wilting I, Sachs GS, Ferrier IN, Cassidy F, et al. the international society for bipolar disorders (ISBD) consensus guidelines for the safety monitoring of bipolar disorder treatments. Bipolar Disord. 2009;11(6):559–95.
Nordenström J, Strigård K, Perbeck L, Willems J, Bågedahl-Strindlund M, Linder J. Hyperparathyroidism associated with treatment of manic-depressive disorders by lithium. Eur J Surg. 1992;158(4):207–11.
Pahwa M, Joseph B, Nunez NA, Jenkins GD, Colby CL, Kashani KB, et al. Long-term lithium therapy and risk of chronic kidney disease in bipolar disorder: a historical cohort study. Bipolar Disord. 2021;23(7):715–23.
Perazella MA. Pharmacology behind common drug nephrotoxicities. CJASN. 2018;13(12):1897–908.
Perazella MA, Rosner MH. Drug-induced acute kidney. Injury. 2022. https://doi.org/10.2215/CJN.11290821.
Presne C, Fakhouri F, Noël L-H, Stengel B, Even C, Kreis H, et al. Lithium-induced nephropathy: rate of progression and prognostic factors. Kidney Int. 2003;64(2):585–92.
Rej S, Herrmann N, Shulman K. The effects of lithium on renal function in older adults—a systematic review. J Geriatr Psychiatry Neurol. 2012;25(1):51–61.
Schmitt R, Melk A. Molecular mechanisms of renal aging. Kidney Int. 2017;92(3):569–79.
Shine B, McKnight RF, Leaver L, Geddes JR. Long-term effects of lithium on renal, thyroid, and parathyroid function: a retrospective analysis of laboratory data. Lancet. 2015;386(9992):461–8.
Szalat A, Mazeh H, Freund HR. Lithium-associated hyperparathyroidism: report of four cases and review of the literature. Eur J Endocrinol. 2009;160(2):317–23.
Tees Esk and Wear Valley NHS Foundation Trust. Guidelines on safe lithium prescribing and shared care. 2021. https://www.tewv.nhs.uk/content/uploads/2022/01/Lithium-Shared-Care-Guidelines.pdf?UNLID=98991256620224215212
Timmer RT, Sands JM. Lithium intoxication. JASN. 1999;10(3):666–74.
Vázquez GH, Bahji A, Undurraga J, Tondo L, Baldessarini RJ. Efficacy and tolerability of combination treatments for major depression: antidepressants plus second-generation antipsychotics vs esketamine vs lithium. J Psychopharmacol. 2021;35(8):890–900.
Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Bond DJ, Frey BN, et al. Canadian network for mood and anxiety treatments (CANMAT) and international society for bipolar disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97–170.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
EB: Data curation, Investigation, Visualization, Writing- Original draft preparation. BLD: Data curation, Visualization, Methodology, Writing- Original draft preparation, Writing- Reviewing and Editing. RB: Writing- Reviewing and Editing. CV: Writing- Reviewing and Editing. MM: Investigation, Data curation, Visualization, Conceptualization, Methodology, Writing- Reviewing and Editing, Supervision. AB: Data curation, Investigation, Visualization, Conceptualization, Methodology, Writing- Reviewing and Editing, Supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was waived in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Consent of publication
We have a waiver of patient consents to participate and for publication due to the retrospective nature of the data, the anonymization of the data and the fact that all procedures presented in this article were performed as part of routine care.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Boivin, E., Le Daré, B., Bellay, R. et al. Long-term lithium therapy and risk of chronic kidney disease, hyperparathyroidism and hypercalcemia: a cohort study. Int J Bipolar Disord 11, 4 (2023). https://doi.org/10.1186/s40345-023-00286-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40345-023-00286-8