Abstract
Background
Treatment in bipolar disorder (BD) is commonly applied as a multimodal therapy based on decision algorithms that lack an integrative understanding of molecular mechanisms or a biomarker associated clinical outcome measure. Pharmacogenetics/genomics study the individual genetic variation associated with drug response. This selective review of pharmacogenomics and pharmacogenomic testing (PGT) in BD will focus on candidate genes and genome wide association studies of pharmacokinetic drug metabolism and pharmacodynamic drug response/adverse event, and the potential role of decision support tools that incorporate multiple genotype/phenotype drug recommendations.
Main body
We searched PubMed from January 2013 to May 2019, to identify studies reporting on BD and pharmacogenetics, pharmacogenomics and PGT. Studies were selected considering their contribution to the field. We summarize our findings in: targeted candidate genes of pharmacokinetic and pharmacodynamic pathways, genome-wide association studies and, PGT platforms, related to BD treatment. This field has grown from studies of metabolizing enzymes (i.e., pharmacokinetics) and drug transporters (i.e., pharmacodynamics), to untargeted investigations across the entire genome with the potential to merge genomic data with additional biological information.
Conclusions
The complexity of BD genetics and, the heterogeneity in BD drug-related phenotypes, are important considerations for the design and interpretation of BD PGT. The clinical applicability of PGT in psychiatry is in its infancy and is far from reaching the robust impact it has in other medical disciplines. Nonetheless, promising findings are discovered with increasing frequency with remarkable relevance in neuroscience, pharmacology and biology.
Similar content being viewed by others
Background
Bipolar Disorder (BD) is a complex chronic mood disorder where patient’s lives are variably associated with episodic recurrence (Angst and Sellaro 2000; Judd and Akiskal 2003), psychosocial and functional disability (Tohen et al. 2000; Zarate et al. 2000), and substantial morbidity and mortality especially in the depressive phase of illness (Frye 2011). While there have been advances in disease classification of illness subtype (i.e., BD-I, BD-II), symptom specifier (i.e., anxious distress, mixed features, rapid cycling, peripartum onset), and increasing recognition of high rates of comorbidity, the illness remains highly heterogeneous within patient groups and within a single patient’s longitudinal course of illness (Malhi et al. 2018). Moreover, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classification is not defined by an underlying pathophysiology and as such, limits the current understanding of neurobiological mechanisms of differential illness presentation and development of biomarkers of disease burden (Frey et al. 2013; Harrison et al. 2018).
There is no greater psychotropic pharmacopoeia in psychiatry than that of BD. Treatment selection with lithium, mood stabilizing anticonvulsants, mood stabilizing atypical antipsychotics, typical antipsychotics, unimodal antidepressants, and benzodiazepines, most commonly as a multimodal therapy, will be based on a number of factors including: clinical evidence base, phase of illness and symptom severity, BD-I vs BD-II subtype, level of cyclicity, and additional mental health and medical diagnoses that may impact efficacy and/or side effect burden. Molecular drug mechanisms of action, biomarkers of treatment response or adverse events, are not part of any clinical decision algorithm in BD. Oftentimes, polypharmacotherapy is necessary to achieve remission (Frye et al. 2000). However, multimodal drug therapy is challenging given the potential for pharmacokinetic drug–drug interactions and cumulative side effect burden. Developing biomarkers to individualize treatment in hopes of increasing rates of remission, tolerability, and adherence or mitigate serious drug related adverse event risk would represent a paradigm shift in current clinical practice models for both prescribers and patients.
Pharmacogenetics/genomics study the individual genetic variation associated with drug response. This field has grown from studies of metabolizing enzymes (i.e., pharmacokinetics) and drug transporters (i.e., pharmacodynamics), to untargeted investigations across the entire genome with the potential to merge genomic data with additional biological information (Weinshilboum and Wang 2017). Additional focus on a patient’s individual biology, vs solely broad Food and Drug Administration (FDA) indication labeling, may facilitate patient care with the “right drug, right dose, right time” (Bielinski et al. 2014). There are early pharmacogenomic studies in most treatment classes in BD (Pisanu et al. 2018b). This is of special importance in BD, where early intervention can have a positive impact in the progression of the disease (Post 2018).
For this selective review of pharmacogenomics in BD we searched PubMed from January 2013 to May 2019, to identify studies reporting on BD and pharmacogenetics, pharmacogenomics and pharmacogenomic testing (PGT). The authors selected studies based on their contribution to the field. We focus on candidate genes and genome wide association studies (GWAS) of pharmacokinetic drug metabolism and pharmacodynamic drug response/adverse event, and the potential role of decision support tools (DST) that incorporate multiple genotype/phenotype drug recommendations. The Clinical Pharmacogenomics Implementation Consortium (CPIC) (Relling and Klein 2011), was established as a joint effort between PharmGKB and the Pharmacogenomics Research Network (PGRN) to develop peer-reviewed guidelines for implementation of PGT, will be reviewed to illustrate early examples of clinical practice recommendations.
Targeted candidate genes in pharmacokinetic drug metabolism
The Cytochrome P450 (CYP) superfamily of proteins (2D6, 2C9, 2C19, 3A4) is one of the most important enzymatic classes responsible for phase I drug-metabolism, and thus, relevant to most of psychiatric medication’s metabolism and bioactivation (Spina and de Leon 2015). The notable exception, given its lack of metabolism is lithium. Early efforts in pharmacogenetics were, in part, dedicated to CYP genotyping/metabolic phenotyping with the goal of operationally defining phenotype classes that would be associated with response and side effects. These CYP phenotypic classifications [i.e., poor, intermediate, extensive (normal), and ultra-rapid] are the most common application of commercial PGT in psychiatry (Eum et al. 2016), however, no standardized model prevails to date (Gaedigk et al. 2017). It is important to acknowledge that race and ethnicity are important sources of variability between populations in allele composition and frequency of CYP genes. Inter-individual variability is even larger than that observed between ancestries producing large ranges of CYP activity among individuals. Moreover, CYP genes are strongly influenced by complex environmental factors that cannot be accounted by current PGT (McGraw et al. 2018). Nonetheless, the poor metabolizer phenotype and use of antidepressants has been the focus of a number of forensic cases of possible drug related fatality (i.e., 2D6), has driven a number of FDA drug label revisions (i.e., 2D6, 2C19) related to arrhythmia risk, and has been speculated, given black box warning for antidepressants in young adults, as a possible mechanism of treatment emergent suicidal ideation and antidepressant induced mania (AIM), both phenomena often identified early in the course of treatment [reviewed by (Nassan et al. 2016)]. Table 1 summarizes the evidence on pharmacokinetic PGT by drug class. Comprehensive sources on CYP PGT in psychiatry (Spina and de Leon 2015; Eum et al. 2016; Solomon et al. 2019) and CYP2D6 genetic variation considerations (Nofziger et al. 2020) are reviewed elsewhere.
CYP2D6
CYP2D6 is the most involved CYP isoform in psychiatric drug metabolism, and hundreds of CYP2D6 polymorphisms and copy number variations have been identified, many of which have unknown effects (McGraw et al. 2018). Multiple antidepressants and antipsychotics of different classes are its substrates, and CYP2D6 is inhibited strongly by fluoxetine, paroxetine, perphenazine and thioridazine. A recent study by Gaedgik et al. (2017) analyzed 177 reports of a world-wide population compromised of approximately 60,000 unrelated subjects and categorized them in metabolism phenotypes according to genotype meeting CPIC guidelines. Europeans represented most of the genotyped population (36%) and also had the greatest proportion of poor metabolizers (average, 5.4%), while Asians, Oceanians, and Middle Eastern populations, showed rates lower or equal to 1%. Ultra-rapid metabolizers were most represented in Oceanian (21.2%), Ashkenazi Jewish (11.5%), and Middle Eastern (11.2%) populations, with the lowest proportion in subjects from East Asia (1.4%). In spite of such efforts, the great genotypic variation in CYP2D6 confers confounding effects to the actual metabolism phenotype observed in individuals, and clinical studies may not always reflect an accurate prediction of treatment response, tolerability, or even pharmacokinetic parameters. It is also important to note that most of these clinical studies are non-prospective, have great heterogeneity in design, often have low subject numbers and do not control for environmental or drug–drug interactions (Eum et al. 2016).
Fifteen antipsychotics are major or minor substrates of CYP2D6 including most options for BD treatment, with quetiapine (CYP3A4, CYP3A5) and ziprasidone (CYP1A2, CYP3A4) as notable exceptions (Eum et al. 2016). There is variability in the magnitude of change in 2D6 poor-metabolizers’ antipsychotic serum concentrations and/or half-life for primary CYP2D6 antipsychotic substrates [i.e., 1.7X increase in aripiprazole serum concentration (Hendset et al. 2007), 2X increase and 7X increase in half-life of aripiprazole and risperidone respectively (Eum et al. 2016)]. A recent large retrospective cohort of CYP2D6 genotyped subjects treated with either risperidone (N = 1288) or aripiprazole (N = 1334) found statistically significant decreased metabolic ratios (i.e. metabolite/parent drug) for both drugs in poor and intermediate metabolizers; while greater metabolic ratios for ultra-rapid metabolizers, were only statistically significant for risperidone (Jukic et al. 2019). Moreover, poor and intermediate metabolizers showed increased risperidone and aripiprazole active moiety. These two drugs seem to present the greatest caution in 2D6 poor-metabolizer dosing; for further information on CYP2D6 and dosing precautions see Table 1.
A meta-analysis found no association between CYP2D6 genotyping and psychosis treatment efficacy in schizophrenia (Fleeman et al. 2011; Muller et al. 2012) however, it is important to point out that the authors found great variability of methodology and outcomes. The same study found, when including only prospective studies, a positive association between genotype, quantified only as mutant (i.e., not normal) vs wild type (i.e., normal), and tardive dyskinesia (Fleeman et al. 2011). In the retrospective study mentioned above, Jukic et al., found dose reductions from clinicians in both risperidone (19%) and aripiprazole (15%) poor metabolizers, however, only risperidone poor and ultra-rapid metabolizers show significantly higher switching to other antipsychotic agents; with no metabolizing phenotype showing greater switch to other agents in the aripiprazole group (Jukic et al. 2019). Performing prospective studies in BD will be of paramount importance before reaching more applicable clinical interpretations of CYP2D6 genotyping and antipsychotic prescription.
Studies associating CYP2D6 genotype and antidepressant pharmacokinetics and treatment response have been mostly performed in major depression. In patients treated with escitalopram (Ng et al. 2013; Hodgson et al. 2014, 2015), venlafaxine (Ng et al. 2013; Taranu et al. 2017) and nortriptyline (Hodgson et al. 2014, 2015), there was no association between metabolizing phenotype of CYP2D6 and response to these agents. The sole exception is the Lobello et al. (2010) study, which reviewed four placebo-controlled studies (n = 464) where 2D6 poor metabolizers, in comparison to extensive metabolizers, had significantly higher levels of serum parent compound venlafaxine, lower levels of active metabolite O-desmethylvenlafaxine, reduced baseline to endpoint change in depression scores, and significantly lower rates of treatment response and remission.
There is limited evidence that CYP2D6 poor-metabolizers were more likely to discontinue antidepressants (Berard et al. 2017). Antidepressant induced mania (AIM) has been reported in 3 bipolar depressed patients with a 2D6 poor metabolizer phenotype when prescribed 2D6 metabolized antidepressants (Sanchez-Iglesias et al. 2016). Similar to antipsychotics, CYP2D6 genotyping does not have a clear role in clinical decision for antidepressant prescription in bipolar patients, further studies, especially regarding the AIM risk warrant further exploration.
CYP2C19
Highly polymorphic-but significantly less than CYP2D6, CYP2C19 is mainly involved in the metabolism of tricyclic and selective serotonin reuptake inhibitors (SSRI) antidepressants, and benzodiazepines. Its genotype status influences the concentrations of amitriptyline and imipramine, and precautions are suggested for poor metabolizers (Hicks et al. 2015, 2017). Citalopram, escitalopram and sertraline show higher serum concentrations in CYP2C19 poor metabolizers, however, in contrast with the above, the wide therapeutic window of these drugs suggest that their effects may be more difficult to simply categorize by their metabolic phenotype (Spina and de Leon 2015). Nonetheless, a recent study by Jukic et al. (Jukic et al. 2018) in more than two-thousand Europeans with multiple psychiatric diagnosis, genotyped for CYP2C19 and medicated with escitalopram, showed that both poor and ultra-rapid CYP2C19 metabolizers predicted greater switching from escitalopram to another antidepressant. In this same study, CYP2C19 poor metabolizers showed greater odds of having lower than threshold therapeutic levels compared to extensive metabolizers; while this makes sense for ultra-rapid metabolizers, this is counterintuitive to poor metabolizer pharmacokinetics and may represent reduced treatment adherence (Jukic et al. 2018). In contrast, Fabbri and colleagues (Fabbri et al. 2018) found in a meta-analysis that CYP2C19 poor-metabolizers had higher side-effects compared to extensive metabolizers at weeks 2–4, however, also showed higher symptom improvement and remission in major depression when treated with citalopram or escitalopram. A 10-year retrospective cohort found that CYP2C19 poor metabolizers were more frequently observed in bipolar (9.8%) vs. unipolar subjects (0.6%, p = 0.003) (Veldic et al. 2019). The apparent impact of CYP2C19 genotype in treatment response to citalopram and escitalopram in depression, together with the observations of differences in CYP2C19 pharmacogenetics of bipolar depressed patients, warrants further exploration.
CYP2C9
CYP2C9 shows similar polymorphic variation to CYP2C19, but its role in the biotransformation of psychotropic drugs is minor (Spina and de Leon 2015). Of relevance, the secondary role it has in adult valproate metabolism seems to become clinically crucial in children, where it is responsible for most of this drug’s metabolism. Thus, its genotyping is recommended by some experts in this population (Monostory et al. 2019). CYP2C9 also modifies fluoxetine’s CYP2D6 metabolism but with an unknown clinical impact (Llerena et al. 2004).
Other pharmacokinetic genes such as ABCB1 and UGT1A4 are mentioned in Table 1.
Ethnic, environmental and drug–drug interaction variables also provide an enormous source of variability to the final metabolic phenotype expressed by the patient. Thus, bioinformatic tools based on systems biology will likely be needed in order to generate more intuitive models and clinical decision tools, based on pharmacokinetic PGT (McGraw et al. 2018).
Targeted candidate genes in pharmacodynamic drug response/adverse event
Pharmacodynamic pharmacogenetic candidate gene studies of most bipolar drug classes have been performed, with genetic variants selected mechanistically from neurotransmission, gene transcription, neuroplasticity, intracellular messenger cascades, and other pathways. However, our drug mechanism of action understanding is incomplete and limits hypothesis-driven design of candidate gene studies and their interpretation; moreover, current PGT may potentiate the intrinsic risk for false positive discoveries (Farrell et al. 2015). Nonetheless, we discuss the findings from such candidate gene studies so that clinicians who are faced with PGT DST, understand how the genetic variants included in these platforms were selected and why they should be careful with their interpretation.
Lithium
Lithium is the gold-standard mood stabilizing agent, with an extensive clinical evidence database for acute mania, bipolar depression, maintenance treatment (Bauer and Gitlin 2016), and suicidality prevention (Cipriani et al. 2013; Song et al. 2017). Clinical markers of response suggest that distinct patient groups may be more responsive to lithium (Grof et al. 1993; Post et al. 2016) suggesting a possible familial trait suggestive of genetic transmission (Grof et al. 1993, 2002, 2009). Lithium has been the most extensively studied of BD medications at the pharmacogenetic level and comprehensive reviews are available covering this topic (Alda 2015; Pisanu et al. 2016; Budde et al. 2017; Pickard 2017; Serretti 2017; Pisanu et al. 2018b).
Lithium mechanism of action involves multiple molecular mechanisms (Li et al. 2012). Thus, pharmacogenomic studies based on candidate genes have focused in genes implicated in many of these pathways. Neurotransmission genes for instance, largely based in monoamines—many of which are included in PGT—did not prompt any sufficiently robust associations of lithium treatment response (Budde et al. 2017; Pisanu et al. 2018b). Also included in PGT, the genetic single nucleotide polymorphism (SNP) rs6265, Val66Met, of BDNF, largely used to study neuroplasticity, showed mixed results (Michelon et al. 2006; Dmitrzak-Weglarz et al. 2008, Drago et al. 2010; Wang et al. 2012). GSK-3β is inhibited by lithium and, it is involved in neurogenesis, plasticity, and transcription through the Wnt canonical signaling pathway (Valvezan and Klein 2012). However, no robust evidence was found or replicated for GSK3B genetic variants (Michelon et al. 2006; Szczepankiewicz et al. 2006; Sathur Raghuraman et al. 2018); nor in other variants involved in genetic transcription, neuronal survival and plasticity, as SNPs in the CREB family (Mamdani et al. 2008) in association to lithium treatment response. Similarly, other variants related to inositol metabolism, involved in lithium’s mechanism of action, did not resulted in strong replicable results (Pisanu et al. 2016).
Lithium renal adverse events are an important though rare concern in BD treatment (Shine et al. 2015). To better inform lithium safety, a pharmacogenetic study of urinary concentration phenotypes were assessed in a group of 78 BD patients receiving lithium for a mean of 16 ± 9 years; in association with the GSK3B-50 C/T polymorphism, the authors found a statistically significant, though very modest association, not subjected to multiple testing correction, between the C-allele and kidney function, encouraging larger studies to better ascertain the potential role of GSK3B in informing lithium renal toxicity (Rybakowski et al. 2013).
Valproic acid
Valproic acid (VPA) is recommended in the treatment of bipolar mania, depression and maintenance (Grunze et al. 2013, 2018; Yatham et al. 2018). Sodium channel blockade is one of VPA’s proposed mechanisms of action. Genetic variation in the SCN family genes, specifically SCN2A, which encodes of the sodium channel (Haug et al. 2001), has shown mixed evidence of association with VPA response (Haerian et al. 2013; Li et al. 2016); it is important to reference that these studies were conducted in epilepsy patients and anticonvulsant and mood stabilization therapeutic mechanisms of action may differ. Included in PGT, CACNA1C and other calcium channel coding genes have been tested for VPA efficacy, but they prompted negative results (Lv et al. 2015), again, these studies were conducted in epilepsy patients. In bipolar populations, VPA response showed a positive association with XBP1-116 C/G polymorphism, but replication is needed (Kim et al. 2009). GNB3 variants have also been associated with metabolic abnormalities in cross-over (Chang et al. 2010) and prospective studies (Chen et al. 2017) of BD patients treated with VPA.
Carbamazepine and lamotrigine
Although rare, serious dermatologic adverse events are observed with antiepileptic mood-stabilizers. Carriers of the HLA-B*15:02 allele in Asian population, specifically of Han Chinese descent, are at risk of developing severe hypersensitivity reactions in association with carbamazepine, lamotrigine, and phenytoin treatment (Bloch et al. 2014); moreover, the FDA recommends PGT in patients of Asian ancestry for this specific variation before initiating carbamazepine treatment (Drozda et al. 2018). The generalizability to other anticonvulsants or other racial ethnic groups in BD has not been investigated.
Atypical antipsychotics
Weight-gain and other metabolic dysfunction is a major concern in BD treatment, especially regarding second-generation antipsychotics (SGAs) and mood-stabilizers. A recent meta-analysis of the genetic risk of anti-psychotics, predominantly SGAs-induced weight gain, explored 38 SNPS from 20 different genes in 6 independent samples (N = 6770) with predominant Caucasian and Asian ancestry (Zhang et al. 2016). 13 SNPs from 9 genes, namely ADRA2A, ADRB3, BDNF, DRD2, GNB3, HTR2C, INSIG2, MC4R and SNAP25 showed statistically significant associations with antipsychotic-related weight gain (P-values < 0.05–0.001), while SNPs in ADRA2A, DRD2, HTR2C, and MC4R had the largest effect sizes (Hedges’ g’s = 0.30–0.80, ORs = 1.47–1.96 (Zhang et al. 2016). Important limitations to this meta-analysis include important heterogeneity, from selected antipsychotic agents, previous exposure to antipsychotics, time of exposure; also, the lack of multiple testing analysis. As with most genetic association studies, further functional analysis of these SNPs is needed before reaching a complete understanding of their actual biological impact on the mentioned genes or else. ADR2A, BDNF, and DRD2 are included in most PGT commercial assays, however, the variants included in these tools are most of the time proprietary and thus it is unknown whether they test for the SNPs found in Zhang et al.’s study. Other efforts in understanding weight gain, specifically in BD, secondary to SGAs or mood stabilizers in 486 Systematic Treatment Enhancement Program for Bipolar Disorder subjects that did not identify significant candidate genes of weight gain liability (Creta et al. 2015).
Antidepressants
Clinical recommendations have been developed to address antidepressant use in bipolar depression hopefully reducing “the striking incongruity” between the widespread use of antidepressants in BD and the limited evidence that supports their use (Pacchiarotti et al. 2013). One concern of antidepressant use in BD is risk of AIM. A meta-analysis of controlled trials of antidepressants in bipolar depression reported a 12.5% rate of treatment emergent mania (Tondo et al. 2010). While there are clinical factors identified with AIM (Frye et al. 2006, Goldberg et al. 2007), there is increasing investigation of genetic markers in this drug related adverse event. The most studied genetic association for AIM has involved the serotonin transporter gene (SLC6A4), that encodes the protein in charge of serotonin synaptic reuptake, and the variants involved in its genetic expression. There are predominantly 2 well-known polymorphisms: (5-HTTLPR) with long (L) and short (S) allele variants and a second intron variable number of tandem repeats (VNTR). 5-HTTLPR association to AIM has been studied with meta-analysis showing conflicting information (Daray et al. 2010; Biernacka et al. 2012). A more recent meta-analysis combining the Mayo Clinic Bipolar Biobank with 5 prior AIM studies, provided marginal evidence of association for the S-allele of 5-HTTLPR with AIM (p = 0.059). On the other hand, haplotype analysis including SNP rs25531 (A/G), and the intron 2 VNTR (9, 10, 12 repeat alleles) showed that the L-A-10 haplotype was associated with a reduced risk of AIM (p = 0.012) (Frye et al. 2015). SLC6A4 variation is included in PGT commercial testing, however, before using it to inform AD prescription in BD, further exploration of the relationship between SLC6A4 variation and risk of AIM is needed. For instance, intron 2 VNTR and other SNPs with an impact in SLC6A4 expression, need to be employed in risk calculation, rather than focusing exclusively on the promoter long/short variant (Frye et al. 2015).
GWAS of drug response/adverse event
GWAS employ an agnostic or untargeted approach and do not rely on mechanistic hypothesis. They have prompted the most promising results regarding genetic markers of treatment response in BD.
Lithium
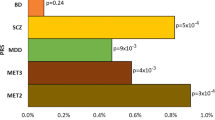
Most pharmacogenetic GWAS of BD have largely focused in Lithium. Initial efforts showed promising SNPs of risk, but they did not reach genome-wide significance of p ≤ 5 × 10−8 (Perlis et al. 2009; Squassina et al. 2011). The first genome-wide significant finding associated with lithium response, assessed by retrospective Alda scales, was achieved with a relatively small population (N = 294) of Han Chinese BD-I patients, and was replicated in an independent population (N = 100) (Chen et al. 2014). A robust association was observed for rs17026688 (p = 5.5 × 10−37) and rs17026651 (p = 2.52 × 10−37), variants in strong linkage disequilibrium (LD) in the GADL1 gene, and replicated (p = 9.19 × 10−15 for each SNP). Moreover, they showed a 93% sensitivity in predicting lithium response (Chen et al. 2014). GADL1 encodes a protein similar to GABA metabolism enzymes, suggesting biological plausibility of this finding. Furthermore, the effect-size of the association for the T-allele carriers and lithium response was enormous: 88.5 [95% confidence interval 41.4–198.0] (Chen et al. 2014). A study of this variant in a candidate gene study of Han Chinese patients additionally suggested a significant association with less recurrence and thus as a potential marker of lithium maintenance treatment (Chen et al. 2016). GADL1 SNPs were not further replicated outside of this initial work (Hou et al. 2014; Ikeda et al. 2014; Cruceanu et al. 2015; Kotambail et al. 2015), however, Asian ancestry replications included both Han Chinese and Japanese populations (Hou et al. 2014) and Japanese-only populations (Ikeda et al. 2014). Moreover, the phenotype in the Chen et al., original study was narrower than further replications (Chen et al. 2014). An analysis of gene expression found no activity of GADL1 in post mortem brain studies from individuals with BD (Birnbaum et al. 2014). The authors of this expression analysis hypothesized that, given the greater expression of GADL1 in the kidney and its involvement in renal function (Liu et al. 2012), GADL1 association to treatment response may be rather due to a renal function phenotype (Birnbaum et al. 2014).This is an important lesson in pharmacogenetics, showing the difficulty in interpreting and replicating even the most promising pharmacogenetic variants. Given its original and strong association with lithium response but further limitations in biological interpretation and replication, GADL1 variants should be regarded with caution as potential pharmacogenetic markers of BD.
The largest pharmacogenetic consortium of lithium, the International Consortium on Lithium Genetics (ConLiGen), performed a GWAS in 2563 “bipolar spectrum” patients—mainly bipolar 1—from 22 participating sites, and showed a genome-wide significant association with a group of SNPs in a single region of chromosome 21 (Hou et al. 2016). This region has two genes that code non-coding RNAs, which in turn could be involved in gene expression (Hou et al. 2016), however, the actual functional effect of these variants is yet to be fully investigated. Interestingly, a prospective sample (N = 73) showed association with this region and lower relapse rates in 2-year follow-up (Hou et al. 2016). Replication, biological and clinical interpretation of this finding remains to be elucidated. Similar findings were found by the same group, showing an inverse relationship between lithium response and schizophrenia polygenic risk (Amare et al. 2018). Moreover, a cross-trait meta-GWAS found 15 genetic variants that may have overlapping effects on lithium treatment response and susceptibility to SCZ; bioinformatic analysis of these variants suggested the involvement of the HLA antigen complex and inflammatory cytokines (Amare et al. 2018). HLA members are included in some commercial PGT, however, their role in establishing lithium response is not yet validated. A GWAS performed in bipolar 1, 2, not specified and schizoaffective disorder, patients from Sweden and the United Kingdom with subjective (N = 2698) and objective (N = 1176) measures of treatment response, showed no genome wide significant results comparing lithium response between BD patients. However, when compared to healthy controls, a variant from imputation, prompted a validated genome-wide significant result in rs116323614 (p = 2.74 × 10−8), located in SESTD1. The later gene seems to be involved in phospholipid synthesis, which are potential lithium targets (Song et al. 2016). The biological and clinical relevance of this association remains to be determined. Not only should they be regarded with caution in PGT but, to our knowledge, none of these variants are available for PGT commercials assays to date.
Clozapine
Clozapine is a SGA used in treatment resistant BD patients (Frye et al. 1998). In spite of its evident clinical benefit, clozapine use is limited due to clozapine-induced agranulocytosis/granulocytopenia (CIAG). Significant pharmacogenetic studied have explored this phenomenon, as recently reviewed by Numata et al. (2018). Several GWAS have been conducted, an initial effort by Goldstein et al., on 161 CIAG cases and 1196 controls of European descent, found genome-wide associations for variants in HLA-DQB1 and in HLA-B (Goldstein et al. 2014). In meta-analysis, only the HLA-DQB1 variant showed a nominally significant independent replication for a variant in HLA-DQB1 (OR = 15.6, P = 0.015, positive predictive value = 35.1), while a novel variant in rs149104283, an intronic transcript of SLCO1B3 and SLCO1B7, was associated with CIAG (OR = 4.32, P = 1.79 × 10−8) (Legge et al. 2017), but was not replicated in a Japanese sample (Saito et al. 2017). A GWAS in Japanese samples including 50 cases of CIAG vs. 2905 controls, identified rs1800625 in the HLA region, particularly an association of HLA-B*59:01 with CIAG (Saito et al. 2016).
Dermatologic severe reactions to mood stabilizers and CIAG genetic risk, are for now better understood in Asian ancestries, thus limiting the use of PGT to this population.
No prospective trials have followed PGT and safety/tolerability phenotypes. Interestingly, a retrospective survey associating efficacy and tolerability in MD and BD patients with PGT, observed accordance between side effect tolerability phenotype and the 15 evaluated genes (70.6%), however, this latter association was not significant (p = 0.71) (Tonozzi et al. 2018).
Potential role of DST that incorporate multiple genotype/phenotype drug recommendations
A number of commercially available platforms have been developed that rapidly assess pharmacokinetic and pharmacodynamic variation and develop a proprietary DST or algorithm to individualize treatment selection. A narrative review by Bousman and Hopwood (Bousman and Hopwood 2016) found 22 commercial companies offering PGT to five countries most prevalent in the USA (n = 13), followed by Australia and Canada (both n = 3). The majority of these platforms have focused on antidepressants in major depressive disorder primarily and antipsychotics in schizophrenia secondarily. Many of the pharmacogenetics candidate genes identified in response or adverse studies are commercially available as part of a DST. The extent of existing literature or clinical evidence base reviewed to assign a specific genotype a phenotypic pharmacokinetic (i.e., poor metabolizer) or pharmacodynamic (i.e., short form vs long form serotonin transporter) classification for each drug of the DST is proprietary. There is early work to suggest that different commercial products vary substantially, both in laboratory analysis of genotype and subsequent phenotypic classification (Bousman and Dunlop 2018).
There are early uncontrolled observations investigating the efficacy of PGT. Tonnozi et al. (2018) reported PGT of 15 genes (specific variants not reported) in 352 patients with major depression and BD. They reported that more than 60% of the self-reported retrospective treatment response and phenotype outcomes agreed (p = 0.001) and more than 70% of the reported side effect tolerability and phenotype outcome agreed, but this latter association was not significant. The retrospective nature of this association is a clear limitation. Prospective studies of DST have been compared to treatment as usual (TAU).
The Genomics Used to Improve Depression Decisions (GUIDED) trial is the largest study to date that randomized 1167 patients with major depression TAU vs genotype guided care. The primary outcome measure, baseline to endpoint in the Hamilton Depression Rating Scale, showed no significant difference between treatment groups, but secondary outcomes of treatment response and remission rates were statistically significant higher in in guided care vs TAU, though it is not clear if multiple testing was accounted for (Greden et al. 2019). Furthermore, patients randomized to guided care who switched from non-concordant treatment to concordant treatment, defined as agreement between DST recommendation and actual treatment selected, in comparison to those who stayed on non-concordant treatment, achieved a significant reduction in depressive symptoms and higher rates of response and remission. A recent meta-analysis of 5 studies, including Greden et al. (2019), reported that patients randomized to genotype guided care (n = 887) were 1.71 (95% CI 1.17–2.48, p = 0.005) times more likely to achieve remission than those patients randomized to TAU (Bousman et al. 2019). While the field continues to investigate these DST and attempt consensus as to their clinical utility, none of these studies have systematically investigated antidepressants or antipsychotics in BD. A small retrospective study of 30 BD-I and BD-II patients reported a similar observation to Greden et al. (2019) that as treatment concordance rates increased (i.e., genotype guided recommendation and actual treatment selected) from 13% at baseline and 40% at 3-month follow up, symptom severity as measured by the Clinical Global Impression—severity measure decreased (Ielmini et al. 2018). The bipolar pharamacopoiea would clearly advance where clinical treatment could be more individualized in reducing the risk:benefit ratio of antidepressants (i.e., AIM: depression efficacy) and atypical antipsychotics (tardive dyskinesia or cardiometabolics: depression efficacy).
There are two important examples of commissions dedicated to the evaluation of PGT in all medicine specialties. The Evaluation of Genomic Applications in Practice and Prevention (EGAPP) working group, part of the Centers of Disease Control and Prevention, developed a systematic process for evaluating genetic and PGT; they reviewed the utility of CYP450 PGT in major depression SSRI prescription more than 10 years ago and concluded, based on criteria of analytical validity, clinical validity, clinical usefulness, among other ethical/social aspects, that more research was needed before the benefit of PGT could be determined (E.o.G.A.i.P.a.P.E.W. Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group 2007). Concern was raised that important evidence from smaller pharmacogenetic trials and meta-analysis were not included that may have excluded important safety considerations related to CYP2D6 genotyping (Mrazek 2010). Commissioned by the National Health Service, the UK Genetic Testing Network (UKGTN) uses similar-to EGAPP but more extended criteria, to determine the benefit of PGT (UKGTN 2019b). Unfortunately, only dementia PGT is part of the psychiatry-related reports generated by this organization (UKGTN 2019a, b). However, using UKGTN modified criteria, Bousman and Hopwood (Bousman and Hopwood 2016) developed levels of evidence for pharmacogenetic testing variants available in commercial tests. Related to antidepressant therapy, a number of important development considerations were reviewed including: (1) 53% of the 46 tested genes had only preliminary or low supporting evidence (20% met criteria for the highest level), (2) only 60% of CYP2D6 and CYP2C19 metabolism-related variants were included in the commercial tests, (3) SNPs included per gene were not always reported in the commercial test, (4) limited availability of drug–drug and drug–gene interaction tools, and (5) not accounting for additional environmental effects and ancestry.
PGT also needs to be cost-effective and studies on willingness-to-pay show patient’s preference for PGT, in order to avoid trial-and-error prescriptions, medication changes and adverse events, is significant (Herbild et al. 2008, 2009). Early first investigations of PGT in mood and anxiety disorders appears promising. In a health claims dataset propensity-score, matched 6-month, case–control analysis, individuals with a mood/anxiety disorder (14.8% bipolar) who received PGT (n = 817), in comparison to similar mood/anxiety disorder individuals who did not receive PGT testing (n = 2745), recorded 40% fewer emergency room visits and 58% fewer inpatient all cause hospitalizations (Perlis et al. 2018). While overall 6-month number of psychotropic medications did not differ, overall costs were estimated to be nearly $2000 lower in the PGT group.
Conclusions
DST based on the pharmacogenomics evidence base for BD are significantly underdeveloped in comparison to antidepressants for major depressive disorder and antipsychotics for schizophrenia. PGT commercial assays provide a few robust clinical applications for safety concerns raised by BD treatment, especially in cutaneous side effects of mood-stabilizers in Asian populations. Other potential uses in BD are mostly limited to metabolic phenotype associated variants. However, in comparison to genetic variation associated with adverse event or quantifiable biological process (i.e., rash, QTc prolongation), the bar to establish pharmacogenomic efficacy is significantly higher and to date, the evidence base for treatment recommendations is significantly less (Ahmed et al. 2018). It is important to note that most of these commercial assays vary in content—which may be not fully disclosed—of the genetic tests provided. Moreover, they may provide limited interpretation tools.
It is possible, but yet not investigated, that pharmacogenetic phenotyping in BD may differ by disease phase (e.g., mania, depression, maintenance), clinical components or subphenotypes (e.g., rapid cycling, obesity, binge eating), presence/absence and composition of multimodal drug therapy, environmental influences that magnify or mitigate genetic variation, and overall illness staging (at-risk, first episode, chronic illness with loss of euthymia and functional baseline).
The complexity of BD genetics and, the heterogeneity in BD drug-related phenotypes, are important considerations for the design and interpretation of BD PGT. As BD genetic risk is better understood by additional GWAS and functional genomic studies, the underlying neurobiology of the illness will provide better guidance for genomic testing of pharmacotherapy interventions. Furthermore, risk calculating tools would need to go beyond PGT, and include other important markers of risk, namely clinical risk factors, neuroimaging findings, among others; to better achieve precision medicine in BD (Perlis 2016).
The fast growing consortiums and GWAS studies on lithium response seem one of the most promising avenues for BD pharmacogenomics. Variants in GADL1 and genes coding non-coding RNAs have been associated with this phenotype. However, these studies have thus far taught us important lessons, such as the one on Chen et al., GADL1 study. In spite of showing genome-wide associations and large effect sizes, further investigation on GADL1 did not support its association with lithium response. Moreover, functional studies seem to suggest that the GADL1 SNPs associated with lithium response, do not have an effect on its genetic expression at the brain level. This is a remarkable reminder of the caution needed when interpreting pharmacogenetic studies, a precaution that is even more crucial before PGT reaches clinical implementation. It is also important to bear in mind that genetics are only a step in the complex “omic” levels that may explain the heritability of a given phenotype. Thus, PGT in BD need to be complemented with epigenetics, gene expression, proteomic, etc., and tested in cellular models such as the ones, for example, provided by induced pluripotent stem cells. Relevant examples of genomic tool integration in BD are emerging. Pisanu et al. (2018a) integrated GWAS lithium response findings in cellular lines, measured their effect on gene expression and, integrating these technologies, they found a potential target in a zinc-finger protein coding gene. Induced pluripotent stem cell lines have revealed hyperexcitability phenotypes in BD neurons that are reversed in lithium response patients (Mertens et al. 2015), underscored the importance of GSK3-β and other Wnt signaling members in the BD neuronal cell-lines (Madison et al. 2015), and elicited a promising new “pathway of lithium response”, that governs the phosphorylation of CRMP2, which seems to be indirectly modulating GSK3-β (Tobe et al. 2017). The implementation of in silico and machine-learning technologies, will also be crucial in integrating these findings to design intuitive models that help us mimic the biological complexity of genetic–phenotypic interactions.
The clinical applicability of PGT in psychiatry is in its infancy (Stern et al. 2018) and is far from reaching the robust impact it has for instance, in other medical disciplines such as oncology. Nonetheless, promising findings in pharmacogenomic markers of efficacy are discovered with increasing frequency, especially for lithium. Over the last 10 years, pharmacogenetics and other pharmacogenomic technologies have evolved significantly, promising results of remarkable relevance in neuroscience, pharmacology and biology. Their ultimate goal of generating precision medicine in BD, may be a reality not so far in our future.
Availability of data and materials
All data used in the review has been published and/or referenced.
Abbreviations
- BD:
-
Bipolar disorder
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders
- FDA:
-
Food and Drug Administration
- CPIC:
-
Clinical Pharmacogenomics Implementation Consortium
- PGRN:
-
Pharmacogenomics Research Network
- PGT:
-
Pharmacogenomic testing
- CYP:
-
Cytochrome P450
- VPA:
-
Valproic acid
- SGA:
-
Second-generation antipsychotics
- AIM:
-
Antidepressant induced mania
- SSRI:
-
Selective serotonin reuptake inhibitors
- SNP:
-
Single nucleotide polymorphism
- SLC6A4 :
-
Serotonin transporter gene
- GWAS:
-
Genome wide association studies
- ConLiGen:
-
Consortium on Lithium Genetics
- CIAG:
-
Clozapine-induced agranulocytosis
- DST:
-
Decision Support Tool
- TAU:
-
Treatment as usual
- GUIDED:
-
The Genomics Used to Improve Depression Decisions
- EGAPP:
-
The Evaluation of Genomic Applications in Practice and Prevention
- UKGTN:
-
UK Genetic Testing Network
References
Ahmed AT, Weinshilboum R, Frye MA. Benefits of and barriers to pharmacogenomics-guided treatment for major depressive disorder. Clin Pharmacol Ther. 2018;103(5):767–9.
Alda M. Lithium in the treatment of bipolar disorder: pharmacology and pharmacogenetics. Mol Psychiatry. 2015;20(6):661–70.
Amare AT, Schubert KO, Hou L, Clark SR, Papiol S, Heilbronner U, Degenhardt F, Tekola-Ayele F, Hsu YH, Shekhtman T, Adli M, Akula N, Akiyama K, Ardau R, Arias B, Aubry JM, Backlund L, Bhattacharjee AK, Bellivier F, Benabarre A, Bengesser S, Biernacka JM, Birner A, Brichant-Petitjean C, Cervantes P, Chen HC, Chillotti C, Cichon S, Cruceanu C, Czerski PM, Dalkner N, Dayer A, Del Zompo M, DePaulo JR, Etain B, Falkai P, Forstner AJ, Frisen L, Frye MA, Fullerton JM, Gard S, Garnham JS, Goes FS, Grigoroiu-Serbanescu M, Grof P, Hashimoto R, Hauser J, Herms S, Hoffmann P, Hofmann A, Jamain S, Jimenez E, Kahn JP, Kassem L, Kuo PH, Kato T, Kelsoe J, Kittel-Schneider S, Kliwicki S, Konig B, Kusumi I, Laje G, Landen M, Lavebratt C, Leboyer M, Leckband SG, Tortorella A, Manchia M, Martinsson L, McCarthy MJ, McElroy S, Colom F, Mitjans M, Mondimore FM, Monteleone P, Nievergelt CM, Nothen MM, Novak T, O’Donovan C, Ozaki N, Osby U, Pfennig A, Potash JB, Reif A, Reininghaus E, Rouleau GA, Rybakowski JK, Schalling M, Schofield PR, Schweizer BW, Severino G, Shilling PD, Shimoda K, Simhandl C, Slaney CM, Squassina A, Stamm T, Stopkova P, Maj M, Turecki G, Vieta E, Volkert J, Witt S, Wright A, Zandi PP, Mitchell PB, Bauer M, Alda M, Rietschel M, McMahon FJ, Schulze TG, Baune BT. Association of polygenic score for schizophrenia and HLA antigen and inflammation genes with response to lithium in bipolar affective disorder: a genome-wide association study. JAMA Psychiatry. 2018;75(1):65–74.
Angst J, Sellaro R. Historical perspectives and natural history of bipolar disorder. Biol Psychiatry. 2000;48(6):445–57.
Bauer M, Gitlin MJ. The essential guide to lithium treatment. New York: Springer; 2016.
Berard A, Gaedigk A, Sheehy O, Chambers C, Roth M, Bozzo P, Johnson D, Kao K, Lavigne S, Wolfe L, Quinn D, Dieter K, Zhao JP. Association between CYP2D6 genotypes and the risk of antidepressant discontinuation, dosage modification and the occurrence of maternal depression during pregnancy. Front Pharmacol. 2017;8:402.
Bielinski SJ, Olson JE, Pathak J, Weinshilboum RM, Wang L, Lyke KJ, Ryu E, Targonski PV, Van Norstrand MD, Hathcock MA, Takahashi PY, McCormick JB, Johnson KJ, Maschke KJ, Rohrer Vitek CR, Ellingson MS, Wieben ED, Farrugia G, Morrisette JA, Kruckeberg KJ, Bruflat JK, Peterson LM, Blommel JH, Skierka JM, Ferber MJ, Black JL, Baudhuin LM, Klee EW, Ross JL, Veldhuizen TL, Schultz CG, Caraballo PJ, Freimuth RR, Chute CG, Kullo IJ. Preemptive genotyping for personalized medicine: design of the right drug, right dose, right time-using genomic data to individualize treatment protocol. Mayo Clin Proc. 2014;89(1):25–33.
Biernacka JM, McElroy SL, Crow S, Sharp A, Benitez J, Veldic M, Kung S, Cunningham JM, Post RM, Mrazek D, Frye MA. Pharmacogenomics of antidepressant induced mania: a review and meta-analysis of the serotonin transporter gene (5HTTLPR) association. J Affect Disord. 2012;136(1–2):e21–9.
Birnbaum R, Shin JH, Weinberger D. Variant GADL1 and response to lithium in bipolar I disorder. N Engl J Med. 2014;370(19):1855–6.
Bloch KM, Sills GJ, Pirmohamed M, Alfirevic A. Pharmacogenetics of antiepileptic drug-induced hypersensitivity. Pharmacogenomics. 2014;15(6):857–68.
Bousman CA, Dunlop BW. Genotype, phenotype, and medication recommendation agreement among commercial pharmacogenetic-based decision support tools. Pharmacogenomics J. 2018;18(5):613–22.
Bousman CA, Hopwood M. Commercial pharmacogenetic-based decision-support tools in psychiatry. Lancet Psychiatry. 2016;3(6):585–90.
Bousman CA, Arandjelovic K, Mancuso SG, Eyre HA, Dunlop BW. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1):37–47.
Bruckl TM, Uhr M. ABCB1 genotyping in the treatment of depression. Pharmacogenomics. 2016;17(18):2039–69.
Budde M, Degner D, Brockmoller J, Schulze TG. Pharmacogenomic aspects of bipolar disorder: an update. Eur Neuropsychopharmacol. 2017;27(6):599–609.
Chang HH, Gean PW, Chou CH, Yang YK, Tsai HC, Lu RB, Chen PS. C825T polymorphism of the GNB3 gene on valproate-related metabolic abnormalities in bipolar disorder patients. J Clin Psychopharmacol. 2010;30(5):512–7.
Chen CH, Lee CS, Lee MT, Ouyang WC, Chen CC, Chong MY, Wu JY, Tan HK, Lee YC, Chuo LJ, Chiu NY, Tsang HY, Chang TJ, Lung FW, Chiu CH, Chang CH, Chen YS, Hou YM, Chen CC, Lai TJ, Tung CL, Chen CY, Lane HY, Su TP, Feng J, Lin JJ, Chang CJ, Teng PR, Liu CY, Chen CK, Liu IC, Chen JJ, Lu T, Fan CC, Wu CK, Li CF, Wang KH, Wu LS, Peng HL, Chang CP, Lu LS, Chen YT, Cheng AT. Variant GADL1 and response to lithium therapy in bipolar I disorder. N Engl J Med. 2014;370(2):119–28.
Chen CK, Lee CS, Chen HY, Wu LS, Chang JC, Liu CY, Cheng AT. GADL1 variant and medication adherence in predicting response to lithium maintenance treatment in bipolar I disorder. BJPsych Open. 2016;2(5):301–6.
Chen PS, Chang HH, Huang CC, Lee CC, Lee SY, Chen SL, Huang SY, Yang YK, Lu RB. A longitudinal study of the association between the GNB3 C825T polymorphism and metabolic disturbance in bipolar II patients treated with valproate. Pharmacogenomics J. 2017;17(2):155–61.
Cipriani A, Hawton K, Stockton S, Geddes JR. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013;346:f3646.
Creta E, Fabbri C, Serretti A. Genetics of second-generation antipsychotic and mood stabilizer-induced weight gain in bipolar disorder: common and specific effects of key regulators of fat-mass homoeostasis genes. Pharmacogenet Genomics. 2015;25(7):354–62.
Cruceanu C, Alda M, Dion PA, Turecki G, Rouleau GA. No evidence for GADL1 variation as a bipolar disorder susceptibility factor in a Caucasian lithium-responsive cohort. Am J Psychiatry. 2015;172(1):94–5.
Daci A, Beretta G, Vllasaliu D, Shala A, Govori V, Norata GD, Krasniqi S. Polymorphic variants of SCN1A and EPHX1 influence plasma carbamazepine concentration, metabolism and pharmacoresistance in a population of Kosovar Albanian epileptic patients. PLoS ONE. 2015;10(11):e0142408.
Daray FM, Thommi SB, Ghaemi SN. The pharmacogenetics of antidepressant-induced mania: a systematic review and meta-analysis. Bipolar Disord. 2010;12(7):702–6.
Dmitrzak-Weglarz M, Rybakowski JK, Suwalska A, Skibinska M, Leszczynska-Rodziewicz A, Szczepankiewicz A, Hauser J. Association studies of the BDNF and the NTRK2 gene polymorphisms with prophylactic lithium response in bipolar patients. Pharmacogenomics. 2008;9(11):1595–603.
Drago A, Serretti A, Smith R, Huezo-Diaz P, Malitas P, Albani D, Ronchi DD, Pae CU, Aitchison KJ. No association between genetic markers in BDNF gene and lithium prophylaxis in a Greek sample. Int J Psychiatry Clin Pract. 2010;14(2):154–7.
Drago A, Giegling I, Schafer M, Hartmann AM, Friedl M, Konte B, Moller HJ, De Ronchi D, Stassen HH, Serretti A, Rujescu D. AKAP13, CACNA1, GRIK4 and GRIA1 genetic variations may be associated with haloperidol efficacy during acute treatment. Eur Neuropsychopharmacol. 2013;23(8):887–94.
Drozda K, Pacanowski MA, Grimstein C, Zineh I. Pharmacogenetic labeling of FDA-Approved drugs: a regulatory retrospective. JACC Basic Transl Sci. 2018;3(4):545–9.
E.o.G.A.i.P.a.P.E.W. Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group. Recommendations from the EGAPP Working Group: testing for cytochrome P450 polymorphisms in adults with nonpsychotic depression treated with selective serotonin reuptake inhibitors. Genet Med. 2007;9(12):819–25.
Eum S, Lee AM, Bishop JR. Pharmacogenetic tests for antipsychotic medications: clinical implications and considerations. Dialogues Clin Neurosci. 2016;18(3):323–37.
Fabbri C, Tansey KE, Perlis RH, Hauser J, Henigsberg N, Maier W, Mors O, Placentino A, Rietschel M, Souery D, Breen G, Curtis C, Lee SH, Newhouse S, Patel H, O’Donovan M, Lewis G, Jenkins G, Weinshilboum RM, Farmer A, Aitchison KJ, Craig I, McGuffin P, Schruers K, Biernacka JM, Uher R, Lewis CM. Effect of cytochrome CYP2C19 metabolizing activity on antidepressant response and side effects: meta-analysis of data from genome-wide association studies. Eur Neuropsychopharmacol. 2018;28(8):945–54.
Farrell MS, Werge T, Sklar P, Owen MJ, Ophoff RA, O’Donovan MC, Corvin A, Cichon S, Sullivan PF. Evaluating historical candidate genes for schizophrenia. Mol Psychiatry. 2015;20(5):555–62.
Fleeman N, Dundar Y, Dickson R, Jorgensen A, Pushpakom S, McLeod C, Pirmohamed M, Walley T. Cytochrome P450 testing for prescribing antipsychotics in adults with schizophrenia: systematic review and meta-analyses. Pharmacogenomics J. 2011;11(1):1–14.
Frey BN, Andreazza AC, Houenou J, Jamain S, Goldstein BI, Frye MA, Leboyer M, Berk M, Malhi GS, Lopez-Jaramillo C, Taylor VH, Dodd S, Frangou S, Hall GB, Fernandes BS, Kauer-Sant’Anna M, Yatham LN, Kapczinski F, Young LT. Biomarkers in bipolar disorder: a positional paper from the International Society for Bipolar Disorders Biomarkers Task Force. Aust N Z J Psychiatry. 2013;47(4):321–32.
Frye MA. Clinical practice. Bipolar disorder—a focus on depression. N Engl J Med. 2011;364(1):51–9.
Frye MA, Ketter TA, Altshuler LL, Denicoff K, Dunn RT, Kimbrell TA, Cora-Locatelli G, Post RM. Clozapine in bipolar disorder: treatment implications for other atypical antipsychotics. J Affect Disord. 1998;48(2–3):91–104.
Frye MA, Ketter TA, Leverich GS, Huggins T, Lantz C, Denicoff KD, Post RM. The increasing use of polypharmacotherapy for refractory mood disorders: 22 years of study. J Clin Psychiatry. 2000;61(1):9–15.
Frye MA, Yatham LN, Calabrese JR, Bowden CL, Ketter TA, Suppes T, Adams BE, Thompson TR. Incidence and time course of subsyndromal symptoms in patients with bipolar I disorder: an evaluation of 2 placebo-controlled maintenance trials. J Clin Psychiatry. 2006;67(11):1721–8.
Frye MA, McElroy SL, Prieto ML, Harper KL, Walker DL, Kung S, Chauhan M, Crow S, Sutor B, Galardy CW, Veldic M, Palmer BA, Geske JR, Fuentes M, Cuellar-Barboza AB, Seymour LR, Mori N, Biernacka JM. Clinical risk factors and serotonin transporter gene variants associated with antidepressant-induced mania. J Clin Psychiatry. 2015;76(2):174–80.
Gaedigk A, Sangkuhl K, Whirl-Carrillo M, Klein T, Leeder JS. Prediction of CYP2D6 phenotype from genotype across world populations. Genet Med. 2017;19(1):69–76.
Goldberg JF, Perlis RH, Ghaemi SN, Calabrese JR, Bowden CL, Wisniewski S, Miklowitz DJ, Sachs GS, Thase ME. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348–55.
Goldstein JI, Jarskog LF, Hilliard C, Alfirevic A, Duncan L, Fourches D, Huang H, Lek M, Neale BM, Ripke S, Shianna K, Szatkiewicz JP, Tropsha A, van den Oord EJ, Cascorbi I, Dettling M, Gazit E, Goff DC, Holden AL, Kelly DL, Malhotra AK, Nielsen J, Pirmohamed M, Rujescu D, Werge T, Levy DL, Josiassen RC, Kennedy JL, Lieberman JA, Daly MJ, Sullivan PF. Clozapine-induced agranulocytosis is associated with rare HLA-DQB1 and HLA-B alleles. Nat Commun. 2014;5:4757.
Greden JF, Parikh SV, Rothschild AJ, Thase ME, Dunlop BW, DeBattista C, Conway CR, Forester BP, Mondimore FM, Shelton RC, Macaluso M, Li J, Brown K, Gilbert A, Burns L, Jablonski MR, Dechairo B. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: a large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res. 2019;111:59–67.
Grof P, Alda M, Grof E, Fox D, Cameron P. The challenge of predicting response to stabilising lithium treatment. The importance of patient selection. Br J Psychiatry. 1993;163(Suppl21):16–9.
Grof P, Duffy A, Cavazzoni P, Grof E, Garnham J, MacDougall M, O’Donovan C, Alda M. Is response to prophylactic lithium a familial trait? J Clin Psychiatry. 2002;63(10):942–7.
Grof P, Duffy A, Alda M, Hajek T. Lithium response across generations. Acta Psychiatr Scand. 2009;120(5):378–85.
Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Moller HJ, Kasper S. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2012 on the long-term treatment of bipolar disorder. World J Biol Psychiatry. 2013;14(3):154–219.
Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Azorin JM, Yatham L, Mosolov S, Moller HJ, Kasper S. The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders: acute and long-term treatment of mixed states in bipolar disorder. World J Biol Psychiatry. 2018;19(1):2–58.
Haerian BS, Baum L, Kwan P, Tan HJ, Raymond AA, Mohamed Z. SCN1A, SCN2A and SCN3A gene polymorphisms and responsiveness to antiepileptic drugs: a multicenter cohort study and meta-analysis. Pharmacogenomics. 2013;14(10):1153–66.
Harrison PJ, Geddes JR, Tunbridge EM. The Emerging Neurobiology of Bipolar Disorder. Trends Neurosci. 2018;41(1):18–30.
Haug K, Hallmann K, Rebstock J, Dullinger J, Muth S, Haverkamp F, Pfeiffer H, Rau B, Elger CE, Propping P, Heils A. The voltage-gated sodium channel gene SCN2A and idiopathic generalized epilepsy. Epilepsy Res. 2001;47(3):243–6.
Hendset M, Hermann M, Lunde H, Refsum H, Molden E. Impact of the CYP2D6 genotype on steady-state serum concentrations of aripiprazole and dehydroaripiprazole. Eur J Clin Pharmacol. 2007;63(12):1147–51.
Herbild L, Gyrd-Hansen D, Bech M. Patient preferences for pharmacogenetic screening in depression. Int J Technol Assess Health Care. 2008;24(1):96–103.
Herbild L, Bech M, Gyrd-Hansen D. Estimating the Danish populations’ preferences for pharmacogenetic testing using a discrete choice experiment. The case of treating depression. Value Health. 2009;12(4):560–7.
Hicks JK, Bishop JR, Sangkuhl K, Muller DJ, Ji Y, Leckband SG, Leeder JS, Graham RL, Chiulli DL, LLerena A, Skaar TC, Scott SA, Stingl JC, Klein TE, Caudle KE, Gaedigk A, C. Clinical Pharmacogenetics Implementation. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6 and CYP2C19 genotypes and dosing of selective serotonin reuptake inhibitors. Clin Pharmacol Ther. 2015;98(2):127–34.
Hicks JK, Sangkuhl K, Swen JJ, Ellingrod VL, Muller DJ, Shimoda K, Bishop JR, Kharasch ED, Skaar TC, Gaedigk A, Dunnenberger HM, Klein TE, Caudle KE, Stingl JC. Clinical pharmacogenetics implementation consortium guideline (CPIC) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clin Pharmacol Ther. 2017;102(1):37–44.
Hodgson K, Tansey K, Dernovsek MZ, Hauser J, Henigsberg N, Maier W, Mors O, Placentino A, Rietschel M, Souery D, Smith R, Craig IW, Farmer AE, Aitchison KJ, Belsey S, Davis OS, Uher R, McGuffin P. Genetic differences in cytochrome P450 enzymes and antidepressant treatment response. J Psychopharmacol. 2014;28(2):133–41.
Hodgson K, Tansey KE, Uher R, Dernovsek MZ, Mors O, Hauser J, Souery D, Maier W, Henigsberg N, Rietschel M, Placentino A, Craig IW, Aitchison KJ, Farmer AE, Dobson RJ, McGuffin P. Exploring the role of drug-metabolising enzymes in antidepressant side effects. Psychopharmacology. 2015;232(14):2609–17.
Hou L, Heilbronner U, Rietschel M, Kato T, Kuo PH, McMahon FJ, Schulze TG. Variant GADL1 and response to lithium in bipolar I disorder. N Engl J Med. 2014;370(19):1857–9.
Hou L, Heilbronner U, Degenhardt F, Adli M, Akiyama K, Akula N, Ardau R, Arias B, Backlund L, Banzato CEM, Benabarre A, Bengesser S, Bhattacharjee AK, Biernacka JM, Birner A, Brichant-Petitjean C, Bui ET, Cervantes P, Chen GB, Chen HC, Chillotti C, Cichon S, Clark SR, Colom F, Cousins DA, Cruceanu C, Czerski PM, Dantas CR, Dayer A, Etain B, Falkai P, Forstner AJ, Frisen L, Fullerton JM, Gard S, Garnham JS, Goes FS, Grof P, Gruber O, Hashimoto R, Hauser J, Herms S, Hoffmann P, Hofmann A, Jamain S, Jimenez E, Kahn JP, Kassem L, Kittel-Schneider S, Kliwicki S, Konig B, Kusumi I, Lackner N, Laje G, Landen M, Lavebratt C, Leboyer M, Leckband SG, Jaramillo CAL, MacQueen G, Manchia M, Martinsson L, Mattheisen M, McCarthy MJ, McElroy SL, Mitjans M, Mondimore FM, Monteleone P, Nievergelt CM, Nothen MM, Osby U, Ozaki N, Perlis RH, Pfennig A, Reich-Erkelenz D, Rouleau GA, Schofield PR, Schubert KO, Schweizer BW, Seemuller F, Severino G, Shekhtman T, Shilling PD, Shimoda K, Simhandl C, Slaney CM, Smoller JW, Squassina A, Stamm T, Stopkova P, Tighe SK, Tortorella A, Turecki G, Volkert J, Witt S, Wright A, Young LT, Zandi PP, Potash JB, DePaulo JR, Bauer M, Reininghaus EZ, Novak T, Aubry JM, Maj M, Baune BT, Mitchell PB, Vieta E, Frye MA, Rybakowski JK, Kuo PH, Kato T, Grigoroiu-Serbanescu M, Reif A, Del Zompo M, Bellivier F, Schalling M, Wray NR, Kelsoe JR, Alda M, Rietschel M, McMahon FJ, Schulze TG. Genetic variants associated with response to lithium treatment in bipolar disorder: a genome-wide association study. Lancet. 2016;387(10023):1085–93.
Ielmini M, Poloni N, Caselli I, Espadaler J, Tuson M, Grecchi A, Callegari C. The utility of pharmacogenetic testing to support the treatment of bipolar disorder. Pharmgenomics Pers Med. 2018;11:35–42.
Ikeda M, Kondo K, Iwata N. Variant GADL1 and response to lithium in bipolar I disorder. N Engl J Med. 2014;370(19):1856–7.
Ji Y, Biernacka J, Snyder K, Drews M, Pelleymounter LL, Colby C, Wang L, Mrazek DA, Weinshilboum RM. Catechol O-methyltransferase pharmacogenomics and selective serotonin reuptake inhibitor response. Pharmacogenomics J. 2012;12(1):78–85.
Judd LL, Akiskal HS. Depressive episodes and symptoms dominate the longitudinal course of bipolar disorder. Curr Psychiatry Rep. 2003;5(6):417–8.
Jukic MM, Haslemo T, Molden E, Ingelman-Sundberg M. Impact of CYP2C19 genotype on escitalopram exposure and therapeutic failure: a retrospective study based on 2087 patients. Am J Psychiatry. 2018;175(5):463–70.
Jukic MM, Smith RL, Haslemo T, Molden E, Ingelman-Sundberg M. Effect of CYP2D6 genotype on exposure and efficacy of risperidone and aripiprazole: a retrospective, cohort study. Lancet Psychiatry. 2019;6(5):418–26.
Kawaguchi DM, Glatt SJ. GRIK4 polymorphism and its association with antidepressant response in depressed patients: a meta-analysis. Pharmacogenomics. 2014;15(11):1451–9.
Kim SC, Kim MG. Meta-analysis of the influence of UGT genetic polymorphisms on lamotrigine concentration. Basic Clin Pharmacol Toxicol. 2019;124(2):163–9.
Kim B, Kim CY, Lee MJ, Joo YH. Preliminary evidence on the association between XBP1-116C/G polymorphism and response to prophylactic treatment with valproate in bipolar disorders. Psychiatry Res. 2009;168(3):209–12.
Kotambail A, Mathur A, Bhat SM, Rai PS, Sharma PS, Satyamoorthy K. GADL1 gene polymorphisms and lithium response in bipolar I disorder: lack of association from an Indian population. Psychiatr Genet. 2015;25(1):39–40.
Legge SE, Hamshere ML, Ripke S, Pardinas AF, Goldstein JI, Rees E, Richards AL, Leonenko G, Jorskog LF, Chambert KD, Collier DA, Genovese G, Giegling I, Holmans P, Jonasdottir A, Kirov G, McCarroll SA, MacCabe JH, Mantripragada K, Moran JL, Neale BM, Stefansson H, Rujescu D, Daly MJ, Sullivan PF, Owen MJ, O’Donovan MC, Walters JTR. Genome-wide common and rare variant analysis provides novel insights into clozapine-associated neutropenia. Mol Psychiatry. 2017;22(10):1502–8.
Li X, Frye MA, Shelton RC. Review of pharmacological treatment in mood disorders and future directions for drug development. Neuropsychopharmacology. 2012;37(1):77–101.
Li X, Zhang J, Wu X, Yan H, Zhang Y, He RH, Tang YJ, He YJ, Tan D, Mao XY, Yin JY, Liu ZQ, Zhou HH, Liu J. Polymorphisms of ABAT, SCN2A and ALDH5A1 may affect valproic acid responses in the treatment of epilepsy in Chinese. Pharmacogenomics. 2016;17(18):2007–14.
Lin JY, Jiang MY, Kan ZM, Chu Y. Influence of 5-HTR2A genetic polymorphisms on the efficacy of antidepressants in the treatment of major depressive disorder: a meta-analysis. J Affect Disord. 2014;168:430–8.
Liu P, Ge X, Ding H, Jiang H, Christensen BM, Li J. Role of glutamate decarboxylase-like protein 1 (GADL1) in taurine biosynthesis. J Biol Chem. 2012;287(49):40898–906.
Llerena A, Dorado ALP, Berecz R, Gonzalez AP, Penas LEM. Effect of CYP2D6 and CYP2C9 genotypes on fluoxetine and norfluoxetine plasma concentrations during steady-state conditions. Eur J Clin Pharmacol. 2004;59(12):869–73.
Lobello KW, Preskorn SH, Guico-Pabia CJ, Jiang Q, Paul J, Nichols AI, Patroneva A, Ninan PT. Cytochrome P450 2D6 phenotype predicts antidepressant efficacy of venlafaxine: a secondary analysis of 4 studies in major depressive disorder. J Clin Psychiatry. 2010;71(11):1482–7.
Lv N, Qu J, Long H, Zhou L, Cao Y, Long L, Liu Z, Xiao B. Association study between polymorphisms in the CACNA1A, CACNA1C, and CACNA1H genes and drug-resistant epilepsy in the Chinese Han population. Seizure. 2015;30:64–9.
Ma X, Maimaitirexiati T, Zhang R, Gui X, Zhang W, Xu G, Hu G. HTR2C polymorphisms, olanzapine-induced weight gain and antipsychotic-induced metabolic syndrome in schizophrenia patients: a meta-analysis. Int J Psychiatry Clin Pract. 2014;18(4):229–42.
Madison JM, Zhou F, Nigam A, Hussain A, Barker DD, Nehme R, van der Ven K, Hsu J, Wolf P, Fleishman M, O’Dushlaine C, Rose S, Chambert K, Lau FH, Ahfeldt T, Rueckert EH, Sheridan SD, Fass DM, Nemesh J, Mullen TE, Daheron L, McCarroll S, Sklar P, Perlis RH, Haggarty SJ. Characterization of bipolar disorder patient-specific induced pluripotent stem cells from a family reveals neurodevelopmental and mRNA expression abnormalities. Mol Psychiatry. 2015;20(6):703–17.
Malhi GS, Irwin L, Hamilton A, Morris G, Boyce P, Mulder R, Porter RJ. Modelling mood disorders: an ACE solution? Bipolar Disord. 2018;20(Suppl 2):4–16.
Mamdani F, Alda M, Grof P, Young LT, Rouleau G, Turecki G. Lithium response and genetic variation in the CREB family of genes. Am J Med Genet B Neuropsychiatr Genet. 2008;147b(4):500–4.
McGraw J, Gerhardt A, Morris TC. Opportunities and obstacles in genotypic prediction of cytochrome P450 phenotypes. Expert Opin Drug Metab Toxicol. 2018;14(7):659–61.
Mertens J, Wang QW, Kim Y, Yu DX, Pham S, Yang B, Zheng Y, Diffenderfer KE, Zhang J, Soltani S, Eames T, Schafer ST, Boyer L, Marchetto MC, Nurnberger JI, Calabrese JR, Odegaard KJ, McCarthy MJ, Zandi PP, Alda M, Nievergelt CM, Mi S, Brennand KJ, Kelsoe JR, Gage FH, Yao J. Differential responses to lithium in hyperexcitable neurons from patients with bipolar disorder. Nature. 2015;527(7576):95–9.
Michelon L, Meira-Lima I, Cordeiro Q, Miguita K, Breen G, Collier D, Vallada H. Association study of the INPP1, 5HTT, BDNF, AP-2beta and GSK-3beta GENE variants and restrospectively scored response to lithium prophylaxis in bipolar disorder. Neurosci Lett. 2006;403(3):288–93.
Monostory K, Nagy A, Toth K, Budi T, Kiss A, Deri M, Csukly G. Relevance of CYP2C9 function in valproate therapy. Curr Neuropharmacol. 2019;17(1):99–106.
Mrazek D. Psychiatric pharmacogenomics. New York: Oxford University Press; 2010.
Muller DJ, Brandl EJ, Hwang R, Tiwari AK, Sturgess JE, Zai CC, Lieberman JA, Kennedy JL, Richter MA. The AmpliChip(R) CYP450 test and response to treatment in schizophrenia and obsessive compulsive disorder: a pilot study and focus on cases with abnormal CYP2D6 drug metabolism. Genet Test Mol Biomarkers. 2012;16(8):897–903.
Nassan M, Nicholson WT, Elliott MA, Rohrer Vitek CR, Black JL, Frye MA. Pharmacokinetic pharmacogenetic prescribing guidelines for antidepressants: a template for psychiatric precision medicine. Mayo Clin Proc. 2016;91(7):897–907.
Ng C, Sarris J, Singh A, Bousman C, Byron K, Peh LH, Smith DJ, Tan CH, Schweitzer I. Pharmacogenetic polymorphisms and response to escitalopram and venlafaxine over 8 weeks in major depression. Hum Psychopharmacol. 2013;28(5):516–22.
Nofziger C, Turner AJ, Sangkuhl K, Whirl-Carrillo M, Agundez JAG, Black JL, Dunnenberger HM, Ruano G, Kennedy MA, Phillips MS, Hachad H, Klein TE, Gaedigk A. PharmVar GeneFocus: CYP2D6. Clin Pharmacol Ther. 2020;107(1):154–70.
Numata S, Umehara H, Ohmori T, Hashimoto R. Clozapine pharmacogenetic studies in schizophrenia: efficacy and agranulocytosis. Front Pharmacol. 2018;9:1049.
Pacchiarotti I, Bond DJ, Baldessarini RJ, Nolen WA, Grunze H, Licht RW, Post RM, Berk M, Goodwin GM, Sachs GS, Tondo L, Findling RL, Youngstrom EA, Tohen M, Undurraga J, Gonzalez-Pinto A, Goldberg JF, Yildiz A, Altshuler LL, Calabrese JR, Mitchell PB, Thase ME, Koukopoulos A, Colom F, Frye MA, Malhi GS, Fountoulakis KN, Vazquez G, Perlis RH, Ketter TA, Cassidy F, Akiskal H, Azorin JM, Valenti M, Mazzei DH, Lafer B, Kato T, Mazzarini L, Martinez-Aran A, Parker G, Souery D, Ozerdem A, McElroy SL, Girardi P, Bauer M, Yatham LN, Zarate CA, Nierenberg AA, Birmaher B, Kanba S, El-Mallakh RS, Serretti A, Rihmer Z, Young AH, Kotzalidis GD, MacQueen GM, Bowden CL, Ghaemi SN, Lopez-Jaramillo C, Rybakowski J, Ha K, Perugi G, Kasper S, Amsterdam JD, Hirschfeld RM, Kapczinski F, Vieta E. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am J Psychiatry. 2013;170(11):1249–62.
Paddock S, Laje G, Charney D, Rush AJ, Wilson AF, Sorant AJM, Lipsky R, Wisniewski SR, Manji H, McMahon FJ. Association of GRIK4 with outcome of antidepressant treatment in the STAR*D cohort. Am J Psychiatry. 2007;164(8):1181–8.
Park JY, Kim KA, Park PW, Lee OJ, Kang DK, Shon JH, Liu KH, Shin JG. Effect of CYP3A5*3 genotype on the pharmacokinetics and pharmacodynamics of alprazolam in healthy subjects. Clin Pharmacol Ther. 2006;79(6):590–9.
Patriquin MA, Bauer IE, Soares JC, Graham DP, Nielsen DA. Addiction pharmacogenetics: a systematic review of the genetic variation of the dopaminergic system. Psychiatr Genet. 2015;25(5):181–93.
Perlis RH. Abandoning personalization to get to precision in the pharmacotherapy of depression. World Psychiatry. 2016;15(3):228–35.
Perlis RH, Smoller JW, Ferreira MA, McQuillin A, Bass N, Lawrence J, Sachs GS, Nimgaonkar V, Scolnick EM, Gurling H, Sklar P, Purcell S. A genomewide association study of response to lithium for prevention of recurrence in bipolar disorder. Am J Psychiatry. 2009;166(6):718–25.
Perlis RH, Mehta R, Edwards AM, Tiwari A, Imbens GW. Pharmacogenetic testing among patients with mood and anxiety disorders is associated with decreased utilization and cost: a propensity-score matched study. Depress Anxiety. 2018;35(10):946–52.
Phillips EJ, Sukasem C, Whirl-Carrillo M, Muller DJ, Dunnenberger HM, Chantratita W, Goldspiel B, Chen YT, Carleton BC, George AL Jr, Mushiroda T, Klein T, Gammal RS, Pirmohamed M. Clinical pharmacogenetics implementation consortium guideline for HLA genotype and use of carbamazepine and oxcarbazepine: 2017 update. Clin Pharmacol Ther. 2018;103(4):574–81.
Pickard BS. Genomics of lithium action and response. Neurotherapeutics. 2017;14(3):582–7.
Pisanu C, Melis C, Squassina A. Lithium pharmacogenetics: where do we stand? Drug Dev Res 2016;77(7):368–73.
Pisanu C, Congiu D, Costa M, Chillotti C, Ardau R, Severino G, Angius A, Heilbronner U, Hou L, McMahon FJ, Schulze TG, Del Zompo M, Squassina A. Convergent analysis of genome-wide genotyping and transcriptomic data suggests association of zinc finger genes with lithium response in bipolar disorder. Am J Med Genet B Neuropsychiatr Genet. 2018a;177(7):658–64.
Pisanu C, Heilbronner U, Squassina A. The role of pharmacogenomics in bipolar disorder: moving towards precision medicine. Mol Diagn Ther. 2018b;22(4):409–20.
Post RM. Preventing the malignant transformation of bipolar disorder. JAMA. 2018;319(12):1197–8.
Post RM, Leverich GS, Kupka R, Keck PE Jr, McElroy SL, Altshuler LL, Frye MA, Rowe M, Grunze H, Suppes T, Nolen WA. Clinical correlates of sustained response to individual drugs used in naturalistic treatment of patients with bipolar disorder. Compr Psychiatry. 2016;66:146–56.
Rao S, Han X, Shi M, Siu CO, Waye MMY, Liu G, Wing YK. Associations of the serotonin transporter promoter polymorphism (5-HTTLPR) with bipolar disorder and treatment response: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;89:214–26.
Relling MV, Klein TE. CPIC: clinical pharmacogenetics implementation consortium of the pharmacogenomics research network. Clin Pharmacol Ther. 2011;89(3):464–7.
Rybakowski JK, Abramowicz M, Szczepankiewicz A, Michalak M, Hauser J, Czekalski S. The association of glycogen synthase kinase-3beta (GSK-3beta) gene polymorphism with kidney function in long-term lithium-treated bipolar patients. Int J Bipolar Disord. 2013;1:8.
Saito T, Ikeda M, Mushiroda T, Ozeki T, Kondo K, Shimasaki A, Kawase K, Hashimoto S, Yamamori H, Yasuda Y, Fujimoto M, Ohi K, Takeda M, Kamatani Y, Numata S, Ohmori T, Ueno S, Makinodan M, Nishihata Y, Kubota M, Kimura T, Kanahara N, Hashimoto N, Fujita K, Nemoto K, Fukao T, Suwa T, Noda T, Yada Y, Takaki M, Kida N, Otsuru T, Murakami M, Takahashi A, Kubo M, Hashimoto R, Iwata N. Pharmacogenomic study of clozapine-induced agranulocytosis/granulocytopenia in a Japanese population. Biol Psychiatry. 2016;80(8):636–42.
Saito T, Ikeda M, Hashimoto R, Iwata N, Yamamori H, Yasuda Y, Fujimoto M, Kondo K, Shimasaki A, Kawase K, Miyata M, Mushiroda T, Ozeki T, Kubo M, Fujita K, Kida N, Nakai M, Otsuru T, Fukuji Y, Murakami M, Mizuno K, Shiratsuchi T, Numata S, Ohmori T, Ueno SI, Yada Y, Tanaka S, Kishi Y, Takaki M, Mamoto A, Taniguchi N, Sawa Y, Watanabe H, Noda T, Amano Y, Kimura T, Fukao T, Suwa T, Murai T, Kubota M, Ueda K, Tabuse H, Kanahara N, Kawai N, Nemoto K, Makinodan M, Nishihata Y, Hashimoto N, Kusumi I, Fujii Y, Miyata R, Hirakawa K, Ozaki N. Transethnic replication study to assess the association between clozapine-induced agranulocytosis/granulocytopenia and genes at 12p12.2 in a Japanese population. Biol Psychiatry. 2017;82(1):e9–10.
Sanchez-Iglesias S, Garcia-Solaesa V, Garcia-Berrocal B, Sanchez-Martin A, Lorenzo-Romo C, Martin-Pinto T, Gaedigk A, Gonzalez-Buitrago JM, Isidoro-Garcia M. Role of pharmacogenetics in improving the safety of psychiatric care by predicting the potential risks of Mania in CYP2D6 poor metabolizers diagnosed with bipolar disorder. Medicine (Baltimore). 2016;95(6):e2473.
Sathur Raghuraman B, Paul P, Nadella RK, Kapur V, Purushottam M, Jain S, Kannan R, Del Zompo M, Viswanath B. GSK-3b 50 T/C polymorphism in bipolar disorder and its relationship with clinical phenotypes and treatment response. J Affect Disord. 2018;241:433–5.
Serretti A. Genetics and pharmacogenetics of mood disorders. Psychiatr Pol. 2017;51(2):197–203.
Shine B, McKnight RF, Leaver L, Geddes JR. Long-term effects of lithium on renal, thyroid, and parathyroid function: a retrospective analysis of laboratory data. Lancet. 2015;386(9992):461–8.
Solomon HV, Cates KW, Li KJ. Does obtaining CYP2D6 and CYP2C19 pharmacogenetic testing predict antidepressant response or adverse drug reactions? Psychiatry Res. 2019;271:604–13.
Song J, Bergen SE, Di Florio A, Karlsson R, Charney A, Ruderfer DM, Stahl EA, Chambert KD, Moran JL, Gordon-Smith K, Forty L, Green EK, Jones I, Jones L, Scolnick EM, Sklar P, Smoller JW, Lichtenstein P, Hultman C, Craddock N, Landen M, Smoller JW, Perlis RH, Lee PH, Castro VM, Hoffnagle AG, Sklar P, Stahl EA, Purcell SM, Ruderfer DM, Charney AW, Roussos P, Michele Pato CP, Medeiros H, Sobel J, Craddock N, Jones I, Forty L, Florio AD, Green E, Jones L, Gordon-Smith K, Landen M, Hultman C, Jureus A, Bergen S, McCarroll S, Moran J, Smoller JW, Chambert K, Belliveau RA. Genome-wide association study identifies SESTD1 as a novel risk gene for lithium-responsive bipolar disorder. Mol Psychiatry. 2016;21(9):1290–7.
Song J, Sjolander A, Joas E, Bergen SE, Runeson B, Larsson H, Landen M, Lichtenstein P. Suicidal behavior during lithium and valproate treatment: a within-individual 8-year prospective study of 50,000 patients with bipolar disorder. Am J Psychiatry. 2017;174(8):795–802.
Spina E, de Leon J. Clinical applications of CYP genotyping in psychiatry. J Neural Transm (Vienna). 2015;122(1):5–28.
Squassina A, Manchia M, Borg J, Congiu D, Costa M, Georgitsi M, Chillotti C, Ardau R, Mitropoulos K, Severino G, Del Zompo M, Patrinos GP. Evidence for association of an ACCN1 gene variant with response to lithium treatment in Sardinian patients with bipolar disorder. Pharmacogenomics. 2011;12(11):1559–69.
Stern S, Linker S, Vadodaria KC, Marchetto MC, Gage FH. Prediction of response to drug therapy in psychiatric disorders. Open Biol. 2018;8(5):180031.
Szczepankiewicz A, Rybakowski JK, Suwalska A, Skibinska M, Leszczynska-Rodziewicz A, Dmitrzak-Weglarz M, Czerski PM, Hauser J. Association study of the glycogen synthase kinase-3beta gene polymorphism with prophylactic lithium response in bipolar patients. World J Biol Psychiatry. 2006;7(3):158–61.
Taranu A, Colle R, Gressier F, El Asmar K, Becquemont L, Corruble E, Verstuyft C. Should a routine genotyping of CYP2D6 and CYP2C19 genetic polymorphisms be recommended to predict venlafaxine efficacy in depressed patients treated in psychiatric settings? Pharmacogenomics. 2017;18(7):639–50.
Tobe BTD, Crain AM, Winquist AM, Calabrese B, Makihara H, Zhao WN, Lalonde J, Nakamura H, Konopaske G, Sidor M, Pernia CD, Yamashita N, Wada M, Inoue Y, Nakamura F, Sheridan SD, Logan RW, Brandel M, Wu D, Hunsberger J, Dorsett L, Duerr C, Basa RCB, McCarthy MJ, Udeshi ND, Mertins P, Carr SA, Rouleau GA, Mastrangelo L, Li J, Gutierrez GJ, Brill LM, Venizelos N, Chen G, Nye JS, Manji H, Price JH, McClung CA, Akiskal HS, Alda M, Chuang DM, Coyle JT, Liu Y, Teng YD, Ohshima T, Mikoshiba K, Sidman RL, Halpain S, Haggarty SJ, Goshima Y, Snyder EY. Probing the lithium-response pathway in hiPSCs implicates the phosphoregulatory set-point for a cytoskeletal modulator in bipolar pathogenesis. Proc Natl Acad Sci USA. 2017;114(22):E4462–e4471.
Tohen M, Hennen J, Zarate CM Jr, Baldessarini RJ, Strakowski SM, Stoll AL, Faedda GL, Suppes T, Gebre-Medhin P, Cohen BM. Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am J Psychiatry. 2000;157(2):220–8.
Tondo L, Vazquez G, Baldessarini RJ. Mania associated with antidepressant treatment: comprehensive meta-analytic review. Acta Psychiatr Scand. 2010;121(6):404–14.
Tonozzi TR, Braunstein GD, Kammesheidt A, Curran C, Golshan S, Kelsoe J. Pharmacogenetic profile and major depressive and/or bipolar disorder treatment: a retrospective, cross-sectional study. Pharmacogenomics. 2018;19(15):1169–79.
UKGTN. 2019a. Report_Gene_Test_Recommendations_CSAG_SEPT17_amend_353.pdf.
UKGTN. UK Genetic Testing Network. 2019b.
Valvezan AJ, Klein PS. GSK-3 and Wnt signaling in neurogenesis and bipolar disorder. Front Mol Neurosci. 2012;5:1.
Veldic M, Ahmed AT, Blacker CJ, Geske JR, Biernacka JM, Borreggine KL, Moore KM, Prieto ML, Vande Voort JL, Croarkin PE, Hoberg AA, Kung S, Alarcon RD, Keeth N, Singh B, Bobo WV, Frye MA. Cytochrome P450 2C19 poor metabolizer phenotype in treatment resistant depression: treatment and diagnostic implications. Front Pharmacol. 2019;10:83.
Wang Z, Li Z, Chen J, Huang J, Yuan C, Hong W, Yu S, Fang Y. Association of BDNF gene polymorphism with bipolar disorders in Han Chinese population. Genes Brain Behav. 2012;11(5):524–8.
Weinshilboum RM, Wang L. Pharmacogenomics: precision medicine and drug response. Mayo Clin Proc. 2017;92(11):1711–22.
Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Bond DJ, Frey BN, Sharma V, Goldstein BI, Rej S, Beaulieu S, Alda M, MacQueen G, Milev RV, Ravindran A, O’Donovan C, McIntosh D, Lam RW, Vazquez G, Kapczinski F, McIntyre RS, Kozicky J, Kanba S, Lafer B, Suppes T, Calabrese JR, Vieta E, Malhi G, Post RM, Berk M. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97–170.
Zarate CA Jr, Tohen M, Land M, Cavanagh S. Functional impairment and cognition in bipolar disorder. Psychiatr Q. 2000;71(4):309–29.
Zhang JP, Lencz T, Malhotra AK. D2 receptor genetic variation and clinical response to antipsychotic drug treatment: a meta-analysis. Am J Psychiatry. 2010;167(7):763–72.
Zhang JP, Robinson DG, Gallego JA, John M, Yu J, Addington J, Tohen M, Kane JM, Malhotra AK, Lencz T. Association of a schizophrenia risk variant at the DRD2 locus with antipsychotic treatment response in first-episode psychosis. Schizophr Bull. 2015;41(6):1248–55.
Zhang JP, Lencz T, Zhang RX, Nitta M, Maayan L, John M, Robinson DG, Fleischhacker WW, Kahn RS, Ophoff RA, Kane JM, Malhotra AK, Correll CU. Pharmacogenetic associations of antipsychotic drug-related weight gain: a systematic review and meta-analysis. Schizophr Bull. 2016;42(6):1418–37.
Acknowledgements
Not applicable.
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
ABCB and MAF conceived the idea, selected the studies, and wrote the original draft of the manuscript. All of the authors contributed with writing and revising the different versions of the manuscript. The final version of the manuscript was accepted by all authors before submission. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
AB Cuellar-Barboza reports no financial relationships with commercial interests. SL McElroy has been a consultant to or member of the scientific advisory boards of Allergan, Avanir, Bracket, F. Hoffmann-La Roche Ltd., Mitsubishi Tanabe Pharma America, Myriad, Opiant, Shire, and Sunovion. She has been a principal or co-investigator on studies sponsored by Allergan, Avanir, Azevan, Brainsway, Marriott Foundation, Medibio, Myriad, Neurocrine, Novo Nordisk, Shire, and Sunovion. She is also an inventor on United States Patent No. 6,323,236 B2, Use of Sulfamate Derivatives for Treating Impulse Control Disorders, and along with the patent’s assignee, University of Cincinnati, Cincinnati, Ohio, has received payments from Johnson & Johnson, which has exclusive rights under the patent. M Veldic reports no financial relationships with commercial interests. B Singh received research time support from Medibio, unrelated to the current study. S Kung reports no financial relationships with commercial interests. F Romo-Nava reports no financial relationships with commercial interests. N Nuñez reports no financial relationships with commercial interests. A Cabello-Arreola reports no financial relationships with commercial interests. B Coombes reports no financial relationships with commercial interests. M Prieto reports no financial relationships with commercial interests. HK Betcher reports no financial relationships with commercial interests. KM Moore reports no financial relationships with commercial interests. SJ Winham reports no financial relationships with commercial interests. JM Biernacka reports no financial relationships with commercial interests. MA Frye reports Grant Support from Assurex Health, Mayo Foundation, Medibio. Consultant (Mayo) - Actify Neurotherapies, Allergan, Intra-Cellular Therapies, Inc., Janssen, Myriad, Neuralstem Inc.,Takeda, Teva Pharmaceuticals. He reports CME/Travel/Honoraria from the American Physician Institute, CME Outfitters, Global Academy for Medical Education. Mayo Clinic has a financial interest in AssureRX and OneOme and the technology referenced in this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cuéllar-Barboza, A.B., McElroy, S.L., Veldic, M. et al. Potential pharmacogenomic targets in bipolar disorder: considerations for current testing and the development of decision support tools to individualize treatment selection. Int J Bipolar Disord 8, 23 (2020). https://doi.org/10.1186/s40345-020-00184-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40345-020-00184-3