Abstract
Background
Eating disorder treatment approaches and outcome studies have historically centered almost exclusively on cisgender populations. Transgender and nonbinary (TGNB) adults are underrepresented in general and intervention research despite being at increased risk for eating and body image-related problems.
Aims
This scoping review was designed to gather and examine the research with TGNB adults who experience eating and body image related problems, as well as clinical studies on the effectiveness of treatment approaches.
Method
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) was used for reporting this review. MEDLINE and PsychInfo were used as electronic databases for searching subject terms. Inclusion criteria for studies required the quantitative measurement or qualitative exploration of body image or eating for TGNB adults. The relevant data were extracted and summarized based on quantitative findings and qualitative themes.
Results
After review of over 1258 articles, 59 studies met criteria and data were extracted and summarized. Factors associated with eating disorders and body image problems across studies suggests gender-affirming medical interventions are effective and emphasized treatment for an eating disorder is warranted alongside gender affirming medical care. Body image was associated with eating patterns aimed at meeting gendered ideals of body shape and size. There was variation in guiding theories and absence of consensus in the definition of transgender in the review studies. This likely demonstrates the changing language, social acceptance of TGNB people and identities, diagnostic criteria, and clinical conceptualizations of eating and body image.
Conclusions
Future research should consider the use of theory for guiding inclusion of salient social factors influencing eating patterns, body image, and treatment outcomes. In addition, future research is needed that centers on nonbinary and genderqueer populations, as well as those from minoritized racial and ethnic groups to inform culturally appropriate concerns, needs, and treatment modalities.
Plain English Summary
Fifty-nine published research studies with transgender adults on eating patterns, body image, and associated risks and comorbidities were collected and summarized. Across studies, gender affirming medical interventions like hormone therapy and surgery were associated with decreases in eating disorder symptoms and improved body image. Studies from interviews with transgender adults found social causes for disordered eating and poor body image including rejection and discrimination. Future studies should use guiding theories for testing the causality and consider rejection and discrimination experienced by transgender adults.
Similar content being viewed by others
Background
Eating disorder treatment approaches and outcome studies have centered almost exclusively on cisgender (i.e., sex-assigned-at-birth aligns with gender identity) participants [1]. Transgender and nonbinary (TGNB; i.e., gender identity differs from sex-assigned-at-birth, inclusive of transmasculine, transfeminine, gender queer, and other genders) adults are underrepresented in research despite disproportionate prevalence rates of eating disorders and body image problems [2]. Gender dysphoria is associated with disordered eating, body image problems [3], and minority stress [4]. This may explain the higher prevalence rates of eating disorders and body image problems for TGNB people [2] and the need for innovations in treatment and intervention.
Minority stress: a guiding theory
A guiding theory for this review is Minority Stress Theory (MST) as it has been applied and expanded for TGNB people. MST, first theorized in the context of gay, lesbian, and bisexual people [5], posits there are external and internal stressors acting on the health and safety of TGNB adults [6]. External stressors include stigma, rejection, employment and housing discrimination, and violence experienced because someone is transgender. External stressors create internal stressors of self-rejection (i.e., internalized transphobia), increased gender dysphoria (e.g., psychological distress associated with gender identity not matching the body/sex-assigned-at-birth), expectations for rejections by others, and pressure to conceal transgender identity and gender expression [7]. Increased external and internal stressors, as MST posited [6], lead to poor physical and mental health [8] and eating and body image problems [4].
MST also proposes key protective factors for TGNB adults, including social acceptance in family, work, social, and healthcare settings (e.g., use of correct pronouns, name, and maintaining a relationship after disclosure of transgender identity), social changes (e.g., name and pronoun changes, gender marker), and access to medical services (e.g., puberty blockers, hormones, surgery, affirming psychotherapy and treatment) [6]. Acceptance and support are protective factors because they may reduce and, in some cases, eliminate gender dysphoria for TGNB adults [9]. Unsurprisingly, these lead to improvements in both mental health [10] and eating and body image-related problems [11]. There is a growing body of research to support using MST to explain differences in the health outcomes of TGNB people, which includes efforts to consider the compounding impact of multiple marginalized identities for TGNB people from minoritized ethnic and racial communities [12].
MST for TGNB research and in this scoping review considers psychological and social factors as significant contributors to outcomes of marginalized subgroups within the TGNB population. Thus, MST aids in identifying missing factors and subgroups (e.g., TGNB people from marginalized racial and ethnic groups) not included in the current literature body. It also provides a critical lens to the review analysis about the types of methods employed for studying TGNB experiences, the language used about TGNB patients, and the treatment approach and outcomes of TGNB people in healthcare. External stressors are experienced across social settings for TGNB people, including in healthcare and research participation, impacting their health and safety [13], thus MST guides this review to take a reflexive look at what empirical research is saying about TGNB adults.
Current study
MST posits that TGNB health outcomes will vary based on external and internal stressors, which are further influenced by mental health comorbidities, age, social acceptance, race/ethnic group, and access to gender affirming healthcare and treatment. MST offers a lens for examining the literature with TGNB adults with eating and body image related problems. As a result, this scoping review aimed to answer four research questions: 1) What methodologies are being used to study eating and body image related problems with TGNB people? 2) What are the risks and protective factors for eating and body image related problems? 3) Who is being included and excluded in the TGNB samples of studies on eating and body image related problems? 4) What are the empirically supported treatments for eating and body image problems for TGNB patients? The focus of this paper is on adults only. Adolescent and young adult literature is detailed in another scoping review (Authors, et al., under review).
Current analyses that center TGNB people are narrative in nature [14, 15], span broader sexual and gender minority populations [16], or provide a narrowed focus on diagnosis rates and symptom presentation [16,17,18]. To inform continued research and treatment innovations, we conducted a scoping literature review to critically examine research about TGNB adults who experience eating and body image problems and any clinical studies that detail treatment approaches and their effectiveness. This review expands on current analyses by incorporating studies that address eating disorder treatments and interventions, mental health comorbidities and gender dysphoria, and general eating patterns that are not necessarily disordered in nature. We also sought to include articles at the intersection of eating and body image given the theorized utility of disordered eating behaviors to attain a body size or shape that is an attempt to meet gendered appearance ideals. In this way, the scoping review maps the breadth of the literature and identifies gaps in the knowledge base [19].
Method
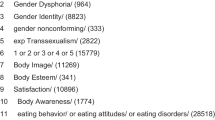
This literature review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines in the search, review, and reporting processes [20, 21]. The search strategy was developed through initial meetings and consultation between the first author and the university librarian (last author, MJ) in the fall of 2020. Preliminary searches were conducted using the OVID interface of possible databases including MEDLINE, PsychINFO, CINAHL: Cumulative Index to Nursing and Allied Health Literature, Cochrane Database of Systemic Reviews, Social work Abstracts, Social Services Abstracts, and Sociological Abstracts to identify potential articles about transgender adults and eating, body, and weight related problems. The second author (WL) was consulted based on her expertise to review initial searches for relevant articles. The preliminary searches demonstrated two databases—MEDLINE and PsychINFO– were superior for identifying relevant articles. To search the databases, the OVID interface was used, and official subject terms were identified for each database to ensure the use of consistent vocabulary. In MEDLINE, the search terms—transgender persons, gender identity, transsexualism, gender dysphoria, body image, body dissatisfaction, self-concept, feeding behavior, anorexia nervosa, binge eating, and bulimia nervosa—were used. The trans/gender terms and body/eating terms were then searched together for identifying articles where both subjects were categorized. A similar process was used for PsychINFO with the following subject terms—transgender, gender dysphoria, gender identity, gender nonconforming, transsexualism, body image, body esteem, body satisfaction, body dissatisfaction, body awareness, and eating behavior or attitudes or disorders. Eating behavior or attitudes or disorders subject terms included anorexia, bulimia nervosa, and binge eating disorders. No limits were set by date of publication in order to capture the changing theories and findings in the field up to literature published online or in print in December 2022.
Inclusion and exclusion criteria
Articles included in this review met the following criteria: 1) published in peer review journals (including online advance publications); 2) published in English language by December 2022; 3) described qualitative or quantitative empirical research (including case reports and case studies); 4) addressed review questions about eating behavior and body image including those addressing treatment and intervention; and 5) sample of transgender participants (inclusive of transgender men, women, nonbinary, and gender expansive or questioning) over the age of 18 years old. The following types of studies were excluded from the review: book chapters; review articles; editorial commentaries; clinical opinion articles without case or research data; non-English language studies; dissertations; studies where outcomes from transgender participant data were not reported separately from larger sample; and studies that did not include at least one of the following—eating behavior or disorder measurement, body image measurement, or interview data on eating or body image. Finally, we removed studies examining only young adults samples (ages 18 to 25) as a unique part of adolescent development [22]. These samples are included in our youth/young adult scoping review article (Authors et al., under review).
Review procedure and analysis
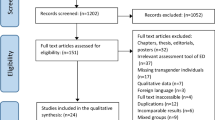
The identified articles were uploaded to Covidence©, an online software, for managing duplicate removal and then the processes of abstract review, full text review, and, finally, data extraction. Duplications were removed initially by the software. This was reviewed by the first author to ensure accuracy of the removal. Reviews were completed by three research team members (KHR, WL, SL) and four graduate research assistants. Pairs of authors and graduate research assistants reviewed abstracts based on the inclusion/exclusion criteria. Discrepancies in the reviews were resolved by the first and second authors. Then full text reviews were completed by the second and third authors and the graduate research assistants. Again, discrepancies were resolved by the first and second authors. Data extraction was completed by the second, third and fourth authors. Finally, one case control study article was removed at data extraction as two reviewers (KHR, SL) agreed that the study did not meet our inclusion criteria as transgender people were the subject of the work, but not the participants in the study [23]. The PRISMA figure (see Fig. 1) outlines the course of the review and article selection and extraction.
Data were finally downloaded from Covidence© to a spreadsheet developed by the first author where the sample characteristics, guiding theories, definitions of ‘transgender’ and/or language about gender, measurements, funding sources, limitations, bias, and other commentary were noted. The third and fourth authors led the data movement to the spreadsheet. Then analysis of the data followed three modalities. First, studies were separated by age to create youth (children to young adult where young adults were analyzed as unique developmental stage) and adult (adult-only samples, 18 years old and older with broad age ranges and analyzed together as an all-adult sample) tables for separate analysis. Again, this manuscript will only report on the adult samples and the youth and young adult articles are summarized in a separate scoping review manuscript (Heiden-Rootes et al. [24]).
Then, study methodology (quantitative, qualitative, and case report) was analyzed by the first and third authors. The method of articles was analyzed for identifying and quantifying types of methodology, sample size and demographics, measurement use, and geographic location. We sought to summarize and critique the current body of literature based on method and the limitations this may create for drawing conclusions and implications from the studies. Finally, variable outcomes (eating disorders, body image) were analyzed by the second and fourth authors. Variable outcomes were reported based on divergent and consistent findings across studies. In addition, unique findings were noted for subsamples, if appropriate. The outcome results were then narratively summarized.
To assess rigor and potential bias in studies, the authors used four items from the STrengthening the Reporting of OBservational Studies in Epidemiology (STROBE) checklist [25] and the Standards for Reporting Qualitative Research (SRQR) checklist [26] as previously used in systematic literature reviews with women with minoritized sexual identities [27]. This allowed for a critical review of study biases. The items were: (1) The authors describe the eligibility criteria and the sources, methods, and rationale of participant selection; (2) The authors describe the characteristics of study participants (coded “yes” if the authors provided information about age, race/ethnicity, and socioeconomic status); (3) The authors describe and provide a rationale for their quantitative or qualitative analytic methods; and (4) The authors discuss the limitations of the study, including sources of potential bias or imprecision. This allowed for the potential for bias to be assessed by the first and second author after data extraction of the results was completed. Finally, funding source was noted for gaging the degree of funding available for TGNB studies on eating and body image and for identifying entities who were investing in research with and for TGNB adults.
Results
The review identified 59 articles for inclusion (see Table 1 for PRISMA figure and Table 2 for Synthesis of Results by Research Question). The results section is organized by areas of analysis to answer the five research questions—bias and limitations, method analysis (including sample demographics and geographic location of studies), and summary results by topic area (eating problems, body image).
Bias and limitations
Review of bias and limitations across studies showed five studies lacked limitations sections and 10 studies were missing acknowledgments of potential biases in the study. Many of the studies lacked a full description of the methodology and demographics of the sample. Over 78% of studies (n = 47) did not include a guiding theory. Of the studies that did include theory, MST (n = 5; 8.5%) [6] and objectification theory (n = 4; 6.8%) [86] were the most commonly identified. In two cases, the studies drew on both MST and objectification theory. Most studies were not funded. Only 18 were funded from a mix of funders—federal or national sources (e.g., Dutch Ministry of Health; National Institute for Health) and internal university or medical system funding (e.g., Harvard Catalyst).
Some studies defined “transgender” and delineated non-binary or gender queer individuals in the samples. Where possible, non-binary and gender queer samples were analyzed in the results separately. Given the clinical nature of many of the studies and samples, some relied on the existence of gender dysphoria or the older diagnosis of gender identity disorder (n = 22). Three studies defined, and some diagnosed, transsexualism (e.g., Kirkpatrick et al., 2019; Kraemer, et al., 2008) now seen as outdated and offensive language. These studies seemed to be grounded in the diagnostic criteria and current language and clinical thinking about transgender identities. While other studies used less clinical terms, like transgender, gender minority, or gender nonconformity or incongruence and, in some cases, allowed for self-identification as part of the inclusion criteria. Some of the clinical samples lacking explicit definition of transgender denoted “male-to-female” or “female-to-male” gender transitions (n = 10) were in progress, complete, or the person was seeking gender affirming clinical medical care. Given the dated and potentially offensive language used in some of the studies, the results, discussion, and tables (see Tables 1 and 2), this article uses the terms transgender, trans men/women, and nonbinary where appropriate.
Method analysis
Quantitative findings
A total of 48 studies relied on quantitative measurements, scales, and analyses. Most of the articles retained for this study employed a cross-sectional study design (n = 46). Several different measures were used to assess the variables of interest, with the most common being the Eating Attitudes Test, Body Uneasiness Test, Symptoms Checklist-90, and Eating Disorders Inventory. The sample sizes of the quantitative studies were well-distributed from less than 50 to over 5000. Demographically, most quantitative studies did not report racial data as part of the sample characteristics, and of the studies that did report racial information, 14 included primarily racially White samples. Most of the quantitative studies originated from outside of the United States, including from Italy (n = 8), Sweden (n = 5), UK/England (n = 2), multicenter data from four European countries (n = 5), Germany (n = 4), Netherlands (n = 2), Belgium (n = 1), Turkey (n = 1), Iran (n = 1), Spain (n = 1), Canada (n = 1), Finland (n = 1), multicenter data from the United States, Canada, and Europe (n = 1). The remaining 15 quantitative studies included data collected only in the United States.
Two studies included both a cohort and cross-sectional element [50, 76]. Both studies assessed body image variables and focused on adult populations. Both studies included European samples; one included patients at a clinic in Italy [50], and the other included patients at gender clinics in the Netherlands, Belgium, and Germany [76]. The gender affirming interventions analyzed in these studies included hormone replacement therapy and gender-affirming surgeries. Six studies included in our analysis utilized a cohort design [41, 56, 59, 60, 76, 78]. All the cohort studies examined body image and most used sample sizes under 50 participants [41, 56, 59, 60]. Half of the cohort studies analyzed the impacts of surgical interventions [56, 60, 76], while others studied hormone replacement therapy [59] or a combination of hormonal and surgical gender-affirming interventions [41, 76]. A variety of measures for eating disorders and body image were used with very little overlap between studies. Two studies were conducted in the Netherlands, two were conducted in Sweden, and one was conducted in Switzerland.
Qualitative and case report studies
Within the articles retained for this scoping literature review of TGNB adults, 12 utilized a qualitative or case study approach. The case studies (n = 5) detailing one to five individual cases of gender dysphoria, eating disorders, body image and dissatisfaction, and obesity with quantitative and qualitative data presented. The findings from these case reports focused on psychiatric care [54] and eating disorder treatment [83]. Two case reports included detailed patient medical records [55, 71]. Four qualitative studies interviewed transgender people [48, 64, 87, 88]. Three of the interview articles included large qualitative sample sizes ranging from 30 to 98 transgender participants. Demographics of the samples in qualitative studies were younger with most being under age 35. Race and ethnicity were not always offered in the published article, though when reported was predominately racially White in samples from the United States. The interview articles with larger samples showed greater age and racial/ethnic diversity.
Eating disorders and treatment
Existing evidence related to eating patterns among the TGNB population centers on the prevalence, risk, and protective factors for eating disorders and disordered eating. In addition, many articles considered treatment outcomes and other clinical concerns for individuals who have been diagnosed with an eating disorder.
Eating disorders
Estimates of eating disorder and disordered eating prevalence among TGNB adults used surveys with smaller population samples [38] and medical records [45]. Medical records data from the United States found that among over 10,000 TGNB patients, between 0.15 and 1.37% were diagnosed a variety of feeding and eating disorders [45]. The prevalence studies sometimes grouped transgender participants into one category or further subdivided into trans man or trans woman identities in others. Most studies utilized validated measures to assess eating disorder risk including: the Eating Attitudes Test-26 (EAT-26) [4, 35, 40], the Eating Disorder Inventory (EDI) [28, 38, 84, 89], and the Eating Disorder Examination Questionnaire (EDE-Q). Others used select questions related to disordered eating patterns [29]. Two measures were tested for validity and reliability with TGNB adults—the EDE-Q and the Nine-Item Avoidant/Restrictive Food Intake Disorder Screen (NIAS). Nagata et al. [65] established community norms for the EDE-Q among adult transgender men, transgender women, and gender expansive individuals [2].
Correlates and risk factors
The existing body of research also addressed correlates, risk, and protective factors for eating disorders and disordered eating among the TGNB population. Correlations of disordered eating with other constructs were reported such as dehumanization, objectification, and discrimination [4], hyper-femininity [35], societal femininity ideals, and a feminine gender role orientation [38]. Vocks et al. (2009) reported differences in eating disturbances among those with gender identity disorder where transgender women reported higher restrained eating, eating concerns, weight concerns, shape concerns, drive for thinness, bulimia, body dissatisfaction, and body checking compared to cisgender women [80]. Transgender men reported higher restrained eating, weight concerns, shape concerns, body dissatisfaction, and body checking compared to cisgender men. Risk and for eating disorders were estimated from clinical survey data finding high body dissatisfaction, perfectionism, anxiety symptoms, low self-esteem [18].
Eating disorder treatment
Authors discussed approaches and treatment considerations for TGNB patients with eating disorders. Treatment considerations included management of coexisting mental health diagnoses [90] and the complex interplay between eating disorder psychopathology and one’s gender identity or gender dysphoria for adults [28, 54, 72]. For example, Hepp and Milos (2002) discussed the relationship between eating behaviors, gender identity, sexual orientation and body dissatisfaction using three case studies of transgender patients diagnosed with an eating disorder [54]. Ålgars et al. (2012) used semi-structured interviews to explore participants own understanding of the causes of their disordered eating; most participants reported experiences with disordered eating that were attributed to a desire to bring their bodies into alignment with their gender identity [28].
Studies on eating disorder treatment also addressed the impact of gender-affirming medical interventions on eating disorder symptomology or recovery using case studies [55, 91, 92] and clinical or survey data [18, 70, 71, 89]. Medical interventions included masculinizing or feminizing hormone therapy [18, 70, 71] and gender-affirming surgeries [55, 70, 71, 89]. Most of the evidence demonstrates eating disorder symptomology improves, but does not entirely resolve, with gender-affirming medical interventions. On the other hand, Turan et al. (2018) found that eating attitudes and behaviors did not significantly improve among transgender men after six months of hormone therapy [72]. Overall, authors of the existing research emphasized that although access to gender-affirming medical interventions may be critical to address the underlying cause, treatment of the eating disorder is still warranted.
Lastly, only two studies centered on the lived experiences of TGNB adults in eating disorder treatment. The studies described the role of the body in eating disorder treatment, negative experiences with clinicians, recommendations for treatment centers and providers caring for TGNB patients with eating disorders, the importance of centering the lived expertise of TGNB people about their experiences and needs [53], and barriers to accessing competent care [57]. Both emphasized the need to address gender dysphoria in eating disorder treatment [53, 57].
Body image—satisfaction, shame, and surveillance
Most studies (n = 44) examined a body image construct either as a primary finding or alongside eating disorders. Body image, as it applies to TGNB populations, utilized varied construct definitions leading to a variety of measures for body image including assessing body satisfaction, shame, and surveillance. Body shame referred to the perception of one’s body failing to meet cultural expectations of attractiveness that become internalized through objectification experiences [40]. Body surveillance, the constant and persistent monitoring of the body, was utilized in just three studies alongside other body image and eating disorder measures [4, 40, 79] for testing objectification theory. Some of the measures utilized included the Body Image Assessment Questionnaire (FBeK), the Body Cathexis Scale (BCS), Body Image Scale, Lindgren-Pauly Body Image Scale, Body Uneasiness Test, Body Dissatisfaction, and Fishers Body Image questionnaire.
Misgendering, or being referred to by the incorrect name, pronouns, or other language that does not align with one’s gender identity, was associated with decreased body satisfaction and restricted eating [63]. Negative body image was associated with altered eating patterns in two studies [40, 93]. Comiskey et al. (2020) found body shame was positively associated with disordered eating and the intention to alter one’s body due to the internalization of cultural standards of beauty for transgender women [40].
Body image was also measured to determine if treatment targeting body image could alleviate gender dysphoria and improve body image and mental health. Eight studies utilized body image as a variable with TGNB samples and included diagnosed conditions of body dysmorphia, gender incongruence, or gender identity disorder [9, 30, 32, 42, 46, 51, 56, 60]. Treatment considerations for TGNB individuals included clinical interventions of psychotherapy, gender affirming hormone therapy, medication, and genital/chest surgery [30, 51, 74, 78]. Those who received surgery reported improved body image and body satisfaction after the top and bottom surgery [76, 77, 89]. Those who received top surgery reported higher body satisfaction and psychological functioning second to improved body and gender identity congruence [77].
Discussion
Existing evidence supports the TGNB adult population experiences elevated rates of eating disorders and disordered eating when compared to cisgender populations [29]. There is, however, an inherent limitation to estimating eating disorder and disordered eating prevalence in that only an initial study offered measurement validity and reliability for use with TGNB adults [2]. TGNB individuals may utilize eating or exercise behaviors for purposes distinct from the cisgender population such as weight manipulation for a body size or shape that better aligns with one’s gender identity, pubertal and/or menstrual suppression, and masking of body features that do not align with one’s gender identity [61]. This creates a complex and common intersection of gender dysphoria, body image, and eating patterns for TGNB people [53, 57]. Despite recommendations to screen TGNB patients for eating disorders, existing measures on eating patterns may not be accurate or reliable with TGNB [2]. Future research should continue to validate existing measures for use among the TGNB individual from minoritized racial/ethnic groups, adapt existing measures to address considerations specific to TGNB patients who seek treatment, or develop and validate new measures.
The risk and protective factors identified in MST associated with eating disorders and body image problems across four decades of studies suggests gender-affirming medical interventions (i.e., gender affirming hormone therapy and surgeries) may alleviate eating disorder symptomology and negative body image [9, 11, 18, 31, 41, 49,50,51, 55, 56, 59, 60, 67, 69, 71, 72, 75,76,77,78, 85, 89]. Though the degree of social stigma [63], cultural standards of femininity and masculinity [35, 40, 79], internalized transphobia [73], lack of social support and acceptance [81], childhood trauma [32], and discrimination [4, 79, 81] experienced by TGNB adults also impacted symptomology limiting the impact of gender-affirming medical interventions alone. Therefore, traditional eating disorder treatment may still be warranted alongside gender-affirming medicine. Furthermore, additional treatment for addressing these minority stressors and promoting a positive body image for TGNB people that goes beyond stereotypical cultural standards are warranted [43].
The existing research is primarily observational in nature. Little is known about how TGNB patients may respond to eating disorder prevention or treatment approaches traditionally designed for cisgender populations. Riddle and colleagues responded that TGNB patients may show improved symptomology in higher levels of eating disorder treatment yet may experience more severe depression and show less improvement during treatment compared to cisgender patients [1]. In contrast, Duffy and colleagues reported that eating disorder treatment may be ineffective from the perspectives of TGNB adults and cause harm to due lack of clinician preparedness or mistreatment from healthcare providers [43]. Future research may explore the efficacy of eating disorder prevention and treatment approaches that are culturally adapted for TGNB adults, treatment for concurrent mental health conditions, as well as approaches to training healthcare professionals and students to provide competent care for TGNB adults. In this effort, MST could be introduced as a guiding theory for considering the social and relational context of discrimination, gender body norms, and structural barriers to health and healthcare.
The review found variations and absences in definitions of transgender, body image or shame, and guiding theories. This demonstrates the changing language, diagnostic criteria, emergence of MST over the past 40 years, and clinical conceptualizations of eating and body image as uniquely intertwined among TGNB populations. The studies rarely addressed social and interpersonal factors; either through theory or inquiry (e.g., including questions about family, relationships, employment, etc.) despite the significance of social supports and resources on the health of TGNB people demonstrated in MST. These social needs are lifelong for TGNB adults [94]. Future research that is inclusive of social factors for understanding eating patterns and body image would be well guided by MST for considering relational dependencies [95], housing stability, and food insecurity [96] that significantly shape eating patterns and health.
Many of the studies, especially qualitative studies, lacked racial and ethnic diversity in the samples and none looked at non-binary or gender queer individuals exclusively. This may reflect high concealment and the associated risk of violence experienced by TGNB people from minoritized racial groups [97] and observations of increased racially white, female-assigned at birth TGNB individuals accessing gender-affirming medical care in some areas of the United States [98]. In case reports and reviews with small sample sizes and known locations, demographic information and the stories of the patients increase the risk for making an already vulnerable TGNB person identifiable. Although case reports are common practice in medical sciences for exploring new phenomena and encouraging emergent treatment, it raises ethical concerns for use of single or identifiable patient records when there are known risks of discrimination and violence.
In addition, the purpose of the study, even in large sample sizes, may begin with a bias where individual academic medical professionals who are not utilizing MST as a framework for understanding the social determinants of health of TGNB people, could further pathologize TGNB patients in their care based on weight and eating patterns [99]. Therefore, future research may explore eating and body image among racially and ethnically marginalized groups of TGNB adults grounded in MST for identifying empirically known factors with a community-participatory action approach to methodology [100] for aiding in expanding and critiquing MST. The critique could draw from intersectionality for illuminating the experiences of those minoritized both racially and in terms of gender expression and identity [101]. Community-participatory designs can center the voices of TGNB people from racially and ethnically marginalized groups while paying for lived expertise as part of the research team. Successful use of this method has informed improved healthcare systems [102] and clinical education with TGNB adults [103]. Similarly, future research should center non-binary or genderqueer populations and their experiences through initial qualitative inquiry aimed at identifying potential cultural adaptations to eating disorder treatment and mental health services.
Limitations
This review has several limitations. The team carefully planned and utilized software to accurately answer the study questions and conduct the review. However, research studies may have been missed. The current studies still lack nuance by variations in gender identity, expression, and social factors. Limiting the search by English means other international studies were missed. Some of the studies included transgender and non-transgender samples, requiring reliance on portions of the data or only descriptive analysis. Many of the studies were cross-sectional in nature, limiting causal associations between risk factors, treatments, and outcomes documented in the studies. Finally, the rigor could have been enhanced by pre-registering our search protocol with the International Prospective Register of Systemic Reviews.
Conclusion
The scoping review offers an overview and examination of research with TGNB adults who experience eating and body image related problems as well as clinical studies on treatment approaches and effectiveness. The 59 studies identified demonstrated the significance of gender-affirming medical interventions for alleviating eating and body image issues though with limitations given the social stigma and discrimination experienced by TGNB people. Future research should consider the use of theory for guiding inclusion of salient social factors influencing eating patterns, body image, and treatment outcomes. In addition, more studies are needed with those from minoritized racial and ethnic groups and varied gender identities (e.g., nonbinary people) for identifying differences in needs and treatment modalities.
Availability of data and materials
Search terms and data retrieved through library searches are available upon request to the corresponding author. Data from searches is available upon request to the first author.
References
Riddle MC, Robertson L, Blalock DV, Duffy A, Le Grange D, Mehler PS, et al. Comparing eating disorder treatment outcomes of transgender and nonbinary individuals with cisgender individuals. Int J Eat Disord. 2022;55(11):1532–40.
Nagata JM, Ganson KT, Austin SB. Emerging trends in eating disorders among sexual and gender minorities. Curr Opin Psychiatry. 2020;33(6):562.
Jones BA, Haycraft E, Murjan S, Arcelus J. Body dissatisfaction and disordered eating in trans people: a systematic review of the literature. 2016.
Brewster ME, Velez BL, Breslow AS, Geiger EF. Unpacking body image concerns and disordered eating for transgender women: The roles of sexual objectification and minority stress. J Couns Psychol. 2019;66(2):131–42.
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674.
Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Prof Psychol Res Pract. 2012;43(5):460.
Rood BA, Reisner SL, Surace FI, Puckett JA, Maroney MR, Pantalone DW. Expecting rejection: understanding the minority stress experiences of transgender and gender-nonconforming individuals. Transgender Health. 2016;1(1):151–63.
Fontanari AMV, Vilanova F, Schneider MA, Chinazzo I, Soll BM, Schwarz K, et al. Gender affirmation is associated with transgender and gender nonbinary youth mental health improvement. LGBT Health. 2020;7(5):237–47.
Becker I, Auer M, Barkmann C, Fuss J, Moller B, Nieder TO, et al. A cross-sectional multicenter study of multidimensional body image in adolescents and adults with gender dysphoria before and after transition-related medical interventions. Arch Sex Behav. 2018;47:2335–47.
Hughto JM, Gunn HA, Rood BA, Pantalone DW. Social and medical gender affirmation experiences are inversely associated with mental health problems in a US non-probability sample of transgender adults. Archives of sexual behavior. 2020:1–13.
Owen-Smith AA, Gerth J, Sineath RC, Barzilay J, Becerra-Culqui TA, Getahun D, et al. Association between gender confirmation treatments and perceived gender congruence, body image satisfaction, and mental health in a cohort of transgender individuals. J Sex Med. 2018;15(4):591–600.
Millar K, Brooks CV. Double jeopardy: minority stress and the influence of transgender identity and race/ethnicity. Int J Transgender Health. 2022;23(1–2):133–48.
Levine S, Heiden-Rootes K, Salas J. Associations between healthcare experiences, mental health outcomes, and substance use among transgender adults. J Am Board Family Med. 2022;35(6):1092–102.
Obarzanek L, Munyan K. Eating disorder behaviors among transgender individuals: exploring the literature. J Am Psychiatr Nurses Assoc. 2021;27(3):203–12.
Parker LL, Harriger JA. Eating disorders and disordered eating behaviors in the LGBT population: a review of the literature. J Eat Disord. 2020;8(1):1–20.
Calzo JP, Blashill AJ, Brown TA, Argenal RL. Eating disorders and disordered weight and shape control behaviors in sexual minority populations. Curr Psychiatry Rep. 2017;19(8):1–10.
Coelho JS, Suen J, Clark BA, Marshall SK, Geller J, Lam P-Y. Eating disorder diagnoses and symptom presentation in transgender youth: a scoping review. Curr Psychiatry Rep. 2019;21(11):1–10.
Jones BA, Haycraft E, Bouman WP, Brewin N, Claes L, Arcelus J. Risk factors for eating disorder psychopathology within the treatment seeking transgender population: the role of cross sex hormone treatment. Eur Eat Disord Rev. 2018;26:120–8.
Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1–7.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Wood D, Crapnell T, Lau L, Bennett A, Lotstein D, Ferris M, et al. Emerging adulthood as a critical stage in the life course. Handbook of life course health development. 2018:123–43.
Mcdermid SA, Zucker KJ, Bradley SJ, Maing DM. Effects of physical appearance on masculine trait ratings of boys and girls with gender identity disorder. Arch Sex Behav. 1998;27(3):253–67.
Heiden-Rootes K, Linsenmeyer W, Levine S, Oliveras M. A Scoping Review of Research Literature on Eating and Body Image for Transgender and Nonbinary Youth (under review)
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51.
Thompson T, Heiden-Rootes K, Joseph M, Gilmore LA, Johnson L, Proulx CM, et al. The support that partners or caregivers provide sexual minority women who have cancer: a systematic review. Soc Sci Med. 2020;261:113214.
Algars M, Alanko K, Santtila P, Sandnabba NK. Disordered eating and gender identity disorder: a qualitative study. Eat Disord. 2012;20:300–11.
Algars M, Santtila P, Sandnabba NK. Conflicted gender identity, body dissatisfaction, and disordered eating in adult men and women. Sex Roles. 2010;63:118–25.
Auer MK, Liedl A, Fuss J, Nieder T, Briken P, Stalla GK, et al. High impact of sleeping problems on quality of life in transgender individuals: a cross-sectional multicenter study. PLoS ONE. 2017;12(2):e0171640.
Bandini E, Fisher AD, Castellini G, Lo Sauro C, Lelli L, Meriggiola MC, et al. Gender identity disorder and eating disorders: similarities and differences in terms of body uneasiness. J Sex Med. 2013;10(4):1012–23.
Bandini E, Fisher A, Ricca V, Ristori J, Meriggiola M, Jannini E, et al. Childhood maltreatment in subjects with male-to-female gender identity disorder. Int J Impot Res. 2011;23(6):276–85.
Bell K, Rieger E, Hirsch JK. Eating disorder symptoms and proneness in gay men, lesbian women, and transgender and non-conforming adults: comparative levels and a proposed mediational model. Front Psychol. 2019;9:2692. https://doi.org/10.3389/fpsyg.2018.02692. Erratum in: Front Psychol. 2019;10:1540.
Bozkurt A, Isikli H, Demir F, Ozmenler K. Nahit, Gulcat Z, Karlidere T, Aydin H. Body image and personality traits of male-to-female transsexuals and homosexuals. Soc Behav Personal Int J. 2006;34(8):927–938. https://doi.org/10.2224/sbp.2006.34.8.927.
Carretta RF, Szymanski DM, DeVore E. Predictors of disordered eating and acceptance of cosmetic surgery among drag queen performers. Body Image. 2019;30:64–74.
Case LK, Brang D, Landazuri R, Viswanathan P, Ramachandran VS. Altered white matter and sensory response to bodily sensation in female-to-male transgender individuals. Arch Sex Behav. 2017;46(5):1223-1237. https://doi.org/10.1007/s10508-016-0850-z.
Castellano E, Crespi C, Dell'Aquila C, Rosato R, Catalano C, Mineccia V, Motta G, Botto E, Manieri C. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest. 2015;38(12):1373–81. https://doi.org/10.1007/s40618-015-0398-0.
Cella S, Iannaccone M, Cotrufo P. Influence of gender role orientation (masculinity versus femininity) on body satisfaction and eating attitudes in homosexuals, heterosexuals and transsexuals. Eat Weight Disord Stud Anorexia Bulimia Obesity. 2013;18:115–24.
Chivers ML, Bailey JM. Sexual orientation of female-to-male transsexuals: a comparison of homosexual and nonhomosexual types. Arch Sex Behav. 2000;29(3):259-78. https://doi.org/10.1023/a:1001915530479.
Comiskey A, Parent MC, Tebbe EA. An inhospitable world: Exploring a model of objectification theory with trans women. Psychol Women Q. 2020;44(1):105–16.
de Vries AL, McGuire JK, Steensma TD, Wagenaar EC, Doreleijers TA, Cohen-Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. 2014;134(4):696–704.
Dharma C, Scheim AI, Bauer GR. Exploratory factor analysis of two sexual health scales for transgender people: Trans-Specific Condom/Barrier Negotiation Self-Efficacy (T-Barrier) and Trans-Specific Sexual Body Image Worries (T-Worries). Arch Sex Behav. 2019;48:1563–72.
Duffy ME, Henkel KE, Earnshaw VA. Transgender clients’ experiences of eating disorder treatment. J LGBT Issues Couns. 2016;10(3):136–49.
Fagan PJ, Wise TN, Derogatis LR, Schmidt CW. Distressed transvestites. Psychometric characteristics. J Nerv Ment Dis. 1988;176(10):626–32. https://doi.org/10.1097/00005053-198810000-00008.
Ferrucci KA, Lapane KL, Jesdale BM. Prevalence of diagnosed eating disorders in US transgender adults and youth in insurance claims. Int J Eat Disord. 2022;55(6):801–9. https://doi.org/10.1002/eat.23729.
Feusner JD, Dervisic J, Kosidou K, Dhejne C, Bookheimer S, Savic I. Female-to-male transsexual individuals demonstrate different own body identification. Arch Sex Behav. 2016;45(3):525–36.
Feusner JD, Dervisic J, Kosidou K, Dhejne C, Bookheimer S, Savic I. Female-to-Male Transsexual Individuals Demonstrate Different Own Body Identification. Arch Sex Behav. 2016;45(3):525-36. https://doi.org/10.1007/s10508-015-0596-z.
Finn M, Dell P. Practices of body management: transgenderism and embodiment. J Commun Appl Soc Psychol. 1999;9(6):463–76.
Fisher AD, Castellini G, Bandini E, Casale H, Fanni E, Benni L, et al. Cross-sex hormonal treatment and body uneasiness in individuals with gender dysphoria. J Sex Med. 2014;11(3):709–19.
Fisher AD, Castellini G, Ristori J, Casale H, Cassioli E, Sensi C, et al. Cross-sex hormone treatment and psychobiological changes in transsexual persons: two-year follow-up data. J Clin Endocrinol Metab. 2016;101(11):4260–9.
Gleming MZ, MacGowan BR, Robinson L, Spitz J, Salt P. The body image of the postoperative female-to-male transsexual. J Consult Clin Psychol. 1982;50(3):461–2.
Gagne P, Tewksbury R. Knowledge and power body and self: an analysis of knowledge systems and the transgendered self. Sociol Quart 1999;40(1):59–83. https://doi.org/10.1111/j.1533-8525.1999.tb02358.x.
Hartman-Munick SM, Silverstein S, Guss CE, Lopez E, Calzo JP, Gordon AR. Eating disorder screening and treatment experiences in transgender and gender diverse young adults. Eat Behav. 2021;41:101517.
Hepp U, Milos G. Gender identity disorder and eating disorders. Int J Eat Disord. 2002;32(4):473–8.
Hiraide M, Harashima S, Yoneda R, Otani M, Kayano M, Yoshiuchi K. Longitudinal course of eating disorders after transsexual treatment: a report of two cases. BioPsychoSocial Med. 2017;11(1):1–5.
Isung J, Mollermark C, Farnebo F, Lundgren K. Craniofacial reconstructive surgery improves appearance congruence in male-to-female transsexual patients. Arch Sex Behav. 2017;46:1573–6.
Joy P, White M, Jones S. Exploring the influence of gender dysphoria in eating disorders among gender diverse individuals. Nutr Diet. 2022;79(3):390–9.
Khoosal D, Langham C, Palmer B, Terry T, Minajagi M. Features of eating disorder among male-to-female transsexuals. Sex Relatsh Ther. 2009;24(2):217–229. https://doi.org/10.1080/14681990903082161.
Kilpatrick LA, Holmberg M, Manzouri A, Savic I. Cross sex hormone treatment is linked with a reversal of cerebral patterns associated with gender dysphoria to the baseline of cisgender controls. Eur J Neurosci. 2019;50(8):3269–81.
Kraemer B, Delsignore A, Schnyder U, Hepp U. Body image and transsexualism. Psychopathology. 2008;41(2):96–100.
Linsenmeyer W, Drallmeier T, Thomure M. Towards gender-affirming nutrition assessment: a case series of adult transgender men with distinct nutrition considerations. Nutr J. 2020;19:1–8.
Majid DS, et al. Neural systems for own-body processing align with gender identity rather than birth-assigned sex. Cereb Cortex. 2020;30(5):2897-2909. https://doi.org/10.1093/cercor/bhz282.
Mitchell L, MacArthur HJ, Blomquist KK. The effect of misgendering on body dissatisfaction and dietary restraint in transgender individuals: Testing a misgendering-congruence process. Int J Eat Disord. 2021;54(7):1295–301.
Morgan SW, Stevens PE. Transgender identity development as represented by a group of transgendered adults. Issues Ment Health Nurs. 2012;33(5):301–8.
Nagata JM, et al. (2020) Community norms for the Eating Disorder Examination Questionnaire (EDE-Q) among transgender men and women. Eat Behav. 2020;37:101381. https://doi.org/10.1016/j.eatbeh.2020.101381.
Nikkelen SWC, Kreukels BPC. Sexual Experiences in Transgender People: The Role of Desire for Gender-Confirming Interventions, Psychological Well-Being, and Body Satisfaction. J Sex Marital Ther. 2018;44(4):370–381. https://doi.org/10.1080/0092623X.2017.1405303.
Nowaskie DZ, Filipowicz AT, Choi Y, Fogel JM. Eating disorder symptomatology in transgender patients: differences across gender identity and gender affirmation. Int J Eat Disord. 2021;54(8):1493–9.
Rabito Alcón MF, et al. Body image in persons with gender dysphoria. Medwave. 201515;15(4):e6138.
Simbar M, Nazarpour S, Mirzababaie M, Emam Hadi MA, Ramezani Tehrani F, Alavi MH. Quality of life and body image of individuals with gender dysphoria. J Sex Marital Ther. 2018;44(6):523–32.
Testa RJ, Rider GN, Haug NA, Balsam KF. Gender confirming medical interventions and eating disorder symptoms among transgender individuals. Health Psychol. 2017;36(10):927–36.
Turan S, Poyraz CA, Duran A. Prolonged anorexia nervosa associated with female-to-male gender dysphoria: a case report [References]. Eat Behav. 2015;18:54–6.
Turan S, Aksoy Poyraz C, Saglam NGU, Demirel OF, Haliloglu O, Kadioglu P, et al. Alterations in body uneasiness, eating attitudes, and psychopathology before and after cross-sex hormonal treatment in patients with female-to-male gender dysphoria. Arch Sex Behav. 2018;47:2349–61.
Uniacke B, Glasofer D, Devlin M, Bockting W, Attia E. Predictors of eating-related psychopathology in transgender and gender nonbinary individuals. Eat Behav. 2021;42:101527.
van de Grift TC, Cohen-Kettenis PT, Elaut E, De Cuypere G, Richter-Appelt H, Haraldsen IR, et al. A network analysis of body satisfaction of people with gender dysphoria. Body Image. 2016;17:184–90.
van de Grift TC, Cohen-Kettenis PT, Steensma TD, De Cuypere G, Richter-Appelt H, Haraldsen IR, et al. Body satisfaction and physical appearance in gender dysphoria. Arch Sex Behav. 2016;45:575–85.
van de Grift TC, Elaut E, Cerwenka SC, Cohen-Kettenis PT, De Cuypere G, Richter-Appelt H, et al. Effects of medical interventions on gender dysphoria and body image: a follow-up study. Psychosomatic Med. 2017;79(7):815–23.
van de Grift TC, Elfering L, Greijdanus M, Smit JM, Bouman M-B, Klassen AF, et al. Subcutaneous mastectomy improves satisfaction with body and psychosocial function in trans men. Plast Reconstr Surg. 2018;142(5):1125–32.
van de Grift TC, Kreukels BPC, Elfering L, Ozer M, Bouman M-B, Buncamper ME, et al. Body image in transmen: Multidimensional measurement and the effects of mastectomy. J Sex Med. 2016;13(11):1778–86.
Velez BL, Breslow AS, Brewster ME, Cox R Jr, Foster AB. Building a pantheoretical model of dehumanization with transgender men: Integrating objectification and minority stress theories. J Couns Psychol. 2016;63(5):497–508.
Vocks S, Stahn C, Loenser K, Legenbauer T. Eating and body image disturbances in male-to-female and female-to-male transsexuals. Arch Sex Behav. 2009;38:364–77.
Watson RJ, Veale JF, Saewyc EM. Disordered eating behaviors among transgender youth: probability profiles from risk and protective factors. Int J Eat Disord. 2017;50(5):515–22.
Weyers S, Elaut E, De Sutter P, Gerris J, T'Sjoen G, Heylens G, De Cuypere G, Verstraelen H. Long-term assessment of the physical, mental, and sexual health among transsexual women. J Sex Med. 2009;6(3):752–60.
Winston AP, Acharya S, Chaudhuri S, Fellowes L. Anorexia nervosa and gender identity disorder in biologic males: a report of two cases. Int J Eat Disord. 2004;36(1):109–13.
Witcomb GL, Bouman WP, Brewin N, Richards C, Fernandez-Aranda F, Arcelus J. Body image dissatisfaction and eating-related psychopathology in trans individuals: a matched control study. Eur Eat Disord Rev. 2015;23(4):287–93.
Wolfradt U, Neumann K. Depersonalization, self-esteem and body image in male-to-female transsexuals compared to male and female controls. Arch Sex Behav. 2001;30(3):301–10.
Fredrickson BL, Roberts TA. Objectification theory: toward understanding women’s lived experiences and mental health risks. Psychol Women Q. 1997;21(2):173–206.
Idrus NI, Hymans TD. Balancing benefits and harm: Chemical use and bodily transformation among Indonesia’s transgender waria. Int J Drug Policy. 2014;25(4):789–97.
Gagne P, Tewksbury R. Knowledge and power, body and self: An analysis of knowledge systems and the transgendered self. Sociol Q. 1999;40(1):59–83.
Khoosal D, Langham C, Palmer B, Terry T, Minajagi M. Features of eating disorder among male-to-female transsexuals. Sex Relation Therapy. 2009;24(2):200–17.
Wagner R, Stevens JR. Clinical barriers to effective treatment of eating disorders and co-occurring psychiatric disorders in transgendered individuals. J Psychiatr Pract. 2017;23(4):284–9.
Ewan LA, Middleman AB, Feldmann J. Treatment of anorexia nervosa in the context of transsexuality: a case report. Int J Eat Disord. 2014;47(1):112–5.
Ristori J, Fisher AD, Castellini G, Sensi C, Cipriani A, Ricca V, et al. Gender dysphoria and anorexia nervosa symptoms in two adolescents. Arch Sex Behav. 2019;48(5):1625–31.
Cibich M, Wade TD. Treating bulimia nervosa in the context of gender dysphoria using 10-session cognitive behavior therapy. Int J Eat Disord. 2019;52(5):602–6.
Persson DI. Unique challenges of transgender aging: Implications from the literature. J Gerontol Soc Work. 2009;52(6):633–46.
Toomey RB. Advancing research on minority stress and resilience in trans children and adolescents in the 21st century. Child Development Perspectives. 2021.
Henderson ER, Jabson J, Russomanno J, Paglisotti T, Blosnich JR. Housing and food stress among transgender adults in the United States. Ann Epidemiol. 2019;38:42–7.
Rood BA, Maroney MR, Puckett JA, Berman AK, Reisner SL, Pantalone DW. Identity concealment in transgender adults: A qualitative assessment of minority stress and gender affirmation. Am J Orthopsychiatry. 2017;87(6):704.
Zhang Q, Rechler W, Bradlyn A, Flanders WD, Getahun D, Lash TL, et al. Changes in size and demographic composition of transgender and gender non-binary population receiving care at integrated health systems. Endocr Pract. 2021;27(5):390–5.
Vincent BW. Studying trans: recommendations for ethical recruitment and collaboration with transgender participants in academic research. Psychol Sex. 2018;9(2):102–16.
Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–23.
Wesp LM, Malcoe LH, Elliott A, Poteat T. Intersectionality research for transgender health justice: a theory-driven conceptual framework for structural analysis of transgender health inequities. Transgender Health. 2019;4(1):287–96.
Radix AE, Lelutiu-Weinberger C, Gamarel KE. Satisfaction and healthcare utilization of transgender and gender non-conforming individuals in NYC: a community-based participatory study. LGBT Health. 2014;1(4):302–8.
Linsenmeyer W, Stiles D, Drallmeier T, Heiden-Rootes K, Rahman R, Buxbaum E, et al. Advancing inclusion of transgender identities in health professional education programs: the interprofessional transgender health education day. J Allied Health. 2023;52(1):24.
Acknowledgements
Several research assistants contributed to the review process for identifying inclusion and excluded articles for the final analysis including Shannon Sabol and Abby Lawrence.
Funding
This study was funded by the Saint Louis University Applied Health Sciences Research Grant Program (#000561).
Author information
Authors and Affiliations
Contributions
Heiden-Rootes contributed to all parts of the design, acquisition of articles, analysis, interpretation, written drafts of the manuscript; Linsenmeyer contributed to all parts of the design, analysis, interpretation, written drafts of the manuscript; Levine contributed to analysis, interpretation, and written drafts of the manuscript; Oliveras contributed to analysis, interpretation, and written drafts of the manuscript; Joseph contributed to design and acquisition of the articles.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The scoping literature review was considered a non-human subject’s research by our university Internal Review Board.
Consent for publication
Consent for publication was not needed for this review study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Heiden-Rootes, K., Linsenmeyer, W., Levine, S. et al. A scoping review of the research literature on eating and body image for transgender and nonbinary adults. J Eat Disord 11, 111 (2023). https://doi.org/10.1186/s40337-023-00828-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40337-023-00828-6