Abstract
Background
During the last two decades, adolescent obesity has increased in western countries. In Iran-as a developing country- the prevalence of obesity is raised among youngsters as well. This study conducted to identify an association of adolescents’ loneliness, self-confidence and relationship with others in home and school environment with their weight status.
Methods
In this cross-sectional national survey, 5682 students aged 10–18 years from urban and rural districts of 27 provinces of Iran were selected via stratified multi-stage sampling method. Data on psychological problems of students was gathered through a questionnaire. Height, weight, and waist circumferences were measured according to standard protocols. Body mass index (BMI) and waist- to-height ratio was calculated.
Results
Boys which did not have best friends, spend time with their friends after school or get acceptance from them, had higher BMI than others. Only girls who did not spend time with their friends had higher BMI (19.48 ± 4.28) vs. (19.09 ± 3.92) and WC (71.04 ± 21.29) vs. (69.15 ± 17.43) than others, P < 0.05. In both sexes, adolescents who had sense of pressure about doing homework or had difficulties in relationship with their parents had higher BMI and WC values. Girls who reported being victim of violent behaviors (being bullied), had lower BMI compared to others. Risk of being overweight and obese, but not abdominal obese was statistically higher in adolescents not having close friends (OR = 1.81, CI: 1.11–2.95). Lack of self-confidence increased only the risk of obesity in teens (OR = 1033, CI: 1.09–1.64).
Conclusions
Our findings suggest that strategies for prevention of overweight and obesity in adolescent should be taking into account a deeper knowledge of psychosocial issues due to be able to design more effective programs for treating overweight teens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
During last two decades, adolescent obesity has increased in western countries [1]. In Iran-as a developing country- the prevalence of obesity is raised among youngsters as well [2]. The overall prevalence of obesity and overweight remained relatively constant during 2000 to 2004 and 2005 to 2010 and are estimated to be about 5.1 % (95 % confidence interval [CI], 4.4–5.8) and 10.8 % (95 % CI, 10.2–11.4), respectively [3]. Overweight children and adolescents may experience some psychosocial problems such as depression, social isolation, and poor self-confidence, dissatisfaction with body-image, reduced quality of life, family disharmony and trouble with teachers [4]. Current epidemiological data show that up to 20 % of children and adolescents suffer from a mental health problem and up to 50 % of these problems onset in adolescence. In the other words, adolescence is a substantial period for development of mental disorders such as depression [5]. Most obese adolescents remain obese as adults, so this age group is an important group for designing preventive programs addressing issues of health promotion, (e.g., body satisfaction, sociability, diet and sedentary behaviors). Overweight and obese adolescents with good body image are more likely to control their weight [6] whereas adolescents with poor body image are at risk for weight gain [7]. Social engagement may affect adolescent body satisfaction [8]. Engaging with friends and a social resource may increase socio-emotional maturity and self-confidence in adolescents [9]. In depressed adolescents the risk for development and persistence of obesity during adolescence are increased [10]. Depression can stimulate neuro-endocrine responses. Activation of Hypothalamic-pituitary axis and sympathetic nervous system may induce abdominal adiposity, insulin resistance and metabolic syndrome through increasing cortisol production [11]. Positive association between some psychological factors (e.g. depression in adolescence) and BMI during adulthood was observed [1]. Clinicians need to identify and help them to address the psychosocial factors that may be contributing to their child’s or adolescent’s obesity. Affected individuals may suffer from depression, low self-esteem, bullying, and weight bias, experiences that can make achieving desired health outcomes more difficult [12]. Most studies assessed the shared biological and psychosocial determinants of obesity-due to cross-sectional design- they are unable to detect causal relationships. Whether factors like low self-esteem and depression lead to obesity or whether obesity causes them, remains unclear [1]. Therefore, studies to determine psychosocial factors that may distinguish obese and overweight adolescents from their peers are needed.
Objectives
This study is conducted to evaluate association of anthropometric measures with some psychosocial factors in nationally representative sample of Iranian adolescents.
Methods
This national level cross-sectional study was performed in 2009–2010 as the third survey of the school-based surveillance system entitled Childhood and Adolescence Surveillance and PreventIon of Adult Non communicable disease (CASPIAN-III) Study in Iran. It was a multicentre study performed among 5682 school students (96 % participation rate), aged 10–18 years, living in urban and rural areas of 27 provinces in the Iran. Details on the study protocol have been described before [13] and here we report it in brief. The sample size was calculated according to the multistage cluster sampling method. The maximum sample size that could give a optimal estimate of all risk factors of interest was selected. Thus, the sample size was calculated as 210 subjects in each province. A total of 21 clusters of 10 subjects in each of the provinces and a total of 5670 students and an equal number of their parents were selected from 27 provinces. Children and adolescents were selected by multistage random cluster sampling from urban and rural areas of each provinces of Iran.
Required approvals have been documented from ethical committees of Isfahan University of Medical sciences (IUMS), Tehran University of Medical sciences (TUMS), and other relevant regulatory organizations at national and provincial levels. The Data and Safety Monitoring Board of the project closely supervised the quality control and quality assurance of the survey at the national level.
All procedure of data gathering and data managing were conducted carefully anonymously under security considering.
The project team obtained written informed consent from parents and oral assent from students. They selected school students by multistage random cluster sampling. Schools were stratified according to location (urban or rural), and the socioeconomic characteristics of their catchment area, taking into consideration the proportion of the different types of schools (public or private) to avoid socioeconomic bias.
Data on psychological problems of students was gathered through a questionnaire based on the standard protocols of WHO global school-based student health survey with participation of trained teams of expert health care providers. The validity and reliability of this questionnaire was approved in previous studies [14, 15]. The questionnaires content validity was evaluated by expert after translation; then two pilot studies were carried out on 120 students in Tehran. After each pilot study, the questions with any difficulty in understanding were modified. In the next step, the questionnaire validation was assessed divided by each group of questions related to a specific item (the Cronbach’s reliability coefficient >0.7). Home and school environment and psychosocial status of students were measured by 18 questions. Relationship with friends was measured by the first 5 questions; if the students gave a positive answer to these questions, it count on as a predictor of having good relationship. In the latter 5 questions, the answer A or B was taken as a predictor of having good sense in school environment [14]. Two questions measured being victim of violent behavior (being bullied) or bulling to others, while self-rated relationship difficulties with family members and friends was assessed by a 5 items. Students were asked to choose an option that indicated their status (Appendix 1: Table 4).
Height, weight, and waist circumferences were measured according to standard protocols with calibrated instruments. Weight was measured to the nearest 200 g in barefoot and lightly dressed condition. Body mass index (BMI) was calculated as weight (Kg) divided by height squared (m2) as index of obesity. Waist circumference (WC) was measured by a nonelastic tape to the nearest 0.2 cm at the end of expiration at the midpoint between the top of iliac crest and the lowest rib in standing position.
Waist- to-height ratio (WHtR), computed by dividing waist circumference (cm) to height (cm), was considered as an index of abdominal obesity [16]. We used the WHO growth curves to define BMI categories, i.e., overweight as gender-specific BMI for age of > +1 z-score, and obesity as gender-specific BMI for > +2 z-score [13]. Abdominal obesity was defined as waist to height ratio more than 0.5 [17].
The data entry staff entered data for all forms and questionnaires twice and checked for completeness and inconsistencies. The data checking process was conducted first at the district and then at the national level [13].
To assess the Screen Time (ST behaviors), the average number of hours per day that participants spent watching TV/VCDs, personal computer (PC), or electronic games [3] asked, and then the total cumulative spent time for ST was estimated. Information recorded separately for week days and weekends. According to the international ST recommendations, ST was categorized into two groups ; less than 2 h per day (Low) , and 2 h per day or more (High) [18, 19].
Through a validated questionnaire, information of past week weekly frequency of leisure time physical activity outside the school was collected. Having physical activity considered as at least 30 min duration of exercises per day which was led to heavy sweating or large increases in breathing or heart rate. Based on this provided definition, participants described their weekly PA habits through three available response choices as follow; none, 1–2 days, 3–6 days, and every day. For statistical analysis, each weekly frequency categorized into three groups; less than two times per week (Mild), two to four times a week (Moderate) and more than 4 times a week (Vigorous) [20].
The method and variables, which was used for calculating Socioeconomic status(SES) was approved previously in the Progress in the International Reading Literacy Study (PIRLS) [21]. In this study, in order to construct socioeconomic using principle component analysis (PCA) variables including parents’ education, parents’ job, possessing private car, school type (public/private), type of home (private/rented) and having personal computer in home were summarized in one main component. Using 25 % and 75 % percentiles, students were categorized into low, intermediate and high socioeconomic status.
Statistical analyses
Continuous and categorical variables are expressed as mean (SD) and number (percentage) respectively. Logistic and linear regression was used to indicate the most important psychosocial and environmental predictors of general and abdominal obesity in Iranian adolescents. A P-value of less than 0.05 was considered as statistically significant. All statistical analyses were performed using programs available in the STATA package using survey data analysis method.
Results
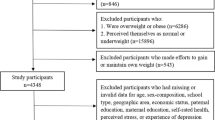
A total number of 5570 out of 5670 invited students completed the study (participation rate: 98.23 %). The average age of participants’ was 14.72 ± 2.40 years, without significant difference among girls and boys. Students consisted of 2848 (50.1 %) boys and 2835 (49.9 %) boys; 67.4 % from urban and 29.6 % from rural areas. The prevalence of overweight, generalized and abdominal obesity was 8.0 %, 8.9 % and 15.8 % respectively (Table 1).
Appendix 2: Table 5 compares mean of BMI and WC between adolescents with and without psychosocial and environmental problems. Boys which did not have best friends, spend time with their friends after school or get acceptance from them, had higher BMI than others. Only girls who did not spend time with their friends had higher BMI and WC than others. In both sexes, adolescents who had sense of pressure about doing homework did not feel good about their progress nor had difficulties in relationship with their parents had higher BMI and WC values. Girls who reported being victim of violent behaviors (being bullied), had lower BMI compared to others.
As shown in the Appendix 3: Table 6, having best friends and relationship with friends specially spending time with them after school was related to lower prevalence of overweight, obesity, and central obesity. Self-confidence only in boys led to lower obesity prevalence than adolescents lacking self-confidence.
Odds of being overweight and obese, but not abdominal obese was statistically higher in adolescents not having close friends. Moreover, adolescents who spent more time with friends after school and returning to home, had lower chance to overweight, obesity, and abdominal obesity. Lack of self-confidence increased only the risk of obesity in teens. Having difficulties in relationship with family members (parents, brothers and sisters) and friends are the predictors of overweight and obesity, too (Table 2).
Increment in BMI and WC with psychosocial and emotional problems was remained statistically significant after adjusting for age, sex, living area (urban or rural), and family history of chronic disease, mother’s education, father’s education, physical activity, and socioeconomic status (Table 3).
Discussion
In this study we found that some psychosocial problems such as lack of self-confidence and proper communication with family members, friends and teachers are related to overweight, general and abdominal obesity in adolescents; however, the direction of this relationship is not very clear.
A review by Nieman revealed that overweight children and adolescents may experience deleterious psychosocial sequelae, including depression, teasing, social isolation and discrimination, diminished self-esteem, behavioural problems, dissatisfaction with body-image, and reduced quality of life [12]. Based on previous studies obesity was associated with body image dissatisfaction in boys and girls [22]. Caccavale et al. [23] found that the prevalence of overweight/obesity was higher in boys than girls but reporting body image dissatisfaction in girls is more than boys. Also the relationship between weight status and body image was moderated by social engagement only for girl adolescents. In boys, regardless of their weight status, social engagement was associated with more body image satisfaction. The gender difference may be related to the fact that girls are more likely to use social comparisons that can increase body dissatisfaction and incorrect weight-control methods in adolescent girls [24].
Most of overweight or obese adolescents may be struggling with poor body image. Obesity and poor body image are main risk factors for low self-confidence and depression, and can lead to psychosocial problems [25]. Also eating disorders may occur, which can increase the risk for weight gain [26].
Friedman et al. reported that body image satisfaction partially mediated the relationship between degree of overweight and depression/self-esteem [27]. Other study stated that body image might explain the poor self-esteem of overweight girl adolescents [28]. In a study on Turkish adolescents, body dissatisfaction was associated with poor self-esteem and depression. Also being overweight was associated with poor self-esteem, but not with depression. This study revealed that actual weight was not associated with poor self-esteem and depression. So they suggest that psychological well-being is more related to body satisfaction than actual weight status [29].
Another study revealed that early onset of obesity has a negative effect on body image in adult life; it means that emerging the obesity in younger people increases the risk of body dissatisfaction, which can impair self-esteem [30].
The results about the relationship between overweight/obesity and psychopathology in different studies are inconsistent. In a study on school-aged adolescents in Ghana and Uganda a psychosocial factor (e.g. loneliness) was significantly associated with overweight or obesity [31]. In a longitudinal study Goodman and his colleague found that the risk for persistence and developing obesity during adolescence is increased at depressed adolescents [32].
In Stice’s study body image dissatisfaction was a significant determinant in predicting for developing adolescent girls depression later [33].
Recent studies revealed that weight criticism and body dissatisfaction caused to lower participation in vigorous physical activity, among overweight girls [34]. Eating behaviors disorders and unhealthy weight control methods among overweight adolescents is more often than others [35].
The associations of overweight, body image, and depressive symptoms may be related to the influence of pubertal development in adolescents. It means that pubertal timing and velocity of transition is related to body fat accumulation, which may be related to different experience of body image concerns and risk of depression. In pubertal development, both growth and sex hormones cause to increase in fat mass accumulation and because of this additional body fat, puberty is related to enhancing the risk of body dissatisfaction [36].
Depression was negatively associated with breakfast consumption behavior in Indian adolescents [37]. The findings of Indian study are in line with similar studies carried out in developed countries which suggested that depression is negatively associated with healthy dietary behaviors such as consuming breakfast, lunch and dinner [38]. A Meta-analytic study found that there was no significant relationship between obesity and depression in the population [39].
Ozmen et al., in their study revealed that overweight based on BMI had no effect on self-esteem and depression [39]. Also, Kim and his colleague stated that weight status based on BMI was not a good predictor for the level of self-esteem and depression [40]. The level of self-esteem and anxiety of obese adolescents did not differ from normal weight ones [41]. In a clinical population, a higher ratio of depression, behavioral problems, poor self-esteem was reported [42]. A literature review study revealed that the relationship between self-esteem and obesity was unclear whether self-esteem was consistently related to obesity [43]. So, there are multiple patterns for association between overweight/obesity and psychosocial risk factors in adolescents. It means that there are some other factors which can mediate the relationship between obesity and psychosocial distress.
In a study carried out on Portuguese adolescents, there was no significant difference between the number of close friends and obesity whereas potential social isolation was associated with overweight among the subjects. Also this study revealed that making new friends was more difficult for obese and overweight adolescents in comparison to non-obese and non-overweight peers [1]. These overweight children and adolescents with co-morbid psychiatric problems and issues with socialization and self-esteem need special interventions [44].
Study limitations and strengths
This study provides valuable information about weight status and some psychosocial factors of adolescents living in Iran. However, this study has some limitations. We didn’t assess household structure (child living with: both parent, mother only, father only, and grandparents only) regarding the risk of overweight and obesity. Therefore, more studies are needed to further explore the role of household structure in the context of parental influences on weight status and some psychosocial factors.
Conclusion
Our findings may greatly contribute to better understanding the association of weight disorders and some psychosocial factors adolescents. The high prevalence of adolescent boys (33.9 %) and girls (27.4 %) who were overweight/ obese in this nationally representative sample, along with the consistent association between overweight/obesity and psychosocial variables highlight the need for concurrent interventions for two problems in adolescents.
Abbreviations
CASPIAN, Childhood and Adolescence Surveillance and PreventIon of Adult Non communicable disease
References
Fonseca H, Matos MG. Perception of overweight and obesity among Portuguese adolescents: an overview of associated factors. Eur J Public Health. 2005;15(3):323–8.
Mehrkash M, Kelishadi R, Mohammadian S, Mousavinasab F, Qorbani M, Hashemi M. Obesity and metabolic syndrome among representative sample of Iranian adolescents. South East Asian J Trop Med Public Health. 2012;43(3):756–63.
Kelishadi R, Haghdoost A-A, Sadeghirad B, Khajehkazemi R. Trend in the prevalence of obesity and overweight among Iranian children and adolescents: A systematic review and meta-analysis. Nutrition. 2014;30:393–400.
Puhl R, Stigma JL. obesity, and the health of the nation’s children. Psychol Bull. 2007;133(4):557–80.
Zahedi H, Kelishadi R, Heshmat R, Motlagh M, Ranjbar S, Ardalan G, et al. Association between junk food consumption and mental health in a national sample of Iranian children and adolescents: the CASPIAN-IV study. Nutrition. 2014;30(11–12):1391–7.
Bahreynian M, Qorbani M, Motlagh ME, Heshmat R, Ardalan G, Kelishadi R. Association of Perceived Weight Status versus Body Mass Index on Adherence to Weight-modifying plan Among Iranian Children and Adolescents: The CASPIAN-IV Study. Indian Pediatr. 2015;52(10):857–63.
Neumark-Sztainer DPS, Hannan PJ, Haines J, Story M. Does body satisfaction matter? Five year longitudinal associations between body satisfaction and health behaviors in adolescent females and males. J Adolesc Health. 2006;39:244–51.
Gerner B, Wilson P. The relationship between friendship factors and adolescent girls’ body image concern, body dissatisfaction, and restrained eating. Inter J Eat Disor. 2005;37:313–20.
Witvliet M, Brendgen M, Lier P, Koot H, Vitaro F. Early adolescent depressive symptoms: Prediction from clique isolation, loneliness, and perceived social acceptance. J Abnorm Child Psychol. 2010;38:1045–56.
Goodman E, Whitaker R. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;109:497–504.
Anagnostis P, Athyros V, Tziomalos K, Karagiannis A, Mikhailidis D. Clinical review: The pathogenetic role of cortisol in the metabolic syndrome: A hypothesis. J Clin Endocrinol Metab. 2009;94(8):2692–701.
Nieman P, LeBlanc C. Psychosocial aspects of child and adolescent obesity. Paediatr Child Health. 2012;17(3):205–6.
Kelishadi R, Heshmat R, Motlagh M, Majdzadeh R, Keramatian K, Qorbani M, et al. Methodology and early findings of the third survey of CASPIAN study: A national school-based surveillance of students’ high risk behaviors. Int J Prev Med. 2012;3:394–401.
Zakeri M, Sedaghat M, Motlagh M, Ashtiani R, Ardalan G. BMI correlation with psychiatric problems among 10–18 years Iranian students. Acta Med Iran. 2012;50(3):177–84.
Kelishadi R, Majdzadeh R, Motlagh ME, Heshmat R, Aminaee T, Ardalan G, et al. Development and evaluation of a questionnaire for assessment of determinants of weight disorders among children and adolescents: the Caspian-IV study. Int J Prev Med. 2012;3(10):699–705.
Cook S, Auinger P, Li C, Ford E. Metabolic syndrome rates in United States adolescents, from the National Health and Nutri¬tion Examination Survey, 1999–2002. J Pediatr. 2008;152(2):165–70.
Knowles KM, Paiva LL, Sanchez SE. Waist circumference, body mass index, and other measures of adiposity in predicting cardiovascular disease risk factors among peruvian adults. Int J Hyperten. 2011;2011:1–10.
American Academy of Pediatrics. Children, adolescents, and television. Pediatrics. 2001;107(2):423.
Salmon J, Campbell K, Crawford D. Television viewing habits associated with obesity risk factors: a survey of Melbourne schoolchildren. Med J Aust. 2006;184(2):64.
Drenowatz C, Carlson J, Pfeiffer K, Eisenmann J. Joint association of physical activity /screen time and diet on CVD risk factors in 10-year-old children. Front Med. 2012;6(4):428.
Caro D, Cortés D. Measuring family socioeconomic status: An illustration using data from PIRLS 2006. 2012.
Mond J, Berg P, Boutelle K, Hannan P, Neumark-Sztainer D. Obesity, body dissatisfaction, and emotional well-being in early and late adolescence: Findings from the project EAT study. Journal of Adolescent Health. 2011;48:373–8.
Caccavale L, Farhat T, Iannotti R. Social engagement in adolescence moderates the association between weight status and body image. Body Image. 2012;9(2):221–6.
Ricciardelli L, Williams R, Kiernan M. Bulimic symptoms in adolescent girls and boys. Int J Eat Disord. 1999;26(2):217–21.
van den Berg PA, Mond J, Eisenberg M, Ackard D, Neumark-Sztainer D. The link between body dissatisfaction and self-esteem in adolescents: Similarities across gender, age, weight status, race/ ethnicity, and socioeconomic status. J Adolesc Health. 2010;47:290–6.
Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan P, Mulert S. Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. Int J of Obes. 2002;26:123–31.
Friedman K, Reichmann S, Costanzo P, Musante G. Body image partially mediates the relationship between obesity and psychological distress. Obes Res. 2002;10:33–41.
Pesa J, Syre T, Jones E. Psychosocial differences associated with body weight among female adolescents: the importance of body image. J Adolesc Health. 2000;26:330–7.
Ozmen D, Ozmen E, Ergin D, et al. The association of self-esteem, depression and body satisfaction with obesity among Turkish adolescents. BMC Public Health. 2007;7:80.
Wardle J, Waller J, Fox E. Age of onset and body dissatisfaction in obesity. Addict Behav. 2002;27:561–73.
Peltzer K, Pengpid S. Overweight and obesity and associated factors among school-aged adolescents in Ghana and Uganda. Int J Environ Res Public Health. 2011;8:3859–70.
Goodman E, Whitaker R. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504.
Stice E, Hayward C, Cameron R, et al. Body-image and eating disturbances predict onset of depression among female adolescents: a longitudinal study. J Abnorm Psychol. 2000;109(3):438–44.
Jensen C, Steele R. Brief report: Body dissatisfaction, weight criticism, and self-reported physical activity in pre-adolescent children. J Pediatr Psychol. 2009;34(8):822–6.
Haines J, Neumark-Sztainer D, Eisenberg M, Hannan P. Weight teasing and disordered eating behaviors in adolescents: Longitudinal findings from Project EAT (Eating Among Teens). Pediatrics. 2006;117(2):E209–E15.
Xie B, Wu Q, Chou C. Overweight, body image, and depression in asian and hispanic adolescents. Am J Health Behav. 2010;34(4):476–88.
Arora M, Nazar G, Gupta V, Perry C, Reddy K, Stigler M. Association of breakfast intake with obesity, dietary and physical activity behavior among urban school-aged adolescents in Delhi, India: results of a cross-sectional study. BMC Public Health. 2012;12:881.
Fulkerson J, Sherwood N, Perry C, Neumark-Sztainer D, Story M. Depressive symptoms and adolescent eating and health behaviors: a multifaceted view in a population-based sample. Prev Med. 2004;38:865–75.
Faith M, Matz P, Jorge M. Obesity-depression associations in the population. J Psychosom Res. 2002;53:935–42.
Kim O, Kim K. Body weight, self-esteem, and depression in Korean Female Adolescents. Adolescence. 2001;36:315–22.
Pastore D, Fisher M, Friedman S. Abnormalities in weight status, eating attitudes, and eating behaviours among urban high school students correlation with self-esteem and anxiety. J Adolesc Health. 1996;18:312–9.
Erermis S, Cetin N, Tamar M, Bukusoglu N, Akdeniz F, Goksen D. Is obesity a risk factor for psychopathology among adolescents? Pediatr Int. 2004;46:296–301.
French S, Story M, Perry C. Self-esteem and obesity in children and adolescents: a literature review. Obes Res. 1995;3:479–90.
Kalra G, Sousa AD, Sonavane S, Shah N. Psychological issues in pediatric obesity. Ind Psychiatry J. 2012;21(1):11–7.
Acknowledgments
The authors are appreciated large team working in this study, as well as the participants and their families. The present study was funded by the Child Health Promotion Research Center Isfahan University of Medical Sciences and Endocrinology and Metabolism Research Center of Tehran University of Medical Sciences.
Authors’ contributions
RH, RK and HA conceived of the study and revised the manuscript. FB participated in study design and wrote draft of the manuscript. MQ conceived of the study and carried out the statistical analysis. FM, GA, HA, MEM, MM and SMA participated in its design and implementation. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Author information
Authors and Affiliations
Corresponding authors
Appendix
Appendix
Appendix 1
Appendix 2
Appendix 3
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Baygi, F., Kelishadi, R., Qorbani, M. et al. Association of some psychosocial factors with anthropometric measures in nationally representative sample of Iranian adolescents: the CASPIAN-III study. J Diabetes Metab Disord 15, 15 (2015). https://doi.org/10.1186/s40200-016-0237-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40200-016-0237-7