Abstract
Background
Elderly individuals with type 2 diabetes mellitus (T2DM) suffer from several comorbidities, which affect their health outcomes, as well as process of care. This study assessed process and intermediate clinical outcomes of diabetes care among elderly individuals with T2DM and co-occurring Parkinson’s disease(PD).
Methods
This study used a retrospective cohort design with propensity score matching using Humana Medicare Advantage Part D claims database (2007-2011) and included elderly (age ≥ 65 years) Medicare beneficiaries with T2DM (identified by ICD-9-CM code of 250.x0 or 250.x2). PD was identified using ICD-9-CM code of 332.xx. After propensity score matching there were 2,703 individuals with T2DM and PD and 8,109 with T2DM and no PD. The three processes of care measures used in this study included: (i) HbA1c test; (ii) Lipid test; (iii) and Nephropathy screening. Intermediate clinical outcomes consisted of glycemic and lipid control.
Results
Multivariable conditional logistic regressions revealed that elderly individuals with T2DM and PD were 12 % (AOR: 0.88, 95 %CI: 0.79-0.97) and 18 % (AOR: 0.82, 95 %CI: 0.72-0.94) less likely to meet the annual American Diabetes Association (ADA) recommended HbA1c and lipid testing goals respectively compared to individuals with T2DM and no PD. Multinomial conditional logistic regressions showed that elderly individuals with T2DM and PD were more likely to have HbA1c and lipid (HbA1c < 8 %; LDL-C <100 mg/dl; HDL-C ≥ 50 mg/dl; triglyceride <150 mg/dl; and total cholesterol <200 mg/dl) control.
Conclusions
Among elderly individuals with T2DM, those with PD were less likely to achieve ADA recommended annual HbA1c and lipid testing compared to those without PD. However, PD individuals were more likely to achieve intermediate glycemic and lipid control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type-2 Diabetes Mellitus (T2DM) and its complications are the leading causes for morbidity and mortality in the United States (U.S.) [1]. Parkinson’s disease (PD) is a progressive neurodegenerative disease characterized by muscular tremor, slowing of movement, partial facial paralysis, peculiarity of gait and posture [2, 3]. Individuals with co-occurring T2DM and PD can have poor quality of life, impaired health and functional status. Moreover, co-occurring T2DM and PD require medical care from different specialties such as neurologists and endocrinologist, and require care in different settings including home-based as well as facility-based care [4]. Co-occurring T2DM and PD can pose significant challenges to diabetes management.
However, clinical guidelines for diabetes management for those with T2DM and PD are lacking. In general, guidelines for clinical practice are developed based on the expert consensus and the scientific evidence for a single disease state [5]. Standards of care and quality of care improvement efforts are based on these guidelines for clinical practice for individual disease state. As for example, there are separate guidelines for treating diabetes (such as the guidelines of the American Diabetes Association) and PD (European Parkinson’s disease Standards of Care Consensus Statement).
Studies on diabetes care among individuals with other co-occurring chronic conditions have revealed mixed findings. One study conducted among veterans with diabetes seeking care in seven different Veterans Affairs (VA) facilities from July 2007 through June 2008 reported that veterans with T2DM were more likely to receive overall good quality for all three quality measures (glycemic, blood pressure and low density lipoprotein-cholesterol control) combined (adjusted OR, 2.17; 95 % CI, 1.96–2.39) [6]. Whereas, another study using the INTERMED classification system for case complexity found that greater complexity (defined as higher INTERMED scores) among individuals with T2DM was associated with higher HbA1c values [7]. Therefore, it is not known whether clinical complexity is associated with poor or better outcomes among individuals with T2DM.
Despite there being no separate guideline recommendations regarding diabetes process of care (e.g., bi-annual HbA1c testing) in the presence of neurodegenerative conditions, it can be perceived that meeting at least the usual diabetes process of care recommendations is critical to providing appropriate care to elderly individuals with T2DM and PD. However, to the best of our knowledge, no prior study have explored the diabetes process of care among elderly individuals with co-occurring T2DM and PD. The results from the current study will fill a critical knowledge gap regarding the current standards of care among individuals with co-occurring T2DM and PD.
A study of diabetes management among elderly with T2DM and PD is important for several reasons. It has been estimated that by 2030, the prevalence of PD will increase by approximately two-folds due to the aging U.S. population [8] and will become a major public health concern in near future. Moreover, existing literature suggests that the presence of T2DM aggravates neurodegeneration and therefore there is a need of controlling T2DM to prevent further deterioration [9–11]. Hence, the primary aim of this study is to assess the process and intermediate clinical outcomes of diabetes care among elderly individuals with T2DM and PD compared to those with T2DM and no PD.
Methods
Study design
A retrospective cohort design with matched case–control approach was used for the purposes of this study. Those with T2DM and PD were considered as cases and those with T2DM and no PD were considered as controls. Controls were selected using propensity score method, which adjusted for gender, age, and diabetes complications severity index (DCSI). The algorithm developed by Chang and colleagues was used to measure the severity of diabetes using DCSI [12]. One case was matched to three controls based on 8 to 1 GREEDY matching technique using propensity score. For 8 to 1 GREEDY matching, the cases and control with same propensity score till the 8th digit are matched, and if they do not match on 8 digits, then it goes to 7-digit matching and so on. The GREEDY matching technique employs a sample without replacement algorithm and if there are more than one matches, then selection of control becomes random. Similar approach for propensity score matching have been used in existing literature to minimize the effect of bias and confounding [13]. Controls were selected from the same calendar year as the cases; if individuals were identified with PD in 2008, all controls were from 2008. If elderly Medicare beneficiaries did not have PD in the initial years and then developed it later during the study time period, they were removed from the control pool.
Elderly individuals with T2DM were followed for a period of 24 months with 12-month baseline period and 12 month follow-up period. Baseline period was defined based on the identification of T2DM and PD. For example, if T2DM and PD cases were identified in 2007, 2007 served as the baseline year, and 2008 served as the follow-up period. Process of care and intermediate clinical outcomes were measured during the follow-up year (i.e., 2008).
Data source
The Humana Medicare Advantage Part D database (MAPD) from January 01, 2007 through December 31, 2011 was used for this study. The Humana claims database consists of more than 12 million current and previous enrollees among which approximately 2 million enrollees are from MAPD plans. This study used medical, prescription, laboratory claims and person enrollment summary files. The medical claims contained information related to the type of plan, treatment date, type of admission (trauma, elective, emergency etc.), inpatient length of stay, diagnosis and procedural codes, and total Medicare allowable charges associated with each claim. Prescription claims included information on prescription fill date, medication dispensed, quantity of medication dispensed, net amount paid by Humana and out-of-pocket costs for enrollees. The laboratory Claims contained information on lab test identifying codes, lab results and abnormal value indicator. However, laboratory results are available only for approximately 30 % of the laboratory claims. The patient enrollment summary file included information on the MAPD enrollees’ age, sex, race/ethnicity, and enrollment dates.
Study population
The study population consisted of elderly Medicare beneficiaries (≥65 years) with T2DM. Elderly Medicare beneficiaries with T2DM were identified by the presence of a minimum of one inpatient or two outpatient visits (at least of 30 days apart) with a primary or secondary diagnosis of T2DM [International Classification of Diseases 9th Modification (ICD-9-CM) code: 250.x0 or 250.x2] [14].
Inclusion criteria
Other inclusion criteria were: (i) continuous enrollment of 24 months (12-month baseline and 12-month follow-up); and (ii) receipt of at least one oral antidiabetic drug (OAD) or insulin during the baseline year.
Dependent variables
Process of care
The three processes of care measures used in this study included: (i) HbA1c testing; (ii) lipid testing; and (iii) nephropathy screening. These measures were considered to meet the American Diabetes Association (ADA) guidelines if: (1) HbA1c testing was conducted at least two times a year with a gap of at least three months; (2) lipid testing was conducted at least once a year; and (3) nephropathy screening was conducted at least once a year [15]. A detailed description of the CPT and HCPCS codes are provided in Appendix.
Intermediate clinical outcomes
Glycemic control
HbA1c > 9 % represents poor glycemic control and is considered to be a poor performance marker among all elderly individuals with T2DM [16]. One study has used HbA1c < 7 % as representative of optimal glycemic control [16]. However, due to the risk of hypoglycemia, less stringent criteria of HbA1C < 8 % is often considered as acceptable glycemic control among elderly individuals with comorbid conditions, or long standing diabetes or multiple medication use [17]. Therefore, glycemic control outcomes were classified into two groups based on HbA1c values as follows: (i) < 8 % and (ii) ≥ 8 % only among those with available HbA1c values during follow-up year (N = 4,983).
Lipid control
Lipid control outcomes were based on Low Density Lipoprotein Cholesterol (LDL-C), High Density Lipoprotein Cholesterol (HDL-C), triglycerides, and total cholesterol. These lipid control outcomes were categorized based on the American Diabetes Association guidelines [15]. LDL-C was categorized as follows: (i) <100 mg/dl and (ii) ≥ 100 mg/dl. HDL-C was categorized into two for both men and women as follows: (i) ≤ 50 mg/dl; and (ii) > 50 mg/dl. Triglycerides were classified into: (i) <150 mg/dl; and (ii) ≥ 150 mg/dl. Total cholesterol was divided into groups as follows: (i) < 200 mg/dl; and (ii) ≥ 200 mg/dl. Again these were restricted to individuals with available LDL-C (N = 2,497), HDL-C (N = 4,833), total cholesterol (N = 2,543) and triglycerides (N = 2,535) values during the follow-up year.
Key independent variable: presence of PD
The key independent variable for all analyses was presence or absence of PD. Identification of PD was achieved by using ICD-9-CM code of 332.xx during the baseline year. The diagnosis of PD was ascertained by the presence of at least one inpatient or two outpatient visits (30 days apart) with a primary or secondary diagnosis of PD (ICD-9-CM code: 332.xx) [18].
Independent variables
Patient complexities
According to the American Geriatric Society (AGS) guidelines, individuals having specific conditions such as cognitive impairment, depression, fall and falls risk, polypharmacy, and urinary incontinence should be provided individualized treatment [19]. These characteristics were measured during the baseline period. Elderly Medicare beneficiaries were considered to have cognitive impairment due to physical illnesses if they had a diagnosis of Huntington’s disease, delirium, dementia, amnestic and other cognitive disorders; whereas if they have a diagnosis of bipolar disorder, schizophrenia and other psychotic disorders, they were considered to have cognitive impairment due to mental illnesses. Elderly Medicare beneficiaries were considered to have any cognitive impairment if they had either mental and/or physical cognitive impairment. To identify accidental falls, E-codes E880 through E888 were used whereas V-code V15.88 was used as a proxy measure for falls risk [20]. Number of therapeutic classes of prescribed medications was used to define polypharmacy, and was categorized into quintiles: (i) 0–0, (ii) 1–1, (iii) 2–3, (iv) 4–5, and (v) 6–31.
Dominant comorbid conditions
Using the framework of Kerr and Piette, cancer, end stage renal disease, and end stage liver disease were included as a dominant comorbid condition in this study [21].
Other independent variables
The current study adapts elements from the Vector model of Complexity proposed by Safford and colleagues to categorize other independent variables associated with complex comorbidities [22]. Socio-economic variables consisted of (i) Medicare prescription drug coverage gap; and (ii) insurance status (Private Fee-for-service, Health Maintenance Organization, and other insurance). Environmental factors consisted of (i) region (South, Mid-West, and Other regions). The cultural factors was defined by race/ethnicity (Whites, African- Americans, Hispanics, and Others). The behavioral factors consisted of baseline emergency room visits, and baseline home health visits.
Statistical analyses
Unadjusted differences in process and intermediate clinical outcomes among elderly individuals with and without Parkinson’s disease were determined using chi-square tests. Conditional Logistic regression analyses and conditional multinomial logistic regression analyses were conducted for binary dependent variables and dependent variables with more than two levels respectively. As 30 % of the study cohort did not have laboratory values, sample selection models were used to test selection bias among individuals with and without laboratory values for misspecification bias due to non-randomly missing data. This was accomplished using “heckprob” selectivity corrected regression. These models consisted of a selection equation in which the presence or absence of laboratory values were modelled. In the outcome equation, the intermediate clinical outcomes were modelled. For example, for HbA1c control, a logistic regression on the presence or absence of HbA1c values was conducted. In the outcome equation, glycemic control (<8 % and ≥ 8 %) was modelled. The Wald test of independence showed that the chi-square probability value was 0.7968 indicating that there is no influence of unobserved variables on glycemic control outcome in this dataset. Similar findings were observed with the lipid outcomes. Therefore, we report results from analyses among elderly individuals with available HbA1C values and lipid values.
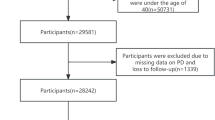
Propensity score matching
Before propensity score matching, there were 2,727 individuals with PD and diabetes (cases), and 249,763 individuals with diabetes only (controls). After propensity score matching and removing pairs with inexact matches, there were 2,703 individuals with PD and diabetes and 8,109 individuals with diabetes only (1:3 case to control matching). The cohort development is depicted in Fig. 1. Age and Diabetes Complications Severity Index (DCSI) total were continuous variables and the group differences in these two variables were ascertained by t-tests. For gender the group differences were ascertained by using chi-square. The number of individuals with PD before and after matching in each year are different because of the fact that we found that 1,282 individuals without PD in previous years were diagnosed with PD in the following year, and as these individuals were included in the control dataset for a particular year, they were deleted from the control dataset so that we do not have overlap between case and control group during matching. For each year, the individuals with PD in the matched sample were unique cases.
The two groups were matched on age, gender and DCSI scores. The c-statistics of the logistic regression to calculate propensity score for each year were found to be satisfactory (around 0.70). From Tables 1 and 2, it can be noted that, before propensity score matching, the two groups differed significantly from each other in terms of age, DCSI total and gender distribution. Before matching, among individuals with T2DM and PD, the total mean DCSI score was significantly higher compared to those with only diabetes. In terms of age, individuals with PD and diabetes had a significantly higher mean age as compared to those with diabetes only prior to propensity score matching. The PD and diabetes group had significantly higher number of males as compared to the group with diabetes only before matching. The propensity score matched sample was found to be well balanced in terms of the variables that were used to match the two groups. After matching there were no significant differences between the two groups in terms of age, DCSI and gender. From the bottom panel of Tables 1 and 2, it can be noted that when the 4 panels (2007–2008, 2008–2009, 2009–2010, and 2010–2011) were stacked, there were no statistically significant group differences in terms of age, gender and DCSI.
Results
Description of study sample by PD status
Table 3 exhibits baseline characteristics of T2DM elderly individuals with and without PD. There was significantly higher proportion of African-Americans (14.4 %) among individuals without PD. Overall, both the groups had higher proportions of whites (75.7 % and 74.3 % of individuals with and without respectively). In terms of region and plan types, there were higher proportion of individuals in the South region (around 75 %) and Health Maintenance Organizations in both the groups (around 48 %). There was significantly higher proportion of individuals who did not reach donut hole (56.6 %) among individuals with only diabetes, whereas the group with PD and diabetes had higher proportions of individuals entering (44.9 %) and having entry and exit information regarding donut hole (17.7 %). Individuals with PD and diabetes had significantly greater proportion of polypharmacy users in the higher quintiles (4–5, and 6–31). With respect to the conditions specific to elderly individuals, individuals with PD and diabetes had significantly higher proportion of urinary incontinence (10.4 %), major depressive disorders (26.7 %), cognitive impairment (33.4 %), and falls and falls risk (9.9 %). Individuals with PD had higher proportion of baseline emergency room (55.5 %) and baseline home health visit (60.9 %).
Bivariate and multivariate analyses of process of care and intermediate clinical outcomes
Table 4 summarizes the findings of bivariate and multivariate analyses in terms of process of care measures and intermediate clinical outcomes. Overall, 66.84 % had ADA recommended HbA1c testing. A lower percentage of individuals with PD received HbA1c testing (63.7 %) compared to those without PD (67.9 %, P-value <0.001). An overwhelming majority of individuals with T2DM received lipid testing (84.65 %). A lower percentage of elderly individuals with PD (80.4 %) received lipid testing compared to those without PD (86.1 %, p-value < 0.001). No statistically significant differences were observed in the two groups in terms of nephropathy screening. Among elderly individuals with available HbA1C values, an overwhelming majority had HbA1C value of < 8 % in both individuals with PD (86 %) and without PD (83.8 %). Elderly individuals with PD had statistically significantly better intermediate clinical outcomes compared to those without PD in terms of LDL-C < 100 mg/dl (75.5 % vs. 69.8 %), triglycerides < 150 mg/dl (63.8 % vs. 58.6 %), total cholesterol < 200 mg/dl (87.2 % vs. 83 %) and HDL-C ≥ 50 mg/dl (39.8 % vs. 35.7 %).
The upper panel of the right hand portion of Table 4 shows the results of conditional logistic regression analyses conducted with HbA1c testing as the dependent variable adjusting for the matched pair design. After controlling for Parkinson’s disease, race/ethnicity, region, plan-type, donut hole, polypharmacy, urinary incontinence, depression, falls and fall risk, cognitive impairment due to physical conditions, cognitive impairment due to mental conditions, dominant conditions, baseline emergency room visits, baseline home health visits and adjusting for the matched pair design, it was observed that individuals with PD were 12 % (AOR: 0.88, 95 % CI: 0.79-0.97) and 18 % (AOR: 0.82, 95 % CI: 0.72-0.94) less likely to meet the annual ADA recommended HbA1c and lipid testing respectively compared to individuals without PD. However, there were no statistically significant difference between individuals with and without PD in terms of nephropathy testing (AOR: 0.99, 95 % CI: 0.88-1.10).
The lower panel of the right hand portion of Table 4 shows the results from conditional multinomial logistic regression with glycemic control as the dependent variable. After adjusting for Parkinson’s disease, race/ethnicity, region, plan-type, donut hole, polypharmacy, urinary incontinence, depression, falls and fall risk, cognitive impairment due to physical conditions, cognitive impairment due to mental conditions, dominant conditions, baseline emergency room visits, baseline home health visits and matched pair design, it was observed that individuals with PD were 34 % (AOR: 1.34, 95 % CI: 1.10-1.63) more likely to have better glycemic control (HbA1c < 8 %) compared to those without PD. Individuals with PD were higher likely to have better outcomes in terms of LDL-C (<100 mg/dl) (AOR: 1.29, 95 % CI: 1.06-1.59), triglyceride (<150 mg/dl) (AOR: 1.31, 95 % CI: 1.06-1.62), total cholesterol (<200 mg/dl) (AOR: 1.46, 95 % CI: 1.08-1.97) and HDL-C (≥50 mg/dl) (AOR: 1.20, 95 % CI: 1.04-1.39).
Discussion
This study examined the association between PD and process and intermediate clinical outcomes of diabetes care among elderly individuals with T2DM. Results from this study indicated that among individuals with T2DM, those with PD did not receive the ADA recommended HbA1c and lipid testing compared to those without PD. These findings suggest that, PD is a barrier to achieving clinically recommended process of care measures. We can speculate the reasons as to why those with PD did not achieve the ADA recommended HbA1c and lipid testing. Some of the reasons which may lead to not achieving the ADA recommended HbA1c and lipid testing can be that elderly Medicare beneficiaries may not be aware of the benefits of meeting these goals, or there can be a gap in patient-provider communication, or the elderly Medicare beneficiaries may not be visiting their physicians on a regular basis [23]. Some of the ways in which these barriers can be overcome include educating patients and helping them to attend group consultations by healthcare providers [24]. Future studies should explore the possible reasons why elderly individuals with co-occurring T2DM and PD are not being able to achieve the ADA recommended process of care goals.
A noteworthy finding from our study is the relationship between PD and intermediate clinical outcomes of diabetes care. For glycemic and lipid outcomes, elderly individuals with PD were more likely to achieve control compared to those without PD. A plausible explanation for better outcomes among those with PD could be due to pathophysiological conditions of the two diseases. For example, it has been suggested that insulin resistance and insulin deficiency, which are the cardinal characteristics of T2DM, can lead to neurodegeneration [9–11]. It is possible that given the risk of neurodegeneration due to T2DM, the providers may be aggressively treating individuals with T2DM and PD for better glycemic and lipid outcomes in order to prevent further neurodegeneration. The findings from this study are consistent with a study conducted among elderly veterans, which showed that veterans with PD were more likely to receive overall good outcomes for all three intermediate clinical outcomes - glycemic, blood pressure and low density lipoprotein-cholesterol combined (adjusted OR, 2.17; 95 % CI, 1.96-2.39) [6]. One of the similarities between VA and the Medicare Advantage (MA) plans is that they follow the Integrated Delivery System (IDS) model or the “coordinated care plan” approach. In the IDS model, the primary physician serves as the gate-keeper and maintains proper referral systems. The coordination of care among different types of specialists (Endocrinologists, Neurologists etc.) is ensured in the IDS models which in turn could lead to better management of individuals with PD. One can speculate that such coordination may involve comprehensive geriatric assessment (CGA) tools, which in turn can lead to better intermediate clinical outcomes among elderly beneficiaries with T2DM and PD.
However, the findings from this study is inconsistent with the findings from the study using the INTERMED classification system for case complexity which found that among individuals with T2DM, greater complexity was associated with higher HbA1c values [7]. The INTERMED classification system utilized different factors such as biological, psychosocial and health care related aspects of T2DM to classify patient complexity and had only 61 patients in the study. The results from this study [7] presented were in the preliminary forms and it required further validation. Hence, it is possible that due to different classification system used to determine patient complexity, greater risk of poor diabetes control among individuals with higher complexity was observed.
Strengths and limitations
Strengths of this study include the use of large sample size, nationwide sample of commercially insured elderly individuals, exhaustive list of variables, availability of laboratory values and use of a robust study design.
As with other studies, this study also has limitations. Findings from this study cannot be generalizable to other populations or settings (e.g., fee-for-service Medicare beneficiaries). Laboratory values are available for only one-third of the population. Unmeasured confounders such lifestyle risk factors (e.g., body mass index and smoking status), physician specialty, duration and severity of PD could influence the study outcomes.
Conclusion
To the best of author’s knowledge, this is the first study to examine the influence of the presence of a chronic illness with complexity such as PD on the process and outcomes of diabetes care. Individuals with PD and diabetes were less likely to achieve ADA recommended annual HbA1c and lipid testing goals compared to those with diabetes but without PD. Future research needs to explore the reasons for lower rates of HbA1C and lipid testing among elderly individuals with T2DM and PD. However, among individuals with PD, the intermediate glycemic and lipid outcomes were better compared to those without PD. These findings suggest that the integrated delivery system coupled with the CGA approach of MA plans may be beneficial to elderly with PD.
References
American Diabetes Association. Statistics About Diabetes: Data from the National Diabetes Statistics Report, 2014. URL available at: http://www.diabetes.org/diabetes-basics/statistics/ Accessed on 18 September 2014.
Muangpaisan W, Mathews A, Hori H, Seidel D. A systematic review of the worldwide prevalence and incidence of Parkinson’s disease. J Med Assoc Thai. 2011;94(6):749–55.
Park A, Stacy M. Non-motor symptoms in Parkinson’s disease. J Neurol. 2009;256 Suppl 3:293–8.
Lapane KL, Fernandez HH, Friedman JH. Prevalence, clinical characteristics, and pharmacologic treatment of Parkinson’s disease in residents in long-term care facilities. SAGE Study Group. Pharmacotherapy. 1999;19(11):1321–7.
Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716–24.
Woodard LD, Urech T, Landrum CR, Wang D, Petersen LA. Impact of comorbidity type on measures of quality for diabetes care. Med Care. 2011;49(6):605–10.
Fischer CJ, Stiefel FC, De Jonge P, Guex P, Troendle A, Bulliard C, et al. Case complexity and clinical outcome in diabetes mellitus. A prospective study using the INTERMED. Diabetes Metab. 2000;26(4):295–302.
Dorsey ER, Constantinescu R, Thompson JP, Biglan KM, Holloway RG, Kieburtz K, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68(5):384–6.
Peila R, Rodriguez BL, White LR, Launer LJ. Fasting insulin and incident dementia in an elderly population of Japanese-American men. Neurology. 2004;63(2):228–33.
Ronnemaa E, Zethelius B, Sundelof J, Sundstrom J, Degerman-Gunnarsson M, Berne C, et al. Impaired insulin secretion increases the risk of Alzheimer disease. Neurology. 2008;71(14):1065–71.
Ronnemaa E, Zethelius B, Sundelof J, Sundstrom J, Degerman-Gunnarsson M, Lannfelt L, et al. Glucose metabolism and the risk of Alzheimer’s disease and dementia: a population-based 12 year follow-up study in 71-year-old men. Diabetologia. 2009;52(8):1504–10.
Chang HY, Weiner JP, Richards TM, Bleich SN, Segal JB. Validating the adapted Diabetes Complications Severity Index in claims data. Am J Manag Care. 2012;18(11):721–6.
Bhattacharjee S, Sambamoorthi U. Co-occurring chronic conditions and healthcare expenditures associated with Parkinson’s disease: a propensity score matched analysis. Parkinsonism Relat Disord. 2013;19(8):746–50.
Wang L, Wei W, Miao R, Xie L, Baser O. Real-world outcomes of US employees with type 2 diabetes mellitus treated with insulin glargine or neutral protamine Hagedorn insulin: a comparative retrospective database study. BMJ Open. 2013;3(4). doi: 10.1136/bmjopen-2012-002348
American DA. Standards of medical care in diabetes--2012. Diabetes Care. 2012;35 Suppl 1:S11–63.
Meduru P, Helmer D, Rajan M, Tseng CL, Pogach L, Sambamoorthi U. Chronic illness with complexity: implications for performance measurement of optimal glycemic control. J Gen Intern Med. 2007;22 Suppl 3:408–18.
Sue Kirkman M, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, et al. Diabetes in older adults: a consensus report. J Am Geriatr Soc. 2012;60(12):2342–56.
Wei YJ, Palumbo FB, Simoni-Wastila L, Shulman LM, Stuart B, Beardsley R, et al. Relationships between antiparkinson medication nonadherence, regimen modifications, and healthcare utilization and expenditures. Parkinsonism Relat Disord. 2015;21(1):36–41.
Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780–91.
Mehta S, Chen H, Johnson ML, Aparasu RR. Risk of falls and fractures in older adults using antipsychotic agents: a propensity-matched retrospective cohort study. Drugs Aging. 2010;27(10):815–29.
Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29(3):725–31.
Safford MM, Allison JJ, Kiefe CI. Patient complexity: more than comorbidity. the vector model of complexity. J Gen Intern Med. 2007;22 Suppl 3:382–90.
Delaronde S. Barriers to A1C testing among a managed care population. Diabetes Educ. 2005;31(2):235–9.
Rubin RJ, Dietrich KA, Hawk AD. Clinical and economic impact of implementing a comprehensive diabetes management program in managed care. J Clin Endocrinol Metab. 1998;83(8):2635–42.
Acknowledgements
Dr. Bhattacharjee received research assistance and Dr. Sambamoorthi was partially supported for infrastructure from the West Virginia Collaborative Health Outcomes Research of Therapies and Services (WV CoHORTS) Center. The statements, findings, conclusions, views, and opinions contained and expressed in this article are those of authors and not of any other affiliated entities. Drs. Bhattacharjee and Sambamoorthi have no conflict of interest to declare. This study was conducted when Dr. Bhattacharjee was a graduate student at the West Virginia University. Drs. Bhattacharjee and Sambamoorthi are the guarantor of this manuscript and takes the full responsibility for the entire study. A part of this project was presented at the International Society of Pharmacoeconomics and Outcomes Research 19th Annual International Meeting, Montreal, QC, Canada, May 2014.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors’ contributions
SB conducted the literature review, data analyses, wrote manuscript. US helped in conceptualizing the study design, participated in data analyses, and reviewed/edited the manuscript. Both authors read and approved the final manuscript.
Appendix
Appendix
HbA1c testing
Individuals with HbA1c testing at least two times a year (with a gap of at least one month) will be considered as meeting standard of care for diabetes management. HbA1c testing will be identified by the following Current Procedural Terminology (CPT) codes.
-
a.
CPT codes: 83036, 83037 (Source : HEDIS, 2012)
-
b.
CPT Category II : 3044F, 3045F, 3046F, 3047F (Source : HEDIS, 2012)
Lipid testing
Individuals who were tested at least once a year will be considered as meeting standard of care for diabetes management. Lipid testing will be identified by the following Current Procedural Terminology (CPT) codes.
-
a.
CPT codes: 80061, 83700, 83701, 83704, 83721, 83715, 83716, 83718, 82465, and 84478 (Source: HEDIS, 2012)
-
b.
CPT Category II: 3048F, 3049F, 3050F
Nephropathy screening
Individuals who were screened at least once a year for urine albumin and serum creatinine will be considered as meeting standard of care for diabetes management. Nephropathy screening will be identified using the following Current Procedural Terminology (CPT) codes.
-
a.
CPT codes: 81000, 81001, 81002, 81003, 36800, 36810, 36815, 50300, 50340, 50360, 50365, 50370, 50380, 90920, 90921, 90924, 90925, 90935, 90937, 90945, 90947, 90989, 90993, 90997, and 90999 82579 for serum creatinine lab; 82042, 82043, 82044, 84156 (Source: HEDIS, 2012)
-
b.
CPT Category II: 3060F, 3061F (Source: HEDIS, 2012)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bhattacharjee, S., Sambamoorthi, U. Diabetes care among elderly medicare beneficiaries with Parkinson’s disease and diabetes. J Diabetes Metab Disord 14, 75 (2015). https://doi.org/10.1186/s40200-015-0209-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40200-015-0209-3