Abstract
Background
It is well-established that thrombus aspiration during primary percutaneous coronary intervention (PCI) in patients with acute myocardial infarction (AMI) indicates a higher thrombus burden and necessitates more intensive antithrombotic therapy. The bidirectional association between adverse events in AMI patients and platelet reactivity is typically observed during dual antiplatelet therapy (DAPT).
Objective
To investigate platelet reactivity after DAPT in AMI patients with thrombus aspiration performed during PCI.
Methods
In this retrospective study, we examined 269 consecutive AMI patients who underwent PCI and recorded their demographic, clinical and laboratory data. The platelet reactivity was measured with thromboelastogram (TEM).
Results
Ultimately, 208 patients were included in this study and divided into a Thrombus Aspiration group (N = 97) and a PCI Alone group (N = 111) based on whether thrombus aspiration was performed or not. The adenosine diphosphate (ADP)-induced platelet inhibition rate in the Thrombus Aspiration group was higher than that in the PCI Alone group (P < 0.001). Furthermore, multivariate linear regression analysis revealed that the ADP-induced platelet inhibition rate was independently associated with leukocyte count, thrombus aspiration and the combination of aspirin and ticagrelor as DAPT after adjusting for potential covariates in all AMI patients.
Conclusion
In conclusion, clinicians should exercise heightened attention towards the bleeding risk among patients undergoing PCI concomitant with Thrombus Aspiration postoperatively.
Similar content being viewed by others
Introduction
Based on existing evidence, it is indicated that the underlying pathophysiology of most cases of acute myocardial infarction (AMI) is associated with thrombosis related to atheromatous plaques [1]. The standard treatment for patients with acute myocardial infarction (AMI), especially those who undergo percutaneous coronary intervention (PCI), involves dual antiplatelet therapy (DAPT) [2]. This therapy combines the use of aspirin and a P2Y12 receptor antagonist to prevent the reoccurrence of thromboembolic events.
For AMI patients with a higher thrombus burden, interventional cardiologists typically opt for thrombus aspiration as a standalone procedure or combine it with balloon angioplasty and/or stent implantation during PCI [3, 4]. Clinically, compared to those without thrombus aspiration, AMI patients undergoing thrombus aspiration typically receive more intensive antithrombotic treatment after PCI, in addition to DAPT. This may involve a prolonged duration of low-molecular-weight heparin injection and/or the addition of glycoprotein IIb/IIIa antagonists [5]. However, excessive use of antithrombotic agents poses an increased risk of bleeding events, which may be life-threatening in some cases [6]. Therefore, it is crucial for judiciously administer antiplatelet agents, maintaining platelet reactivity within a safe and effective range for AMI patients.
In recent years, various methods have been developed to measure platelet function and assess the efficacy of antithrombotic agents [7]. Among these, thromboelastography (TEM) has emerged as a new platelet function test that is more accurate and reliable [8]. It can measure the actual platelet inhibitory effect of aspirin and ADP receptor antagonists, even when these agents taken in combination.
Nonetheless, whether AMI patients undergoing thrombus aspiration exhibit a higher platelet reactivity after standard DAPT, potentially increasing the risk of future thrombotic events, has not been comprehensively investigated. Herein, we sought out to examine platelet reactivity in AMI patients with and without thrombus aspiration after DAPT in our center.
Methods
Study population
This retrospective cohort study examines a cohort of 269 AMI patients who underwent percutaneous coronary intervention (PCI) and were admitted to the Cardiac Care Unit (CCU) at Xinhua Hospital, affiliated with Shanghai Jiao Tong University School of Medicine, from January 2022 to December 2023. The study's protocol adhered to the principles of the Declaration of Helsinki. Approval for this study was obtained from the Ethics Committee of Xinhua Hospital affiliated to Shanghai Jiao Tong University School of Medicine (No. XHEC-D-2024-005).
Medication and procedure protocol
A loading dose of 300 mg aspirin and either 300 mg or 600 mg clopidogrel or 180 mg ticagrelor, was administered before PCI. Maintenance doses of DAPT consisted of 100 mg aspirin per day and either 75 mg clopidogrel per day or 90 mg ticagrelor twice a day. The decision to perform thrombus aspiration during PCI was made based on the experience of interventional cardiologists and in accordance with relevant relative guidelines.
Clinical data collection
Complete blood count, liver function, renal function, blood lipid levels, fasting glucose, glycosylated hemoglobin, and hypersensitivity C-reactive protein were assessed with fasting blood samples on the morning of following admission. An intracoronary thrombus was detected through angiography and assessed using a five-point grading system, in accordance with previous research. Following the reclassification of the thrombus and guided by clinical data, 3–4 grades in the classification are defined as high thrombus [9].
Platelet function measurement
TEM was conducted at least 5 days, and at most 7 days, after the initiation of DAPT. Whole blood samples were collected in vacutainer tubes containing 3.2% trisodium citrate, and the initial 2–4 ml of blood was discarded to avoid platelet activation. The TEG assay was performed according to the manufacturer’s instructions, measuring the antiplatelet effect through the adenosine diphosphate (ADP) or arachidonic acid (AA) pathway. The percentage of platelet inhibition was calculated using computer software based on the formula: ADP or AA-induced platelet inhibition (%) = 100 – 100 × [(MAAAorADP-MAFibrin) / (MAThrombin – MAFibrin)] × 100%. Where, MAADP represents adenosine diphosphate-induced clot strength, MAFIBRIN is FIBRIN-induced clot strength, and MATHROMBIN is THROMBIN-induced clot strength.
Statistical analysis
Continuous variables were presented as mean ± standard deviation for variables following a normal distribution and median (interquartile range) for data with skewed distributions. Continuous variables were compared using the Student’s t-test or Mann–Whitney U test. Categorical variables were expressed as numbers (percentages) and were compared using the chi-square (X2) test or Fisher's exact test. Normality was assessed using the Kolmogorov–Smirnov test. ADP-induced platelet inhibition (ADP%) was subjected to a normal transformation to ADP%' for multivariate linear regression analysis: ADP%' = SQRT(K-ADP%), where K = (ADP%)max + 1. Univariate analysis identified variables with P < 0.1, considered significant, which were then included in multivariate linear regression analysis. Adjustments were made for seven variables, including age, male, baseline hemoglobin level, total cholesterol, leukocyte count, thrombus aspiration, and the combination of aspirin and ticagrelor. During multivariate linear regression analysis, the stepwise elimination method was used to identify independent factors associated with ADP-induced platelet inhibition. A two-sided P-value < 0.05 was statistically significant, and all data analyses were performed using SPSS software version 26.0.
Results
Baseline characteristics
Cases that did not receive DAPT (n = 15), those lacking TEG results (n = 26), and those with incomplete data (n = 4) were excluded. Another 16 patients were excluded based on additional exclusion criteria, including severe anemia, malignant disease, serious renal or hepatic insufficiency, and a total platelet count < 100 × 109 /L. Finally, 208 patients were enrolled in this study (Fig. 1).
A total of 208 patients were included in this retrospective study, exhibiting male predominance (n = 168, 80.8%) with a mean age of 65.5 ± 11.5 years. The Thrombus Aspiration group comprised 97 (46.6%) patients, while the PCI Alone group included 111 (53.3%) patients.
Compared to the PCI Alone group, patients in the Thrombus Aspiration group were significantly younger (P < 0.001), with a higher proportion of males (P = 0.002) and higher levels of hemoglobin (P < 0.001), mean platelet volume (P = 0.014), and alanine transaminase (P < 0.001). Additionally, the Thrombus Aspiration group comprised significantly more patients treated with aspirin and ticagrelor (P < 0.001) and a higher prevalence of patients with ST-elevation myocardial infarction (STEMI) type (P = 0.005). No significant differences were observed in other indicators between the two groups (Table 1, Fig. 2).
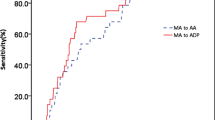
Comparison of medication (A), MI Type (B), AA-induced platelet inhibition rate (C), and ADP-induced platelet inhibition rate (D) between the thrombus aspiration and PCI alone groups. E Comparison of ADP-induced platelet inhibition rate between AMI patients using aspirin + clopidogrel and aspirin + ticagrelor. P represents the comparison of the proportion of STEMI type or the combination of aspirin and ticagrelor between the two groups in (A) and (B). The dotted line in the middle represents the median, while the upper and lower solid lines denote quartiles in (C), (D), and (E). AA arachidonic acid, ADP adenosine diphosphate, NSTEMI non-ST-segment elevation myocardial infarction, STEMI ST-segment elevation myocardial infarction
TEG analysis
In comparison to the PCI Alone group, the thrombus aspiration group demonstrated a significantly higher ADP-induced platelet inhibition rate (P < 0.001). However, there was no significant difference in the AA-induced platelet inhibition rate between these two groups (P > 0.05) (Table 2, Fig. 2).
Multivariate analysis for ADP-induced platelet inhibition rate in PCI patients
During multivariate analysis with ADP-induced platelet inhibition rate as the dependent variable, significant factors identified during the univariate analysis (age, male, baseline hemoglobin level, leukocyte count, thrombus aspiration, high thrombus and the combination of aspirin and ticagrelor with P < 0.1) were utilized as independent variables. The results of the multivariate regression analysis indicated that a higher ADP-induced platelet inhibition rate independently correlated with three factors: lower leukocyte count (P = 0.01), thrombus aspiration (P < 0.001), and the combination of aspirin and ticagrelor (P < 0.001) (Table 3).
Discussion
In this study, we used TEG to evaluate platelet reactivity and examine the efficacy of DAPT in AMI patients undergoing PCI and thrombus aspiration. In addition, the determinants of platelet reactivity in AMI patients were investigated. Contrary to our expectations, AMI patients subjected to thrombus aspiration exhibited a higher ADP-induced platelet inhibition rate after DAPT. Besides, AMI patients with an elevated ADP-induced platelet inhibition rate demonstrated a higher baseline leukocyte count, more frequent thrombus aspiration, and a higher prevalence of treatment with the combination of aspirin and ticagrelor as DAPT.
AMI stands as one of the most life-threatening cardiovascular diseases globally, with thrombosis affecting over 90% of AMI patients [1]. PCI is the preferred method for achieving rapid coronary reperfusion in AMI patients, though it introduces the risk of distal embolization from proximal thrombotic particles and/or atherosclerotic plaque debris during guidewire passage through the occlusive lesion. Thrombus burden as an independent predictor of adverse cardiovascular events in STEMI patients underscores the importance of thrombus aspiration as a viable intervention characterized by high thrombus burden [10]. Although not recommended as a routine procedure, the European Society of Cardiology (ESC) 2017 guidelines suggest thrombus aspiration in the management of AMI patients with elevated thrombus burden to mitigate the risk of distal embolization and preserve coronary microcirculation [4, 11]. Recent findings by Elfekky et al. consistently highlighted the significant value of thrombus aspiration in reducing in-hospital mortality and improving various cardiovascular parameters in STEMI patients with high thrombus burden, compared to those undergoing PCI alone, as observed over a 1-month follow-up period [12].
Given the pivotal role of platelets in thrombosis, the evaluation of platelet activity has attracted significant interest [13]. Over the years, several platelet function tests, such as light transmission platelet aggregation (LTA), Vasodilator-Stimulated Phosphoprotein (VASP) index, VerifyNow P2Y12 assay, and TEG, have been employed to assess individual responses to antiplatelet therapy [8, 14, 15]. LTA is commonly seen as the gold standard for platelet function testing, but its clinical use is limited due to drawbacks like time-consuming detection, complex sample preparation, and low specificity for P2Y12 antagonists [14]. It is now understood that ticagrelor, in addition to inhibiting the P2Y12-ADP pathway, can reduce platelet reactivity by enhancing adenosine activation through increased adenosine levels and subsequent engagement of adenosine A2A receptors [16]. Hence, traditional assays like the VASP index and VerifyNow P2Y12, which focus solely on the P2Y12-ADP pathway, may not accurately capture the overall antiplatelet effect of ticagrelor. TEG has emerged as a novel platelet function test, providing rapid and precise platelet aggregation detection without the constraints of other methods [17]. However, there is no clear international consensus on the "safety range" of ADP% in TEG. It has been shown that an ADP% greater than 30 indicates effective drug action, while an ADP% greater than 92.5 is an independent predictor of bleeding, though these data are specific to clopidogrel [18,19,20]. Whether different types of P2Y12 receptor inhibitors share the same "safety margins" remains to be further explored. Recently, a study on DAPT treatment in stroke patients with ticagrelor suggested a recommended ADP% safety range of 30–82.3% [21]. In our study, the ADP% in the Thrombus Aspiration group is approximately 80.3%. Therefore, clinicians should be particularly vigilant regarding the bleeding risk in PCI patients with Thrombus Aspiration undergoing DAPT.
The mean platelet volume (MPV) is recognized as an indicator of platelet size and, consequently, platelet reactivity [22]. Lai et al. demonstrated that elevated mean platelet volume at admission was an independent predictor of a large thrombus burden in STEMI patients, consistent with the findings of our study [23]. Notably, in this study, the Thrombus Aspiration group exhibited a higher mean platelet volume and comprised a significantly higher percentage of patients with STEMI. STEMI typically indicates complete coronary artery occlusion with thrombosis and aligns with the pathophysiology of type 1 myocardial infarction (MI) according to the fourth universal definition of myocardial infarction. Conversely, non-ST-elevation myocardial infarction (NSTEMI) often indicates incomplete coronary artery occlusion, with the pathophysiology of NSTEMI tending to be more diverse. The observed correlation between higher mean platelet volume, ST-segment elevation, and a higher percentage of STEMI patients in the Thrombus Aspiration group suggests an association between elevated platelet volume and increased thrombus burden in AMI patients.
Contrary to expectations, we found that AMI patients with a higher thrombus burden, indicated by thrombus aspiration during the PCI procedure, experienced more significant ADP-induced platelet inhibition compared to those with a lower thrombus burden. Meanwhile, the Thrombus Aspiration group in our study showed a significantly higher percentage of ticagrelor usage compared to the PCI Alone group. Clopidogrel and ticagrelor, both P2Y12 receptor antagonists, differ in their mechanisms of action. clopidogrel, a prodrug, undergoes liver metabolism via CYP2C19, which, when genetically variant (25–35% of population), may cause variable drug response and resistance [24]. In contrast, ticagrelor, not requiring hepatic metabolism, binds reversibly to the P2Y12 receptor, resulting in a consistently faster, more potent, and less variable antiplatelet effect compared to clopidogrel in clinical studies [9]. Our study's findings, exemplified by the higher antiplatelet effect of ticagrelor in AMI patients compared to clopidogrel (Fig. 2E), align with previous research. However, numerous studies have demonstrated that, compared to clopidogrel, the use of ticagrelor is significantly associated with a higher risk of bleeding in Chinese patients [25]. The increased proportion of ticagrelor usage also reflected clinicians' consideration that these AMI patients might benefit from more intensive antithrombotic therapy.
To investigate factors impacting platelet reactivity, particularly to ascertain whether the elevated ADP-induced platelet inhibition observed in the Thrombus Aspiration group resulted from increased ticagrelor usage, we conducted a multiple linear regression analysis of ADP-induced platelet inhibition rates. The outcomes revealed that ADP-induced platelet inhibition was independently associated with thrombus aspiration. Furthermore, heightened leukocyte counts and the administration of ticagrelor independently correlated with increased ADP-induced platelet inhibition. It is widely acknowledged that in the intricate pathogenesis of coronary atherosclerotic disease (CAD), inflammation assumes a pivotal role [26]. The activation of inflammatory cells within atherosclerotic plaques renders them unstable, fostering thrombotic events. A heightened leukocyte count, as an inflammatory marker, not only signals a graver prognosis and elevated mortality in CAD patients, but is also a constituent of the "PRECISE-DAPT" score [27]. Widely employed to assess bleeding risk in AMI patients and guide the duration of DAPT post-stent implantation, the "PRECISE-DAPT" score incorporates leukocyte count as a contributing factor [28]. This study revealed that AMI patients with an elevated leukocyte count exhibited a heightened ADP-platelet inhibition rate after DAPT. This is in accordance with the predictive function of bleeding risk in the "PRECISE-DAPT" score and also potentially elucidates the mechanism behind bleeding risks during DAPT. Controversies persist regarding the relationship between leukocyte count and the antiplatelet effect in CAD patients. A recent study by Li et al. uncovered that the leukocyte count was an independent predictor of low platelet reactivity in PCI patients undergoing DAPT [29]. These discrepancies may primarily stem from variations in antiplatelet medications and participant demographics. Li et al.'s study, limited to clopidogrel treatment and encompassing participants beyond AMI patients, contrasts with our study's focus.
Despite our comprehensive investigation, the correlation between thrombus aspiration and post-DAPT platelet reactivity in AMI patients remains elusive. It is highly conceivable that thrombus aspiration is not the causative factor for the heightened ADP-induced platelet inhibitory effects observed in AMI patients undergoing DAPT; rather, it is a distinctive characteristic. AMI patients with a higher thrombus burden and elevated leukocyte count are predisposed to an increased bleeding risk after DAPT, particularly with ticagrelor treatment. This subset of patients exhibits a propensity for a more pronounced platelet inhibitory effect. TEM has emerged as a valuable tool for assessing bleeding risk in these individuals. Indeed, its application can guide clinicians in evaluating bleeding risk, prompting adjustments in medical dosage, shortening DAPT duration, and implementing specific precautions.
Despite these promising findings, certain limitations of this study should be acknowledged. Firstly, being a retrospective study conducted at a single center, there may be constraints on the applicability of the results to broader populations. Secondly, the relatively small sample size introduces the possibility of deviations in statistical outcomes, impacting the study's representativeness and reliability. Consequently, multi-centered larger-scale randomized clinical trials are imperative to conclusively confirm the relationship between thrombus aspiration and platelet inhibition rate. Thirdly, the mechanisms underlying thrombus burden, leukocyte count, and the efficacy of antiplatelet therapy remain unclear, necessitating further in-depth mechanistic experiments.
Conclusion
In the present study, thrombus aspiration is independently associated with a higher ADP-induced platelet inhibition rate after DAPT in AMI patients.Attention should be directed towards AMI patients undergoing thrombus aspiration, exhibiting elevated leukocyte counts, and receiving ticagrelor, as they are prone to a bleed risk following antithrombotic therapy.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet. 2017;389(10065):197–210.
Gragnano F, Mehran R, Branca M, Franzone A, Baber U, Jang Y, Kimura T, Hahn JY, Zhao Q, Windecker S, Gibson CM, Kim BK, Watanabe H, Song YB, Zhu Y, Vranckx P, Mehta S, Hong SJ, Ando K, Gwon HC, Calabro P, Serruys PW, Dangas GD, McFadden EP, Angiolillo DJ, Heg D, Valgimigli M. Single versus dual antiplatelet therapy, P2Y(12) inhibitor monotherapy or dual antiplatelet therapy after complex percutaneous coronary interventions. J Am Coll Cardiol. 2023;81(6):537–52.
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, Prescott E, Storey RF, Deaton C, Cuisset T, Agewall S, Dickstein K, Edvardsen T, Escaned J, Gersh BJ, Svitil P, Gilard M, Hasdai D, Hatala R, Mahfoud F, Masip J, Muneretto C, Valgimigli M, Achenbach S, Bax JJ, Group ESCSD. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–77.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimsky P, Group ESCSD. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Kumar V, Sharma AK, Kumar T, Nath RK. Large intracoronary thrombus and its management during primary PCI. Indian Heart J. 2020;72(6):508–16.
Laine M, Panagides V, Frère C, Cuisset T, Gouarne C, Jouve B, Thuny F, Paganelli F, Alessi MC, Mancini J, Bonello L. Platelet reactivity inhibition following ticagrelor loading dose in patients undergoing percutaneous coronary intervention for acute coronary syndrome. J Thromb Haemost. 2019;17(12):2188–95.
Helten C, Naguib D, Dannenberg L, Pohl M, Ayhan A, Hohlfeld T, Levkau B, Kelm M, Zeus T, Polzin A. Platelet function testing: dead or alive. J Thromb Haemost. 2018;16(5):984–6.
Shen W, Zhou JY, Gu Y, Shen WY, Li M. Establishing a reference range for thromboelastography maximum amplitude in patients administrating with antiplatelet drugs. J Clin Lab Anal. 2020;34(4): e23144.
Wang Y, Meng X, Wang A, Xie X, Pan Y, Johnston SC, Li H, Bath PM, Dong Q, Xu A, Jing J, Lin J, Niu S, Wang Y, Zhao X, Li Z, Jiang Y, Li W, Liu L, Xu J, Chang L, Wang L, Zhuang X, Zhao J, Feng Y, Man H, Li G, Wang B. Ticagrelor versus clopidogrel in CYP2C19 loss-of-function carriers with stroke or TIA. N Engl J Med. 2021;385(27):2520–30.
Jolly SS, Cairns JA, Lavi S, Cantor WJ, Bernat I, Cheema AN, Moreno R, Kedev S, Stankovic G, Rao SV, Meeks B, Chowdhary S, Gao P, Sibbald M, Velianou JL, Mehta SR, Tsang M, Sheth T, Dzavik V, Investigators T. Thrombus aspiration in patients with high thrombus burden in the TOTAL Trial. J Am Coll Cardiol. 2018;72(14):1589–96.
Pruthi S, Bangalore S. The state of coronary thrombus aspiration. J Am Heart Assoc. 2022;11(16): e026849.
Elfekky EM, Penjameen MN, Nassar AI, Elias RR. Outcome of manual thrombus aspiration for patients undergoing primary PCI for acute STEMI showing large thrombus burden. Egypt Heart J. 2021;73(1):8.
Gurbel PA, Jeong YH, Navarese EP, Tantry US. Platelet-mediated thrombosis: from bench to bedside. Circ Res. 2016;118(9):1380–91.
Koltai K, Kesmarky G, Feher G, Tibold A, Toth K. Platelet aggregometry testing: molecular mechanisms, techniques and clinical implications. Int J Mol Sci. 2017. https://doi.org/10.3390/ijms18081803.
Vinholt PJ, Hvas AM, Nielsen C, Söderström AC, Sprogøe U, Fialla AD, Nybo M. Reduced platelet activation and platelet aggregation in patients with alcoholic liver cirrhosis. Platelets. 2018;29(5):520–7.
Ortega-Paz L, Brugaletta S, Ariotti S, Akkerhuis KM, Karagiannis A, Windecker S, Valgimigli M. Adenosine and ticagrelor plasma levels in patients with and without ticagrelor-related dyspnea. Circulation. 2018;138(6):646–8.
Li Y, Chang H, Ni L, Xue P, Li C, Yuan L, Cui H, Yu C. Analysis of thrombelastogram-guided medication in patients with coronary heart disease after percutaneous coronary intervention. Exp Ther Med. 2019;17(4):3047–52.
Hou XM, Han WZ, Qiu XB, Fang WY. Clinical characteristics associated with high on-treatment platelet reactivity of patients undergoing PCI after a 300 mg loading dose of clopidogrel, measured by thrombelastography. Heart Asia. 2013;5(1):66–9.
Zhang JH, Tang XF, Zhang Y, Wang J, Yao Y, Ma YL, Xu B, Gao RL, Gao Z, Chen J, Song L, Wu Y, Meng XM, Yuan JQ. Relationship between ABCB1 polymorphisms, thromboelastography and risk of bleeding events in clopidogrel-treated patients with ST-elevation myocardial infarction. Thromb Res. 2014;134(5):970–5.
Tantry US, Bonello L, Aradi D, Price MJ, Jeong YH, Angiolillo DJ, Stone GW, Curzen N, Geisler T, TenBerg J, Kirtane A, Siller-Matula J, Mahla E, Becker RC, Bhatt DL, Waksman R, Rao SV, Alexopoulos D, Marcucci R, Reny JL, Trenk D, Sibbing D, Gurbel PA. Working group on on-treatment platelet, consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol. 2013;62(24):2261–73.
He D, Guo Y, Zhang Y, Zhao J, Wu L, Yu Z, Qu W, Luo X. Thromboelastography predicts dual antiplatelet therapy-related hemorrhage in patients with acute ischemic stroke. J Neurointerv Surg. 2022;14(7):672–6.
Arachchillage DRJ, Laffan M. Can mean platelet volume be used as a predictor of vascular disease? Problems and pitfalls. Semin Thromb Hemost. 2017;43(6):599–608.
Lai HM, Xu R, Yang YN, Ma YT, Li XM, Zhao Q, Chen QJ, Zhai H, Liu F, Chen BD. Association of mean platelet volume with angiographic thrombus burden and short-term mortality in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Catheter Cardiovasc Interv. 2015;85(Suppl 1):724–33.
Akkaif MA, Daud NAA, Sha’aban A, Ng ML, Abdul Kader MAS, Noor DAM, Ibrahim B. The role of genetic polymorphism and other factors on clopidogrel resistance (CR) in an Asian population with coronary heart disease (CHD). Molecules. 2021. https://doi.org/10.3390/molecules26071987.
Park DW, Kwon O, Jang JS, Yun SC, Park H, Kang DY, Ahn JM, Lee PH, Lee SW, Park SW, Choi SW, Lee SG, Yoon HJ, Ahn T, Kim MH, Nah DY, Lee SY, Chae JK, Park SJ. Clinically significant bleeding with ticagrelor versus clopidogrel in Korean patients with acute coronary syndromes intended for invasive management: a randomized clinical trial. Circulation. 2019;140(23):1865–77.
Back M, Yurdagul A Jr, Tabas I, Oorni K, Kovanen PT. Inflammation and its resolution in atherosclerosis: mediators and therapeutic opportunities. Nat Rev Cardiol. 2019;16(7):389–406.
Ono M, Tomaniak M, Koenig W, Khamis R, de Silva R, Chichareon P, Kawashima H, Hara H, Gao C, Wang R, Huber K, Vrolix M, Jasionowicz P, Wykrzykowska JJ, Piek JJ, Jüni P, Hamm C, Steg PG, Windecker S, Onuma Y, Storey RF, Serruys PW. Impact of white blood cell count on clinical outcomes in patients treated with aspirin-free ticagrelor monotherapy after percutaneous coronary intervention: insights from the GLOBAL LEADERS trial. Eur Heart J Cardiovasc Pharmacotherapy. 2022;8(1):39–47.
Costa F, van Klaveren D, James S, Heg D, Räber L, Feres F, Pilgrim T, Hong M-K, Kim H-S, Colombo A, Steg PG, Zanchin T, Palmerini T, Wallentin L, Bhatt DL, Stone GW, Windecker S, Steyerberg EW, Valgimigli M. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet. 2017;389(10073):1025–34.
Li J, Yuan D, Jiang L, Tang X, Xu J, Song Y, Chen J, Qiao S, Yang Y, Gao R, Xu B, Yuan J, Zhao X. Similar inflammatory biomarkers reflect different platelet reactivity in percutaneous coronary intervention patients treated with clopidogrel: a large-sample study from China. Front Cardiovasc Med. 2021;8: 736466.
Acknowledgements
The authors declare no conflicts of interest. All authors have read the journal's policy and the journal’s authorship agreement. The manuscript has been reviewed and approved by all named authors.
Funding
No funding to declare.
Author information
Authors and Affiliations
Contributions
Qianyi Li, Chunxuan Wu wrote the manuscript. Chunxuan Wu, Yanyan Li, Juan Ma, Shiqun Sun and Xiaoxing Xu collected the data. Lingchao Yang and Ping Li analyed the data. Ying Yu and Wei Li modified the manuscript. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Approval for this study was obtained from the Ethics Committee of Xinhua Hospital affiliated to Shanghai Jiao Tong University School of Medicine (No. XHEC-D-2024-005).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, C., Li, Q., Ma, J. et al. Thrombus aspiration is associated with improved platelet inhibition rate following dual antiplatelet therapy in acute myocardial infarction patients. Eur J Med Res 29, 420 (2024). https://doi.org/10.1186/s40001-024-02018-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-02018-9