Abstract
Background
Ischemic cardio-cerebrovascular disease is the leading cause of mortality worldwide. However, studies focusing on elderly and very elderly patients are scarce. Hence, our study aimed to characterize and investigate the long-term prognostic implications of ischemic cardio-cerebrovascular diseases in elderly Chinese patients.
Methods
This retrospective cohort study included 1026 patients aged ≥ 65 years who were categorized into the mono ischemic cardio-cerebrovascular disease (MICCD) (either coronary artery disease or ischemic stroke/transient ischemic attack) (n = 912) and the comorbidity of ischemic cardio-cerebrovascular disease (CICCD) (diagnosed with both coronary artery disease and ischemic stroke/transient ischemic attack at admission) (n = 114). The primary outcome was all-cause death. The mortality risk was evaluated using the Cox proportional hazards risk model with multiple adjustments by conventional and propensity-score-based approaches.
Results
Of the 2494 consecutive elderly patients admitted to the hospital, 1026 (median age 83 years [interquartile range]: 76.5–86.4; 94.4% men) met the inclusion criteria. Patients with CICCD consisted mostly of very elderly (79.2% vs. 66.1%, P < 0.001) individuals with a higher burden of comorbidities. Over a median follow-up of 10.4 years, 398 (38.8%) all-cause deaths were identified. Compared with the MICCD group, the CICCD group exhibited a higher adjusted hazard ratio (HR) (95% confidential interval, CI) of 1.71 (1.32–2.39) for long-term mortality after adjusting for potential confounders. The sensitivity analysis results remained robust. After inverse probability of treatment weighting (IPTW) modeling, the CICCD group displayed an even worse mortality risk (IPTW-adjusted HR: 2.07; 95% CI 1.47–2.90). In addition, anemia (adjusted HR: 1.48; 95% CI 1.16–1.89) and malnutrition (adjusted HR: 1.43; 95% CI 1.15–1.78) are also independent risk factors for all-cause mortality among elderly and very elderly patients.
Conclusions
Our results thus suggest that elderly patients with ischemic cardio-cerebrovascular disease and anemia or malnutrition may have higher mortality, which may be predicted upon admission. These findings, however, warrant further investigation.
Graphical Abstract

Similar content being viewed by others
Introduction
Ischemic cardio-cerebrovascular disease, one of the leading causes of death worldwide, is a broad spectrum of serious health conditions including cardiovascular disease, hypertension, stroke, transient ischemic attack (TIA), and atherosclerosis [1, 2]. Their morbidity and mortality rates eclipse those of neoplastic conditions, thereby ascending to the foremost rank [3]. Physiologically, the heart and brain are profoundly interconnected; the cerebral tissue fundamentally depends on cardiac-driven blood circulation to sustain its regular functions. In the past few decades, the pathogenesis and clinical features of cardiovascular diseases have been extensively investigated, and it is believed that cardiovascular and cerebrovascular diseases have a common pathological basis. An empirical study reported that approximately 10–45% of the patients with cardiac issues might experience a stroke, 78.1–90.2% of those with cerebrovascular anomalies have an abnormal electrocardiogram, and 12.7% may be complicated by cerebral infarctions [4].
The concept of the "cardio-cerebrovascular continuum" delineates a state characterized by an increased likelihood of fatal progression in the absence of interventions that disrupt this pathological cycle [5]. Contemporary advancements, particularly in the domains of potent antithrombotic and lipid-lowering treatments, have markedly altered the prognosis of these patients. Nevertheless, despite implementing secondary prevention measures in patients diagnosed with coronary artery disease or cerebrovascular disease, the criteria for systematic pan-vascular screening and the judicious administration of newly developed therapies remain contentious. This ongoing debate may lead to underestimating risk and, consequently, undertreatment [6].
The prevalence of atherosclerotic involvement in extracardiac vascular beds is prominent among elderly patients and is an indicator of systemic atherosclerosis, thereby posing an increased risk for subsequent ischemic events [7]. Systemic atherosclerotic burden, such as myocardial infarction, coronary artery disease, and peripheral arterial disease, has consistently been reported as an independent risk factor for adverse cardiovascular events and short-term outcomes across various populations. These deleterious effects are largely consistent regardless of age and other vascular risk factors [8,9,10,11]. With the increase in life expectancy, ischemic cardio-cerebrovascular diseases have become significant conditions that severely impact the quality of life and survival of elderly and very elderly patients [12]. Consequently, the management of these patients has become a major concern. In 2019, the life expectancy of the Chinese population reached 77.3 years, and it is projected to increase to 81.3 years by 2035 [13]. During the urbanization and social transition processes, the effects of ischemic cardio-cerebrovascular diseases on the life expectancy of the oldest-old (≥ 80 years) patients remain unclear. Therefore, this study aims to evaluate the long-term prognosis of elderly patients with ischemic cardio-cerebrovascular diseases to improve their management in tertiary hospitals.
Methods
Study design and population
This study was conducted at the Second Medical Center of the Chinese PLA General Hospital. A total of 2493 consecutive elderly patients (over 65 years of age) who were admitted from January 1, 2007, to December 31, 2012, were enrolled in this retrospective aging-related cohort study. The inclusion criteria were (1) age ≥ 65 years; (2) a diagnosis of one of the ischemic cardio-cerebrovascular diseases, including coronary artery disease, ischemic stroke/TIA; (3) a diagnosis of both of these diseases were defined as the comorbidity of ischemic cardio-cerebrovascular disease (CICCD). The exclusion criteria were (1) no diagnosis of ischemic cardio-cerebrovascular disease; (2) known severe renal impairment (eGFR < 30 mL/min/1.73m2); (3) moderate to severe heart failure (NYHA III–IV); (4) significant hepatic disease (eg, ALT > 3 × upper limit of normal, cirrhosis, ascites); (5) malignancy (except non-metastatic, non-melanoma skin cancers, cervical in-situ carcinoma, breast ductal carcinoma in situ, or stage 1 prostate carcinoma); (6) no data on total cholesterol (TC), triglycerides (TG), high-density lipoprotein (HDL), and/or low-density lipoprotein (LDL) measurements; (7) no medication records; (8) potential cardioembolic stroke classified by the CISS classification [14]; and (9) no censoring information. The study protocol complied with the tenets of the Declaration of Helsinki and was approved by the ethics committee of the Chinese People’s Liberation Army General Hospital (S2021-326-02). Due to this study's retrospective nature, the ethics committee waived the need for written informed consent of the included patients. Meanwhile, we de-identified and anonymized patient records/information before analysis.
Definition of ischemic cardio-cerebrovascular diseases
In this study, ischemic cardio-cerebrovascular disease was used as a general term for (1) coronary artery disease; and (2) cerebrovascular disease. Coronary artery disease was defined based on (1) physician diagnosis; (2) history of myocardial infarction, coronary artery bypass grafting, or percutaneous coronary intervention; and (3) treatment with statins. Cerebrovascular disease was defined as ischemic stroke or TIA [15]. Comorbidity of ischemic cardio-cerebrovascular disease was defined as a diagnosis with both coronary artery disease and cerebrovascular disease. A panel of three physicians reviewed patient medical records to confirm the diagnosis of the abovementioned diseases.
The main parameter in this study was the number of ischemic cardio-cerebrovascular diseases a patient was diagnosed with, based on which they were categorized into the following groups: (1) mono ischemic cardio-cerebrovascular disease; and (2) comorbidity of ischemic cardio-cerebrovascular disease.
Endpoints and follow-up
For follow-up, the hospital’s electronic medical services were used. Considering the cause of death was not consistently available in our clinical cohort, and therefore we included all-cause and not cardiovascular mortality. Follow-up commenced on the day of admission and ended at the time of experiencing death or censoring events. Patients were censored for the event of interest, death, loss to follow-up, or December 31, 2020, whichever occurred first. Data on mortality, censoring events, and loss to follow-up were extracted from the hospital’s electronic medical record database. Lost to follow-up was determined based on the last date of active use of hospital electronic medical services (inpatient, outpatient, or laboratory).
Data collection and definition
Information on baseline patient demographic characteristics, anthropometric measurements, smoking status, laboratory values, comorbid conditions, and medication use were extracted from the hospital’s electronic medical record database. Demographic characteristics included age and sex. Anthropometric measurements included height and weight. Body mass index (BMI) was calculated as weight (kg) divided by the square of height (m). BMI was categorized into four levels [16]: underweight (< 18.5 kg/m2), normal (18.5–23.9 kg/m2), overweight (24–27.9 kg/m2) and obese (≥ 28 kg/m2). Smoking status was classified into three categories: never, past, and current smoking. Laboratory values comprised measurements of hemoglobin, C-reactive protein (CRP), serum creatinine, urine acid, albumin, B-type natriuretic peptide (BNP), TC, TG, HDL, LDL, and glycated hemoglobin (HbA1c). The estimated glomerular filtration rate (eGFR) was calculated using the CKD Epidemiology Collaboration formula [17]. For laboratory values that were repeated, the mean value was included in analyses. Medications included aspirin, statins, ADP receptor inhibitors, anticoagulants, renin–angiotensin–aldosterone system inhibitors (RAASi), beta-blockers, and calcium channel blockers (CCBs).
The burden of other comorbidities was assessed by the age-adjusted Charlson community index (CCI) [18], an easily replicable approach, which was among the first indexes to determine disease severity and was widely used to assess physical functioning. The International Classification of Diseases, 10th Revision, was used to identify relevant diagnoses in the CCI disease inventory. Diabetes was identified by fasting blood glucose ≥ 7 mmol/L, random blood glucose ≥ 11.1 mmol/L, HbA1c ≥ 6.5%, or hypoglycemic medication use. Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or the current use of antihypertensive medications. CKD was defined as eGFR < 60 mL/min/1.73m2. Chronic pulmonary disease includes a history of chronic obstructive pulmonary disease or asthma.
Statistical analysis
Patients’ baseline demographic and clinical characteristics were presented as mean ± standard deviation, median (interquartile range [IQR]), or percentages as appropriate for the total cohort and stratified by ischemic cardio-cerebrovascular disease numbers. Continuous variables were compared using a one-way analysis of variance or the Kruskal–Wallis test, as deemed appropriate. Categorical variables were compared using the chi-square test. Time-to-first event data were graphically presented using the Kaplan–Meier method. Cox proportional hazards regression was employed to calculate hazard ratios (HRs) with 95% CIs to examine the link between the comorbidity of ischemic cardio-cerebrovascular disease and all-cause mortality. The proportional hazard assumption was checked using Schoenfeld residuals. Before performing multivariable Cox proportional hazards regression analysis, the Mann–Whitney U test was used to ascertain the association between continuous variables in participants with the outcomes. Furthermore, Cox regression analysis was used to determine the association between the outcomes and each of the categorical variables. Variables for the multivariable Cox regression analysis were selected based on clinical knowledge or a significance probability of P < 0.2. To establish whether the continuous variables should be included as continuous or categorical variables in the model, restricted cubic splines were used to inspect nonlinear effects. The fully adjusted model included age, sex, BMI, smoking status, hemoglobin, CRP, albumin, BNP, TG, HDL, LDL, HbA1c, eGFR, history of hypertension or cancer, aspirin, ADP receptor inhibitors, beta-blockers, CCBs, and CCI-score. Missing category data on patients’ smoking status constituted 2.7% and were considered nonsmokers. Less than 5% of the baseline urine acid and HbA1c data were missing. Assumed to be missing at random, these data were imputed with multiple imputation of chained equations method using the R package “mice” (version 3.16).
To test the robustness and consistency of our findings, three sensitivity analyses were performed: (1) inverse probability of treatment weights (IPTW) was applied to balance confounding between two groups. The propensity score (PS) was determined by multivariable-adjusted logistic regression analysis using the variables listed in Table 1. IPTW was calculated by PS. Patients with CICCD and controls were matched 1:4 using the “greedy” nearest neighbor matching algorithm without replacement, with a caliper size of 0.05. The risk of mortality was tested by IPTW-based fully adjusted Cox regression model; (2) the fully adjusted model tested in male participants was used; and (3) to reduce the possibility of reverse causation in the long-term mortality analysis, patients who died within the 1st year of follow-up were excluded from the fully adjusted model.
Post hoc subgroup analysis was performed to explore whether the potential association between comorbidity of ischemic cardio-cerebrovascular disease and outcomes was moderated by the following clinical characteristics: age (≥ 80 and 65–79 years) [16], BMI (≥ 24 and < 24), smoking, hemoglobin (≤ 120 and > 120 g/L in men, ≤ 110 and > 110 g/L in women) [19], CRP (≥ 0.3 and < 0.3 mg/dL) [20], albumin (< 40 and ≥ 40 g/L) [21], TG (≥ 1.2 and < 1.2 mmol/L) [22], LDL (≥ 1.8 and < 1.8 mmol/L), eGFR (< 60 and ≥ 60 mL/min per 1.73 m2), hypertension, aspirin, ADP receptor inhibitors, statins, and CCBs.
Statistical analyses were conducted using SPSS 25.0 (SPSS, Inc.) and R version 4.2.1 (The R Project for Statistical Computing). Two-sided P < 0.05 was considered significant.
Results
Patient characteristics
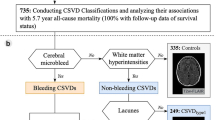
Finally, as shown in Fig. 1, 1026 patients with ischemic cardio-cerebrovascular disease were included, of which 912 (88.89%) had MICCD and 114 (11.11%) had CICCD. The median (IQR) age at the baseline was 82.90 (76.53, 86.40) years, including 5.6% of women. A total of 889 individuals were diagnosed with coronary artery disease, and 251 were diagnosed with stroke or TIA. Table 1 shows the characteristics of the participants. Patients with CICCD were more likely to be older (84.65 [81.03, 87.65] vs. 82.65 [75.80, 86.32]; difference, 2.20 years; 95% CI 1.00–3.40 years; P < 0.001), had higher TC (4.22 [3.81, 4.93] vs. 4.06 [3.50, 4.71] mmol/L; difference, 0.20 mmol/L; 95% CI 0.03–0.36 mmol/L; P = 0.019) and HDL (1.25 [1.08, 1.47] vs. 1.17 [0.96, 1.41] mmol/L; difference, 0.07 mmol/L; 95% CI 0.01–0.14 mmol/L; P = 0.023). The CCI-score was higher in patients with CICCD (4.00 [3.00, 4.00] vs 3.00 [3.00, 4.00]; difference, 0.00; 95% CI 0.00–1.00; P < 0.001). Medication use on statins seemed to be more prevalent in CICCD patients (64.91% vs 50.77%; difference, 14.14%; 95% CI 4.80%–23.49%; P = 0.006).
Age, hemoglobin, CRP, creatinine, albumin, BNP, HDL, LDL, HbA1c, eGFR, and CCI-score differed significantly between patients without and with all-cause mortality, and the only exceptions were UA and TC (Supplementary Table 1). Smoking status, cancer, and use of ADP receptor inhibitors and CCBs were associated with all-cause mortality in univariable analysis (Supplementary Table 2). Nonlinear relationships between the selected continuous variables and the risk of all-cause mortality were tested using restricted cubic splines (for nonlinearity, P < 0.001 for BNP, P = 0.039 for eGFR).
Variation in all-cause mortality
During a median follow-up of 10.4 (10.1–10.8) years, 398 patients experienced all-cause mortality. The incidence rate of all-cause mortality was 7.64 per 100 person-years among participants with CICCD and 4.84 per 100 person-years among participants with MICCD. Compared with patients having MICCD, those with CICCD had higher crude rates of all-cause mortality (Fig. 2A). After adjustment for age and other potential confounders (Table 2), CICCD was independently associated with a 71% increased risk of all-cause mortality (all-cause mortality: adjusted HR: 1.71; 95% CI 1.32–2.39). The results did not change in the sensitivity analysis (Table 3). In addition, anemia (adjusted HR: 1.48; 95% CI 1.16–1.89) and malnutrition (adjusted HR: 1.43; 95% CI 1.15–1.78) are also independent risk factors for all-cause mortality among the elderly and very elderly patients with ischemic cardio-cerebrovascular disease.
Ischemic cardio-cerebrovascular disease and all-cause mortality after propensity-score (PS) matching
Furthermore, after PS matching for prognostic factors that differed significantly between groups, a total of 114 cases from the CICCD group and 456 individuals from the control groups were considered for matched analysis. When the biases were eliminated by PS matching, the demographic and clinical characteristics were comparable between the two groups (P > 0.05; SMD < 0.10; Table 1). The median follow-up for the matched cohort was 10.1 years. In total, 334 patients experienced all-cause mortality. Compared with patients having MICCD, those with CICCD displayed higher rates of all-cause mortality (Fig. 2B). The fully adjusted model yielded similar results (all-cause mortality: adjusted HR: 2.07; 95% CI 1.47–2.90; Table 2).
Subgroup analysis
In the subgroup analysis, significant interactions were not observed between CICCD groups and age, BMI, smoking, CRP, albumin, TG, LDL, eGFR, hypertension, medication use aspirin, ADP receptor inhibitors, statins, and CCBs with regard to all-cause mortality (P-interaction > 0.05 for all). The association of CICCD with all-cause mortality was modified by hemoglobin status (P-interaction = 0.009). An increased risk of CICCD with all-cause mortality showed among anemia status (HR: 3.55; 95% CI 1.47–8.54) (Fig. 3).
Subgroup analyses. Subgroup analyses for the adjusted HR (95% CI) of ischemic cardio-cerebrovascular disease groups for long-term mortality by age, BMI, smoking, hemoglobin, CRP, albumin, TG, LDL, eGFR, hypertension, aspirin, ADP receptor inhibitors, statins, and CCB. BMI, body mass index; CCB, calcium channel blocker; MICCD, Mono ischemic cardio-cerebrovascular disease; CI, confidence interval; CRP, C-reactive protein; eGFR, estimated glomerular filtration rate; HR, hazard ratio; LDL, low-density lipoprotein; TG, triglycerides
Discussion
Main interpretation
Cardiac/neurologic-related chronic diseases remain the main killer worldwide [23,24,25,26,27,28,29]. The results of this study provide valuable insights into the association between comorbidity of ischemic cardio-cerebrovascular disease and all-cause mortality among Chinese elderly patients (see Fig. 4). A significant increase was noted in the risk of all-cause death in patients with CICCD and anemia or malnutrition, which may be predicted from admission. These findings persisted after adjusting for various confounding factors and in sensitivity analyses. Our results agree with the impact of poly-vascular disease on mortality outcomes reported in several studies [30,31,32], further strengthening this evidence by specifically focusing on the Chinese elderly population and examining the influence of comorbidity of ischemic cardio-cerebrovascular disease.
Atherosclerosis is a complex systemic disease driven by intricate pathophysiological mechanisms affecting the vascular wall's intima [33]. With advancing age, the incidence of vascular diseases rises, drawing significant attention to the characteristics of poly-vascular disease. Despite this, there is a lack of long-term follow-up studies on elderly patients with comorbid ischemic cardio-cerebrovascular disease (CICCD). Comprehensive assessment of patients with atherosclerotic disease, including detailed medical history and thorough physical examination, is crucial. Recent studies [34] indicate that the incidence of poly-vascular disease increases with age, with approximately 3.0% of asymptomatic patients showing vascular lesions in 2–3 different sites, significantly elevating the risk of all-cause mortality. Our study corroborates these findings, revealing that patients with CICCD have a markedly higher risk of all-cause mortality, with differences in prognosis evident as early as the first year of follow-up and persisting long-term. Therefore, screening elderly patients for poly-vascular diseases is justified.
Despite the elevated all-cause death risk among individuals with CICCD, our results also identified that being underweight and elevated triglyceride are other significant factors. Elderly patients with ICCD and higher BMI have better outcomes than those with lower BMI, a phenomenon often referred to as the “obesity paradox” [35]. Triglyceride contributes to atherosclerosis development by promoting atherogenic lipoprotein formation and inducing endothelial dysfunction [36]. Subgroup analysis showed that CICCD only matters when triglyceride is controlled in an ideal condition, underscoring the importance of managing triglyceride levels in elderly patients with ischemic cardio-cerebrovascular disease to improve their long-term prognosis.
In the present study, we note that our clinical cohort included more than 90% male participants, and potential gender bias could affect the representativeness of the results. To minimize potential gender bias that could affect the representativeness of the results, we performed sensitivity and subgroup analysis for individual men and women. There were no substantial differences in the strength of association between coronary artery disease, ischemic stroke/TIA, or all-cause death risk factors and sex in elderly patients. Our results are similar to the historical reports [37, 38].
Anemia ranks as the fifth cardiovascular risk factor following smoking, diabetes, hypertension, and dyslipidemia [39]. The following may be the underlying mechanisms [40]: (1) reduction in tissue oxygen intake; (2) increased instability of the plaque; and (3) decreased nitric oxide secretion. Past studies have suggested anemia as an independent risk factor for adverse outcomes in elderly individuals [41, 42]. Notably, our investigation also identified an intriguing interaction between cardio-cerebrovascular comorbidities and anemia concerning all-cause mortality. Subgroup analysis alluded that anemia may exacerbate the impact of ischemic cardio-cerebrovascular comorbidities on mortality risk. Malnutrition is associated with poor prognosis in various illnesses. Previous studies have shown that malnutrition has a strong impact on both short-term and long-term mortality in older adults, especially those with coronary artery disease [43, 44]. Once it occurs, malnutrition can advance to a condition known as overt cardiac cachexia. This comprehensive wasting syndrome impacts all bodily systems, including muscles, fats, and bones [45]. The origins of cachexia are complex and may stem from inadequate nutrition. Research has proposed that systemic inflammation can lead to a generally catabolic state by increasing the breakdown of proteins and decreasing their synthesis [46, 47]. Additionally, inflammation might contribute to a loss of appetite. These combined outcomes can result in protein-energy malnutrition and a reduced body mass index. Identifying patients at risk for developing cachexia may be achieved through early screening for malnutrition and its characterization.
In this special population, the findings of this study have also identified anemia and malnutrition as independent risk factors for elderly patients diagnosed with ischemic cardio-cerebrovascular disease. The significant impact of these factors on prognosis suggests that they should be a focal point in clinical management. With population life expectancy increasing, our study provides new, detailed insights into the long-term prognosis of elderly and very elderly patients with ischemic cardiovascular and cerebrovascular disease. It will provide valuable guidance for clinicians to optimize the management and treatment of this vulnerable population.
Limitations
The strengths of our study included the cohort design, confirmed medical reports, and long-term follow-up time. However, it should be noted that our study has several limitations. First, our investigation was conducted in a single medical center with over 90% male participants, and it lacked non-Asian elderly patients, thus limiting the generalizability of our findings to other ethnic or demographic groups. Second, all-cause mortality was used as the endpoint without distinguishing between cardiovascular and nonvascular deaths, which are inherently different in terms of their pathogenesis. Third, considering chronic kidney disease, diabetes, and peripheral artery disease are common comorbidities in elderly patients, we used the age-adjusted Charlson comorbidity index in the multivariate analysis to control confounders. Statistical analysis was not conducted on the degree of stenosis in peripheral vessels, renal arteries, and the abdominal aorta. Fourth, our study may include ischemic strokes from vascular dissection and moyamoya disease, potentially affecting the interpretation of the association between comorbidities of ischemic cardio-cerebrovascular disease and long-term outcomes in elderly patients, despite efforts to minimize non-atherosclerotic stroke impact.
Conclusion
In conclusion, the presence of comorbidity of ischemic cardio-cerebrovascular disease in elderly patients is associated with a higher burden of comorbidities and a progressive increase in long-term adverse prognosis. Patients with CICCD suffering from anemia or malnutrition appear to have a greater risk of all-cause mortality. These findings emphasize the need to acknowledge the accumulating risk linked with poly-vascular disease in elderly patients, owing to its consequential impact on risk assessment and the allocation of intensive and preventive medical interventions.
Data availability
The data are on https://www.jianguoyun.com/p/DbltF1cQuaiFChjRlbkFIAA.
Abbreviations
- BMI:
-
Body mass index
- BNP:
-
B-type natriuretic peptide
- CCBs:
-
Calcium channel blockers
- CCI:
-
Charlson Community Index
- CICCD:
-
Comorbidity of ischemic cardio-cerebrovascular disease
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CRP:
-
C-reactive protein
- eGFR:
-
Estimated glomerular filtration rate
- HbA1c:
-
Glycated hemoglobin
- HDL:
-
High-density lipoprotein
- HR:
-
Hazard ratio
- IPTW:
-
Inverse probability of treatment weights
- IQR:
-
Interquartile range
- LDL:
-
Low-density lipoprotein
- MICCD:
-
Mono ischemic cardio-cerebrovascular disease
- PSM:
-
Propensity-score matching
- RAASi:
-
Renin–angiotensin–aldosterone system inhibitors
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- TIA:
-
Transient ischemic attack
References
Feng J, Yang Y, Zhou Y, Wang B, Xiong H, Fan C, et al. Bakuchiol attenuates myocardial ischemia reperfusion injury by maintaining mitochondrial function: the role of silent information regulator 1. Apoptosis. 2016;21(5):532–45.
Zhang F, Liu L, Zhang C, Ji S, Mei Z, Li T. Association of metabolic syndrome and its components with risk of stroke recurrence and mortality: a meta-analysis. Neurology. 2021;97(7):e695–705.
Xu J, Zhang X, Jin A, Pan Y, Li Z, Meng X, et al. Trends and risk factors associated with stroke recurrence in China, 2007–2018. JAMA Netw Open. 2022;5(6): e2216341.
Lu X, Liu Z, Cui Q, Liu F, Li J, Niu X, et al. A polygenic risk score improves risk stratification of coronary artery disease: a large-scale prospective Chinese cohort study. Eur Heart J. 2022;43(18):1702–11.
Gioscia R, Castagno C, Verdoia M, Conti B, Forliti E, Rognoni A. Optimization of the pharmacological therapy in patients with poly-vascular disease: a multidisciplinary approach. World J Cardiol. 2023;15(4):142–53.
Gutierrez JA, Aday AW, Patel MR, Jones WS. Polyvascular disease: reappraisal of the current clinical landscape. Circ Cardiovasc Interv. 2019;12(12): e007385.
Jansen-Chaparro S, Lopez-Carmona MD, Cobos-Palacios L, Sanz-Canovas J, Bernal-Lopez MR, Gomez-Huelgas R. Statins and peripheral arterial disease: a narrative review. Front Cardiovasc Med. 2021;8: 777016.
Takeuchi M, Wada H, Ogita M, Takahashi D, Okada-Nozaki Y, Nishio R, et al. Impact of prior stroke on long-term outcomes in patients with acute coronary syndrome. Circ Rep. 2021;3(5):267–72.
Attar R, Wester A, Koul S, Eggert S, Andell P. Peripheral artery disease and outcomes in patients with acute myocardial infarction. Open Heart. 2019;6(1): e001004.
De Luca L, Di Pasquale G, Gonzini L, Chiarella F, Di Chiara A, Boccanelli A, et al. Trends in management and outcome of patients with non-ST elevation acute coronary syndromes and peripheral arterial disease. Eur J Intern Med. 2019;59:70–6.
Adam L, Strickler E, Borozadi MK, Bein S, Bano A, Muka T, et al. Prognostic role of polyvascular involvement in patients with symptomatic peripheral artery disease. J Clin Med. 2023;12(10):3410.
Writing Committee of the Annual Report on Cardiovascular Health and Diseases in China. Interpretation of the annual report on cardiovascular health and diseases in China 2022. Cardiol Discov. 2024;4(1):58–80.
Bai R, Liu Y, Zhang L, Dong W, Bai Z, Zhou M. Projections of future life expectancy in China up to 2035: a modelling study. Lancet Public Health. 2023;8(12):e915–22.
Gao S, Wang YJ, Xu AD, Li YS, Wang DZ. Chinese ischemic stroke subclassification. Front Neurol. 2011;2:6.
Park JH, Seo EJ, Bae SH. Incidence and risk factors of cardio-cerebrovascular disease in Korean menopausal women: a retrospective observational study using the Korean genome and epidemiology study data. Asian Nurs Res (Korean Soc Nurs Sci). 2021;15(4):265–71.
Zhang Y, Xiong Y, Yu Q, Shen S, Chen L, Lei X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. 2021;21(1):30.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Bannay A, Chaignot C, Blotiere PO, Basson M, Weill A, Ricordeau P, et al. The best use of the Charlson Comorbidity index with electronic health care database to predict mortality. Med Care. 2016;54(2):188–94.
Zakai NA, French B, Arnold AM, Newman AB, Fried LF, Robbins J, et al. Hemoglobin decline, function, and mortality in the elderly: the cardiovascular health study. Am J Hematol. 2013;88(1):5–9.
Menon V, Greene T, Wang X, Pereira AA, Marcovina SM, Beck GJ, et al. C-reactive protein and albumin as predictors of all-cause and cardiovascular mortality in chronic kidney disease. Kidney Int. 2005;68(2):766–72.
Choi SR, Lee YK, Cho AJ, Park HC, Han CH, Choi MJ, et al. Malnutrition, inflammation, progression of vascular calcification and survival: inter-relationships in hemodialysis patients. PLoS ONE. 2019;14(5): e0216415.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Back M, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–337.
Li T, Jiang S, Yang Z, Ma Z, Yi W, Wang D, et al. Targeting the energy guardian AMPK: another avenue for treating cardiomyopathy? Cell Mol Life Sci. 2017;74(8):1413–29.
Li X, Liu L, Li T, Liu M, Wang Y, Ma H, et al. SIRT6 in senescence and aging-related cardiovascular diseases. Front Cell Dev Biol. 2021;9: 641315.
Zhang M, Wang S, Cheng Z, Xiong Z, Lv J, Yang Z, et al. Polydatin ameliorates diabetic cardiomyopathy via Sirt3 activation. Biochem Biophys Res Commun. 2017;493(3):1280–7.
Liao W, Xu J, Li B, Ruan Y, Li T, Liu J. Deciphering the roles of metformin in Alzheimer’s disease: a snapshot. Front Pharmacol. 2021;12: 728315.
Li T, Providencia R, Mu N, Yin Y, Chen M, Wang Y, et al. Association of metformin monotherapy or combined therapy with cardiovascular risks in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2021;20(1):30.
Li T, Mu N, Yin Y, Yu L, Ma H. Targeting AMP-Activated protein kinase in aging-related cardiovascular diseases. Aging Dis. 2020;11(4):967–77.
Jiang S, Yang Y, Li T, Ma Z, Hu W, Deng C, et al. An overview of the mechanisms and novel roles of Nrf2 in cardiovascular diseases. Expert Opin Ther Targets. 2016;20(12):1413–24.
Gutierrez JA, Scirica BM, Bonaca MP, Steg PG, Mosenzon O, Hirshberg B, et al. Prevalence and outcomes of polyvascular (coronary, peripheral, or cerebrovascular) disease in patients with diabetes mellitus (from the SAVOR-TIMI 53 Trial). Am J Cardiol. 2019;123(1):145–52.
Chunawala ZS, Qamar A, Arora S, Pandey A, Fudim M, Vaduganathan M, et al. Prevalence and prognostic significance of polyvascular disease in patients hospitalized with acute decompensated heart failure: the ARIC study. J Card Fail. 2022;28(8):1267–77.
Manolis AA, Manolis TA, Manolis AS. Patients with polyvascular disease: a very high-risk group. Curr Vasc Pharmacol. 2022;20(6):475–90.
Alkhalil M, Kuzemczak M, Whitehead N, Kavvouras C, Dzavik V. Meta-analysis of intensive lipid-lowering therapy in patients with polyvascular disease. J Am Heart Assoc. 2021;10(5): e017948.
Zhang Q, Wang A, Zhang S, Li N, Chen S, Zhang Y, et al. Asymptomatic polyvascular disease and the risks of cardiovascular events and all-cause death. Atherosclerosis. 2017;262:1–7.
Tutor AW, Lavie CJ, Kachur S, Milani RV, Ventura HO. Updates on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2023;78:2–10.
Talayero BG, Sacks FM. The role of triglycerides in atherosclerosis. Curr Cardiol Rep. 2011;13(6):544–52.
Benson RA, Okoth K, Keerthy D, Gokhale K, Adderley NJ, Nirantharakumar K, et al. Analysis of the relationship between sex and prescriptions for guideline-recommended therapy in peripheral arterial disease, in relation to 1-year all-cause mortality: a primary care cohort study. BMJ Open. 2022;12(3): e055952.
Ntaios G, Lip GYH, Vemmos K, Koroboki E, Manios E, Vemmou A, et al. Age- and sex-specific analysis of patients with embolic stroke of undetermined source. Neurology. 2017;89(6):532–9.
Fonseca AC, Silva DP, Infante J, Ferro JM. Cerebrovascular complications of anemia. Curr Neurol Neurosci Rep. 2021;21(10):51.
Venugopalan Pathiyil D, Henry RA, Joseph J, Oomen AT, Janardhanan KJ. Severe iron deficiency anemia leading to thrombocytosis with arterial and venous thrombosis. Cureus. 2021;13(9): e17893.
Hanna RM, Streja E, Kalantar-Zadeh K. Burden of anemia in chronic kidney disease: beyond erythropoietin. Adv Ther. 2021;38(1):52–75.
Khalaji A, Ajam A, Sheikhy A, Behnoush AH, Fallahzadeh A, Bagheri J, et al. Mortality across the spectrum of hemoglobin level in patients undergoing surgical coronary revascularization. Clin Cardiol. 2023;46(5):535–42.
Liu J, Huang Z, Huang H, He Y, Yu Y, Chen G, et al. Malnutrition in patients with coronary artery disease: prevalence and mortality in a 46,485 Chinese cohort study. Nutr Metab Cardiovasc Dis. 2022;32(5):1186–94.
Raposeiras Roubin S, Abu Assi E, Cespon Fernandez M, Barreiro Pardal C, Lizancos Castro A, Parada JA, et al. Prevalence and prognostic significance of malnutrition in patients with acute coronary syndrome. J Am Coll Cardiol. 2020;76(7):828–40.
Muscaritoli M, Imbimbo G, Jager-Wittenaar H, Cederholm T, Rothenberg E, di Girolamo FG, et al. Disease-related malnutrition with inflammation and cachexia. Clin Nutr. 2023;42(8):1475–9.
Kunimura A, Ishii H, Uetani T, Aoki T, Harada K, Hirayama K, et al. Impact of Geriatric Nutritional Risk Index on cardiovascular outcomes in patients with stable coronary artery disease. J Cardiol. 2017;69(1):383–8.
Sze S, Pellicori P, Kazmi S, Rigby A, Cleland JGF, Wong K, et al. Prevalence and prognostic significance of malnutrition using 3 scoring systems among outpatients with heart failure: a comparison with body mass index. JACC Heart Fail. 2018;6(6):476–86.
Acknowledgements
We thank the staff of the Medical Big Data Research Center, Medical Innovation Research Department of PLA General Hospital for their contributions. We also thank Dr. T.L. and EditorBar Language Editing for their language editing.
Funding
The study was supported by Grants from the National Key Research and Development Program of China (No. 2022YFC3602400).
Author information
Authors and Affiliations
Contributions
We thank Prof. F.C. for designing the whole project. We also appreciate Dr. LB.C., Dr. SS.S, Dr. ZH.G., Dr. ZY.F. and Dr. S.G. for collecting the data. Dr. Q.Y. did the analysis, wrote the main manuscript, and prepared Figs. 1–4. Dr. YJ.Z., Dr. SJ.C and Dr. NY.S. scrubbed data and maintained research data for initial use and later reuse. Prof. YB.W. supervised the drafting of the manuscript. All the authors have read and approved the final manuscript and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol complied with the tenets of the Declaration of Helsinki and was approved by the ethics committee of the Chinese People’s Liberation Army General Hospital (S2021-326-02).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
40001_2024_1929_MOESM1_ESM.docx
Additional file 1. Table S1. Comparison between participants with and without all-cause mortality for continuous variables.
40001_2024_1929_MOESM2_ESM.docx
Additional file 2. Table S2. Univariable Cox regression for the association of categorical variables with all-cause mortality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, Q., Sun, S., Cui, LB. et al. Ischemic cardio-cerebrovascular disease and all-cause mortality in Chinese elderly patients: a propensity-score matching study. Eur J Med Res 29, 330 (2024). https://doi.org/10.1186/s40001-024-01929-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-01929-x