Abstract
Background
Varicose vein is a chronic condition that affects the lower extremities of the human body. Several factors have been implicated in the development of this disease, viz age, gender, weight, height and prolonged standing. Recently, genome-wide studies have identified genetic biomarkers that are associated with varicose veins in different ethnic groups. Such genetic studies are lacking in South Asians specifically in Indians where the prevalence of varicose veins is high, and it is important to replicate these variants in the stated population. The study aimed to replicate the association of genetic variants associated with varicose veins in this target population, which were found to be associated with the other ethnic groups.
Methodology
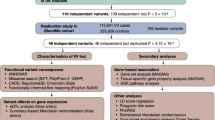
The studied cohort is of the Indian population comprising unrelated 104 varicose veins cases and 448 non-varicose vein controls. The samples were genotyped using the Illumina Global Screening Array. Using the genomic data from UK BioBank and 23andMe studied cohorts; eight genetic variants were selected to replicate in our dataset. The allelic association was performed to identify the effective allele and risk was estimated using odds ratio and p-value as level of significance. Multifactor Dimensionality Reduction was used to estimate the cumulative effect of variants in Indians.
Result
Variant rs3791679 of EFEMP1 was found to be associated with varicose veins in Indians. After observing the association of the EFEMP1 with varicose veins, we further ensued to identify all genetic variants within EFEMP1 to uncover the additional variants associated with this trait. Interestingly, we identified six new variants of EFEMP1 gene that have shown association. Moreover, the cumulative effect of all associated variations was estimated and the risk was 2.7 times higher in cases than controls whereas independently their effect ranges from 0.37–1.58.
Conclusion
This study identifies EFEMP1 as a potential gene related to the risk of varicose veins in Indians. It also highlights that evaluating the maximum number of variants of a gene rather than focusing solely on replicating single variations offers a more comprehensive and nuanced understanding of the genetic factors contributing to a complex trait like varicose veins.
Similar content being viewed by others
Introduction
Varicose veins (VV) is a prevalent venous disorder characterized by the dilated, tortuous, elongated subcutaneous veins of the legs that occur due to a multitude of factors, primarily affecting either the vein valve functionality or the vein wall [1]. To obtain a degree of uniformity one of the most common classifications used for VV is CEAP classification (clinical, etiological, anatomical, and pathophysiological) [2, 3]. Clinically, the patients present with one of the following: complaints, cosmesis or complications of varicose veins, with venostatic symptoms being the most common presentation, closely followed by the need for esthetics [4].
Characteristic features of VV include dilated, tortuous, elongated subcutaneous veins that appear on the lower extremities. It causes discomfort, pain, and cosmetic concerns, and in some cases, leads to severe morbidity [5]. The pathophysiology of VV involves a complex interplay of venous insufficiency and valvular dysfunctions [6]. Several theories have been forecasted and tested in the last century including the leucocyte entrapment theory, fibrin cuff theory and the ambulatory venous hypertension theory. Despite all odds ambulatory venous hypertension theory has held its ground and is the most accepted theory in the contemporary world [7]. Collaborative evidence directs towards the valvular dysfunction which primarily affects the one-way valves in the veins, contributing to the retrograde flow of blood and further exacerbating venous insufficiency [8]. These collectively result in involvement of the vein valve and the vein wall thus leading to venous dilation, increased wall tension, and subsequent varicose vein formation [9, [10].
The reported prevalence of VV varies from 5 to 60% depending on the age group, underscoring the urgent need to identify the contributing variables [11,12,13,14]. Numerous risk factors have been identified that contribute to the development and progression of varicose veins. Advancing age, genetic predisposition, and female gender are considered non-modifiable risk factors [15]. Hormonal influences, such as pregnancy and hormonal replacement therapy are implicated in worsening the condition [16]. Lifestyle factors, including occupations demanding prolonged standing, obesity, and lack of physical activity, are modifiable risk factors that can be addressed to reduce the likelihood of varicose vein [17]. Review of the extant world literature reveals that different ethnicities have different disease-related genes that induce VV [11, 18,19,20,21]. Genetic studies of VV in Indians are almost absent and only CASZ1 variants have shown susceptibility towards the risk of VV in South Asian Indians by our research group (unpublished study). To identify more genetic variants associated with VV to explain the missing heritability in the background of significant disease burden of VV in Indians, the present study has replicated the newly identified risk loci in South Asian Indians. This study was an endeavor to provide insight into the role of genetics in the development of VV and to decipher potential risk markers in the studied population group.
Materials and methods
Sample collection criteria
The study cohort of 552 individuals comprised 104 cases of primary VV and 448 controls. The clinical, etiological, anatomical, and pathological (CEAP) classification was used to categorize these individuals [22]. Each patient was assessed by a group of expert vascular surgeons. A phlebotomist collected 3–4 mL of blood under stringent aseptic conditions after obtaining the consent of the patient in ethylenediamine tetra acetic acid (EDTA) vials which were maintained at 4 °C. The study was approved by Institutional Ethical committee (IEC reg No. 35/2021).
DNA isolation and genotyping
DNA was isolated using the QIAGEN DNA Mini Kit by following the manufacturer’s protocol. The quality and concentration of DNA was checked on 1% Agarose gel. After screening of the DNA samples, they underwent the genotyping using the Illumina Global Screening Array. The genotyping process was adapted from our earlier work [23]. The genotype call rate observed was greater than 98% and GenomeStudio 2.0 software was used to convert the genotyping data into plink format files for further analysis.
SNP selection
Eight genetic variations that were found to be associated with VV in UK Bio Bank and 23andMe cohort were taken for the evaluation [24] and were also present in our dataset. The details of the replicated variants are summarized in Additional file 1: Table S1.
Data analysis
Continuous socio-demographic, anthropometric and clinical data were provided as an average and count of individuals, with frequency expressed as a percentage and standard deviation (Additional file 1: Table S2).The genetic data analysis was done using the plink 1.09 [25]. Hardy–Weinberg equilibrium (HWE) was determined for each variation. Variant with call rate of < 95% and minor allele frequency < 0.05, or deviation from HWE (Phwe < 0.05) were excluded from downstream analysis. After data quality check, the genotypes of each variant were extracted using command—extract snps.txt—recode from the large dataset. The association of variants was estimated using odds ratio and 95% confidence interval (CI) with respect to minor allele frequency. The synergic effect of significantly associated SNPs was estimated using Multifactor Dimensionality Reduction (MDR) software [26]. The variations that were found to be associated were further evaluated for the linkage disequilibrium using Haploview [27].
Results
The replication study included 104 patients with primary VV and 448 control samples. The socio-demographic details of cases and controls are summarized in Additional file 1: Table S2. The present cohort of VV was categorized according to the CEAP classification system and it showed the following distribution pattern: 7.77% of cases fell under C1disease; the majority, accounting for 53.40% of cases, were classified as C2 disease, signifying the presence of varicose veins; 14.56% were categorized as C3, indicating edema; while 10.68%, 8.74%, and 4.85% were classified as C4 (pigmentation and/or eczema), C5 (healed ulcer), and C6 (active ulcer), respectively. These findings are summarized in Additional file 1: Table S3.
Initially, the association was carried out among eight genetic variants which were previously found to be associated with VV in GWAS (Additional file 1: Table S1). Out of these eight genetic variants, EFEMP1 variant rs3791679 was found to be significantly associated with VV in the studied cohort. The OR observed for EFEMP1 variant rs3791679 was 1.43 (1.04–1.97, at 95% CI) implicating it as a potential gene causing risk of VV in Indians (Table 1).
Considering EFEMP1 as a potential candidate gene for VV in Indians, we evaluated all the variations of EFEMP1 present in our dataset. A total of 27 variants were screened. After applying quality check parameters, 21 variations (Additional file 1: Table S4) passed the quality check. Out of these 21 variations, six variants were found to be associated on the basis of their OR and p-value. The OR had a range of 0.37–1.58 and p-value of < 0.05 (Table 2). The variant rs3791665 which was causing protection had an OR of 0.37 and the other five variations rs3791679, rs59985551, rs3791675, rs11125610, rs1430197 were causing risk of VV and had a high OR of 1.36–1.58 (Table 2). Furthermore, in the evaluation of linkage disequilibrium (LD) among the six associated SNPs of EFEMP1, a robust LD association was observed between rs59985551 and rs3791675 at a genomic distance of 4 kb, with an R2 0.94 (Fig. 1) in the studied cohort.
The interactive association of LD variants was also estimated and no association was observed OR 1.50 (95%CI 0.80–2.81, p-value 0.20). This observation prompted us to explore the cumulative effect of all six SNPs in the studied cohort to shed light on the potential synergistic impact of these genetic variations on VV susceptibility. Assessment of the cumulative effect of six significantly associated variants revealed that the risk increases 2.7 times of the risk caused by independent variants. The OR observed was 2.73 (1.75–4.23, 95% CI) with a p-value < 0.00001. MDR analysis showed that the risk contribution of all six associated variants increased to 2.7 times than the independent risk, indicating multiple small effects of different variants of EFEMP1 gene plays crucial role in the development of VV in the studied population group.
Discussion
Varicose veins are defined as dilated, tortuous, elongated subcutaneous veins of ≥ 4 mm diameter. A multitude of risk factors like chronic cough, constipation, family history of venous diseases, gender, obesity, advanced age, pregnancy, and prolonged periods of standing have been implicated in the development of VV. Although precise pathophysiology is a subject of debate, VV is believed to encompass a genetic predisposition leading to dysfunctional vein valves, compromised vascular walls, expressing as elevated venous pressure within the axial veins and tributaries [28]. The heredity seems to influence the etiology, yet the genetic factors are poorly understood. Decoding this elusive genetic component will open new frontiers to determine the molecular triggers of the disease, extending insights into the pathophysiology, and redefine the goals of management.
Several studies have been conducted to find out the genetic association of different genes with VV [18, 19, 29,30,31,32]. In this study, we found that EFEMP1 gene and its variants play an important role in the pathophysiology of VV. The gene shows significant association in the studied Indian cohort and it emphasizes its genetic role in the development of VV, as already proven in the German population [33].
Previously, we found out that CASZ1 gene has shown susceptibility towards association with VV (paper under revision) in South Asian Indians. Taking lead, we did a replication study for another eight genetic variants which have been studied in Europeans [24]. Out of these variations, one of the variations rs3791679 of EFEMP1 gene showed a strong association as a risk factor for VV in Indian cohort.
As we investigated the other 27 variations of EFEMP1 gene and screened them for their potential link to varicose veins, only six variations passed quality check parameters. These 6 variations were responsible for the development of VV and had OR of 0.37–1.58 and a p-value of < 0.05 and were analyzed using reactome pathway database [34] (Additional file 1: Fig. S1). These variants were found to play a significant role in pathways linked to extracellular matrix organization and molecules associated with elastic fibers thus indicating association with maintenance of structural and mechanical integrity of the vein’s architecture. They thus hold the potential to serve as genetic markers for detecting VV in individuals of Indian descent.
Open Targets Genetics platform [35] was used to confirm the association between six variants of EFEMP1 using a phenome-wide association study (PheWAS) approach) using GWAS catalog and UK BioBank database. One of the lead variant (rs3791679) demonstrated an association with various phenotypes including VV (Additional file 1: Fig. S2). Five variations were found to offer at risk potential and one variation offered protection.
To ascertain the cumulative effect of these 6 preferably use one connotation only, either numerical 6 or alphabet six variants, MDR was performed for the associated SNPs. We found that their contribution towards the risk of VV increased 2.7 times as compared to their individual risks. It shows that the multiple small effects of different variants of EFEMP1 gene plays crucial role in the development of VV in the studied population group.
The present study provides an insight into studying multiple variants within a single gene for a complex trait and necessity of extending our findings to larger and more diverse ethnic cohorts. To establish EFEMP1 as a viable candidate gene for VV additional research involving different ethnicities to investigate the variations linked to the disease risk.
The present study heralds a conscious reasoning into the complex genetic landscape of VV, stressing the importance of EFEMP1 gene variations in the Indian population. The outcomes echo existence of potential genetic markers for detecting VV and highlight the role of numerous genetic variations of same phenotypic disease development. This study contributes to a better scientific understanding of the genetic basis of VV in an unexplored population cohort with a sizable disease burden. The findings might have far reaching ramifications in shaping management protocols with advent of further translational research.
Availability of data and materials
The datasets utilized and/or analyzed during the present study are accessible from the corresponding author upon reasonable request.
References
Nael R, Rathbun S. Treatment of varicose veins. Curr Treat Options Cardiovasc Med. 2009;11(2):91–103.
Bergan JJ, et al. Chronic venous disease. N Engl J Med. 2006;355(5):488–98.
Wang M, Sharma AK. Varicose veins. J Radiol Nurs. 2019;38(3):150–4.
Teruya TH, Ballard JL. New approaches for the treatment of varicose veins. Surg Clin N Am. 2004;84(5):1397–417, viii–ix.
Campbell B. Varicose veins and their management. BMJ. 2006;333(7562):287–92.
Fan CM. Venous pathophysiology. Semin Intervent Radiol. 2005;22(3):157–61.
Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation. 2005;111(18):2398–409.
Min RJ, Khilnani NM, Golia P. Duplex ultrasound evaluation of lower extremity venous insufficiency. J Vasc Interv Radiol. 2003;14(10):1233–41.
Raffetto JD, Khalil RA. Mechanisms of varicose vein formation: valve dysfunction and wall dilation. Phlebology. 2008;23(2):85–98.
Callam MJ. Epidemiology of varicose veins. Br J Surg. 1994;81(2):167–73.
Evans CJ, et al. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. J Epidemiol Community Health. 1999;53(3):149–53.
Joseph N, et al. A multicenter review of epidemiology and management of varicose veins for national guidance. Ann Med Surg (Lond). 2016;8:21–7.
Krysa J, Jones GT, van Rij AM. Evidence for a genetic role in varicose veins and chronic venous insufficiency. Phlebology. 2012;27(7):329–35.
Ramu A, Kenchetty P, Chidananda A. Varicose veins: our experience in KVG Medical College and Hospital, Karnataka. Int Surg J. 2021;8:3392.
AlBader B, et al. Prevalence of varicose veins among nurses at different departments in a single tertiary care center in Riyadh. Cureus. 2020;12(12): e12319.
Garcia-Honduvilla N, et al. Increase and redistribution of sex hormone receptors in premenopausal women are associated with varicose vein remodelling. Oxid Med Cell Longev. 2018;2018:3974026.
Elamrawy S, et al. Epidemiological, life style, and occupational factors associated with lower limb varicose veins: a case control study. J Egypt Public Health Assoc. 2021;96(1):19.
Helkkula P, et al. Genome-wide association study of varicose veins identifies a protective missense variant in GJD3 enriched in the Finnish population. Commun Biol. 2023;6(1):71.
Shadrina A, et al. Genome-wide association study in ethnic Russians suggests an association of the MHC class III genomic region with the risk of primary varicose veins. Gene. 2018;659:93–9.
Shashkova TI, et al. The GWAS-MAP platform for aggregation of results of genome-wide association studies and the GWAS-MAP|homo database of 70 billion genetic associations of human traits. Vavilovskii Zhurnal Genet Selektsii. 2020;24(8):876–84.
Makivaara LA, et al. Persons with varicose veins have a high subsequent incidence of arterial disease: a population-based study in Tampere, Finland. Angiology. 2007;58(6):704–9.
Rabe E, Pannier F. Clinical, aetiological, anatomical and pathological classification (CEAP): gold standard and limits. Phlebology. 2012;27(Suppl 1):114–8.
Bhat KG, et al. Preliminary genome wide screening identifies new variants associated with coronary artery disease in Indian population. Am J Transl Res. 2022;14(7):5124–31.
Ahmed WU, et al. Genome-wide association analysis and replication in 810,625 individuals with varicose veins. Nat Commun. 2022;13(1):3065.
Purcell S, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81(3):559–75.
Motsinger AA, Ritchie MD. Multifactor dimensionality reduction: an analysis strategy for modelling and detecting gene-gene interactions in human genetics and pharmacogenomics studies. Hum Genomics. 2006;2(5):318–28.
Barrett JC, et al. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21(2):263–5.
Jones RH, Carek PJ. Management of varicose veins. Am Fam Physician. 2008;78(11):1289–94.
Lee ML, et al. A genome-wide association study for varicose veins. Phlebology. 2022;37(4):267–78.
Fukaya E, et al. Clinical and genetic determinants of varicose veins. Circulation. 2018;138(25):2869–80.
Grant Y, Onida S, Davies A. Genetics in chronic venous disease. Phlebology. 2017;32(1):3–5.
Mariya AS, et al. The genetic constituent of varicose vein pathogenesis as a key for future treatment option development. Vessel Plus. 2021;5:19.
Ellinghaus E, et al. Genome-wide association analysis for chronic venous disease identifies EFEMP1 and KCNH8 as susceptibility loci. Sci Rep. 2017;7(1):45652.
Fabregat A, et al. Reactome pathway analysis: a high-performance in-memory approach. BMC Bioinform. 2017;18(1):142.
Ghoussaini M, et al. Open targets genetics: systematic identification of trait-associated genes using large-scale genetics and functional genomics. Nucleic Acids Res. 2021;49(D1):D1311–20.
Acknowledgements
All authors acknowledges Dr. Indu Sharma, University of South California for support in data analyses and reconfirming results by reiterating data and Dr. Nidhi Chahal, NMC Genetics India Pvt. Ltd. for providing valuable suggestion while revising the manuscript.
Funding
None.
Author information
Authors and Affiliations
Contributions
RM, VP, and RD primarily designed the study; patient screening and collection of samples, GR, LG, and AS were involved in generating and compiling the data, VS, CC, RM, and RS analyzed the data, VS, SK, RM, and AS wrote the manuscript. RS, VP, RM, and DS critically revised and edited the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The population-based case control study has been approved by Institutional Ethical committee. (Approval No.: IEC reg No. 35/2021).
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Additionally, it is important to note that Dr. Anuka Sharma, Love Gupta, Garima Rastogi, and Dr. Varun Sharma are affiliated with NMC Genetics India Pvt. Ltd., serving as its employees, for the purpose of disclosure.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Genetic Variants that were replicated in Indians and are adopted from GWAS. Table S2. Socio Demographic details observed in Case and Control. Table S3. Frequency of CEAP classification observed in the studied cases of varicose veins. Table S4. Twenty one variants of EFEMP1 that have passed the QC and evaluated for association of VV in studied cohort. Table S5. Allele frequency and functional annotation of EFEMp1 variants observed in the 1000genome and gnomAD. Figure S1. Pathway analysis of EFEMP1 variants using Reactome pathway database. Figure S2. The forest plot depicting various traits associated with the lead variant of EFEMP1 (rs3791679) revealed significant connections with different phenotypes, including deep vein thrombosis, chronic venous insufficiency, etc. https://genetics.opentargets.org/ was used to access the data of GWAS catalog and UK biobank.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mehra, R., Patra, V., Dhillan, R. et al. Replication study identified EFEMP1 association with varicose vein predisposition among Indians. Eur J Med Res 29, 232 (2024). https://doi.org/10.1186/s40001-024-01786-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-01786-8