Abstract
Background
It is common to support cardiovascular function in critically ill patients with extracorporeal membrane oxygenation (ECMO). The purpose of this study was to identify patients receiving ECMO with a considerable risk of dying in hospital using machine learning algorithms.
Methods
A total of 1342 adult patients on ECMO support were randomly assigned to the training and test groups. The discriminatory power (DP) for predicting in-hospital mortality was tested using both random forest (RF) and logistic regression (LR) algorithms.
Results
Urine output on the first day of ECMO implantation was found to be one of the most predictive features that were related to in-hospital death in both RF and LR models. For those with oliguria, the hazard ratio for 1 year mortality was 1.445 (p < 0.001, 95% CI 1.265–1.650).
Conclusions
Oliguria within the first 24 h was deemed especially significant in differentiating in-hospital death and 1 year mortality.
Similar content being viewed by others
Introduction
Patients with severe heart or lung failure can benefit from extracorporeal membrane oxygenation (ECMO). ECMO was required for critically ill patients with guarded prognoses regardless of the initial etiology [1]. Taiwan's national registry reports that the overall morality of adults was near 60% after 1 month and 75% after 1 year [2]. At 1 month and 1 year, overall mortality rates were near 30 and 45%, respectively, for patients under 18 years [3]. As an invasive procedure, ECMO is associated with bleeding, embolisms, and infections [2, 3]. Consequently, finding objective criteria to select suitable critical care candidates for ECMO and to identify those likely to require extraordinary measures is crucial [4].
To predict outcomes in patients receiving ECMO support, risk scores have been developed, such as the Survival After Veno-Arterial ECMO (SAVE) Score and the ECMO-ACCEPTS Score [4,5,6,7,8]. The prognosis of using ECMO and the potential to receive subsequent therapy is highly variable among individuals according to their underlying etiologies and baseline pathophysiological conditions. Consequently, the reported discriminatory power (DP) of these approaches varies based on the inclusion criteria, ECMO setup, statistical algorithms, stratification strategies, and system evaluation.
The highly correlated variables included in the analysis could also be a significant reason for this disequilibrium. Despite the fact that these clinical parameters represent damage to different organs, there is interaction between these organs, and they are always interconnected. Due to this, it is vital to clarify this issue using a different method than the traditional one. Using newly developed machine learning algorithms to perform supervised classification, it sheds light on a distinct method of clarifying this issue [9,10,11,12].
Machine learning algorithms employ various methods, such as probabilistic and optimization approaches, to learn from past experience and detect useful patterns in large, unstructured and complex data sets [13]. The random forest algorithm (RF) has shown superior accuracy for disease prediction among multiple supervised machine learning algorithms [13]. To determine the most reliable predictor of clinical outcome for ECMO patients, we have applied this novel algorithm and also compared to the conventionally used logistic regression (LR) model.
Methods
Setting and participants
Data from the ECMO registry of a single medical center in Taiwan were retrospectively analyzed. All patients on ECMO were included in the analysis. As potential predictive markers of future outcomes, clinical metrics were collected prior to ECMO and early in resuscitation. This study has been conducted in accordance with the ethical standards in the 1964 Declaration of Helsinki. The collection and review of patient information was approved by the Institutional Review Board of National Taiwan University Hospital (#201002034R, 2010/02, ECMO data analysis study).
Materials
As part of the analysis, demographic, anthropometric, cardiorespiratory, standard laboratory tests, inotropic therapy, urine output, and ventilator settings were used both before and after ECMO placement (Additional file 1: Table S1). Placement of ECMO was classified as cardiovascular, respiratory, or other. A binary ECMO mode was available: veno-arterial (VA) or veno-venous (VV). A single metric labeled inotropic equivalent (IE) was developed by combining dopamine, dobutamine, epinephrine, norepinephrine, isoproterenol, and milrinone in inotropic therapy [14]. Cardiopulmonary resuscitation, intra-aortic balloon pump support, renal replacement therapy, infection, and the Glasgow Coma Scale (GCS) were recorded [1, 4, 5, 7, 15]. It was possible to calculate different risk scores by combining these variables. A total of 55 parameters were available as predicting variables (features). Serial renal function and blood lactate collected afterward in the intensive care unit were not considered early markers and, therefore, were not used. In-hospital mortality during the index hospitalization when ECMO was instituted was the primary endpoint of this study. We recorded the date, time, and cause of death.
Management of missing data
Missing data points are inevitable in a data set of this size. To avoid listwise deletion in the following analyses, a mean value was substituted for continuous variables or the most frequent value for categorical variables if the absent variable comprised less than 5% of the total values. As per clinical convention, continuous measures with a higher percentage of missing data (> 5%) were categorized into three (normal, abnormal, and missing) or four classes (high, intermediate, low, and missing). Additional file 1: Table S1 shows details of data management for each variable. For every patient, the target outcome variable (in-hospital death) was available.
Statistics
The baseline characteristics of the patients are reported as a distinct group. We presented continuous variables as means and standard deviations (SD) and categorical variables as percentages. We estimated the probability of in-hospital death using a random forest (RF) and multi-variable logistic regression (LR) model. All predicting variables were included in the "non-parsimonious model," regardless of their statistical significance or potential collinearity. Based on this model, each individual was assigned a risk score. Further receiver operating characteristic (ROC) curve analysis used this "estimator" as the test variable. To identify variables statistically associated with in-hospital death, a novel LR model was applied (stepwise selection, p < 0.05 for inclusion). We developed a parsimonious model using the newly selected variables partitioned as before with recalculated AUC of ROCs.
Feature importance is the degree to which a feature (or a predicting factor) relates to the target outcome. The Gini importance calculated from the RF structure was used to identify the most relevant features among the predicting variables based on the mean decreased "impurity" [16, 17]. To ensure that the select feature also played an imperative role when different models were applied, LR was used again to calculate feature importance [17].
According to the select feature, survival analyses were performed regarding overall mortality up to 1 year, including Kaplan Meier curves, log-rank tests, and Cox regression models. In this study, the duration of ECMO was defined as beginning at the time of its placement and ending at the date of death (event), 1 year after the placement of ECMO, or termination of the study (censored).
IBM SPSS Statistics for Windows, version 24 (IBM Corp., Armonk, N.Y. USA) was used for statistical analysis. Python 3.10.6 (Python Software Foundation, Beaverton, USA) and IBM SPSS Modeler trial version for Windows (IBM Corp., Armonk, N.Y. USA) were used to execute machine learning algorithms.
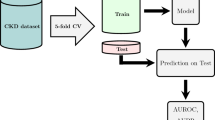
Evaluation of system performance by random forest
Patient groups were randomly divided into training and test sets by the following ratios: 75%:25%, 70%:30%, 60%:40%, and 50%:50%. The model was developed using cases from the training set. On the test set, the same model was applied. The area under the curve (AUC) of the ROC analyses in each set was used to determine the DP of the estimator derived from each model.
Results
During the study period, 1,342 patients underwent ECMO. The mean age was 53.5 years (SD 15.7), and 71.5% were male. It was found that VA mode (83.4%) was used in most cardiovascular cases (80.6%) and VV mode in most of the remaining cases (Additional file 1: Table S2). Table 1 summarizes continuous variables and associated risk scores with Table 2 including categorical metrics. Overall, 62.3% of cases resulted in in-hospital deaths.
Under different partitions, RF and LR showed different discriminatory power (DP) in terms of area under the ROC curve. For partition 2, which used 934 cases for training, the training DP was 1.00 for RF and 0.80 for LR (Additional file 1: Table S3, upper panel, partition 2). The AUC of ROC became far more uniform when the resulting model was applied to the accompanying test set. For RF and LR, it was 0.70 and 0.74, respectively. Additional file 1: Table S3, upper panel, shows the same pattern regardless of the size of the training and test sets. Based on the parsimonious LR model, 11 clinical variables were significantly associated with in-hospital death. These 11 clinical variables include age, ventilation rate (VR), inotropic equivalent (IE), extracorporeal cardiopulmonary resuscitation (ECPR), infection before ECMO, systolic blood pressure (SBP), urine output (U/O), GCS, non-cardiovascular presentation, and bilirubin or creatine kinase levels. As shown in Table 3, a logit transformation of the probability of in-hospital death equals a linear combination of the 11 clinical variables. Both RF and LR models were constructed using parsimonious models with statistically significant variables. In both models, the in-hospital mortality rate showed a favorable DP. For RF, it was 0.73 and for LR, it was 0.76. (Additional file 1: Table S3, lower panel, partition 3).
RF and LR models were used to examine the relative importance of all 55 features. The urine output (in deciliters) on the first day of ECMO institution was ranked as the first critical feature under the RF model (Fig. 1A), and again as the second important feature under the LR model (Fig. 1B). Although the ranking order of the other variables varied between the two models, the first 24 h urine output remained a powerful predictor of in-hospital mortality. In the subsequent survival analysis, this variable was selected as the major classifying feature [17].
Ranking of the clinical features in the random forest (A) and logistic regression (B) models. bh: body height, bw: body weight, bmi: body mass index, NYHA: New York Hear Association functional class, ECMO: extracorporeal membrane oxygenation, Post OP: ECMO placed after an operation, IABP: Intra-aortic balloon pumping, ECPR: extracorporeal cardiopulmonary resuscitation, Infection: infection before ECMO, PE: pulmonary emboli, GCS: Glasgow coma scale, IE: inotropic equivalent, Dialysis: renal replacement therapy before ECMO, LVEF: left ventricular ejection fraction, VR: preset ventilation rate, FiO2: fraction of inspired oxygen, PIP: peak inspiratory pressure, PEEP: peak end-expiratory pressure, MAP: mean airway pressure, BT: body temperature, RR: respiratory rate, HR: heart rate, SBP: systolic blood pressure, DBP: diastolic blood pressure, CVP: central venous pressure, Urine_dl: 24-h urine amount (deciliter), pH: PH value, PaCO2: the partial pressure of carbon dioxide in the arterial blood, PaO2: the partial pressure of oxygen in the arterial blood, PaO2 over FiO2: PaO2/FiO2, HCO3: bicarbonate, Bil: total bilirubin, BUN: blood urine nitrogen, Cre: creatinine, Na: sodium, K: potassium, Lact: lactate, WBC: white blood cell, Hct: hematocrit, Pla: platelet, PT: prothrombin time, CK: creatine kinase, GOT: aspartate aminotransferase, CKMB: creatine kinase MB, Trop: troponin I, Charlson Score: Charlson Comorbidity Index, APACHE: Acute Physiologic Assessment and Chronic Health Evaluation II Scoring System, SOFA: Sequential Organ Failure Assessment Score, LODS: Logistic Organ Dysfunction System, MODS: Multiple Organ Dysfunction, SAVE: Survival after Veno-Arterial ECMO, SAPS3: Simplified Acute Physiology Score III
There were three categories of urine output in the first 24 h: (1) normal (more than 10 dl), decreased (5 dl to 10 dl), and oliguric (less than 5 dl). A comparison of decreased urine group and normal urine group showed that the HR of in-hospital death was 1.005 (p = 0.970) for decreased urine group and 1.446 (p < 0.001) for oliguric group. Therefore, urine output less than 500 ml (i.e., 5 dl) seemed to affect in-hospital mortality. Our study compared patients with oliguria to those without oliguria by combining the first two categories (normal and decreased urine amount). As compared to patients whose initial urine output was greater than 5 dl, the HR for 1 year mortality in patients with oliguria was 1.445 (95% CI 1.265–1.650). Kaplan–Meier curve and log-rank test both revealed a significant difference between the overall mortality of the oliguric group and patients with normal and slightly reduced urine output (p < 0.001) (Fig. 2).
A multi-variable Cox regression model adjusted for other variables was also used to analyze 1 year mortality. As compared with the normal group, the HR for 1 year mortality was 1.016 (p = 0.90, 95% CI 0.798–1.000) for the decreased urine group and 1.295 (p < 0.001, 95% CI 1.116–1.502) for the oliguric group. When the patients were categorized only into oliguric and non-oliguric groups, the former (i.e., urine output < 5 dl) had a HR of 1.291 (p = 0.001, 95% CI 1.121–1.486) compared with the latter (urine output over 5 dl). For each 1 dl increase in urine output, the HR for 1 year mortality dropped by 0.986 (p < 0.001, 95% CI 0.979–0.992).
Discussion
The final analysis of this study included 1342 patients with ECMO support. Compared to conventional approaches, this was by far the largest study of patients on ECMO evaluating prognostic indicators using machine learning algorithms of RF. One of the most influential features in predicting future death, among all anthropometric, hemodynamic, and laboratory variables, was urine output during the first 24 h after ECMO placement.
As part of the training process, RF uses many decision trees (DT) to determine a classifier. In both classification and regression tasks, the DT model is a non-parametric model based on a tree-like graph. A top-to-bottom tree-like structure represents the relationship between the recruiting features and the target variable. The DTs are very sensitive to the training data, so they are error-prone on the test data set. Different parts of the training data set are used for each DT to search for the most “votes,” which are combinations of features and thresholds which will result in the "most effective" separation between the two classes. Due to the fact that the RF algorithm interprets and gets the results from multiple DTs, it can reduce the variance that would result from considering just one DT alone [13]. In addition, we applied a series of solutions to reduce over-fitting in the RF algorithm, and found that the DP was comparable to that derived from LR model. On the other hand, parsimonious models based on select, clinically and statistically significant variables offer the prospect of numerical stability and generalizability, and as demonstrated here, better DP than non-parsimonious models. Thus, including a wider range of variables in the model regardless of their significance decreases the consistency between training and testing. The current analyses illustrate that concentrating only on key variables among all those available can produce a simpler model that also optimizes the DP.
According to both RF and LR models (Fig. 1A, B), urine output was one of the leading predictors, despite other features drifting their ranking scores irregularly. Furthermore, the amount of the 24 h urine output of the first day under ECMO institution determined the clinical outcomes of these critical patients. Oliguric patients were expected to have a poor prognosis. Clinical outcomes after ECMO may be determined by urine output due to global ischemia–reperfusion injury and renal hypoperfusion [18]. According to previous studies, oliguria is one of the earliest signs of insufficient organ perfusion [19]. Acute renal injury was reported in more than half of patients who were resuscitated following cardiopulmonary resuscitation (CPR) [18]. Oliguria could be used as a biomarker of acute kidney injury in critically ill patients [20]. A prior study also showed that in unselected critically ill patients, urine output obtained on ICU entry was associated with hospital mortality [21]. In patients receiving ECMO support, Combes et al. demonstrated that renal failure with a 24 h urine output less than 500 ml was significantly associated with ICU death (OR = 6.52) after ECMO implantation under cardiopulmonary resuscitation [22]. In out-of-hospital cardiac arrest patients receiving ECMO following CPR, Lee et al. found oliguria to be an independent risk factor for 30 day mortality [23]. According to Distelmaier et al. [19] 24 h urine output was a significant variable to predict 30 day and 2 year mortality after cardiovascular surgery. In comparison with previous studies (81, 23, and 205 in the studies by Combes, Lee, and Distelmaier, respectively), ours was by far the largest study and an entirely novel method for examining this issue [19, 22, 23].
In addition, urine output was routinely monitored in the ICU. Thus, urine output is a noninvasive, easily accessible, inexpensive, and ideal parameter for detecting high-risk mortality patients receiving ECMO support in time and intervening before adverse clinical outcomes occur. Low cardiac output (cardiogenic shock), systemic vasodilation (sepsis), and organ hypoperfusion may account for the decreased urine production under ECMO [19]. The condition may also be caused by decreased pump flow, impaired pulsatility, air embolization, hormonal disorders, or a change in platelet concentration [19, 24]. In addition, extracorporeal membranes and mechanical circuits may trigger inflammatory cascades with hypercoagulable states that could adversely affect microcirculation [19]. Due to the possibility that ECMO could trigger an acute inflammatory reaction, there might be capillary leakage and intravascular volume depletion resulting in acute tubular necrosis and oliguria [25].
Limitations
It is possible that information might be lost if missing variables are replaced or if continuous variables are converted to categorical variables. To clarify this issue, we repeated the RF and LR analysis on 200 patients with complete data. The AUC for the in-hospital death remained near 0.75. The final DP did not appear to be altered by the pre-processing.
Conclusions
In this study, 1342 patients undergoing ECMO support were enrolled, and independent predictors of in-hospital death were evaluated. The machine learning algorithm with RF and LR was used to find the most stable feature and robust DP in this prediction task. Our study found that oliguria, defined as urine output less than 500 ml within the first 24 h after ECMO implantation, was strongly associated with in-hospital death and 1 year mortality. To detect high-risk ECMO patients in advance and treat them promptly, urine output was a reliable and easy-to-use parameter.
Availability of data and materials
The data sets generated during and/or analyzed during the current study are not publicly available due to restrictions imposed by the institute and the government. This study's authors declare that all data supporting the conclusions are included in the paper and its supplementary information.
Abbreviations
- APACHE:
-
Acute Physiologic Assessment and Chronic Health Evaluation
- AST:
-
Aspartate transaminase
- AUC:
-
Area under curve
- CI:
-
Confidence interval
- CPR:
-
Cardiopulmonary resuscitation
- DP:
-
Discriminatory power
- ECMO:
-
Extracorporeal membrane oxygenation
- ELSO:
-
Extracorporeal Life Support Organization
- GCS:
-
Glasgow Coma Scale
- GOT:
-
Aspartate transaminase
- HR:
-
Hazard ratio
- IABP:
-
Intra-aortic balloon pump
- ICU:
-
Intensive care unit
- IE:
-
Inotropic equivalent
- LODS:
-
Logistic Organ Dysfunction System
- LR:
-
Logistical regression
- LVEF:
-
Left ventricular ejection fraction
- MODS:
-
Multiple Organ Dysfunction
- NTUH:
-
National Taiwan University Hospital
- NYHA:
-
New York Heart Association
- ROC:
-
Receiver operating characteristic
- SAPS III:
-
Simplified acute physiology score III
- SAVE:
-
Survival After Veno-arterial ECMO
- SOFA:
-
Sequential Organ Failure Assessment
- SVM:
-
Support vector machine
- VA:
-
Veno-arterial
- VV:
-
Veno-venous
References
Chen YS, Lin JW, Yu HY, Ko WJ, Jerng JS, Chang WT, Chen WJ, Huang SC, Chi NH, Wang CH, Chen LC, Tsai PR, Wang SS, Hwang JJ, Lin FY. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008;372:554–61.
Chang CH, Chen HC, Caffrey JL, Hsu J, Lin JW, Lai MS, Chen YS. Survival analysis after extracorporeal membrane oxygenation in critically Ill Adults: a nationwide cohort study. Circulation. 2016;133:2423–33.
Hsu J, Chang CH, Chiang LT, Caffrey JL, Lin JW, Chen YS. Survival analysis of extracorporeal membrane oxygenation in neonatal and pediatric patients-a nationwide cohort study. J Formos Med Assoc. 2019;118:1339–46.
Tseng LJ, Yu HY, Wang CH, Chi NH, Huang SC, Chou HW, Shih HC, Chou NK, Chen YS. Impact of age-adjusted charlson comorbidity on hospital survival and short-term outcome of patients with extracorporeal cardiopulmonary resuscitation. J Clin Med. 2018;7:313.
Bailly DK, Reeder RW, Winder M, Barbaro RP, Pollack MM, Moler FW, Meert KL, Berg RA, Carcillo J, Zuppa AF, Newth C, Berger J, Bell MJ, Dean MJ, Nicholson C, Garcia-Filion P, Wessel D, Heidemann S, Doctor A, Harrison R, Bratton SL. Dalton H, Eunice Kennedy Shriver National Institute of Child H and Human Development Collaborative Pediatric Critical Care Research N Development of the Pediatric Extracorporeal Membrane Oxygenation Prediction Model for Risk-Adjusting Mortality. Pediatr Crit Care Med. 2019;20:426–34.
Hilder M, Herbstreit F, Adamzik M, Beiderlinden M, Burschen M, Peters J, Frey UH. Comparison of mortality prediction models in acute respiratory distress syndrome undergoing extracorporeal membrane oxygenation and development of a novel prediction score: the PREdiction of Survival on ECMO Therapy-Score (PRESET-Score). Crit Care. 2017;21:301.
Schmidt M, Burrell A, Roberts L, Bailey M, Sheldrake J, Rycus PT, Hodgson C, Scheinkestel C, Cooper DJ, Thiagarajan RR, Brodie D, Pellegrino V, Pilcher D. Predicting survival after ECMO for refractory cardiogenic shock: the survival after veno-arterial-ECMO (SAVE)-score. Eur Heart J. 2015;36:2246–56.
Becher PM, Twerenbold R, Schrage B, Schmack B, Sinning CR, Fluschnik N, Schwarzl M, Waldeyer C, Seiffert M, Clemmensen P, Neumann JT, Bernhardt AM, Zeymer U, Thiele H, Reichenspurner H, Blankenberg S, Westermann D. Risk prediction of in-hospital mortality in patients with venoarterial extracorporeal membrane oxygenation for cardiopulmonary support: The ECMO-ACCEPTS score. J Crit Care. 2020;56:100–5.
Lin SY, Hsieh MH, Lin CL, Hsieh MJ, Hsu WH, Lin CC, Hsu CY, Kao CH. Artificial intelligence prediction model for the cost and mortality of renal replacement therapy in aged and super-aged populations in Taiwan. J Clin Med. 2019;8:995.
Siga MM, Ducher M, Florens N, Roth H, Mahloul N, Fouque D, Fauvel JP. Prediction of all-cause mortality in haemodialysis patients using a Bayesian network. Nephrol Dial Transplant. 2020;35(8):1420–5.
Matsuo K, Aihara H, Nakai T, Morishita A, Tohma Y, Kohmura E. Machine learning to predict in-hospital morbidity and mortality after traumatic brain injury. J Neurotrauma. 2020;37:202–10.
Keuning BE, Kaufmann T, Wiersema R, Granholm A, Pettila V, Moller MH, Christiansen CF, Castela Forte J, Snieder H, Keus F, Pleijhuis RG. van der Horst ICC and consortium H Mortality prediction models in the adult critically ill: A scoping review. Acta Anaesthesiol Scand. 2020;64:424–42.
Uddin S, Khan A, Hossain ME, Moni MA. Comparing different supervised machine learning algorithms for disease prediction. BMC Med Inform Decis Mak. 2019;19:281.
Chen YS, Ko WJ, Chi NH, Wu IH, Huang SC, Chen RJ, Chou NK, Hsu RB, Lin FY, Wang SS, Chu SH, Yu HY. Risk factor screening scale to optimize treatment for potential heart transplant candidates under extracorporeal membrane oxygenation. Am J Transplant. 2004;4:1818–25.
Lin YH, Huang HC, Chang YC, Lin C, Lo MT, Liu LY, Tsai PR, Chen YS, Ko WJ, Ho YL, Chen MF, Peng CK, Buchman TG. Multi-scale symbolic entropy analysis provides prognostic prediction in patients receiving extracorporeal life support. Crit Care. 2014;18:548.
Nembrini S, Konig IR, Wright MN. The revival of the Gini importance? Bioinformatics. 2018;34:3711–8.
Singh SR, Murthy HA, Gonsalves TA. Feature selection for text classification based on gini coefficient of inequality. JMLR. 2010;10:76–85.
D’Arrigo S, Cacciola S, Dennis M, Jung C, Kagawa E, Antonelli M, Sandroni C. Predictors of favourable outcome after in-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation. 2017;121:62–70.
Distelmaier K, Roth C, Binder C, Schrutka L, Schreiber C, Hoffelner F, Heinz G, Lang IM, Maurer G, Koinig H, Steinlechner B, Niessner A, Goliasch G. Urinary output predicts survival in patients undergoing extracorporeal membrane oxygenation following cardiovascular surgery. Crit Care Med. 2016;44:531–8.
Prowle JR, Liu YL, Licari E, Bagshaw SM, Egi M, Haase M, Haase-Fielitz A, Kellum JA, Cruz D, Ronco C, Tsutsui K, Uchino S, Bellomo R. Oliguria as predictive biomarker of acute kidney injury in critically ill patients. Crit Care. 2011;15:R172.
Zhang Z, Xu X, Ni H, Deng H. Urine output on ICU entry is associated with hospital mortality in unselected critically ill patients. J Nephrol. 2014;27:65–71.
Combes A, Leprince P, Luyt CE, Bonnet N, Trouillet JL, Léger P, Pavie A, Chastre J. Outcomes and long-term quality-of-life of patients supported by extracorporeal membrane oxygenation for refractory cardiogenic shock. Crit Care Med. 2008;36:1404–11.
Lee JJ, Han SJ, Kim HS, Hong KS, Choi HH, Park KT, Seo JY, Lee TH, Kim HC, Kim S, Lee SH, Hwang SM, Ha SO. Out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal membrane oxygenation: focus on survival rate and neurologic outcome. Scand J Trauma Resusc Emerg Med. 2016;24:74.
Ratnani I, Tuazon D, Zainab A, Uddin F. The role and impact of extracorporeal membrane oxygenation in critical care. Methodist Debakey Cardiovasc J. 2018;14:110–9.
Hsiao CC, Chang CH, Fan PC, Ho HT, Jenq CC, Kao KC, Chiu LC, Lee SY, Hsu HH, Tian YC, Hung CC, Fang JT, Yang CW, Tsai FC, Chen YC. Prognosis of patients with acute respiratory distress syndrome on extracorporeal membrane oxygenation: the impact of urine output on mortality. Ann Thorac Surg. 2014;97:1939–44.
Acknowledgements
The senior author, Jou-Wei Lin, would like to pay tribute to Mrs. Yuri Lin-Wang for her unwavering love, support, and encouragement in every aspect of life, including this academic pursuit.
Funding
The study was funded by grants from the Taiwan Ministry of Science and Technology (MOST 110-2221-E-002-161-), National Science and Technology Council (NSTC 111-2221-E-002-115-), and National Taiwan University Hospital Yunlin Branch (YLH110.A003). The study design, data collection and analysis, decision to publish, or preparation of the manuscript were not influenced by any funding bodies.
Author information
Authors and Affiliations
Contributions
The study concept and design were carried out by CSN, LJW, HJ, and HNZ. HJ, YHY, and CYS collected data. WJH, LJW, CHM, and HNZ analyzed and interpreted the data. CSN, WJH, LJW, and CJL drafted the manuscript. CSN, HJ, CHM, CJL, and CCH revised and edited the manuscript. HNZ, CHM, and LJW performed statistical analyses. The study was conducted by HNZ, HJ, and LJW. JWL is the senior author who is responsible for leading the research project, securing funding, and providing overall guidance to the research team.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The collection and review of patient information was approved by the Institutional Review Board of National Taiwan University Hospital (#201002034R, 2010/02, ECMO data analysis study).
Consent for publication
All the authors have read and approved the final manuscript and agreed to transfer the copyright ownership in the event of acceptance. We also certify that our work is original. This work has not been published and is not under consideration for publication elsewhere.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Variables and Definitions. Table S2. ECMO indications classified into three categories: cardiovascular, respiratory, and others. The numbers of VA and VV ECMO in each category were shown, and specific indications were reported. Table S3. Discriminatory power determined by the area under curve (AUC) in receiver operating characteristic curve (ROC) analyses using random forest and logistic regression model. Upper panel: non-parsimonious model when all variables were used. Lower panel: parsimonious model when only selected variables that were statistically significant were used. Figure S1. ROC curves for parsimonious models using random forest (Panel A) and logistic regression (Panel B) in the training set (70%, left column) and the test set (30%, right column).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chang, SN., Hu, NZ., Wu, JH. et al. Urine output as one of the most important features in differentiating in-hospital death among patients receiving extracorporeal membrane oxygenation: a random forest approach. Eur J Med Res 28, 347 (2023). https://doi.org/10.1186/s40001-023-01294-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01294-1