Abstract
Background
Prolyl 4-hydroxylase subunit beta (P4HB) has been reported as a suppressor in ferroptosis. However, no known empirical research has focused on exploring relationships between P4HB and prostate cancer (PCa). In this research, we initially examine the function of P4HB in PCa by thorough analysis of numerous databases and proliferation experiment.
Methods
We analyzed the correlations of P4HB expression with prognosis, clinical features, mutation genes, tumor heterogeneity, stemness, tumor immune microenvironment and PCa cells using multiple databases and in vitro experiment with R 3.6.3 software and its suitable packages.
Results
P4HB was significantly upregulated in tumor tissues compared to normal tissues and was closely related to biochemical recurrence-free survival. In terms of clinical correlations, we found that higher P4HB expression was significantly related to older age, higher Gleason score, advanced T stage and residual tumor. Surprisingly, P4HB had highly diagnostic accuracy of radiotherapy resistance (AUC 0.938). TGF beta signaling pathway and dorso ventral axis formation were upregulated in the group of low-expression P4HB. For tumor stemness, P4HB expression was positively related to EREG.EXPss and RNAss, but was negatively associated with ENHss and DNAss with statistical significance. For tumor heterogeneity, P4HB expression was positively related to MATH, but was negatively associated with tumor ploidy and microsatellite instability. For the overall assessment of TME, we observed that P4HB expression was negatively associated with all parameters, including B cells, CD4+ T cells, CD8+ T cells, neutrophils, macrophages, dendritic cells, stromal score, immune score and ESTIMATE score. Spearman analysis showed that P4HB expression was negatively related to TIDE score with statistical significance. In vitro experiment, RT-qPCR and western blot showed that three siRNAs of P4HB were effective on the knockdown of P4HB expression. Furthermore, we observed that the downregulation of P4HB had significant influence on the cell proliferation of six PCa cell lines, including LNCap, C4-2, C4-2B, PC3, DU145 and 22RV1 cells.
Conclusions
In this study, we found that P4HB might serve as a prognostic biomarker and predict radiotherapy resistance for PCa patients. Downregulation of P4HB expression could inhibit the cell proliferation of PCa cells.
Similar content being viewed by others
Introduction
In 2022, new cancer cases are projected to total 4,820,000 and 2,370,000 in China and the USA, respectively [1]. Prostate cancer (PCa) serves as the third and sixth most prevailing malignancy among newly diagnosed cases in China and the USA, respectively [1,2,3]. The incidence, mortality, and disability-adjusted life years for PCa were also greater in areas and nations with higher sociodemographic indices [4]. Inflammation and age are risk factors of many diseases, such as macular degeneration [5, 6], cardiovascular diseases [7, 8], periodontitis [9], neurological disorders [10], and human cancer [11,12,13,14,15]. Globally, aging is posing a severe threat to human health [16]. The vast majority of PCa cases occurred in elderly people and it is anticipated that this trend will worsen as the world’s population ages [4, 17,18,19,20,21,22,23,24]. There is growing recognition that genetic variability in PCa encompasses many tumor forms with unique biologic characteristics and clinical behaviors [25]. The primary methods for treating patients with localized PCa include radical prostatectomy or radiation, while biochemical recurrence (BCR) is unavoidable for patients after radical prostatectomy (27–53%) or radiotherapy (10–70%), respectively [26,27,28]. Eight years is the typical period from BCR to metastasis, while 5 years is the median time from metastatic to death [19, 27, 28]. In addition, treatment resistance is fast developing more deadly and malignant neuroendocrine PCa, and the prognosis for such patients is quite dismal with a survival time of less than 1 year [29]. By integrating genetic and clinical data, the advancement of sequencing technology, particularly the completion of the Cancer Genome Atlas (TCGA), offers a feasible and effective method to screen such patients.
The role of ferroptosis has received increased attention across a number of diseases, since it was proposed by Prof. Brent R.Stockwell et al. in 2012 [30]. It is a novel of nonapoptotic cell death and is controlled by iron pool, lipid metabolism and antioxidant metabolism [31,32,33,34]. In 2020, Dr. Nan Zhou and Jinku Bao proclaimed an excellent FerrDb data set, which took 784 ferroptosis studies from the PubMed database and extracted ferroptosis regulators and markers and relevant diseases [35]. Using the TCGA and FerrDb databases [35], prolyl 4-hydroxylase subunit beta (P4HB) and prostaglandin–endoperoxide synthase 2 (PTGS2) were detected to be potential biomarker for PCa patients from the perspective of ferroptosis, where research to date has not yet determined the impact of P4HB on PCa patients. Herein, through a thorough review of numerous databases and an in vitro experiment, we primarily investigated the function of P4HB in PCa.
Methods
Bioinformatic analysis
We obtained the PCa data of TCGA database and gene expression omnibus (GEO) data sets (GSE46602 [36], GSE32571 [37] and GSE62872 [38]) from our previous study [19]. From the FerrDb database, 474 genes relevant to human ferroptosis were taken [35]. llogFCl 0.5 and p.adj 0.05 were used to determine the differentially expressed genes (DEGs) between 498 tumour and 52 normal samples in the TCCG database. The BCR-free survival P value was constrained to less than 0.05. By combining DEGs, prognosis-related genes, and ferroptosis-related genes, P4HB and PTGS2 were discovered. GEO data sets [36,37,38] were utilized to confirm the differential expression of P4HB and PTGS2. We selected P4HB for further research due to its less information in PCa. The pan-cancer distinct expression of P4HB between cancer and normal samples was evaluated through the TIMER database [39]. In addition, we again confirmed P4HB expression between samples of cancer and normal using UALCAN [40] and GEPIA [41]. We then conducted an analysis of the clinical P4HB levels and created a nomogram. Using GSE53902 [42], We evaluated P4HB's diagnostic effectiveness with regard to radiation resistance. Mutation data of PCa patients were downloaded from GDC (https://portal.gdc.cancer.gov/) and were visualized by MuTect2 software and R package “maftools (version 2.2.10)” [43]. Using the median value of P4HB expression, we divided the PCa patients into groups based on the expression levels. Analysis was done on the variations about gene mutation frequency between these two groups. We used the human protein atlas (HPA) to examine P4HB's potential intracellular localization [44, 45]. We also assessed the predicted functional partners of P4HB using multiple databases, including HPA, GeneMANIA [46] and STRING [47].
In terms of the functional analysis, We used the R program "gene set variation analysis (GSVA)" [48] and “c2.cp.v7.4.symbols.gmt” subset from the molecular signature database [49] to determine the enrichment scores of each sample's relevant molecular processes and pathways. The set contained between 5 and 5000 genes. The "wilcox.test" tool was then applied to compare each pathway between P4HB expression levels that were high and low. The fold change was 1.5, and statistical significance was defined as p. adj. 0.01 and false discovery rate 0.01. Using the Spearman analysis, the overall tumor immune microenvironment (TME) and immune cells were evaluated by ESTIMATE and TIMER algorithms [50,51,52]. The TISIDB database examined the interactions of P4HB with tumor-infiltrating cells, immunoinhibitors, and immunostimulators [53]. Poor effectiveness of immune checkpoint blockade (ICB) is associated with high tumor immune dysfunction and exclusion (TIDE) score. We used the TIDE algorithm [54] to estimate the TIDE score and assess the relationship of P4HB with TIDE score with Spearman analysis.
The correlation between P4HB and tumor heterogeneity and stemness related indexes was analyzed and the specific methods could be seen from the previous studies [55,56,57,58,59,60,61,62]. GSCALite was used to examine the relationship between P4HB and medication sensitivity in pan cancer [63], which integrated the data of the cancer therapeutics response portal and genomics of drug sensitivity in cancer.
In vitro experiment
The acquisition of PCa cell lines and their culture were described from our previous study [64]. The culture condition of 22RV1 cell is similar to common PCa cells, such as DU145 cells. In addition, RT-qPCR methods was also described in the previous study [64]. siRNA was obtained by HIPPOBIO (www.hippobiotec.com). P4HB si-1sense: 5′-UGCUGUUCUUGCCCAAGAGUGdTdT-3′; P4HB si-1 antisense: 5′-CACUCUUGGGCAAGAACAGCAdTdT-3′. P4HB si-2 sense: 5′-AGGUGAAAUCAAGACUCACAUdTdT-3′; P4HB si-2 antisense: 5′-AUGUGAGUCUUGAUUUCACCUdTdT-3′; P4HB si-3 sense: 5′-GUGUGGUCACUGCAAACAGUUdTdT-3′; P4HB si-3 antisense: 5′-AACUGUUUGCAGUGACCACACdTdT-3′. An internal control was implemented using glyceraldehyde-3-phosphate dehydrogenase (GAPDH). GAPDH: 5′-CTGGGCTACACTGAGCACC-3′ (forward) and 5′-TCC AAGTGGTCGTTGAGGGCAATG-3′ (reverse); P4HB: 5′-GGTGCTGCGGAAAAGCAAC-3′ (forward) and 5′-ACCTGATCTCGGAACCTTCTG-3′ (reverse). The siRNAs of P4HB that were most efficient were found using RT-qPCR. Cells were collected and lysed in RIPA Lysis Buffer containing freshly added PMSF and a protease inhibitor cocktail for the western blot. Using a BSA kit, protein concentration was discovered. A 30 ug protein sample was run via an SDS–PAGE gel. Gel electrophoresis was used to separate the proteins, which were then transferred to a polyvinylidene difluoride membrane. The membranes were blocked for 2 h at room temperature with 5% nonfat dry skim milk before being incubated with matching primary antibodies overnight at 4 ℃. The main antibodies are anti-P4HB (1:1000, ab2792 Abcam, USA) and β-Actin (1:10,000, 81115-1-RR, Proteintech, China). The membranes were detected using horseradish peroxidase-conjugated secondary antibodies (1:3000, SA00001-1, SA00001-2, Proteintech, China) followed by exposure to enhanced chemiluminescence substrate (Millipore, WBKLS0500, USA). Six PCa cell lines were transfected with P4HB siRNAs, and the impact of P4HB on their ability to proliferate was examined using the cell counting kit-8 (CCK8) assay at 24 h, 48 h, and 72 h. The study's flowchart is shown in Fig. 1.
Statistical analysis
For statistical analysis, R 3.6.3 software and its appropriate packages were utilised. Through the use of log-rank tests and Kaplan–Meier curves, the survival analysis was carried out. Based on the findings of the Cox regression studies, a nomogram was created, and the nomogram model was assessed using the Harrell's concordance index (C-index) and decision curve analysis (DCA) curve. The aforementioned statistical tests are all two-sided. Statistical significance was defined as a P value of 0.05. The following symbols were noteworthy: ns, p ≥ 0.05; *p < 0.05; **p < 0.01; ***p < 0.001.
Results
Bioinformatic analysis
P4HB and PTGS2 were discovered as a result of the intersection of DEGs, prognosis-related genes, and ferroptosis-related genes (Fig. 2a). P4HB was upregulated in the TCGA database (Fig. 2b) and was validated in the GEO data sets [14,15,16] (Fig. 2c). With statistical significance, P4HB was differently expressed in a variety of malignancies, including PCa (Fig. 2d). In comparison to normal samples, UALCAN [18] and GEPIA [19] were used to confirm that tumor samples had increased P4HB expression (Fig. 2e, f). In the GEPIA database [19], Based on the median value of P4HB, PCa patients were split into two groups, and those with lower expression of P4HB had significantly shorter disease-free life than those with higher expression of P4HB (Fig. 2g). In addition, we found that P4HB was strongly linked with BCR-free survival in our analysis (Fig. 3a). In the subgroup survival study, higher P4HB expression was associated with a reduced probability of BCR in terms of N0 stage, White population, residual tumor, age < 60, and overlapping or multiple zones than lower P4HB expression (Fig. 3b–f). In addition, we created a nomogram incorporating P4HB and clinical characteristics to forecast the likelihood of BCR for PCa patients (Fig. 3g). DCA curve indicated that this might be acceptable (C-index: 0.718; Fig. 3h). Surprisingly, P4HB demonstrated a high level of diagnostic accuracy about radiation resistance (AUC: 0.938; Fig. 3i). Clinical correlations revealed that older age, a higher Gleason score, an advanced T stage, and residual tumour were all strongly correlated with increased P4HB expression (Table 1).
Process of screening P4HB. a Upset plot shwnig the intersection of DEGs, prognosis-related genes and ferroptosis-related genes; b volcano plot showing the expression of P4HB and PTGS2 between tumor and normal samples in the TCGA database; c volcano plot showing the expression of P4HB and PTGS2 between tumor and normal samples in the GEO data sets; d bar graph showing the expression of P4HB between tumor and normal samples at pan-cancer level; e bar graph showing P4HB expression between tumor and normal samples in the UALCAN database; f bar graph showing P4HB expression between tumor and normal samples in the GEPIA database; g Kaplan–Meier curve showing the survival differences of high and low P4HB expression using GEPIA database. DEGs differentially expressed genes, TCGA the cancer genome atlas, GEO gene expression omnibus
Correlations of P4HB with prognosis and radiotherapy resistance. a Kaplan–Meier curve showing the survival differences of high and low P4HB expression in the TCGA database; b Kaplan–Meier curve showing the survival differences of high and low P4HB expression in patients with N0 stage; c Kaplan–Meier curve showing the survival differences of high and low P4HB expression in White patients; d Kaplan–Meier curve showing the survival differences of high and low P4HB expression in patients with residual tumor; e Kaplan–Meier curve showing the survival differences of high and low P4HB expression in patients with age < 60 years; f Kaplan–Meier curve showing the survival differences of high and low P4HB expression in patients with overlapping or multiple zones; g nomogram plot integrating P4HB expression and clinical featurs; h decision curve analysis curve; i ROC curve showing the diagnostic ability of P4HB in radiotherapy resistance. TCGA the cancer genome atlas, ROC receiver operating characteristic curve
Missense mutations were found in 0.2% of PCa patients, according to the mutation landscape (Fig. 4a). We divided the PCa patients into two groups according to the median value of P4HB. OBSCN, FLG, AGCA13, NALCN, CNTN6, DGKI, and DYNC1HI were significantly differentially expressed between the two groups among the top 20 altered genes, while TP53 was the most frequently mutant gene in PCa (Fig. 4b). In the HPA database [22, 23], P4HB was found in the endoplasmic reticulum (ER) and was implicated in the metabolism of arginine, proline, insulin, and glutathione (Fig. 4c, d). P4HB was predicted to be potential partner of MTTP, P4HA2 and GPX7 using the GeneMANIA [24] (Fig. 4e) and STRING databases [25] (Fig. 4f). Glyoxylate and dicarboxylate metabolism, proteasome, oxidative phosphorylation, protein export, N glycan biosynthesis, glycosylphosphatidylinositol anchor biosynthesis, amino sugar and nucleotide sugar metabolism and terpenoid backbone biosynthesis were upregulated in the group of high-expression P4HB, while TGF beta signaling pathway and dorso ventral axis formation were upregulated in the group of low-expression P4HB (Fig. 4g).
Mutation genes, location, predicted partners, functional pathway, tumor immune microenvironment, tumor heterogeneity and stemness of P4HB. a Mutation landscape of PCa patients in the TCGA database; b mutation genes between high and low P4HB expression; c predicted sublocation of P4HB; d reported pathway of P4HB in the HPA database; e predicted interaction genes of P4HB using GeneMANIA database; f predicted functional partners of P4HB using STRING database; g functional pathways between high and low P4HB expression using GSVA methods; h bubble diagram showing the correlations of P4HB expression with tumor heterogeneity and stemness; i bubble diagram showing the correlations of P4HB expression with tumor microenvironment scores; j heatmap showing the relationship between P4HB expression and tumor-infiltrating cells; k scatter diagram showing the relationship between P4HB expression and TIDE score; l heatmap showing the relationship between P4HB expression and immunostimulators; m heatmap showing the relationship between P4HB expression and immunoinhibitors; n scatter diagram showing the relationship between P4HB expression and PVRL2. TIDE tumor immune dysfunction and exclusion
P4HB expression had statistically significant positive relationships with EREG.EXPss and RNAss, but negative relationships with ENHss and DNAss (Fig. 4h). For tumor heterogeneity, P4HB expression was positively related to MATH, but was negatively associated with tumor ploidy and microsatellite instability. However, the correlation values of P4HB with the above indicators were smaller than 0.3, which indicated that the correlation strength was low. For the overall assessment of TME, we observed that P4HB expression was negatively associated with all parameters, including macrophages, dendritic cells, B cells, CD8+ T cells, CD4+ T cells, neutrophils, stromal score, immunological score and ESTIMATE score (Fig. 4i), which was confirmed by the TISIDB database [31] (Fig. 4j). Spearman analysis showed that P4HB expression was negatively related to TIDE score with statistical significance (Fig. 4k). Similar results were observed in terms of immunostimulators (Fig. 4l) and immunoinhibitors (Fig. 4m) in the TISIDB database [31]. Among these indicators, it was striking that P4HB expression showed significant relationship with PVRL2 expression with good correlation (r = 0.659, p < 0.001; Fig. 4n).
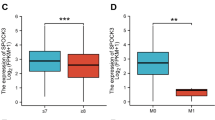
Owing to the opposite results of between prognostic analysis and differential expression and clinical correlations, we detected the impact of P4HB on the cell proliferation of PCa cell lines. RT-qPCR and western blot showed that three siRNAs of P4HB were effective on the knockdown of P4HB expression (Fig. 5a, b). Furthermore, we observed that the downregulation of P4HB had significant influence on the cell proliferation of six PCa cell lines, including LNCap, C4-2, C4-2B, PC3, DU145 and 22RV1 cells (Fig. 5c–h).
Effect of P4HB on PCa cell proliferation. a RT-qPCR results of P4HB siRNAs; b western blot results of P4HB siRNAs using C4-2B and DU145 cells; c effect of P4HB siRNAs on LNCap using CCK8 assay; d effect of P4HB siRNAs on C4-2 using CCK8 assay; e effect of P4HB siRNAs on C4-2B using CCK8 assay; f effect of P4HB siRNAs on PC3 using CCK8 assay; g effect of P4HB siRNAs on DU145 using CCK8 assay; h effect of P4HB siRNAs on 22RV1 using CCK8 assay. RT-qPCR real-time quantitative polymerase chain reaction
Discussion
Similar to apoptosis, ferroptosis is a form of programmed cell death brought on by the fatal accumulation of iron-dependent lipid peroxides [65,66,67,68,69]. The ferroptosis-related enzyme GSH peroxidase 4 (GPX4) is the only one that can use glutathione (GSH) as an electron donor to remove harmful lipids from biofilms. Glutathione (GSH) can reduce lipid peroxidation to prevent membrane damage [70]. The basic mechanisms of ferroptosis include GSH depletion and decreased GPX4 activity. Another recently found GSH-independent ferroptosis pathway includes Q10 (CoQ10) and CoQ oxidoreductase ferroptosis-suppressing protein 1 (FSP1) [71, 72]. Some ferroptosis inducers, such as erastin and sorafenib, work by inactivating GPX4, while the tiny molecule FIN56 works by depleting GPX4 protein and CoQ10 at the same time [73, 74]. Even tumor cells that have demonstrated resistance to apoptosis are innately susceptible to ferroptosis. For instance, PCa is reliant on mitochondrial metabolism early on and exhibits altered fatty acid production and oxidation pathways, which raises the possibility that ferroptosis may be involved in the carcinogenesis of this disease [27].
The most prevalent cancer in the western world is unquestionably PCa [75]. It is a type of cancer liable to ferroptosis induction, e.g., enzalutamide therapy results in GPX4 inhibition and consequent ferroptosis sensitization [76, 77]. The ferroptosis inducers erastin or RSL3 markedly decreased prostate cancer cell growth and migration in vitro and markedly slowed tumor growth of treatment-resistant prostate cancer in vivo, indicating that this could be used in conjunction with conventional second-generation antiandrogens for PCa treatment [77]. Furthermore, even in PCa that is resistant to castration, PCa cells respond to the ferroptosis inducer erastin [77]. Recent research has revealed that the ferroptosis inducer erastin can both in vitro and in vivo down-regulate the androgen receptor (AR) and its splice variants, which are essential for the development of castration-resistant PCa [78]. Future prospects for PCa therapy may involve combining several ferroptosis inducers with conventional antineoplastic or antiandrogen medications. For instance, the combination of docetaxel and erastin improves the inhibition of castration-resistant PCa by inhibiting the expression of both full-length and splice variants in cancer cells, and the combination of an isothiocyanate-containing hybrid AR antagonist and the GSH synthesis inhibitor buthionine sulfoximine results in ferroptosis and lowers AR activity [78]. Ferroptosis has considerable prospects in PCa tumorigenesis [79] and treatment.
The prolyl 4-hydroxylase beta subunit is encoded by the gene P4HB, which is located at 17q25.3. Preprocollagen's prolyl residues are hydroxylated by P4HB, and this process has the primary effect of preventing the aggregation of improperly folded proteins. For the protein-folding catalyst, bacitracin is regarded as either a selective or nonspecific P4HB inhibitor [80]. P4HB has been reported to be associated with a variety of cancer and oncological outcomes, like bladder cancer from our previous study [81]. Direct deletion of this gene makes cells more susceptible to known ferroptosis inducers, while the P4HB inhibitor PACMA31 directly promotes ferroptosis [82]. The intermediate regulators SLC7A11 and GSH work in concert with a variety of upstream factors, such as many lncRNAs and circRNAs, to control ferroptosis. The expression of circP4HB in lung adenocarcinoma (LUAD) was found to be elevated both in vivo and in vitro, and it was shown to prevent ferroptosis caused by erastin through regulating miR-1184/SLC7A11-mediated GSH production, which promoted tumor growth [83]. In addition, in LUAD cells with significant P4BH expression, the enrichment and positive expression of the GSH metabolic pathway were clearly seen [83]. Our study is the first to describe the predictive role of P4HB in PCa prognosis and speculate its possible mechanism related to ferroptosis. Similar to LUAD, the results of our in vitro experiments showed that P4HB downregulation of multiple PCa cell lines significantly reduced proliferation, and the P4HB high-expression group had significantly higher Gleason score and more advanced T stage.
The majority of protein synthesis takes place in the ER, and the P4HB protein serves as an ER chaperone to ensure that newly generated proteins are folded correctly [84, 85]. The chemicals that influence ferroptosis by altering lipid peroxidation are predominantly located in the ER, which is the most significant organelle for ferroptosis [86]. One of the fundamentals of prostate carcinogenesis, ER stress is a rapidly reproducing cell's adaptive defensive response that frequently manifests in tumor cells [87, 88]. Ferroptosis was discovered to be brought on by the activation of the ER stress signaling system [89, 90]. In these conditions, the requirement for protein synthesis rises, activating the unfolded protein response (UPR) [91, 92]. In PCa, it was discovered that the UPR is androgen-sensitive, and AR signaling controls enhanced protein folding, mRNA degradation, and protein translation, boosting PCa cell survival by blocking the PERK-eIF2a axis [93,94,95]. During endoplasmic reticulum stress, the chaperones are primarily in charge of facilitating protein folding and removing abnormal proteins [96]. While some chaperone proteins have been discovered to be involved in cancer and drug resistance, ER chaperones are currently not thought to be confined to functions required for protein folding, assembly, and membrane protein transport [97, 98]. Fonseca et al. found that P4HB and other protein disulfide isomerases are immunogenic, and the gene products they produce could be used as therapeutic monoclonal antibody targets [99].
We also discovered that the high-expressing P4HB group had an up-regulated level of energy metabolism, including oxidative phosphorylation, as well as protein production. According to the Warburg effect, it is well known that maintaining tumor metabolism necessitates greater energy supply and metabolic activity and that tumor cells significantly rely on antioxidant systems. For instance, oxidative phosphorylation disruption can raise unstable iron pools and increase the risk of ferroptosis in cells by preventing mitochondrial metabolism [100]. This implies that the main gene of P4HB can be used to particularly increase the ferroptosis sensitivity of malignancies by blocking metabolism.
We discovered through functional analysis that P4HB, which was found in the ER, was involved in GSH metabolism. GSH is a crucial cofactor for the enzyme GPX4 in the conversion of lipid hydroperoxides to lipid alcohols, which reduces lipid peroxidation and prevents ferroptosis [101, 102]. We hypothesized that P4HB might control tumor cell ferroptosis by contributing to GSH depletion. Fibroblasts has been reported to be important to many diseases, including cancers [8, 103,104,105,106,107,108]. Our previous study also observed that P4HB was related to cancer-related fibroblasts [62]. Apart from this kind of stromal cell, we discovered that P4HB had a negative correlation with a range of immune cells in the tumor microenvironment, such as T cells, B cells, and macrophages. This finding inferred that P4HB functions as a pro-oncogene with immunosuppressive, pro-angiogenic, and anti-inflammatory effects, creating a stromal microenvironment that is favorable for the growth and transformation of prostate epithelial cells, resulting in PCa [109]. However, the causal relationship between immune cells and ferroptosis remains questionable. For instance, interferon gamma (IFN)-mediated ferroptosis of tumor cells is one way that CD8+ T lymphocytes contribute to the suppression of malignancies [110]. T cells have the ability to internalize P4HB, which improves their activation, proliferation, adhesion, and migration [111]. In addition, the novel PDI inhibitor E64FC26 was discovered to alter T cell metabolism and decrease global P4HB expression in healthy T cells, which improves immune responses against tumors [112]. Notably, we found that the P4HB group with low expression triggered the TGF signaling pathway. Inhibiting the TGF signaling pathway enhances the immune response in the TME, which is followed by the polarization of M1-type macrophages, which triggers the Fenton response and the consequent ferroptosis of tumor cells. This provides a possible course of action for the therapy of cancers [113]. PCa patients may benefit from this TGF-β receptor inhibitor and modified nanoparticle breast cancer medication (SB431542) [114]. Thus, there is reason to believe that the immune microenvironment's crosstalk may contribute to the up-regulation of the ferroptosis-related gene P4HB in malignancies.
In addition, even though we were able to demonstrate that si-P4HB has an anti-proliferative effect on six PCa cells, more researches are required to show and understand the role of P4HB in PCa, like overexpressing P4HB in PCa cells as well as in vivo animal studies and so forth. Further research is needed based on our current findings. According to our research, P4HB is a new oncogene connected to the development of prostate tumors. ER stress and modifications to the metabolic route may be related to the process. We hypothesized that one of the anti-cancer targets could be achieved by inhibiting the pro-oncogene P4HB, such as using the P4HB inhibitor bacitracin. This hypothesis has to be verified by subsequent in vitro and in vivo testing. The mechanism of P4HB and ferroptosis in PCa must be identified, as well as if ferroptosis-inducing drugs may be utilized in conjunction with immune checkpoint inhibitors, or whether using ferroptosis to activate immune cells or target metabolic patterns to trigger ferroptosis can help treat PCa.
Conclusions
In this study, we found that P4HB might serve as a prognostic biomarker and predict radiotherapy resistance for PCa patients. Downregulation of P4HB expression could inhibit the cell proliferation of PCa cells.
Availability of data and materials
The results showed here are in whole or part based upon data generated by the TCGA Research Network: https://www.cancer.gov/tcga.
References
Xia C, Dong X, Li H, Cao M, Sun D, He S, Yang F, Yan X, Zhang S, Li N, Chen W. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (Engl). 2022;135(5):584–90.
Yang Y. Comments on National guidelines for diagnosis and treatment of prostate cancer 2022 in China (English version). Chin J Cancer Res. 2022;34(5):456–7.
Health Commission Of The People’s Republic Of China N. National guidelines for diagnosis and treatment of prostate cancer 2022 in China (English version). Chin J Cancer Res. 2022;34(3):270–88.
Zi H, He SH, Leng XY, Xu XF, Huang Q, Weng H, Zhu C, Li LY, Gu JM, Li XH, Ming DJ, Li XD, Yuan S, et al. Global, regional, and national burden of kidney, bladder, and prostate cancers and their attributable risk factors, 1990–2019. Mil Med Res. 2021;8(1):60.
Deng Y, Qiao L, Du M, Qu C, Wan L, Li J, Huang L. Age-related macular degeneration: epidemiology, genetics, pathophysiology, diagnosis, and targeted therapy. Genes Dis. 2022;9(1):62–79.
Li X, Ma B, Zhang W, Song Z, Zhang X, Liao M, Li X, Zhao X, Du M, Yu J, He S, Yan H. The essential role of N6-methyladenosine RNA methylation in complex eye diseases. Genes Dis. 2023;10(2):505–20.
Zhang X, Zhang Y, Sun A, Ge J. The effects of nicotinamide adenine dinucleotide in cardiovascular diseases: molecular mechanisms, roles and therapeutic potential. Genes Dis. 2022;9(4):959–72.
Hu C, Zhang X, Teng T, Ma ZG, Tang QZ. Cellular senescence in cardiovascular diseases: a systematic review. Aging Dis. 2022;13(1):103–28.
Elsayed R, Elashiry M, Liu Y, Morandini AC, El-Awady A, Elashiry MM, Hamrick M, Cutler CW. Microbially-induced exosomes from dendritic cells promote paracrine immune senescence: novel mechanism of bone degenerative disease in mice. Aging Dis. 2023;14(1):136–51.
Balakrishnan R, Azam S, Kim IS, Choi DK. Neuroprotective effects of black pepper and its bioactive compounds in age-related neurological disorders. Aging Dis. 2023;14(3):750–77.
Ruiz E, Kandil E, Alhassan S, Toraih E, Errami Y, Elmageed ZYA, Zerfaoui M. An integrative multi-omics analysis of the molecular links between aging and aggressiveness in thyroid cancers. Aging Dis. 2023;14(3):992–1012.
Shen W, He J, Hou T, Si J, Chen S. Common pathogenetic mechanisms underlying aging and tumor and means of interventions. Aging Dis. 2022;13(4):1063–91.
Schwartz AG. Dehydroepiandrosterone, cancer, and aging. Aging Dis. 2022;13(2):423–32.
Liu X, Yin L, Shen S, Hou Y. Inflammation and cancer: paradoxical roles in tumorigenesis and implications in immunotherapies. Genes Dis. 2023;10(1):151–64.
Zeng Z, Lan T, Wei Y, Wei X. CCL5/CCR5 axis in human diseases and related treatments. Genes Dis. 2022;9(1):12–27.
Zhu R, Ji X, Wu X, Chen J, Li X, Jiang H, Fu H, Wang H, Lin Z, Tang X, Sun S, Li Q, Wang B, et al. Melatonin antagonizes ovarian aging via YTHDF2-MAPK-NF-kappaB pathway. Genes Dis. 2022;9(2):494–509.
Feng D, Li D, Shi X, Xiong Q, Zhang F, Wei Q, Yang L. A gene prognostic index from cellular senescence predicting metastasis and radioresistance for prostate cancer. J Transl Med. 2022;20(1):252.
Feng D, Shi X, Xiong Q, Zhang F, Li D, Yang L. A gene prognostic index associated with epithelial-mesenchymal transition predicting biochemical recurrence and tumor chemoresistance for prostate cancer. Front Oncol. 2021;11:805571.
Feng D, Shi X, Zhang F, Xiong Q, Wei Q, Yang L. Mitochondria dysfunction-mediated molecular subtypes and gene prognostic index for prostate cancer patients undergoing radical prostatectomy or radiotherapy. Front Oncol. 2022;12:858479.
Feng D, Li D, Wu R, Han P. Scientific advancements in drug development and trials for urothelial carcinoma insights from the 2023 ASCOGU cancers symposium. Aging Dis. 2023. https://doi.org/10.14336/AD.2023.0502.
Megerian MF, Kim JS, Badreddine J, Hong SH, Ponsky LE, Shin JI, Ghayda RA. Melatonin and prostate Cancer: anti-tumor roles and therapeutic application. Aging Dis. 2023;14(3):840–57.
Yang R, Zuo L, Ma H, Zhou Y, Zhou P, Wang L, Wang M, Latif M, Kong L. Downregulation of nc886 contributes to prostate cancer cell invasion and TGFbeta1-induced EMT. Genes Dis. 2022;9(4):1086–98.
Xu Z, Huang J, Gao M, Guo G, Zeng S, Chen X, Wang X, Gong Z, Yan Y. Current perspectives on the clinical implications of oxidative RNA damage in aging research: challenges and opportunities. Geroscience. 2021;43(2):487–505.
Zheng W, Feng D, Xiong X, Liao X, Wang S, Xu H, Le W, Wei Q, Yang L. The role of cGAS-STING in age-related diseases from mechanisms to therapies. Aging Dis. 2023. https://doi.org/10.14336/AD.2023.0117.
Feng D, Xiong Q, Wei Q, Yang L. Cellular landscape of tumour microenvironment in prostate cancer. Immunology. 2022. https://doi.org/10.1111/imm.13456.
Feng D, Liu S, Li D, Han P, Wei W. Analysis of conventional versus advanced pelvic floor muscle training in the management of urinary incontinence after radical prostatectomy: a systematic review and meta-analysis of randomized controlled trials. Transl Androl Urol. 2020;9(5):2031–45.
Feng D, Shi X, Xiong Q, Zhang F, Li D, Wei W, Yang L. A ferroptosis-related gene prognostic index associated with biochemical recurrence and radiation resistance for patients with prostate cancer undergoing radical radiotherapy. Front Cell Dev Biol. 2022;10:803766.
Feng D, Shi X, Zhang F, Xiong Q, Wei Q, Yang L. Energy metabolism-related gene prognostic index predicts biochemical recurrence for patients with prostate cancer undergoing radical prostatectomy. Front Immunol. 2022;13:839362.
Song Z, Cao Q, Guo B, Zhao Y, Li X, Lou N, Zhu C, Luo G, Peng S, Li G, Chen K, Wang Y, Ruan H, et al. Overexpression of RACGAP1 by E2F1 promotes neuroendocrine differentiation of prostate cancer by stabilizing EZH2 expression. Aging Dis. 2023. https://doi.org/10.14336/AD.2023.0202.
Dixon SJ, Lemberg KM, Lamprecht MR, Skouta R, Zaitsev EM, Gleason CE, Patel DN, Bauer AJ, Cantley AM, Yang WS, Morrison B 3rd, Stockwell BR. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149(5):1060–72.
Stockwell BR. Ferroptosis turns 10: emerging mechanisms, physiological functions, and therapeutic applications. Cell. 2022;185(14):2401–21.
Zhao L, Zhou X, Xie F, Zhang L, Yan H, Huang J, Zhang C, Zhou F, Chen J, Zhang L. Ferroptosis in cancer and cancer immunotherapy. Cancer Commun. 2022;42(2):88–116.
Xu J, Ding Y, Shi C, Yuan F, Sheng X, Liu Y, Xie Y, Lu H, Duan C, Hu J, Jiang L. Identification of cathepsin B as a therapeutic target for ferroptosis of macrophage after spinal cord injury. Aging Dis. 2023. https://doi.org/10.2139/ssrn.4165354.
Lu C, Tan C, Ouyang H, Chen Z, Yan Z, Zhang M. Ferroptosis in intracerebral hemorrhage: a panoramic perspective of the metabolism mechanism and theranostics. Aging Dis. 2022;13(5):1348–64.
Zhou N, Bao J. FerrDb: a manually curated resource for regulators and markers of ferroptosis and ferroptosis-disease associations. Database. 2020. https://doi.org/10.1093/database/baaa021.
Mortensen MM, Hoyer S, Lynnerup AS, Orntoft TF, Sorensen KD, Borre M, Dyrskjot L. Expression profiling of prostate cancer tissue delineates genes associated with recurrence after prostatectomy. Sci Rep. 2015;5:16018.
Kuner R, Falth M, Pressinotti NC, Brase JC, Puig SB, Metzger J, Gade S, Schafer G, Bartsch G, Steiner E, Klocker H, Sultmann H. The maternal embryonic leucine zipper kinase (MELK) is upregulated in high-grade prostate cancer. J Mol Med (Berl). 2013;91(2):237–48.
Penney KL, Sinnott JA, Tyekucheva S, Gerke T, Shui IM, Kraft P, Sesso HD, Freedman ML, Loda M, Mucci LA, Stampfer MJ. Association of prostate cancer risk variants with gene expression in normal and tumor tissue. Cancer Epidemiol Biomarkers Prev. 2015;24(1):255–60.
Li T, Fan J, Wang B, Traugh N, Chen Q, Liu JS, Li B, Liu XS. TIMER: a web server for comprehensive analysis of tumor-infiltrating immune cells. Cancer Res. 2017;77(21):e108–10.
Chandrashekar DS, Bashel B, Balasubramanya SAH, Creighton CJ, Ponce-Rodriguez I, Chakravarthi B, Varambally S. UALCAN: a portal for facilitating tumor subgroup gene expression and survival analyses. Neoplasia. 2017;19(8):649–58.
Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z. GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017;45(W1):W98–102.
Cojoc M, Peitzsch C, Kurth I, Trautmann F, Kunz-Schughart LA, Telegeev GD, Stakhovsky EA, Walker JR, Simin K, Lyle S, Fuessel S, Erdmann K, Wirth MP, et al. Aldehyde dehydrogenase Is regulated by beta-catenin/TCF and promotes radioresistance in prostate cancer progenitor cells. Cancer Res. 2015;75(7):1482–94.
Beroukhim R, Mermel CH, Porter D, Wei G, Raychaudhuri S, Donovan J, Barretina J, Boehm JS, Dobson J, Urashima M, Mc Henry KT, Pinchback RM, Ligon AH, et al. The landscape of somatic copy-number alteration across human cancers. Nature. 2010;463(7283):899–905.
Uhlen M, Fagerberg L, Hallstrom BM, Lindskog C, Oksvold P, Mardinoglu A, Sivertsson A, Kampf C, Sjostedt E, Asplund A, Olsson I, Edlund K, Lundberg E, et al. Proteomics tissue-based map of the human proteome. Science. 2015;347(6220):1260419.
Uhlen M, Zhang C, Lee S, Sjostedt E, Fagerberg L, Bidkhori G, Benfeitas R, Arif M, Liu Z, Edfors F, Sanli K, von Feilitzen K, Oksvold P, et al. A pathology atlas of the human cancer transcriptome. Science. 2017. https://doi.org/10.1126/science.aan2507.
Warde-Farley D, Donaldson SL, Comes O, Zuberi K, Badrawi R, Chao P, Franz M, Grouios C, Kazi F, Lopes CT, Maitland A, Mostafavi S, Montojo J, et al. The GeneMANIA prediction server: biological network integration for gene prioritization and predicting gene function. Nucleic Acids Res. 2010;38:W214-220.
Szklarczyk D, Gable AL, Nastou KC, Lyon D, Kirsch R, Pyysalo S, Doncheva NT, Legeay M, Fang T, Bork P, Jensen LJ, von Mering C. The STRING database in 2021: customizable protein-protein networks, and functional characterization of user-uploaded gene/measurement sets. Nucleic Acids Res. 2021;49(D1):D605–12.
Hanzelmann S, Castelo R, Guinney J. GSVA: gene set variation analysis for microarray and RNA-seq data. BMC Bioinformatics. 2013;14:7.
Liberzon A, Subramanian A, Pinchback R, Thorvaldsdottir H, Tamayo P, Mesirov JP. Molecular signatures database (MSigDB) 3.0. Bioinformatics. 2011;27(12):1739–40.
Li B, Severson E, Pignon JC, Zhao H, Li T, Novak J, Jiang P, Shen H, Aster JC, Rodig S, Signoretti S, Liu JS, Liu XS. Comprehensive analyses of tumor immunity: implications for cancer immunotherapy. Genome Biol. 2016;17(1):174.
Yoshihara K, Shahmoradgoli M, Martinez E, Vegesna R, Kim H, Torres-Garcia W, Trevino V, Shen H, Laird PW, Levine DA, Carter SL, Getz G, Stemke-Hale K, et al. Inferring tumour purity and stromal and immune cell admixture from expression data. Nat Commun. 2013;4:2612.
Zeng D, Ye Z, Shen R, Yu G, Wu J, Xiong Y, Zhou R, Qiu W, Huang N, Sun L, Li X, Bin J, Liao Y, et al. IOBR: multi-omics immuno-oncology biological research to decode tumor microenvironment and signatures. Front Immunol. 2021;12:687975.
Ru B, Wong CN, Tong Y, Zhong JY, Zhong SSW, Wu WC, Chu KC, Wong CY, Lau CY, Chen I, Chan NW, Zhang J. TISIDB: an integrated repository portal for tumor-immune system interactions. Bioinformatics. 2019;35(20):4200–2.
Jiang P, Gu S, Pan D, Fu J, Sahu A, Hu X, Li Z, Traugh N, Bu X, Li B, Liu J, Freeman GJ, Brown MA, et al. Signatures of T cell dysfunction and exclusion predict cancer immunotherapy response. Nat Med. 2018;24(10):1550–8.
Thorsson V, Gibbs DL, Brown SD, Wolf D, Bortone DS, Ou Yang T-H, Porta-Pardo E, Gao GF, Plaisier CL, Eddy JA, Ziv E, Culhane AC, Paull EO, et al. The immune landscape of cancer. Immunity. 2018;48(4):812-830.e814.
Bonneville R, Krook MA, Kautto EA, Miya J, Wing MR, Chen H-Z, Reeser JW, Yu L, Roychowdhury S. Landscape of microsatellite instability across 39 cancer types. JCO Precis Oncol. 2017;2017:1.
Malta TM, Sokolov A, Gentles AJ, Burzykowski T, Poisson L, Weinstein JN, Kamińska B, Huelsken J, Omberg L, Gevaert O, Colaprico A, Czerwińska P, Mazurek S, et al. Machine learning identifies stemness features associated with oncogenic dedifferentiation. Cell. 2018;173(2):338-354.e315.
Feng D, Wang J, Shi X, Li D, Wei W, Han P. Membrane tension-mediated stiff and soft tumor subtypes closely associated with prognosis for prostate cancer patients. Eur J Med Res. 2023;28(1):172.
Shi X, Feng D, Li D, Han P, Yang L, Wei W. A pan-cancer analysis of the oncogenic and immunological roles of apolipoprotein F (APOF) in human cancer. Eur J Med Res. 2023;28(1):190.
Feng D, Shi X, Zhu W, Zhang F, Li D, Han P, Wei Q, Yang L. A pan-cancer analysis of the oncogenic role of leucine zipper protein 2 in human cancer. Exp Hematol Oncol. 2022;11(1):55.
Zhu W, Feng D, Shi X, Li D, Wei Q, Yang L. A pan-cancer analysis of the oncogenic role of zinc finger protein 419 in human cancer. Front Oncol. 2022;12:1042118.
Qian Y, Feng D, Wang J, Wei W, Wei Q, Han P, Yang L. Establishment of cancer-associated fibroblasts-related subtypes and prognostic index for prostate cancer through single-cell and bulk RNA transcriptome. Sci Rep. 2023;13(1):9016.
Liu CJ, Hu FF, Xia MX, Han L, Zhang Q, Guo AY. GSCALite: a web server for gene set cancer analysis. Bioinformatics. 2018;34(21):3771–2.
Feng D, Zhu W, Shi X, Wei W, Han P, Wei Q, Yang L. Leucine zipper protein 2 serves as a prognostic biomarker for prostate cancer correlating with immune infiltration and epigenetic regulation. Heliyon. 2022;8(10):e10750.
Stockwell BR, Friedmann Angeli JP, Bayir H, Bush AI, Conrad M, Dixon SJ, Fulda S, Gascon S, Hatzios SK, Kagan VE, Noel K, Jiang X, Linkermann A, et al. Ferroptosis: a regulated cell death nexus linking metabolism, redox biology, and disease. Cell. 2017;171(2):273–85.
Yao F, Zhao Y, Ma L. LIF-ting ferroptosis to improve liver cancer therapy. Genes Dis. 2022;9(5):1153–5.
Wang L, Chen X, Yan C. Ferroptosis: an emerging therapeutic opportunity for cancer. Genes Dis. 2022;9(2):334–46.
Sun Y, He Y, Tong J, Liu D, Zhang H, He T, Bi Y. All-trans retinoic acid inhibits the malignant behaviors of hepatocarcinoma cells by regulating ferroptosis. Genes Dis. 2022;9(6):1742–56.
Pu F, Chen F, Zhang Z, Shi D, Zhong B, Lv X, Tucker AB, Fan J, Li AJ, Qin K, Hu D, Chen C, Wang H, et al. Ferroptosis as a novel form of regulated cell death: implications in the pathogenesis, oncometabolism and treatment of human cancer. Genes Dis. 2022;9(2):347–57.
Yang WS, SriRamaratnam R, Welsch ME, Shimada K, Skouta R, Viswanathan VS, Cheah JH, Clemons PA, Shamji AF, Clish CB, Brown LM, Girotti AW, Cornish VW, et al. Regulation of ferroptotic cancer cell death by GPX4. Cell. 2014;156(1–2):317–31.
Doll S, Freitas FP, Shah R, Aldrovandi M, da Silva MC, Ingold I, Goya Grocin A, Xavier da Silva TN, Panzilius E, Scheel CH, Mourao A, Buday K, Sato M, et al. FSP1 is a glutathione-independent ferroptosis suppressor. Nature. 2019;575(7784):693–8.
Bersuker K, Hendricks JM, Li Z, Magtanong L, Ford B, Tang PH, Roberts MA, Tong B, Maimone TJ, Zoncu R, Bassik MC, Nomura DK, Dixon SJ, et al. The CoQ oxidoreductase FSP1 acts parallel to GPX4 to inhibit ferroptosis. Nature. 2019;575(7784):688–92.
Shimada K, Skouta R, Kaplan A, Yang WS, Hayano M, Dixon SJ, Brown LM, Valenzuela CA, Wolpaw AJ, Stockwell BR. Global survey of cell death mechanisms reveals metabolic regulation of ferroptosis. Nat Chem Biol. 2016;12(7):497–503.
Yang WS, Stockwell BR. Ferroptosis: death by lipid peroxidation. Trends Cell Biol. 2016;26(3):165–76.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Tousignant KD, Rockstroh A, Poad BLJ, Talebi A, Young RSE, Taherian Fard A, Gupta R, Zang T, Wang C, Lehman ML, Swinnen JV, Blanksby SJ, Nelson CC, et al. Therapy-induced lipid uptake and remodeling underpin ferroptosis hypersensitivity in prostate cancer. Cancer Metab. 2020;8:11.
Ghoochani A, Hsu EC, Aslan M, Rice MA, Nguyen HM, Brooks JD, Corey E, Paulmurugan R, Stoyanova T. Ferroptosis inducers are a novel therapeutic approach for advanced prostate cancer. Cancer Res. 2021;81(6):1583–94.
Yang Y, Liu T, Hu C, Xia H, Liu W, Chen J, Wu S, Jiang Y, Xu Y, Liu W, Zhao L. Ferroptosis inducer erastin downregulates androgen receptor and its splice variants in castrationresistant prostate cancer. Oncol Rep. 2021. https://doi.org/10.3892/or.2021.7976.
Qin Z, Ou S, Xu L, Sorensen K, Zhang Y, Hu DP, Yang Z, Hu WY, Chen F, Prins GS. Design and synthesis of isothiocyanate-containing hybrid androgen receptor (AR) antagonist to downregulate AR and induce ferroptosis in GSH-Deficient prostate cancer cells. Chem Biol Drug Des. 2021;97(5):1059–78.
Karala AR, Ruddock LW. Bacitracin is not a specific inhibitor of protein disulfide isomerase. FEBS J. 2010;277(11):2454–62.
Wang X, Bai Y, Zhang F, Yang Y, Feng D, Li A, Yang Z, Li D, Tang Y, Wei X, Wei W, Han P. Targeted inhibition of P4HB promotes cell sensitivity to gemcitabine in urothelial carcinoma of the bladder. Onco Targets Ther. 2020;13:9543–58.
Chen YC, Oses-Prieto JA, Pope LE, Burlingame AL, Dixon SJ, Renslo AR. Reactivity-based probe of the iron(II)-dependent interactome identifies new cellular modulators of ferroptosis. J Am Chem Soc. 2020;142(45):19085–93.
Pan CF, Wei K, Ma ZJ, He YZ, Huang JJ, Guo ZZ, Chen ZP, Barr MP, Shackelford RE, Xia Y, Wang J. CircP4HB regulates ferroptosis via SLC7A11-mediated glutathione synthesis in lung adenocarcinoma. Transl Lung Cancer Res. 2022;11(3):366–80.
Sun S, Kiang KMY, Ho ASW, Lee D, Poon MW, Xu FF, Pu JKS, Kan ANC, Lee NPY, Liu XB, Man K, Day PJR, Lui WM, et al. Endoplasmic reticulum chaperone prolyl 4-hydroxylase, beta polypeptide (P4HB) promotes malignant phenotypes in glioma via MAPK signaling. Oncotarget. 2017;8(42):71911–23.
Wen Z, Sun Q, Shan Y, Xie W, Ding Y, Wang W, Ye R, Xiao W, Li Y. Endoplasmic reticulum stress in osteoarthritis: a novel perspective on the pathogenesis and treatment. Aging Dis. 2023;14(2):283–6.
Gaschler MM, Hu F, Feng H, Linkermann A, Min W, Stockwell BR. Determination of the subcellular localization and mechanism of action of ferrostatins in suppressing ferroptosis. ACS Chem Biol. 2018;13(4):1013–20.
Banhegyi G, Baumeister P, Benedetti A, Dong D, Fu Y, Lee AS, Li J, Mao C, Margittai E, Ni M, Paschen W, Piccirella S, Senesi S, et al. Endoplasmic reticulum stress. Ann N Y Acad Sci. 2007;1113:58–71.
Pachikov AN, Gough RR, Christy CE, Morris ME, Casey CA, LaGrange CA, Bhat G, Kubyshkin AV, Fomochkina II, Zyablitskaya EY, Makalish TP, Golubinskaya EP, Davydenko KA, et al. The non-canonical mechanism of ER stress-mediated progression of prostate cancer. J Exp Clin Cancer Res. 2021;40(1):289.
Dixon SJ, Patel DN, Welsch M, Skouta R, Lee ED, Hayano M, Thomas AG, Gleason CE, Tatonetti NP, Slusher BS, Stockwell BR. Pharmacological inhibition of cystine-glutamate exchange induces endoplasmic reticulum stress and ferroptosis. Elife. 2014;3:e02523.
Lee YS, Lee DH, Choudry HA, Bartlett DL, Lee YJ. Ferroptosis-induced endoplasmic reticulum stress: cross-talk between ferroptosis and apoptosis. Mol Cancer Res. 2018;16(7):1073–6.
Luo B, Lee AS. The critical roles of endoplasmic reticulum chaperones and unfolded protein response in tumorigenesis and anticancer therapies. Oncogene. 2013;32(7):805–18.
Ma Y, Hendershot LM. The role of the unfolded protein response in tumour development: friend or foe? Nat Rev Cancer. 2004;4(12):966–77.
Jin Y, Saatcioglu F. Targeting the unfolded protein response in hormone-regulated cancers. Trends Cancer. 2020;6(2):160–71.
Sheng X, Arnoldussen YJ, Storm M, Tesikova M, Nenseth HZ, Zhao S, Fazli L, Rennie P, Risberg B, Waehre H, Danielsen H, Mills IG, Jin Y, et al. Divergent androgen regulation of unfolded protein response pathways drives prostate cancer. EMBO Mol Med. 2015;7(6):788–801.
Stelloo S, Linder S, Nevedomskaya E, Valle-Encinas E, de Rink I, Wessels LFA, van der Poel H, Bergman AM, Zwart W. Androgen modulation of XBP1 is functionally driving part of the AR transcriptional program. Endocr Relat Cancer. 2020;27(2):67–79.
Johnson GG, White MC, Grimaldi M. Stressed to death: targeting endoplasmic reticulum stress response induced apoptosis in gliomas. Curr Pharm Des. 2011;17(3):284–92.
Boyce M, Yuan J. Cellular response to endoplasmic reticulum stress: a matter of life or death. Cell Death Differ. 2006;13(3):363–73.
Virrey JJ, Dong D, Stiles C, Patterson JB, Pen L, Ni M, Schonthal AH, Chen TC, Hofman FM, Lee AS. Stress chaperone GRP78/BiP confers chemoresistance to tumor-associated endothelial cells. Mol Cancer Res. 2008;6(8):1268–75.
Fonseca C, Soiffer R, Ho V, Vanneman M, Jinushi M, Ritz J, Neuberg D, Stone R, DeAngelo D, Dranoff G. Protein disulfide isomerases are antibody targets during immune-mediated tumor destruction. Blood. 2009;113(8):1681–8.
Kremer DM, Nelson BS, Lin L, Yarosz EL, Halbrook CJ, Kerk SA, Sajjakulnukit P, Myers A, Thurston G, Hou SW, Carpenter ES, Andren AC, Nwosu ZC, et al. GOT1 inhibition promotes pancreatic cancer cell death by ferroptosis. Nat Commun. 2021;12(1):4860.
Seibt TM, Proneth B, Conrad M. Role of GPX4 in ferroptosis and its pharmacological implication. Free Radic Biol Med. 2019;133:144–52.
Hinshaw DC, Shevde LA. The tumor microenvironment innately modulates cancer progression. Cancer Res. 2019;79(18):4557–66.
Feng D, Xiong Q, Wei Q, Yang L. Cellular landscape of tumour microenvironment in prostate cancer. Immunology. 2023;168(2):199–202.
Yan J, Xiao G, Yang C, Liu Q, Lv C, Yu X, Zhou Z, Lin S, Bai Z, Lin H, Zhang R, Liu C. Cancer-associated fibroblasts promote lymphatic metastasis in cholangiocarcinoma via the PDGF-BB/PDGFR-beta mediated paracrine signaling network. Aging Dis. 2023. https://doi.org/10.14336/AD.2023.0420.
Yang Y, Gu J, Li X, Xue C, Ba L, Gao Y, Zhou J, Bai C, Sun Z, Zhao RC. HIF-1alpha promotes the migration and invasion of cancer-associated fibroblasts by miR-210. Aging Dis. 2021;12(7):1794–807.
You T, Tang H, Wu W, Gao J, Li X, Li N, Xu X, Xing J, Ge H, Xiao Y, Guo J, Wu B, Li X, et al. POSTN secretion by extracellular matrix cancer-associated fibroblasts (eCAFs) correlates with poor ICB response via macrophage chemotaxis activation of Akt signaling pathway in gastric cancer. Aging Dis. 2023. https://doi.org/10.14336/AD.2023.0503.
Shu H, Wen Z, Li N, Zhang Z, Ceesay BM, Peng Y, Zhou N, Wang DW. COVID-19 and cardiovascular diseases: from cellular mechanisms to clinical manifestations. Aging Dis. 2023. https://doi.org/10.14336/AD.2023.0314.
Schulz L, Hornung F, Hader A, Radosa L, Brakhage AA, Loffler B, Deinhardt-Emmer S. Influenza virus-induced paracrine cellular senescence of the lung contributes to enhanced viral load. Aging Dis. 2023. https://doi.org/10.14336/AD.2023.0310.
Shiao SL, Chu GC, Chung LW. Regulation of prostate cancer progression by the tumor microenvironment. Cancer Lett. 2016;380(1):340–8.
Wang W, Green M, Choi JE, Gijon M, Kennedy PD, Johnson JK, Liao P, Lang X, Kryczek I, Sell A, Xia H, Zhou J, Li G, et al. CD8(+) T cells regulate tumour ferroptosis during cancer immunotherapy. Nature. 2019;569(7755):270–4.
Wu P, Xiang T, Wang J, Lv R, Ma S, Yuan L, Wu G, Che X. Identification of immunization-related new prognostic biomarkers for papillary renal cell carcinoma by integrated bioinformatics analysis. BMC Med Genomics. 2021;14(1):241.
Robinson RM, Reyes L, Duncan RM, Bian H, Strobel ED, Hyman SL, Reitz AB, Dolloff NG. Tuning isoform selectivity and bortezomib sensitivity with a new class of alkenyl indene PDI inhibitor. Eur J Med Chem. 2020;186:111906.
Wan C, Sun Y, Tian Y, Lu L, Dai X, Meng J, Huang J, He Q, Wu B, Zhang Z, Jiang K, Hu D, Wu G, et al. Irradiated tumor cell-derived microparticles mediate tumor eradication via cell killing and immune reprogramming. Sci Adv. 2020;6(13):eaay9789.
Zhang J, Yang J, Zuo T, Ma S, Xokrat N, Hu Z, Wang Z, Xu R, Wei Y, Shen Q. Heparanase-driven sequential released nanoparticles for ferroptosis and tumor microenvironment modulations synergism in breast cancer therapy. Biomaterials. 2021;266:120429.
Acknowledgements
We appreciated the Figdraw (www.figdraw.com) and Chengdu Basebiotech Co., Ltd (http://www.basebio.cc) for their assistance in drawing and data process.
Funding
This program was supported by the National Key Research and Development Program of China (2021YFC2009303), Project of Health Commission of Sichuan Province (21PJ041) and the Key Research and Development Support Plan of Chengdu Science and Technology Bureau (2022-YF05-01568-SN). The funders had no role in the study design, data collection or analysis, preparation of the manuscript, or the decision to publish.
Author information
Authors and Affiliations
Contributions
DCF and LL proposed the project, conducted data analysis, interpreted the data, and wrote the manuscript; JW, DXL, RCW and LXY conducted data analysis, interpreted the data; DCF and PH supervised the project, and interpreted the data. All authors reviewed and edited the manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Feng, D., Li, L., Li, D. et al. Prolyl 4-hydroxylase subunit beta (P4HB) could serve as a prognostic and radiosensitivity biomarker for prostate cancer patients. Eur J Med Res 28, 245 (2023). https://doi.org/10.1186/s40001-023-01215-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01215-2