Abstract
Global Coronavir us disease 2019 (COVID-19) vaccination efforts are being intensified to combat the pandemic. As the frequency of immunization against COVID-19 has increased, some adverse effects related to vaccination have emerged. Within this context, this article reviewed 62 Graves’ disease (GD) cases following COVID-19 vaccination, to probe the potential association between the vaccination and the onset of GD. A comprehensive search of the PubMed, Web of Science, and Scopus databases was conducted to collect GD cases following COVID-19 vaccination up to June 7, 2023. Among the 62 GD cases included in this review, there were 33 (53.2%) new-onset GD and 10 (16.1%) relapsed GD patients following mRNA vaccination, 14 (22.6%) new-onset GD and 4 (6.5%) relapsed GD patients following viral vector vaccination, and 1 (1.6%) relapsed GD patients following inactivated vaccination. Median durations to symptoms onset for new-onset and relapsed GD were 12 (range: 1–60) and 21 (range: 5–30) days following mRNA vaccination, while 7 (range: 1–28) and 14 (range: 10–14) days following viral vector vaccination, respectively. While the definitive pathogenesis of GD following COVID-19 vaccination remains unclear, it might be associated with cross-immune responses triggered by molecular mimicry, and an adjuvant-induced autoimmune/inflammatory syndrome. However, due to the limited number of observed GD cases following COVID-19 vaccination and the lack of systematic experimental studies, a causal relationship between COVID-19 vaccination and the onset of GD has not been definitively confirmed. It should be highlighted that most of GD patients following COVID-19 vaccination experienced positive outcomes after treatment. In the broader context of ending the COVID-19 pandemic and reducing mortality rates, the benefits of COVID-19 vaccination significantly outweigh mild risks such as treatable GD. Adherence to the COVID-19 vaccination schedule is therefore imperative in effectively managing the pandemic.
Similar content being viewed by others
Introduction
COVID-19, an acute respiratory infectious disease instigated by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1], poses a formidable global challenge. As of 7 June 2023, the World Health Organization reported an excess of 700 million COVID-19 cases and over six million associated fatalities all over the world [2]. As the pandemic spreads, researchers have found that SARS-CoV-2 infection can affect not only the respiratory system but also multiple organs, including the endocrine glands [3,4,5,6]. At present, the emergence of conditions such as GD, subacute thyroiditis, and diabetes mellitus in association with COVID-19 has been reported [7,8,9,10,11,12,13,14]. In response to this global crisis, COVID-19 vaccination efforts are being intensified globally to control the COVID-19 pandemic. In a meta-analysis, Zheng et al. [15] found that the effectiveness of COVID-19 vaccines against SARS-CoV-2 infection, COVID-19-related hospitalization, intensive care unit hospitalization and death was 89.1%, 97.2%, 97.4%, and 99.0%, respectively, among fully vaccinated populations. Thus, COVID-19 vaccination emerges as a crucial strategy for curtailing SARS-CoV-2 infection and related adverse outcomes,which can provide substantial population protection.
Based on statistics from Our World in Data, as published by the University of Oxford, 70.1% of the global population have received at least a single dose of COVID-19 vaccine, with a total of 13.41 billion doses administered worldwide, and 102,962 doses administered daily [16]. With the rise in COVID-19 vaccination rates, several associated adverse effects have been observed, including fever, fatigue, muscle aches, and some autoimmune diseases [17,18,19,20,21,22]. Hyperthyroidism refers to thyrotoxicosis caused by the thyroid gland itself producing excessive thyroid hormones, and GD is the most common etiology of hyperthyroidism [23, 24]. GD falls under the umbrella of autoimmune thyroid diseases, characterized primarily by the presence of thyrotropin receptor antibody (TRAb) in the serum [24,25,26]. While the pathophysiology of GD remains unclear, recent studies suggest that genetic, epigenetic, and environmental factors may all be significant contributors to the disease [27,28,29,30]. Recently, there has been a succession of reported cases of GD following COVID-19 vaccination [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64]. However, it is unclear whether COVID-19 vaccination has any effect on the occurrence and development of GD. This article reviewed 47 new-onset GD cases and 15 relapsed GD cases following COVID-19 vaccination in order to explore whether there is a correlation between COVID-19 vaccination and GD onset and the pathogenic mechanisms.
Methods
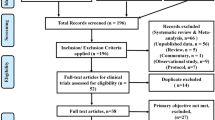
We performed a comprehensive literature review to identify all reports of GD cases following COVID-19 vaccination by searching for indexed articles up to 7 June 2023 in databases including PubMed, Web of Science, and Scopus. Only articles written and published in English were considered. The search strategy employed various keywords both individually and in combination, namely: SARS-CoV-2, COVID-19, thyroid, Graves’ disease, autoimmune thyroid disease, hyperthyroidism, thyrotoxicosis, vaccine, and vaccination. The main inclusion criteria were as follows: 1. case reports, case series, and original articles with adequate case data; 2. letters and comments to the editor published in international journals with adequate case data. The main exclusion criteria were as follows: 1. cases with inadequate data; 2. cases with overlapping patient data; 3. patients previously infected with SARS-CoV-2. From an initial selection of 71 articles, 33 articles met our inclusion criteria, and a total of 62 GD cases following COVID-19 vaccination were included in the analysis.
For each patient, we collected demographic data including sex and age, the type of administered COVID-19 vaccine (mRNA vaccine, viral vector vaccine, inactivated vaccine), the onset time of hyperthyroidism symptoms following COVID-19 vaccination, symptoms and signs at presentation, thyroid function tests (TFTs) such as free thyroxine (fT4), free triiodothyronine (fT3), and thyroid-stimulating hormone (TSH), thyroid antibody tests such as thyroid-stimulating immunoglobulin (TSI), thyroid peroxidase antibodies (TPOAb), and thyroglobulin antibodies (TgAb), as well as other diagnostic examinations such as thyroid ultrasonography and thyroid scintigraphy."
Specific medical therapies and clinical or hormonal follow-up data were also recorded. Based on the 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis [24], the diagnostic criteria for GD included: (a) TFTs consistent with hyperthyroidism; (b) positive TRAb or TSI; (c) the presence of a thyroid scan showing high radioactive iodine or 99mtechnetium uptake; or (d) a thyroid ultrasound showing diffuse hypervascularization of the glandular parenchyma.
New-onset and relapsed GD following COVID-19 vaccination
Among the 62 GD cases following COVID-19 vaccination, the mean age was 42.98 ± 14.34 years, with 45/62 (72.6%) of the patients being female and 17/62 (27.4%) male (Table 2). All patients tested positive for TRAb or TSI. Although GD can affect all ages, it is notably more prevalent among women of reproductive age, and the female-to-male ratio is 5–10: 1 [30, 31]. This gender and age distribution of GD cases following COVID-19 vaccination aligned with that of classical GD cases. The distribution of new-onset and relapsed GD after administration of COVID-19 mRNA vaccines and viral vector vaccines was illustrated in Table 1. However, neither reports have presented new-onset GD cases after receiving inactivated vaccines, nor were there any new-onset and relapsed GD cases after protein subunit vaccine administration. Of the 62 GD patients after receiving COVID-19 vaccines, six female patients and two males were diagnosed with hyperthyroidism through TFTs rather than by presenting hyperthyroidism-related symptoms. Two female patients had received two doses of COVID-19 inactivated vaccines before the mRNA and viral vector vaccines. Excluding the aforementioned 10 patients, the remaining 52 patients developed common hyperthyroidism symptoms after receiving COVID-19 vaccines, such as weight loss, palpitations, and hyperhidrosis, with a median symptom onset time of 12 days. The median durations to symptoms onset for new-onset (12 days vs 7 days) and relapsed GD (21 days vs 14 days) were longer following COVID-19 mRNA vaccine administration than viral vector vaccination. In female patients, the incidences of both new-onset and relapsed GD following the first dose of COVID-19 vaccines were higher than those after the second dose (Table 2).
The main characteristics of the 47 new-onset GD patients associated with COVID-19 vaccination were summarized in Table 3. In the reported new-onset GD cases, the main clinical manifestations, thyroid functions, and thyroid ultrasonography were consistent with those of the classical GD cases (Table 3). Notably, a female patient (Case 5), who was inoculated with two doses of the COVID-19 inactivated vaccine, followed by a dose of the mRNA vaccine, experienced hyperthyroidism symptoms, such as palpitations in two days after the mRNA vaccination (Table 3) [33]. Among all the new-onset GD patients following COVID-19 vaccination, 3 female patients (Cases 17, 26, and 47) and 2 males (Cases 15 and 31) did not exhibit hyperthyroidism symptoms after COVID-19 vaccination [37, 39, 47, 49, 52]. Their hyperthyroidism was incidentally identified due to routine TFTs (Table 3). According to literature, most of those patients found symptoms relieved following anti-thyroid drug (ATD) treatment [34, 35, 37,38,39]. It is worth noting that 3 female patients (Cases 8, 9, and 11) developed hyperthyroidism symptoms after the first COVID-19 mRNA vaccine dose and were diagnosed as new-onset GD [35], as another 2 female patients (Cases 42 and 44) after the first COVID-19 viral vector vaccine dose did [60]. These patients had also received their second doses of COVID-19 vaccines when their conditions stabilized post-ATD treatment. Their conditions did not worsen or require adjusting the doses of ATD and beta-blocker after receiving the second doses [35, 60]. Filippo et al. [65] conducted a case–control study and found that among 64 patients who developed new-onset GD after COVID-19 vaccination, and 20/64 (31.2%) patients experienced post-vaccine early-onset GD (PoVEO) within 4 weeks. The patients with PoVEO GD exhibited unique clinical characteristics as compared to the other 44 patients, including older age at onset, higher male prevalence, and a better initial biochemical and immunologic response to ATD treatments. However, in contrast to those clinical trials, our study is a review of the existing patients, which has aimed to observe the clinical characteristics of new-onset GD cases following COVID-19 vaccination. Based on their clinical characteristics, we analyzed the potential impacts of COVID-19 vaccines on the development of GD. The limited series suggest that for new-onset GD patients following the first COVID-19 mRNA and viral vector vaccine injections, a second dose may be administered once the hyperthyroid conditions are adequately controlled. Nonetheless, constant monitoring of thyroid functions should be kept after the second dose administration.
Table 4 summarized the main characteristics of the 15 relapsed GD cases associated with COVID-19 vaccination. Among those cases, a female patient (Case 14), who had received two doses of inactivated COVID-19 vaccines followed by a viral vector vaccine, developed hyperthyroidism symptoms like palpitations four days after viral vector vaccination (Table 4) [36]. However, among all the relapsed GD patients following COVID-19 vaccination, 3 female patients (Cases 4, 5, and 7) did not present any hyperthyroidism symptoms after COVID-19 vaccination (Table 4) [35]. Their hyperthyroidism was incidentally identified due to routine TFTs. Studies have suggested that approximately 50% of GD patients treated with ATD would experience relapse and it typically occurs between 6 and 18 months after the cessation of ATD treatment [66,67,68]. Among the 15 cases of relapsed GD after COVID-19 vaccination, a male patient and a female (Cases 1 and 2) relapsed approximately 12 months after ceasing ATD treatment [34]. This potentially represents the natural course of GD. However, in the 3 female patients (Cases 9, 10, and 15), their GD relapse occurred at the 17th, 7th, and 12th years, respectively, after ceasing ATD treatment [34, 37, 62]. This underlines the necessity for further investigations into the potential correlation between COVID-19 vaccination and GD relapse. Furthermore, a 30-year-old female (Case 14) was diagnosed with GD in October 2018 and has been treated with 2.5 mg of methimazole daily to maintain euthyroidism. She received two doses of COVID-19 inactivated vaccine on April 7 and 26, 2021, and her thyroid function remained normal after COVID-19 vaccination. However, following a dose of the viral vector vaccine on July 19, 2021, she developed symptoms such as palpitations and weight loss four days later. By self-increasing the methimazole dose to 5 mg, she managed to relieve some symptoms, but her fT3 level remained elevated and TRAb was positive one month after adjusting the dose of methimazole [56]. Due to the limited number of reported GD cases following COVID-19 vaccination, and the lack of GD cases after receiving the protein subunit vaccine, it is currently impossible to clarify the causal relationship between COVID-19 vaccination and the onset of GD. Fortunately, most patients who developed GD following COVID-19 vaccination experienced positive outcomes after ATD treatment. In the broader context of ending the COVID-19 pandemic and reducing mortality rates, the benefits of COVID-19 vaccination significantly outweigh mild risks such as treatable GD.
Possible pathogenesis of COVID-19 vaccination-related GD
Currently, the pathogenic mechanisms of COVID-19 vaccination-related GD has not yet been fully elucidated. Several studies suggest that new-onset and relapsed GD following COVID-19 vaccination may be linked to several potential mechanisms as follows [32,33,34,35,36,37,38,39,40, 56, 57, 62]. One possible mechanism could be molecular mimicry. The antigen structure of the COVID-19 vaccine closely resembles some autoantigens, eliciting an immune response that could erroneously target host cells with similar autoantigens [32,33,34,35,36, 38, 39, 57]. There are four genera of the coronavirus family: α, β, γ, and δ coronaviruses [69, 70]. SARS-CoV-2, the causative agent of COVID-19, is a member of the Coronaviridae family. This virus is enveloped and possesses a positive single-stranded RNA genome [71,72,73]. The genome's length varies between 26 and 32 kb, including 6 to 11 open reading frames [74]. It encodes four essential structural proteins—spike, envelope, membrane, and nucleocapsid, all of which play critical roles in the assembly and infectivity of SARS-CoV-2 [69, 75, 76]. Among these proteins, the spike protein is particularly important in facilitating the virus's pathogenicity [77, 78]. It operates as a trimeric fusion type I glycoprotein, binding to the angiotensin converting enzyme 2 (ACE2) on the host cell membrane through its receptor-binding domain (RBD) on the S1 subunit [79]. The binding of the RBD to the ACE2 receptor on the host cell membrane instigates the shedding of the S1 subunit. This event prompts the S2 subunit to adopt a stable post-fusion conformation. The consequent structural changes within the S2 subunit facilitate the integration of the viral lipid membrane into the host cell membrane. This action thereby allows the viral RNA to enter the host cell for replication [80,81,82]. Hence, due to its crucial role in the infection process, the spike protein is the primary immunogen in the development of the COVID-19 vaccine [83]. Vojdani et al. [84] found that SARS-CoV-2 antibodies could immunoreact with multiple tissue antigens, including those of the thyroid gland. They employed the Basic Local Alignment Search Tool provided by the National Institutes of Health/National Library of Medicine to conduct a sequence matching analysis. Their findings revealed that the amino acid sequences of the SARS-CoV-2 spike protein, nucleoprotein, and membrane protein share a similarity ranging from 50 to 70% with that of thyroid peroxidase [84]. Given that the spike protein plays a pivotal role as an immunogen in the development of the COVID-19 vaccine [83], there is a possibility that the COVID-19 vaccine could incite an autoimmune response against thyroid tissue through molecular mimicry, thereby contributing to the onset of GD. It is important to note that molecular similarity does not necessarily result in the development of GD. A systematic review, including 48 new-onset and 15 relapsed GD cases following COVID-19 vaccination, proposed that individual susceptibility appears to play a critical role in the development of GD following COVID-19 vaccination, regardless of the underlying pathogenic mechanisms [85]. Therefore, other factors such as genetic susceptibility may also contribute to the development of GD. However, it should be noted that unlike our study, this systematic review did not exclude patients with a history of SARS-CoV-2 infection. In our study, we specifically excluded patients who had previously been infected with SARS-CoV-2 to further eliminate the potential impact of SARS-CoV-2 infection on the pathogenesis of GD.
Moreover, another pathogenesis connected to Autoimmune/Inflammatory Syndrome Induced by Adjuvants (ASIA) has been proposed in the literature [32,33,34,35,36,37,38,39,40, 56, 57, 62]. The term 'ASIA', first proposed by Shoenfeld et al., describes the aberrant autoimmune response post-exposure to a vaccine adjuvant [86]. Common types include post-vaccination syndrome, Gulf War syndrome, and macrophagic myofasciitis syndrome [87]. According to the diagnostic criteria outlined in Table 5, all 62 patients with new-onset or relapsed GD after COVID-19 vaccination satisfied the diagnosis of ASIA [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64]. In 2013, Perricone et al. [88] first revealed that adjuvant stimuli, such as aluminum and tetramethylpentadecane, could provoke autoimmunity. For instance, aluminum hydroxide was associated with postinoculation phenomena, and silicone was associated with silicosis. In the cohort of patients with relapsed GD after COVID-19 vaccination, a 44-year-old female (Case 15) stood out. With a medical history of GD spanning 13 years, she was administered the first dose of COVID-19 inactivated vaccine on June 10, 2021. A mere week later, symptoms such as hyperhidrosis, palpitations, and fatigue manifested. Subsequently, she was diagnosed with relapsed GD based on laboratory and imaging tests [34]. Given that the inactivated vaccine employs aluminum hydroxide as the adjuvant [89], her GD relapse might be attributed to ASIA triggered by adjuvant-induced enhancement of immune response. However, Perricone et al. [88] suggested that adjuvant-induced autoimmunity could involve multiple mechanisms, including genetic predisposition. Emerging as one of the most promising vaccine types, the mRNA vaccine has been proven with a robust capacity to induce both cellular and humoral immunity [90,91,92]. The functionality of the mRNA vaccine necessitates its entry into the cell cytoplasm. In this context, Lipid Nanoparticles (LNPs) play an indispensable role as carriers, encapsulating mRNA molecules and facilitating their targeted delivery to specific cells for subsequent action [93]. Animal experiments by Alameh et al. [92] indicated that LNPs could enhance the responses of follicular helper T cells and germinal center B cells, suggesting the potential contribution of LNPs as adjuvants to ASIA syndrome. Furthermore, polyethylene glycol (PEG), a lipid adjuvant in COVID-19 mRNA vaccines, can stabilize LNPs, and PEG exposure may also provoke an amplified immune response leading to thyroid autoimmunity [40]. PEG reactions have been reported, but this condition is exceedingly rare [94]. Despite these insights, the related mechanisms remain unclear, and await large-scale clinical epidemiological studies and systematic experiments to clarify the relationship between the development of GD and COVID-19 vaccination.
Limitations
We must acknowledge the limitations of our study. Firstly, due to the limited number of existing papers and clinical cases, our results may not fully represent all instances of GD that could potentially appear after COVID-19 vaccination. Secondly, there are variations in the number of individuals receiving different types of COVID-19 vaccines across different regions, which may lead to an overestimation of GD risks associated with certain types of COVID-19 vaccines. Lastly, the proposed pathogenic mechanisms presented in this review are merely attempts to describe the progression of this immune event. Due to a lack of systematic experimental studies, we cannot establish a clear causal relationship between COVID-19 vaccination and the onset of GD. Despite these limitations, our study still provides preliminary information on GD following COVID-19 vaccination, laying a foundation for further research.
Conclusion
In summary, the COVID-19 vaccination may promote the onset of GD through pathogenic mechanisms such as cross-immune responses triggered by molecular mimicry and ASIA caused by LNPs with adjuvant activity. However, due to the limited number of observed GD cases following COVID-19 vaccination and the lack of systematic experimental studies, a causal relationship between COVID-19 vaccination and the onset of GD could not be definitively confirmed yet. When compared to the total vaccinated population, the occurrence rates of new-onset and relapsed GD after COVID-19 vaccination were extremely low, and most of those GD patients following COVID-19 vaccination experienced positive outcomes after treatment. Therefore, the extensive benefits of COVID-19 vaccination significantly outweigh mild risks such as treatable GD. For patients who have developed GD following the first dose, and those with a history of GD, the COVID-19 vaccine should be actively administered once their conditions are stabilized after treatment. It should be reminded to immediately seek medical attention and have thyroid functions monitored if symptoms of hyperthyroidism develop after COVID-19 vaccination. Treatment regimen may be adjusted as necessary. Currently, clinical epidemiological studies with large sample sizes and systematic experimental studies are needed to elucidate the correlation between COVID-19 vaccination and GD occurrence, and the underlying pathogenic mechanisms.
Availability of data and materials
Not applicable.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- GD:
-
Graves' disease
- fT4:
-
Free thyroxine
- fT3:
-
Free triiodothyronine
- TSH:
-
Thyroid-stimulating hormone
- TRAb:
-
Thyrotropin receptor antibody
- TSI:
-
Thyroid-stimulating immunoglobulin
- TPOAb:
-
Thyroid peroxidase antibodies
- TgAb:
-
Thyroglobulin antibodies
- TFTs:
-
Thyroid function tests
- T4:
-
Thyroxine
- T3:
-
Triiodo thyronine
- ATD:
-
Antithyroid drug
- TED:
-
Thyroid eye disease
- ASIA:
-
Autoimmune/inflammatory syndrome induced by adjuvants
- LNPs:
-
Lipid nanoparticles
- PEG:
-
Polyethylene glycol
- HLA:
-
Human leukocyte antigen
- F:
-
Female
- M:
-
Male
References
Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19(3):141–54. https://doi.org/10.1038/s41579-020-00459-7.
World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/. Accessed 7 June 2023.
Upadhya S, Rehman J, Malik AB, Chen S. Mechanisms of lung injury induced by SARS-CoV-2 infection. Physiology (Bethesda). 2022;37(2):88–100. https://doi.org/10.1152/physiol.00033.2021.
Wang F, Kream RM, Stefano GB. Long-term respiratory and neurological sequelae of COVID-19. Med Sci Monit. 2020;26:e928996. https://doi.org/10.12659/MSM.928996.
Pal R, Banerjee M. COVID-19 and the endocrine system: exploring the unexplored. J Endocrinol Invest. 2020;43(7):1027–31. https://doi.org/10.1007/s40618-020-01276-8.
Rhee EJ, Kim JH, Moon SJ, Lee WY. Encountering COVID-19 as endocrinologists. Endocrinol Metab (Seoul). 2020;35(2):197–205. https://doi.org/10.3803/EnM.2020.35.2.197.
Lanzolla G, Marcocci C, Marino M. Graves’ disease and Graves’ orbitopathy following COVID-19. J Endocrinol Invest. 2021;44(9):2011–2. https://doi.org/10.1007/s40618-021-01576-7.
Brancatella A, Ricci D, Viola N, Sgro D, Santini F, Latrofa F. Subacute thyroiditis after sars-COV-2 infection. J Clin Endocrinol Metab. 2020;105(7):dgaa276. https://doi.org/10.1210/clinem/dgaa276.
Seyed Resuli A, Bezgal M. Subacute thyroiditis in COVID-19 patients. Ear Nose Throat J. 2022;101(8):501–5. https://doi.org/10.1177/01455613211012114.
Alshamam MS, Nso N, Idrees Z, Iqbal S, Ghernautan V, Sumbly V, et al. New-onset diabetes in the setting of beta-cell dysfunction in a young patient with COVID-19 infection. Cureus. 2021;13(7):16497. https://doi.org/10.7759/cureus.16497.
Yang JK, Zhao MM, Jin JM, Liu S, Bai P, He W, et al. New-onset COVID-19-related diabetes: an early indicator of multi-organ injury and mortally of SARS-CoV-2 infection. Curr Med (Cham). 2022;1(1):6. https://doi.org/10.1007/s44194-022-00006-x.
Mateu-Salat M, Urgell E, Chico A. SARS-COV-2 as a trigger for autoimmune disease: report of two cases of Graves’ disease after COVID-19. J Endocrinol Invest. 2020;43(10):1527–8. https://doi.org/10.1007/s40618-020-01366-7.
Ghareebian H, Mariash C. COVID-19-induced Graves’ disease. Cureus. 2022;14(2):e22260.
de la Higuera L-F, Perdomo CM, Galofre JC. Subacute thyroiditis following COVID-19 infection. Rev Clin Esp (Barc). 2021;221(6):370–2. https://doi.org/10.1016/j.rceng.2021.01.002.
Zheng C, Shao W, Chen X, Zhang B, Wang G, Zhang W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int J Infect Dis. 2022;114:252–60. https://doi.org/10.1016/j.ijid.2021.11.009.
Our World in Data. Coronavirus (COVID-19) Vaccinations. https://ourworldindata.org/covid-vaccinations. Accessed 7 June 2023.
Meo SA, Bukhari IA, Akram J, Meo AS, Klonoff DC. COVID-19 vaccines: comparison of biological, pharmacological characteristics and adverse effects of Pfizer/BioNTech and Moderna Vaccines. Eur Rev Med Pharmacol Sci. 2021;25(3):1663–9. https://doi.org/10.26355/eurrev_202102_24877.
Al Khames Aga QA, Alkhaffaf WH, Hatem TH, Nassir KF, Batineh Y, Dahham AT, et al. Safety of COVID-19 vaccines. J Med Virol. 2021;93(12):6588–94. https://doi.org/10.1002/jmv.27214.
Montgomery J, Ryan M, Engler R, Hoffman D, McClenathan B, Collins L, et al. Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol. 2021;6(10):1202–6. https://doi.org/10.1001/jamacardio.2021.2833.
Arepally GM, Ortel TL. Vaccine-induced immune thrombotic thrombocytopenia: what we know and do not know. Blood. 2021;138(4):293–8. https://doi.org/10.1182/blood.2021012152.
Elrashdy F, Tambuwala MM, Hassan SS, Adadi P, Seyran M, Abd El-Aziz TM, et al. Autoimmunity roots of the thrombotic events after COVID-19 vaccination. Autoimmun Rev. 2021;20(11):102941. https://doi.org/10.1016/j.autrev.2021.102941.
Badier L, Toledano A, Porel T, Dumond S, Jouglen J, Sailler L, et al. IgA vasculitis in adult patient following vaccination by ChadOx1 nCoV-19. Autoimmun Rev. 2021;20(11):102951. https://doi.org/10.1016/j.autrev.2021.102951.
De Leo S, Lee SY, Braverman LE. Hyperthyroidism. Lancet. 2016;388(10047):906–18. https://doi.org/10.1016/S0140-6736(16)00278-6.
Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American thyroid association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016;26(10):1343–421. https://doi.org/10.1089/thy.2016.0229.
D’Aurizio F. The role of laboratory medicine in the diagnosis of the hyperthyroidism. Q J Nucl Med Mol Imag. 2021;65(2):91–101. https://doi.org/10.23736/S1824-4785.21.03344-6.
McIver B, Morris JC. The pathogenesis of Graves’ disease. Endocrinol Metab Clin North Am. 1998;27(1):73–89. https://doi.org/10.1016/s0889-8529(05)70299-1.
Shukla SK, Singh G, Ahmad S, Pant P. Infections, genetic and environmental factors in pathogenesis of autoimmune thyroid diseases. Microb Pathog. 2018;116:279–88. https://doi.org/10.1016/j.micpath.2018.01.004.
Zhou F, Wang X, Wang L, Sun X, Tan G, Wei W, et al. Genetics, epigenetics, cellular immunology, and gut microbiota: emerging links with Graves’ disease. Front Cell Dev Biol. 2021;9:794912. https://doi.org/10.3389/fcell.2021.794912.
Razmara E, Salehi M, Aslani S, Bitaraf A, Yousefi H, Colon JR, et al. Graves’ disease: introducing new genetic and epigenetic contributors. J Mol Endocrinol. 2021;66(2):R33–55. https://doi.org/10.1530/JME-20-0078.
Antonelli A, Ferrari SM, Ragusa F, Elia G, Paparo SR, Ruffilli I, et al. Graves’ disease: epidemiology, genetic and environmental risk factors and viruses. Best Pract Res Clin Endocrinol Metab. 2020;34(1):101387. https://doi.org/10.1016/j.beem.2020.101387.
Davies TF, Andersen S, Latif R, Nagayama Y, Barbesino G, Brito M, et al. Graves’ disease. Nat Rev Dis Primers. 2020;6(1):52. https://doi.org/10.1038/s41572-020-0184-y.
Pla Peris B, Merchante Alfaro AA, Maravall Royo FJ, Abellan Galiana P, Perez Naranjo S, Gonzalez BM. Thyrotoxicosis following SARS-COV-2 vaccination: a case series and discussion. J Endocrinol Invest. 2022;45(5):1071–7. https://doi.org/10.1007/s40618-022-01739-0.
Oguz SH, Sendur SN, Iremli BG, Gurlek A, Erbas T, Unluturk U. SARS-CoV-2 vaccine-induced thyroiditis: safety of revaccinations and clinical follow-up. J Clin Endocrinol Metab. 2022;107(5):e1823–34. https://doi.org/10.1210/clinem/dgac049.
Bostan H, Ucan B, Kizilgul M, Calapkulu M, Hepsen S, Gul U, et al. Relapsed and newly diagnosed Graves’ disease due to immunization against COVID-19: a case series and review of the literature. J Autoimmun. 2022;128:102809. https://doi.org/10.1016/j.jaut.2022.102809.
Chee YJ, Liew H, Hoi WH, Lee Y, Lim B, Chin HX, et al. SARS-CoV-2 mRNA vaccination and graves’ Disease: a report of 12 cases and review of the literature. J Clin Endocrinol Metab. 2022;107(6):e2324–30. https://doi.org/10.1210/clinem/dgac119.
Chua MWJ. Graves’ disease after COVID-19 vaccination. Ann Acad Med Singap. 2022;51(2):127–8. https://doi.org/10.47102/annals-acadmedsg.2021398.
Zettinig G, Krebs M. Two further cases of Graves’ disease following SARS-Cov-2 vaccination. J Endocrinol Invest. 2022;45(1):227–8. https://doi.org/10.1007/s40618-021-01650-0.
Patrizio A, Ferrari SM, Antonelli A, Fallahi P. A case of Graves’ disease and type 1 diabetes mellitus following SARS-CoV-2 vaccination. J Autoimmun. 2021;125:102738. https://doi.org/10.1016/j.jaut.2021.102738.
Weintraub MA, Ameer B, Sinha GN. Graves disease following the SARS-CoV-2 vaccine: case series. J Investig Med High Impact Case Rep. 2021;9:23247096211063356. https://doi.org/10.1177/23247096211063356.
Vera-Lastra O, Ordinola Navarro A, Cruz Domiguez MP, Medina G, Sanchez Valadez TI, Jara LJ. Two cases of Graves’ disease following SARS-CoV-2 vaccination: an autoimmune/inflammatory syndrome induced by adjuvants. Thyroid. 2021;31(9):1436–9. https://doi.org/10.1089/thy.2021.0142.
Goblirsch TJ, Paulson AE, Tashko G, Mekonnen AJ. Graves’ disease following administration of second dose of SARS-CoV-2 vaccine. BMJ Case Rep. 2021. https://doi.org/10.1136/bcr-2021-246432.
Pujol A, Gomez LA, Gallegos C, Nicolau J, Sanchis P, Gonzalez-Freire M, et al. Thyroid as a target of adjuvant autoimmunity/inflammatory syndrome due to mRNA-based SARS-CoV2 vaccination: from Graves’ disease to silent thyroiditis. J Endocrinol Invest. 2022;45(4):875–82. https://doi.org/10.1007/s40618-021-01707-0.
Lui DTW, Lee KK, Lee CH, Lee ACH, Hung IFN, Tan KCB. Development of Graves’ disease after SARS-CoV-2 mRNA vaccination: a case report and literature review. Front Public Health. 2021;9:778964. https://doi.org/10.3389/fpubh.2021.778964.
Yamamoto K, Mashiba T, Takano K, Suzuki T, Kami M, Takita M, et al. A case of exacerbation of subclinical hyperthyroidism after first administration of BNT162b2 mRNA COVID-19 vaccine. Vaccines (Basel). 2021;9(10):1108. https://doi.org/10.3390/vaccines9101108.
Sakai M, Takao K, Kato T, Ito K, Kubota S, Hirose T, et al. Graves’ disease after administration of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccine in a type 1 diabetes patient. Intern Med. 2022;61(10):1561–5. https://doi.org/10.2169/internalmedicine.
Manta R, Martin C, Muls V, Poppe KG. New-onset Graves’ disease following SARS-CoV-2 vaccination: a case report. Eur Thyroid J. 2022;11(4):e220049. https://doi.org/10.1530/ETJ-22-0049.
Bres F, Joyeux MA, Delemer B, Vitellius G, Barraud S. Three cases of thyroiditis after COVID-19 RNA-vaccine. Ann Endocrinol (Paris). 2022;83(4):262–4. https://doi.org/10.1016/j.ando.2022.04.014.
Taieb A, Sawsen N, Asma BA, Ghada S, Hamza E, Yosra H, et al. A rare case of grave’s disease after SARS-CoV-2 vaccine: is it an adjuvant effect? Eur Rev Med Pharmacol Sci. 2022;26(7):2627–30. https://doi.org/10.26355/eurrev_202204_28500.
Singh G, Howland T. Graves’ disease following COVID-19 vaccination. Cureus. 2022;14(4):e24418. https://doi.org/10.7759/cureus.24418.
Ruggeri RM, Giovanellla L, Campenni A. SARS-CoV-2 vaccine may trigger thyroid autoimmunity: real-life experience and review of the literature. J Endocrinol Invest. 2022;45(12):2283–9. https://doi.org/10.1007/s40618-022-01863-x.
Nakamura F, Awaya T, Ohira M, Enomoto Y, Moroi M, Nakamura M. Graves’ disease after mRNA COVID-19 vaccination, with the presence of autoimmune antibodies even one year later. Vaccines (Basel). 2023. https://doi.org/10.3390/vaccines11050934.
Lioulios G, Tsouchnikas I, Dimitriadis C, Giamalis P, Pella E, Christodoulou M, et al. Two cases of autoimmune thyroid disorders after COVID vaccination in dialysis patients. Int J Mol Sci. 2022;23(19):11492. https://doi.org/10.3390/ijms231911492.
Yasuda S, Suzuki S, Yanagisawa S, Morita H, Haisa A, Satomura A, et al. HLA typing of patients who developed subacute thyroiditis and Graves’ disease after SARS-CoV-2 vaccination: a case report. BMC Endocr Disord. 2023;23(1):54. https://doi.org/10.1186/s12902-023-01287-5.
Taskaldiran I, Altay FP, Bozkus Y, Iyidir OT, Nar A, Tutuncu NB. A case report of conversion from Hashimoto’s thyroiditis to Graves’ disease in type 1 diabetic patient following the COVID-19 vaccination. Endocr Metab Immune Disord Drug Targets. 2023;23(3):405–9. https://doi.org/10.2174/1871530322666220616104058.
Shih SR, Wang CY. SARS-CoV-2 vaccination related hyperthyroidism of Graves’ disease. J Formos Med Assoc. 2022;121(9):1881–2. https://doi.org/10.1016/j.jfma.2022.02.010.
Sriphrapradang C, Shantavasinkul PC. Graves’ disease following SARS-CoV-2 vaccination. Endocrine. 2021;74(3):473–4. https://doi.org/10.1007/s12020-021-02902-y.
Lee KA, Kim YJ, Jin HY. Thyrotoxicosis after COVID-19 vaccination: seven case reports and a literature review. Endocrine. 2021;74(3):470–2. https://doi.org/10.1007/s12020-021-02898-5.
Di Filippo L, Castellino L, Giustina A. Occurrence and response to treatment of Graves’ disease after COVID vaccination in two male patients. Endocrine. 2022;75(1):19–21. https://doi.org/10.1007/s12020-021-02919-3.
Raven LM, McCormack AI, Greenfield JR, et al. Three cases of subacute thyroiditis following SARS-CoV-2 vaccine. J Clin Endocrinol Metab. 2022;107(4):e1767–8. https://doi.org/10.1210/clinem/dgab822.
Chaudhary S, Dogra V, Walia R. Four cases of Graves’ disease following viral vector severe acute respiratory syndrome corona virus-2 (SARS-CoV-2) vaccine. Endocr J. 2022;69(12):1431–5. https://doi.org/10.1507/endocrj.EJ22-0208.
Cuenca D, Aguilar-Soto M, Mercado M. A case of Graves’ disease following vaccination with the Oxford-AstraZeneca SARS-CoV-2 vaccine: case report and review of the literature. Eur J Case Rep Intern Med. 2022;9(4):003275. https://doi.org/10.12890/2022_003275.
Pierman G, Delgrange E, Jonas C. Recurrence of Graves’ disease (a Th1-type Cytokine Disease) following SARS-CoV-2 mRNA vaccine administration: a simple coincidence? Eur J Case Rep Intern Med. 2021;8(9):002807. https://doi.org/10.12890/2021_002807.
Yan BC, Luo RR. Thyrotoxicosis in patients with a history of Graves’ disease after SARS-CoV-2 vaccination (adenovirus vector vaccine): two case reports. World J Clin Cases. 2023;11(5):1122–8. https://doi.org/10.12998/wjcc.v11.i5.1122.
Sriphrapradang C. Aggravation of hyperthyroidism after heterologous prime-boost immunization with inactivated and adenovirus-vectored SARS-CoV-2 vaccine in a patient with Graves’ disease. Endocrine. 2021;74(2):226–7. https://doi.org/10.1007/s12020-021-02879-8.
Filippo L, Castellino L, Allora A, Frara S, Lanzi R, Perticone F, et al. Distinct clinical features of post-COVID-19 vaccination early-onset Graves’ disease. J Clin Endocrinol Metab. 2022;108(1):107–13. https://doi.org/10.1210/clinem/dgac550.
Wiersinga WM. Graves’ disease: can it be cured? Endocrinol Metab (Seoul). 2019;34(1):29–38. https://doi.org/10.3803/EnM.2019.34.1.29.
Vejrazkova D, Vcelak J, Vaclavikova E, Vankova M, Zajickova K, Duskova M, et al. Genetic predictors of the development and recurrence of Graves’ disease. Physiol Res. 2018;67(Suppl 3):S431–9. https://doi.org/10.33549/physiolres.934018.
Struja T, Fehlberg H, Kutz A, Guebelin L, Degen C, Mueller B, et al. Can we predict relapse in Graves’ disease? Results from a systematic review and meta-analysis. Eur J Endocrinol. 2017;176(1):87–97. https://doi.org/10.1530/EJE-16-0725.
Li H, Liu SM, Yu XH, Tang SL, Tang CK. Coronavirus disease 2019 (COVID-19): current status and future perspectives. Int J Antimicrob Agents. 2020;55(5):105951. https://doi.org/10.1016/j.ijantimicag.2020.105951.
Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7(1):11. https://doi.org/10.1186/s40779-020-00240-0.
Araf Y, Faruqui NA, Anwar S, Hosen MJ. SARS-CoV-2: a new dimension to our understanding of coronaviruses. Int Microbiol. 2021;24(1):19–24. https://doi.org/10.1007/s10123-020-00152-y.
Scialo F, Daniele A, Amato F, Pastore L, Matera MG, Cazzola M, et al. ACE2: the major cell entry receptor for SARS-CoV-2. Lung. 2020;198(6):867–77. https://doi.org/10.1007/s00408-020-00408-4.
Asselah T, Durantel D, Pasmant E, Lau G, Schinazi RF. COVID-19: discovery, diagnostics and drug development. J Hepatol. 2021;74(1):168–84. https://doi.org/10.1016/j.jhep.2020.09.031.
Behera BC, Mishra RR, Thatoi H. Recent biotechnological tools for diagnosis of corona virus disease: a review. Biotechnol Prog. 2021;37(1):e3078. https://doi.org/10.1002/btpr.3078.
Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, et al. Coronavirus disease 2019-COVID-19. Clin Microbiol Rev. 2020;33(4):e00028-e120. https://doi.org/10.1128/CMR.00028-20.
Wu A, Peng Y, Huang B, Ding X, Wang X, Niu P, et al. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020;27(3):325–8. https://doi.org/10.1016/j.chom.2020.02.001.
Soraci L, Lattanzio F, Soraci G, Gambuzza ME, Pulvirenti C, Cozza A, et al. COVID-19 vaccines: current and future perspectives. Vaccines (Basel). 2022;10(4):608. https://doi.org/10.3390/vaccines10040608.
Prates ET, Garvin MR, Pavicic M, Jones P, Shah M, Demerdash O, et al. Potential pathogenicity determinants identified from structural proteomics of SARS-CoV and SARS-CoV-2. Mol Biol Evol. 2021;38(2):702–15. https://doi.org/10.1093/molbev/msaa231.
Li F, Li W, Farzan M, Harrison SC. Structure of SARS coronavirus spike receptor-binding domain complexed with receptor. Science. 2005;309(5742):1864–8. https://doi.org/10.1126/science.1116480.
Walls AC, Xiong X, Park YJ, Tortorici MA, Snijder J, Quispe J, et al. Unexpected receptor functional mimicry elucidates activation of coronavirus fusion. Cell. 2019;176(5):1026-39.e15. https://doi.org/10.1016/j.cell.2018.12.028.
Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–3.
Li F. Structure, function, and evolution of coronavirus spike proteins. Annu Rev Virol. 2016;3(1):237–61. https://doi.org/10.1126/science.abb2507.
Dai L, Gao GF. Viral targets for vaccines against COVID-19. Nat Rev Immunol. 2021;21(2):73–82. https://doi.org/10.1038/s41577-020-00480-0.
Vojdani A, Vojdani E, Kharrazian D. Reaction of human monoclonal antibodies to SARS-CoV-2 proteins with tissue antigens: implications for autoimmune diseases. Front Immunol. 2020;11:617089. https://doi.org/10.3389/fimmu.2020.617089.
Patrizio A, Ferrari SM, Elia G, Ragusa F, Paparo SR, Mazzi V, et al. Graves’ disease following SARS-CoV-2 vaccination: a systematic review. Vaccines (Basel). 2022;10(9):1445. https://doi.org/10.3390/vaccines10091445.
Shoenfeld Y, Agmon-Levin N. “ASIA” - autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun. 2011;36(1):4–8. https://doi.org/10.1016/j.jaut.2010.07.003.
Esposito S, Prada E, Mastrolia MV, Tarantino G, Codeca C, Rigante D. Autoimmune/inflammatory syndrome induced by adjuvants (ASIA): clues and pitfalls in the Pediatric background. Immunol Res. 2014;60(2–3):366–75. https://doi.org/10.1007/s12026-014-8586-0.
Perricone C, Colafrancesco S, Mazor RD, Soriano A, Agmon-Levin N, Shoenfeld Y. Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) 2013: unveiling the pathogenic, clinical and diagnostic aspects. J Autoimmun. 2013;47:1–16. https://doi.org/10.1016/j.jaut.2013.10.004.
Palacios R, Patino EG, de Oliveira PR, Conde M, Batista AP, Zeng G, et al. Double-blind, randomized, placebo-controlled phase III clinical trial to evaluate the efficacy and safety of treating healthcare professionals with the adsorbed COVID-19 (Inactivated) vaccine manufactured by Sinovac—PROFISCOV: a structured summary of a study protocol for a randomised controlled trial. Trials. 2020;21(1):853. https://doi.org/10.1186/s13063-020-04775-4.
Laczko D, Hogan MJ, Toulmin SA, Hicks P, Lederer K, Gaudette BT, et al. A single immunization with nucleoside-modified mRNA vaccines elicits strong cellular and humoral immune responses against SARS-CoV-2 in Mice. Immunity. 2020;53(4):724-32e7. https://doi.org/10.1016/j.immuni.2020.07.019.
Jackson LA, Anderson EJ, Rouphael NG, Roberts PC, Makhene M, Coler RN, et al. An mRNA vaccine against SARS-CoV-2—preliminary report. N Engl J Med. 2020;383(20):1920–31. https://doi.org/10.1056/NEJMoa2022483.
Alameh MG, Tombacz I, Bettini E, Lederer K, Sittplangkoon C, Wilmore JR, et al. Lipid nanoparticles enhance the efficacy of mRNA and protein subunit vaccines by inducing robust T follicular helper cell and humoral responses. Immunity. 2021;54(12):2877-92.e7. https://doi.org/10.1016/j.immuni.2021.11.001.
Kon E, Elia U, Peer D. Principles for designing an optimal mRNA lipid nanoparticle vaccine. Curr Opin Biotechnol. 2022;73:329–36. https://doi.org/10.1016/j.copbio.2021.09.016.
Garvey LH, Nasser S. Anaphylaxis to the first COVID-19 vaccine: is polyethylene glycol (PEG) the culprit? Br J Anaesth. 2021;126(3):e106–8. https://doi.org/10.1016/j.bja.2020.12.020.
Acknowledgements
The authors gratefully acknowledge the support of the First Hospital of China Medical University.
Funding
This study was supported by the National Nature Science Foundation of China (grant number No.81771741) and the Distinguished Professor at Educational Department of Liaoning Province (Grant Number No. [2014] 187).
Author information
Authors and Affiliations
Contributions
KC, YG and JL designed the study. KC and JL collected the data. KC drafted the manuscript. KC, YG and JL interpreted the data and revised the article critically for important intellectual content. JL approved the final version of the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, K., Gao, Y. & Li, J. New-onset and relapsed Graves’ disease following COVID-19 vaccination: a comprehensive review of reported cases. Eur J Med Res 28, 232 (2023). https://doi.org/10.1186/s40001-023-01210-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01210-7