Abstract
Introduction
This study is to examine the predictors of survival and to construct a nomogram for predicting the overall survival (OS) of primary bladder signet ring cell carcinoma (SRCC) patients based on the analysis of the Surveillance, Epidemiology, and End Results (SEER) database.
Methods
A total of 219 eligible patients diagnosed with SRCC were analyzed using the 2004–2015 data from SEER database. Univariate and multivariate Cox regression were used to determine independent prognostic factors, followed by development of a nomogram based on the multivariate Cox regression models. The consistency index (C-index), receiver operating characteristic (ROC) curve, and calibration curve were used to validate the prognostic nomogram.
Results
The nomograms indicated appreciable accuracy in predicting the OS, with C-index of 0.771 and 0.715, respectively. The area under the curve (AUC) of the nomogram was 0.713 for 1 year, 0.742 for 3 years, and 0.776 for 5 years in the training set, while was 0.730 for 1 year, 0.727 for 3 years, and 0.697 for 5 years in the validation set. The calibration curves revealed satisfactory consistency between the prediction of deviation correction and ideal reference line.
Conclusions
The prognostic nomogram developed in the analytical data of SEER it provided high accuracy and reliability in predicting the survival outcomes of primary bladder SRCC patients and could be used to comprehensively assess the risk of SRCC. Moreover, they could enable clinicians to make more precise treatment decisions for primary bladder SRCC patients.
Similar content being viewed by others
Introduction
Bladder cancer (BCa) is the second most diagnosed malignant carcinoma of the genitourinary tract, being the 10th tumor for incidence when considering both sexes, and the 7th considering only the men population [1]. The most common type of BCa is urothelial carcinoma, which occurs in 90% of all cases. Most BCas can be diagnosed at an early stage. Although 75% are non-muscle-invasive tumors at first diagnosis, approximately 78% of patients relapse within 5 years. Patients with the same pathologic type of BCa and clinical stage could have different prognoses.
Signet ring cell carcinoma (SRCC), classified as subtypes of adenocarcinoma, most commonly occurs in the stomach and colon. Primary bladder SRCC is a rare type of bladder cancer, accounting for approximately <1% of cases, with a high mortality rate [2, 3]. Because of its rarity, it is impossible to fully comprehensively its clinicopathological features, prognosis and histogenesis [4, 5].
In this regard, although numerous steps in the past have been taken in the management of this pathology, still little knowledge we have of the characteristics that influence its prognosis. Continuing to investigate them is the first step to do to develop new strategies for a more efficacy BCa treatment and management.
A standardized treatment for primary bladder SRCC has not been established and surgery is generally considered the most predominant treatment method, but the optimal surgical approach and whether radiotherapy or chemotherapy cannot be determined by consensus. Primary bladder SRCC may often overlooked by patients and clinicians as its low frequency.
TNM staging system is used by the American Joint Committee on Cancer (AJCC) to predict prognosis and guide treatment in BCa; however, it is not specially designed for SRCC. Ferro et al. [6] found that neutrophil percentage-to-albumin ratio could predict both overall survival (OS) and cancer-specific survival (CSS). They indicated that patients, treated with neoadjuvant chemotherapy and radical cystectomy, with high neutrophil percentage-to-albumin ratio had a longer OS and CSS than low neutrophil percentage-to-albumin ratio. However, many individualized characteristics, such as histologic grade, tumor size, lymph node metastasis, surgery, lymph nodes removed, chemotherapy and radiotherapy, that may be predictive are not involved [5, 7]. Nomograms can present simple statistical analysis and visualization results, which can help physicians make better clinical decisions and to promote personalized medical therapy. Unfortunately, there is no consensus prognostic model for primary bladder SRCC.
Prognostic nomograms are currently used widely in oncologic medicine as prognostic devices. Because the knowledge of the prognosis of primary bladder SRCC is essential for pretherapeutic assessment the aim of the current study was to describe the frequency of occurrence based on the SEER database. Another aim of the study was to construct a nomogram to predict OS in de novo diagnosed primary bladder SRCC patients. The study may also help to choose suitable management strategies by increasing the understanding of prognosis in newly diagnosed primary bladder SRCC patients.
Methods
Patients and variables
Around 28% of the US population has cancer incidence in the SEER database that includes 18 cancer registries. The SEER * Stat software (version 8.4.0.1) was used to identify all primary SRCC of the bladder cases reported in the SEER database from 2004 to 2015. We collected the following data: (1) primary bladder SRCC patients; (2) the diagnosis of SRCC was based on the ICD-O-3; coded as 8490/3; (3) confirmed by positive histology and diagnosed by first or only cancer. Those who did not have a histological diagnosis or lacked survival information were excluded.
Patient demographics analyzed included sex, age, race, marital status, and year of diagnosis. Tumor characteristics studied included tumor size, primary site, AJCC T stage, N stage, M stage, and histologic grade. Information on distant metastasis sites only became available after 2010, so the metastasis information was included from 2010 to 2015. Treatment characteristics included surgery, lymph nodes removed, radiation, chemotherapy, and the sequence of surgery between radiation. OS was the main endpoint. A patient‘s OS is defined as the period from the time of first diagnosis to his death or last follow-up.
Statistical analyses
In the ratio of 1:1, all included samples were randomly split into the training and validation sets. The categorical data were presented as frequency (percentage), and the chi-square test was used to compare groups.
Based on multivariate Cox proportional hazard analysis, we constructed nomograms using the factors with P < 0.05. Multivariate analysis using the Cox proportional hazards model enabled the identification of baseline and clinical variables associated with OS time. The Kaplan–Meier survival curves were plotted and compared by log-rank test.
Last but not least, we considered variables with a P value of less than 0.05 as independent predictors in the multivariate Cox model and incorporated them into the nomogram model. In addition, both the training and validation sets were validated using the consistency index (C-index), receiver operating characteristic (ROC) curve, and calibration curve. And also to calibrate the prediction capacity of the nomogram for 1-, 3- and 5-year OS. Those who had a C-index and an area under the curve (AUC) of > 0.65 were considered as having an acceptable fit. R software (www.rproject.org) and SPSS software program (version 25.0) were used for statistical analysis. Statistical significance was determined by P values < 0.05 (P < 0.05).
The study was conducted in accordance with the Helsinki Declaration (revised in 2013). Because cancer is a reportable disease in every state of the US, it is not required that informed patient consent be obtained for the release of data from the SEER database.
Results
Baseline characteristics of the overall, training and validation sets
Table 1 presents the demographic and clinicopathological characteristics of 219 patients.
Prognostic factor analysis
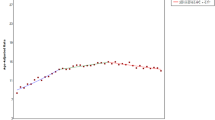
In this study, univariate analyses confirmed that risk factors of bladder SRCC include sex, race, marital status, tumor size, T stage, N stage, M stage, surgery, lymph node removed, and radiation. However, multivariate analyses showed independent risk factors only include race (Unknown vs. White, HR = 59.085, 95% CI = 2.638 ~ 913.422, P = 0.009), marital status(SDW vs. Single, HR = 2.878, 95% CI = 1.296 ~ 6.391, P = 0.009), T stage (T2 vs. T1, HR = 2.710, 95% CI = 1.127 ~ 6.518, P = 0.026; T3 vs. T1, HR = 6.124, 95% CI = 1.881 ~ 19.924, P = 0.003; and T4 vs. T1, HR = 4.141, 95% CI = 1.534 ~ 11.252, P = 0.005), N stage (N2 vs. N0, HR = 4.461, 95% CI = 2.016 ~ 9.873, P < 0.001), M stage (M1 vs. M0, HR = 2.400, 95% CI = 1.156 ~ 4.983, P = 0.019), surgery (Pelvic exenteration vs. None, HR = 0.223, 95% CI = 0.069 ~ 0.726, P < 0.012; and Others vs. None, HR = 0.194, 95% CI = 0.064 ~ 0.591, P = 0.004), and lymph node removed (4 or more regional vs. None, HR = 0.299, 95% CI = 0.127 ~ 0.703, P = 0.006; and Unknown vs. None, HR = 0.120, 95% CI = 0.023 ~ 0.627, P = 0.012) (Table 2). The Kaplan–Meier survival curves shown in Fig. 1 show the OS of the training set patient population by subgroups of sex, tumor size, surgery, lymph nodes removed, and radiation (Fig. 1a–e). The median OS was only 14 months. The median OS, respectively, were 4, 10, 24, 17, and 22 months for none, transurethral resection of the bladder (TURB), complete cystectomy with reconstruction, pelvic exenteration and others surgery (P < 0.001). The none lymph nodes removed, 1 to 3 regional, 4 or more regional, and unknown were 10, 26, 21 and 12 months, respectively (P = 0.004). Figure 1f shows that, compared with high-risk patients, low-risk patients tended to have a better OS (P < 0.001).
Development and validations of predicting nomograms for OS
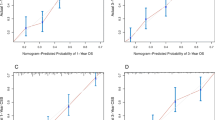
Based on the significant risk factors, the nomogram for predicting 1-, 2- and 3-year OS was developed using Cox multivariate analysis (Fig. 2). The C-index and ROC curves were compared to determine, whether the survival months predicted by the nomograms were in accordance with the actual survival times. The C-index of the nomogram OS was 0.771 and 0.715 in the training and validation sets, respectively. The ROC curve estimation of the nomogram in the training set also showed acceptable accuracy, with a 1-, 3-, and 5-year AUC of 0.713, 0.742 and 0.776, respectively (Fig. 3a–c). In addition, the validation set were 0.730, 0.727 and 0.697, respectively (Fig. 4a–c). These results indicated that the model we constructed was relatively accurate.
More importantly, we calibrated the 1-, 3-, and 5-year OS nomogram in both the training and validation sets. The calibration plots showed that the nomogram had a favorable predictive accuracy in both the training set (Fig. 5a–c) and validation set (Fig. 6a–c). This result indicated good agreement between the nomogram predictions and the observed results in the training and validation sets.
Discussion
The primary bladder SRCC is a rare form of bladder cancer, with an incidence rate of less than 0.6% [8, 9]. It was less commonly reported, since the first patient was reported by Saphir [10]. Due to the rarity of bladder SRCC, most reports were case reports or reviews of previous cases [4, 11, 12].
The present study showed that lymph node metastasis did not occur in 58.0% overall patients and distant metastasis did not occur in 73.1% overall patients. The bladder SRCC had a lower rate of lymph node metastases and distant metastases, but their prognoses were worse. As previously described, SRCC presents a higher histological grade rate and advanced stage disease, which could induce a poor prognosis [5, 13, 14]. According to the literature reported, the survival rate of bladder SRCC was lower than urothelial carcinoma, and the natural duration of the disease was 3.5 months [4]. A Japanese study, reported by Dadhania et al. [15] also demonstrated that almost half of the bladder SRCC patients were already at AJCC stage IV at the time of diagnosis, and the median survival time was approximately 8 months. Besides, the surviving period of time did not exceed 2 years. In the analytical data of SEER it showed, the median survival was 13, 14, and 12 months, respectively, for oveall, training and validation sets.
As for the prognostic factors of bladder SRCC, clinical study results were inconsistent.
Multiple studies, compared with bladder SRCC and urothelial carcinoma, have shown that histological type, cystectomy, marital status, histological grade, year of diagnosis and sex have been identified as prognostic factors. In addition, SRCC, histological type, is an independent risk factor for Bca. [4, 14]. Wang et al. [13] suggested that patient characteristics such as age, marital status, AJCC stage, and cystectomy were independent predictors of survival for bladder SRCC patients. In this study, univariate analyses confirmed that risk factors of bladder SRCC include sex (Male vs. Female, HR = 0.536, 95% CI = 0.348 ~ 0.825, P = 0.005), race (Unknown vs. White, HR = 66.305, 95% CI = 6.556 ~ 670.578, P < 0.001), marital status (SDW vs. Single, HR = 3.416, 95% CI = 1.709 ~ 6.830, P < 0.001), tumor size (≥ 4.0 cm vs. < 4.0 cm, HR = 2.437, 95% CI = 1.326 ~ 4.478, P = 0.004; and Unknown vs. < 4.0 cm, HR = 2.058, 95% CI = 1.215 ~ 3.486, P = 0.007), T stage (T3 vs. T1, HR = 2.486, 95% CI = 1.186 ~ 5.212, P = 0.015; T4 vs. T1, HR = 2.569, 95% CI = 1.307 ~ 5.049, P = 0.006; and TX vs. T1, HR = 3.263, 95% CI = 1.209 ~ 8.805, P = 0.020), N stage (N2 vs. N0, HR = 2.247, 95% CI = 1.309 ~ 3.859, P = 0.003), M stage (M1 vs. M0, HR = 3.898, 95% CI = 2.355 ~ 6.452, P < 0.001), surgery (TURB vs. None, HR = 0.498, 95% CI = 0.256 ~ 0.972, P = 0.040; Complete cystectomy + reconstruction vs. None, HR = 0.275, 95% CI = 0.131 ~ 0.579, P < 0.001; Pelvic exenteration vs. None, HR = 0.371, 95% CI = 0.178 ~ 0.777, P = 0.008; and Others vs. None, HR = 0.349, 95% CI = 0.160 ~ 0.762, P = 0.008), lymph nodes removed (4 or more regional vs. None, HR = 0.540, 95% CI = 0.345 ~ 0.867, P = 0.007), and radiation (Yes vs. None/Unknown, HR = 1.773, 95% CI = 1.024 ~ 3.070, P = 0.041). However, multivariate analyses showed independent risk factors only include race (Unknown vs. White, HR = 59.085, 95% CI = 2.638 ~ 913.422, P = 0.009), marital status(SDW vs. Single, HR = 2.878, 95% CI = 1.296 ~ 6.391, P = 0.009), T stage (T2 vs. T1, HR = 2.710, 95% CI = 1.127 ~ 6.518, P = 0.026; T3 vs. T1, HR = 6.124, 95% CI = 1.881 ~ 19.924, P = 0.003; and T4 vs. T1, HR = 4.141, 95% CI = 1.534 ~ 11.252, P = 0.005), N stage (N2 vs. N0, HR = 4.461, 95% CI = 2.016 ~ 9.873, P < 0.001), M stage (M1 vs. M0, HR = 2.400, 95% CI = 1.156 ~ 4.983, P = 0.019), surgery (Pelvic exenteration vs. None, HR = 0.223, 95% CI = 0.069 ~ 0.726, P < 0.012; and Others vs. None, HR = 0.194, 95% CI = 0.064 ~ 0.591, P = 0.004), and lymph node removed (4 or more regional vs. None, HR = 0.299, 95% CI = 0.127 ~ 0.703, P = 0.006; and Unknown vs. None, HR = 0.120, 95% CI = 0.023 ~ 0.627, P = 0.012) (Table 2). Data from our study and a previous studies proved that marital status and surgery were independent risk factors for bladder SRCC. However, our study did not show age, sex, and histological grade et. are prognostic factors.
Our study suggests that race, marital status, T stage, N stage, M stage, surgery, and lymph node removed were independent prognostic factors for OS in bladder SRCC patients. Using the nomogram we developed and validated, we were able to predict the 1-, 3-, and 5-year OS for bladder SRCC patients with good discrimination and high accuracy. Notably, radiation and chemotherapy were not significantly associated with the OS and were not present in the nomograms.
However, due to the rarity of the bladder SRCC and the lack of randomized clinical trials, there are no accepted guidelines for treating it. The most common surgery for bladder SRCC was TURB (62, 28.3%), and followed by radical cystectomy with reconstruction (49, 22.4%) in overall set. Due to infiltrative pattern of growth and early propensity of metastasis, nevertheless, certain scholars [16, 17] reported that TURB and partial cystectomy carry the risk of tumor recurrence. Therefore, radical cystectomy appears to be the treatment of first choice [18,19,20]. A recent systematic review concluded that all muscle invasive BCa patients, which accompanied with histological variants, including SRCC, should perform radical cystectomy [7]. Meanwhile, Guo et al. found that radical cystectomy with lymphadenectomy was associated with improved OS in SRCC patients when compared with radical cystectomy alone [21]. Recently, 70% patients were reportedly treated with surgery [22]. The number of patients with surgery (188, 85.8%) in the overall set was higher than the above values, suggesting that clinicians already have more knowledge of this disease and have attracted increasing attention for surgery. Some Scholars have suggested that bladder SRCC patients would benefit from adjuvant chemotherapy [23, 24]. However, our result shows that bladder SRCC can not benefit from postoperative adjuvant chemotherapy. The neoadjuvant nature of chemotherapy has some benefits: delivering effective systemic therapy for micrometastases; improvement of direct drug delivery into the bladder and to surrounding lymphatic vessels and lymph nodes; and improves the performance status of naive patients undergoing major surgery [25]. It can be downgrade of disease and an overall improved prognosis. However, a high-grade toxicity in more than one patient out of three, without a significant OS improvement in this patients. Therefore, the selection of patients that could benefit from neoadjuvant chemotherapy avoiding toxicity is a challenge for the future [26]. Recently, immunity checkpoint inhibitors have been introduced as an alternative treatment option for bladder SRCC patients [27]. The molecular biology represents the key to reveal the possible Achilles’ heel in BC as well as identifying novel targets. A consensus, identified 6 consensus muscle invasive bladder cancer: Luminal-papillary (LumP), Luminal-Unstable (LumU), Luminal-non-Specified (LumNS), Basal/Squamous (Ba/Sq), Stromarich, and Neuroendocrine-like (NE-like), was published in 2020 in the European Urology Journal [28]. In several phase II trials, immunotherapy was shown to be a valuable strategy for neoadjuvant therapy, especially for patients who were unable to receive cisplatin [29].
In summary, further multicenter clinical trial should be conducted to treatment bladder SRCC. Most importantly, our clinical prognostic model was innovative, rational and clinically feasible, which could be an accessible prognosis tool in clinical practice.
Several limitations are noteworthy. The first was that it was retrospective. In addition, there is little detailed information on chemotherapy drugs. Finally, The predictive accuracy of the nomogram for OS needed to be validated by external cohorts.
Conclusions
Our study shows that race, marital status, T stage, N stage, M stage, surgery and lymph node removed were independent predictive factors of OS in bladder SRCC patients. We established a nomogram based on the above parametric, and identified the high accuracy and reliability in estimating the survival of individual patients. Thus, the nomogram could be an accessible prognosis tool in clinical practice and provide personalized treatment plans.
Availability of data and materials
The data sets generated and/or analyzed during the current study are available in the SEER repository, https://seer.cancer.gov/.
Abbreviations
- SRCC:
-
Signet ring cell carcinoma
- C-index:
-
Consistency index
- AUC:
-
Area under the curve
- OS:
-
Overall survival
- CSS:
-
Cancer-specific survival
- BCa:
-
Bladder cancer
- US:
-
United States
- ROC:
-
Receiver operating characteristic
- TRUB:
-
Transurethral resection of the bladder
- SEER:
-
Surveillance, epidemiology, and end results
- AJCC:
-
The American joint committee on cancer
- HR:
-
Hazard ratio
- CI:
-
Confdence interval
- SDW:
-
Divorced + Separated + Widowed + Unmarried or Domestic Partner
- PE:
-
Pelvic exenteration
References
Grignon DJ, Ro JY, Ayala AG, Johnson DE. Primary signet-ring cell carcinoma of the urinary bladder. Am J Clin Pathol. 1991;95(1):13–20. https://doi.org/10.1093/ajcp/95.1.13.
Akamatsu S, Takahashi A, Ito M, Ogura K. Primary signet-ring cell carcinoma of the urinary bladder. Urology. 2010;75(3):615–8. https://doi.org/10.1016/j.urology.2009.06.065.
Lendorf ME, Dohn LHR, Dunga BÁ, Loya AC, Pappot H. An updated review on primary signet-ring cell carcinoma of the urinary bladder and report of a case. Scand J Urol. 2018;52(2):87–93. https://doi.org/10.1080/21681805.2017.1418020.
Jin D, Qiu S, Jin K, Zhou X, Cao Q, Yang L, et al. Signet-ring cell carcinoma as an independent prognostic factor for patients with urinary bladder cancer: a population-based study. Front Oncol. 2020;10:653. https://doi.org/10.3389/fonc.2020.00653.
Ferro M, Babă DF, de C O, et al. Neutrophil percentage-to-albumin ratio predicts mortality in bladder cancer patients treated with neoadjuvant chemotherapy followed by radical cystectomy. Future Sci OA. 2021;7(7):709. https://doi.org/10.2144/fsoa-2021-0008.
Veskimäe E, Espinos EL, Bruins HM, Yuan Y, Sylvester R, Kamat AM, et al. What is the prognostic and clinical importance of urothelial and nonurothelial histological variants of bladder cancer in predicting oncological outcomes in patients with muscle-invasive and metastatic bladder cancer? a European association of urology muscle invasive and metastatic bladder cancer guidelines panel systematic review. Eur Urol Oncol. 2019;2(6):625–42. https://doi.org/10.1016/j.euo.2019.09.003.
Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO classification of tumours of the urinary system and male genital organs-part b: prostate and bladder tumours [J]. Eur Urol. 2016;70(1):106–19. https://doi.org/10.1016/j.eururo.2016.02.028.
Holmäng S, Borghede G, Johansson SL. Primary signet ring cell carcinoma of the bladder: a report on 10 cases [J]. Scand J Urol Nephrol. 1997;31(2):145–8. https://doi.org/10.3109/00365599709070320.
Saphir O. Signet-ring cell carcinoma of the urinary bladder [J]. Am J Pathol. 1955;31(2):223–31.
Allameh F, Fallah Karkan M, Nilipour Y, Rakhshan A. Primary signet-ring cell carcinoma of the urinary bladder successfully managed with radical cystectomy in a young patient. Case Rep Urol. 2017;2017:9121078. https://doi.org/10.1155/2017/9121078.
Bouhajja L, Farah F, Garbouj N, Rammeh S. Primary signet-ring cell carcinoma of the urinary bladder: a report of two cases. Tunis Med. 2019;97:167–9.
Wang J, Wang FW. Clinical characteristics and outcomes of patients with primary signet-ring cell carcinoma of the urinary bladder. Urol Int. 2011;86:453–60. https://doi.org/10.1159/000324263.
Wang J, Wang FW, Kessinger A. The impact of signet-ring cell carcinoma histology on bladder cancer outcome. World J Urol. 2012;30:777–83. https://doi.org/10.1007/s00345-011-0718-8.
Dadhania V, Czerniak B, Guo CC. Adenocarcinoma of the urinary bladder [J]. Am J Clin Exp Urol. 2015;3(2):51–63.
Ponz M, Luzuriaga J, Robles JE, Guillén F, Urmeneta JM, Salvá A, et al. Primary signet-ring cell carcinoma of the urinary bladder (linitis plastica) [J]. Eur Urol. 1985;11(3):212–4. https://doi.org/10.1159/000472497.
Choi H, Lamb S, Pintar K, Jacobs SC. Primary signet-ring cell carcinoma of the urinary bladder [J]. Cancer. 1984;53(9):1985–90. https://doi.org/10.1002/1097-0142(19840501)53:9%3c1985::aid-cncr2820530930%3e3.0.co;2-z.
Thomas AA, Stephenson AJ, Campbell SC, Jones JS, Hansel DE. Clinicopathologic features and utility of immunohistochemical markers in signet-ring cell adenocarcinoma of the bladder [J]. Hum Pathol. 2009;40(1):108–16. https://doi.org/10.1016/j.humpath.2008.06.022.
Romics I, Székely E, Szendroi A. Signet-ring cell carcinoma arising from the urinary bladder [J]. Can J Urol. 2008;15(5):4266–8.
Burnett AL, Epstein JI, Marshall FF. Adenocarcinoma of urinary bladder: classification and management [J]. Urology. 1991;37(4):315–21. https://doi.org/10.1016/0090-4295(91)80256-7.
Guo L, Zhang L, Wang J, Zhang X, Zhu Z. Pelvic lymph node dissection during cystectomy for patients with bladder carcinoma with variant histology: does histologic type matter? Front Oncol. 2020;10:545921. https://doi.org/10.3389/fonc.2020.545921.
Pugashetti N, Yap SA, Lara PN, Gandour-Edwards R, Dall’Era MA. Metastatic signet-ring cell carcinoma of the urinary bladder: a novel management approach to a rare tumour [J]. Can Urol Assoc J. 2015;9(3–4):E204–7. https://doi.org/10.5489/cuaj.2447.
Hamakawa T, Kojima Y, Naiki T, Kubota Y, Yasui T, Tozawa K, et al. Long-term survival of a patient with invasive signet-ring cell carcinoma of the urinary bladder managed by combined s-1 and cisplatin adjuvant chemotherapy [J]. Case Rep Urol. 2013;2013:915874. https://doi.org/10.1155/2013/915874.
El Ammari JE, Ahsaini M, Riyach O, El Fassi MJ, Farih MH, Hammas N, et al. Primary signet-ring cell carcinoma of the urinary bladder successfully managed with cisplatin and gemcitabine: a case report. J Med Case Rep. 2013;7:37. https://doi.org/10.1186/1752-1947-7-37.
Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol. 1984;2(3):187–93. https://doi.org/10.1200/JCO.1984.2.3.187.
Iacovino ML, Miceli CC, De FM, et al. Novel therapeutic opportunities in neoadjuvant setting in urothelial cancers a new horizon opened by molecular classification and immune checkpoint inhibitors. Int J Mol Sci. 2022;23:3. https://doi.org/10.3390/ijms23031133.
Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–61. https://doi.org/10.1016/j.ccell.2015.03.001.
Kamoun A, de Aure R, Allory Y, et al. A consensus molecular classification of muscle-invasive bladder cancer. Eur Urol. 2020;77(4):420–33. https://doi.org/10.1016/j.eururo.2019.09.006.
Rey-Cárdenas M, Guerrero-Ramos F, de Liaño G, Lista A, et al. Recent advances in neoadjuvant immunotherapy for urothelial bladder cancer: what to expect in the near future. Cancer Treat Rev. 2021;93:102142. https://doi.org/10.1016/j.ctrv.2020.102142.
Acknowledgements
We thank the National Cancer Institute, which supports and oversees the SEER database.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
LL, QW, and HY contributed to the conception and design. LL, CL and QW contributed to the collection and assembly of data. LL, HY and YW contributed to the data analysis and interpretation. LL, QW and YW wrote the manuscript. CL data collection, manuscript editing and revised manuscript. LL, CL, QW, HY and YW gave final approval of the manuscript and agreed to be accountable for all aspects of work. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Since SEER is a publicly available database and all records have been deidentifed, no additional ethical approval or informed consent was required after the SEER Research Data Agreement was signed for accessing data. The study was carried out in accordance with the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, L., Li, C., Wang, Q. et al. A model for predicting overall survival in bladder cancer patients with signet ring cell carcinoma: a population-based study. Eur J Med Res 28, 61 (2023). https://doi.org/10.1186/s40001-022-00970-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-022-00970-y