Abstract
Iron deficiency (ID) is the most common nutritional disorder worldwide. It is often observed in patients with chronic diseases, such as heart failure (HF), chronic kidney disease (CKD), inflammatory bowel disease (IBD) and cancer. ID is associated with poor clinical outcome, including poor performance, reduced quality of life, as well as increased hospitalization and mortality. The aim of this review is to provide an overview about the role of ID in chronic diseases (HF, CKD, IBD, cancer) regarding their current definitions and clinical relevance; diagnostic accuracy of iron parameters in chronic inflammatory conditions and its potential as prognostic markers. Due to different definitions and guideline recommendations of ID, various laboratory parameters for ID diagnostic exist and there is no general consensus about the definition of ID and its treatment. Still, a general trend can be observed across all investigated indications of this review (HF, CKD, IBD, cancer) that serum ferritin and transferrin saturation (TSAT) are the two parameters mentioned most often and emphasized in all guidelines to define ID and guide treatment. The most commonly used threshold values for the diagnosis of ID are TSAT of < 20% and serum ferritin of < 100–300 µg/L. Noteworthy, both TSAT and particularly ferritin are frequently applied, but both may vary due to inflammatory conditions. Studies showed that TSAT is less affected by inflammatory processes and may therefore be more accurate and reliable than serum ferritin, particularly in conditions with elevated inflammatory state. A low iron status and particularly a low TSAT value was associated with a poor outcome in all investigated indications, with the strongest evidence in HF patients. Routine surveillance of iron status in these groups of patients with chronic conditions is advisable to detect ID early. Depending on the inflammatory state, TSAT < 20% may be the more accurate diagnostic marker of ID than ferritin. Moreover, TSAT may also be the more reliable estimate for the prognosis, particularly in HF.
Similar content being viewed by others
Introduction
Iron deficiency (ID) is the most common nutritional disorder in the world [1]. Multifactorial causes can lead to ID, of which blood loss, insufficient dietary intake and reduced iron absorption and metabolism due to inflammatory conditions are the most important ones [2, 3]. ID is associated with a worse clinical outcome such as poor performance, reduced quality of life, increased hospitalization and mortality [4, 5]. Moreover, ID may also aggravate underlying chronic diseases [4,5,6]; e.g., heart failure (HF) patients with ID have more symptoms and worse outcome [7, 8] or patients with chronic kidney disease (CKD) plus ID progress more often to end-stage kidney disease [9, 10]. ID is often overlooked, as the most common symptoms of ID (e.g., fatigue, headache, hair loss, sleeplessness) are unspecific and often difficult to distinguish from symptoms of the primary disease [4, 11]. Moreover, ID and the presence of anemia (iron-deficiency anemia) are not necessarily linked with each other, i.e., each can be present in the absent of the other [4]. Hence, screening for hemoglobin concentration and red blood cell indices is insufficient to adequately diagnose ID [11]. In addition, the definition of ID is not consistent [5]. Thus, a uniform diagnosis would be necessary for an accurate identification of ID, based on its specific pathophysiological role, independent of anemia [12]. The aim of this review is to provide an illustrative overview and comparison of the role of ID in different chronic diseases. Therefore, we defined three core themes of this review:
-
(1)
To evaluate the current definitions of ID and their clinical relevance;
-
(2)
To discuss the diagnostic accuracy of iron parameters in chronic inflammatory conditions;
-
(3)
To assess the role of iron parameters as prognostic markers.
Pathophysiology of ID in chronic inflammation
In case of inflammatory conditions, the availability of iron is limited, this includes reduced bioavailability by down-regulated intestinal absorption as well as transfer from iron storages and utilization in the bone marrow [5]. The mechanism of reduced iron metabolism is complex and still not fully understood, but the peptide hepcidin plays a key role as master switch in the regulation of iron uptake and distribution in inflammatory conditions [13, 14]. Studies examined pathophysiologic processes of ID in inflammatory conditions, showing that ID is triggered by pro-inflammatory cytokines (IL-6, IL-1, TNF-α). Cytokine-activated signaling pathways lead to blunted responses to erythropoietin (EPO), apoptosis of erythroid progenitors and hepcidin-mediated malabsorption and reticuloendothelial system (RES) trapping of iron [13]. Hepcidin is an antimicrobial peptide hormone and is mainly expressed in the liver due to cytokine activation such as IL-6. Hepcidin regulates iron by binding to and inducing internalization of ferroportin, the only known cellular iron-exporting protein [13]. Ferroportin channels are present on the basolateral membrane of enterocytes, hepatocytes and macrophages, and iron transport is inhibited by an elevated hepcidin level [13, 14]. Hence, hepcidin can be described as a central gate-keeper, which is triggered by inflammatory conditions and contributes to ID, especially in chronic diseases [4, 5, 13].
Definition of iron deficiency
Understanding the pathophysiology of ID is also essential to properly define the iron status and for subsequent diagnosis. Alterations in iron availability can be described in terms of ‘absolute’ or ‘functional’ ID [15]. The reduction of stored iron in the monocyte-macrophage system, including bone marrow, liver and spleen is referred to as absolute ID. This is characterized by a low level of stored iron resulting in low serum ferritin and a reduced saturation of the iron transport protein transferrin (i.e., low level of transferrin saturation—TSAT). Functional ID is described by normal iron stores, but iron cannot be released sufficiently due to internalized ferroportin channels, caused by hepcidin [11, 16]. This results in normal ferritin levels, but iron is not sufficiently available for the system [13, 16]. As ferritin is an acute phase protein, it may be even increased, whereas TSAT may be less affected by inflammatory effects. The low availability of iron results in a low TSAT level [5]. Inflammatory processes are not absolute static as the extent and effects of chronic inflammation depend on several internal and external pathogenic factors, resulting in significant changes in inflammation status and disease activity, resulting in changes in iron availability [4, 5, 13]. Thus, the definition of ID should reflect the body’s needs of iron in the context of its iron availability. Importantly, ID needs to be clearly distinguished from ID anemia as ID and ID anemia have different physiological characteristics with their individual symptomatic, diagnostic and treatment profiles [4].
Diagnosis of iron deficiency
The gold standard to determine ID is to determine iron content of the bone marrow. However, this is not feasible in routine clinical practice [17]. Therefore, different non-invasive biochemical markers are widely used to determine ID.
Types of biochemical markers
Serum iron
In case of ID, serum iron falls below the normal range of 40–165 μg/L [3]. Assessing iron status solely upon serum iron measurement is limited due to rapid fluctuations of serum iron depending, e.g., on nutritional intake and circadian rhythm [11]. It is reduced by inflammation [11, 14]. The variability of serum iron concentrations, which are necessary for determination of TSAT, should be included for interpretation of TSAT results [5].
Serum transferrin
Transferrin is a plasma glycoprotein mainly synthesized in the liver. The two binding sites for Fe3+ ions enable the transport of iron in the body to target cells for absorption by transferrin receptors. The binding affinity to transferrin is dependent on the pH value. Thus, iron-bound transferrin circulates with a high affinity in the healthy plasma and releases iron in endosomes with acidic pH [14, 18]. In case of ID and hypoxia, transferrin synthesis rate increases. Steroid hormones (e.g., estrogens) also stimulate transferrin synthesis, but it is inhibited by lack of nutrients. In addition, inflammatory conditions have a negative impact on synthesis of transferrin, but data are not consistent [14]. Normal serum transferrin conc. is 200–400 mg/dL [11]. For the diagnosis of ID, transferrin is mainly used for the calculation of transferrin saturation [14].
Transferrin saturation (TSAT)
TSAT provides information about iron availability. It is calculated from serum iron concentration and the total iron binding capacity (TIBC) and is expressed in %. The TIBC reflects the blood’s binding capacity of iron and is very closely correlated with transferrin [11, 18, 19]. Under normal conditions, 20–45% of the TICB is loaded with iron (= TSAT) [18].
\(\text {Total iron binding capacity (TIBC)\,=\,serum Transferrin x conversion factor }\)
converting factor (25.1 for TIBC (μmol/L) or 1.4 for TIBC (μg/L)) [18]
In ID, TSAT usually falls below 20% [18]. TSAT as a reliable diagnostic maker for ID is often used in clinical practice and recommended in several guidelines and studies [11, 20,21,22,23] with high sensitivity and specificity [24]. Noteworthy, the value of TSAT may fluctuate as both serum iron and transferrin are influenced by various factors as addressed above [11, 14]. Due to the influence of the circadian rhythm and dietary intake of iron, TSAT should always be measured in the morning under fasting conditions [5]. The impact of inflammation seems to be negligible, because studies show that TSAT is fluctuating less than serum ferritin in inflammatory conditions [2, 5, 24]. Therefore, TSAT can be used to determine ID with chronic diseases [2, 4].
Serum ferritin
Ferritin is a marker to evaluate the iron stores. Decreased serum ferritin with a threshold of < 30 μg/L in otherwise healthy individuals or < 100 μg/L in chronic conditions indicates an inadequate level of iron reservoir and thereby absolute ID [5]. However, the thresholds of serum ferritin concentrations may vary depending on age. Ferritin values are higher at birth, decrease in childhood and increase again in adulthood [17]. Low ferritin levels are also observed in elderly patients due to iron resorption disorders or lower food intake [5].
In inflammatory processes, ferritin acts as an acute phase protein leading to increased values [5]. Other factors, such as liver disease/damage, multiple malignancies, infections, renal failure, muscular cytolysis, decompensated diabetes and hyperthyroidism and certain metabolic syndromes can also cause increased ferritin levels [14, 25]. An increased ferritin value occurs after iron administration or blood transfusion, which may influence the accuracy of the ID diagnosis [14, 26]. Falsely low ferritin values independent of iron depletion are reported in hypothyroidism or vitamin C deficiency [17]. In addition, a high variability between the laboratory methods for serum ferritin measurement was found [5, 25]. Therefore, ferritin alone is not suitable for the diagnosis of ID, especially in inflammatory conditions. If acute or chronic inflammation is suspected, the CRP (C-reactive protein) value should be determined as well [5].
Soluble transferrin receptor (sTfR)
The sTfR is a protein dimer that results from proteolytic cleavage of the extracellular transferrin receptor on cell surfaces. The serum concentration is directly proportional to the erythropoietic rate and inversely proportional to tissue iron availability [27]. The normal range of sTfR is 0.8–2.2 mg/L [3]. In iron-deficient patients and generally in every expansion of erythropoiesis, increased sTfR levels (> 1.8 m/L (Dade-Behring test); > 4.4 mg/L for women and > 5.0 mg/L for men (Roche test)) are observed [11]. Therefore, increased levels can also be shown in patients with hemolysis or after administration of erythropoiesis-stimulating agents (ESAs). Reduced sTfR levels were found in conditions of hypoproliferative erythropoiesis (e.g., aplastic anemia or renal anemia) [3, 11]. The main advantage of sTfR is the reflection of the entire erythropoiesis, which is useful for a differential diagnosis in iron-deficient erythropoiesis. A disadvantage of this parameter might be its inaccuracy in case of functional ID, where false normal sTfR values are measured due to inhibited erythropoiesis [11]. Regarding its clinical use, the calculation of the sTfR–ferritin index is recommended [3].
sTfR–ferritin index
The ratio of sTfR (in mg/L) and the log of ferritin (in μg/L), is called sTfR–ferritin index (sTfR/log-ferritin). This index is convenient for the diagnosis of functional ID in inflammatory conditions, and also for anemia of chronic diseases (ACD). The sTfR reflects the erythropoiesis and increases with ID, whereas ferritin describes decreased iron stores in case of ID, and is normal or increased in ACD [11]. The threshold of sTfR–ferritin index depends on inflammatory conditions and individual assay methods. For absolute ID, the threshold of sTfR–ferritin index is > 1.5 (Dade-Behring test) or > 3.2 (Roche test), whereas for functional ID (CRP > 5 mg/L) and ACD (reduced hemoglobin (Hb) and CRP > 5 mg/L) > 0.8 (Dade-Behring test) or > 2.0 (Roche test) [11, 28]. In general, the sTfR–ferritin index is highly specific [29]. Several factors limit the use of this parameter in clinical practice such as high costs, availability of heterogeneous assays and different sTfR norms [3, 15].
Guideline recommendations for ID diagnostics
A total of 12 guidelines in chronic disease (HF, CKD, IBD, cancer) [11, 20, 21, 23, 30,31,32,33,34,35,36,37] and 3 guidelines in general population [38,39,40] were identified that deal with the diagnosis of ID (Table 1). All guidelines recommended the screening for ID, but their definitions of ID vary significantly. However, all guidelines recommend to measure ferritin concentrations and nearly three-quarters (11 of 15) propose TSAT as an alternative or complementary parameter for ID diagnosis, especially in the presence of inflammation and/or for functional ID in chronic disease.
Iron deficiency diagnosis and outcome in chronic diseases
Iron deficiency in heart failure (HF)
A large number of patients with HF suffer from ID [8]. The etiology of ID in HF is multifactorial. It often arises from reduced iron intake, impaired intestinal absorption, gastrointestinal bleeding (e.g., by concomitant use of aspirin), uraemia (e.g., CKD), venepuncture, chronic low-grade inflammation or inhibition of EPO synthesis (CKD, possible due to use of angiotensin-converting inhibitors (ACE-I) or angiotensin receptor blockers (ARB)) [41, 42]. Different mechanism of EPO inhibition by ACE-I and ARB have been described [42, 43]. One is the inhibition of circulating angiotensin II levels resulting in lower levels of erythroid progenitor cells [44]. Other studies have demonstrated that levels of insulin-like growth factor 1 are reduced, which is associated with erythroid stimulation [45]. Another is the increasing level of the erythropoiesis inhibitor N-acetyl-seryl-aspartyl-lysine-proline by ACE-I use, leading to a decrease in erythropoiesis [46].
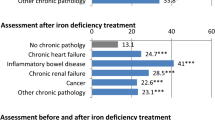
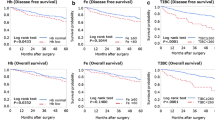
The prevalence of ID ranges from 33–74%, depending on the clinical study characteristics and the applied definition of ID [47]. Within an international pooled cohort of 1506 patients with chronic HF, an ID prevalence of 50% was found, defined by serum ferritin < 100 μg/L or serum ferritin 100–299 μg/L with TSAT < 20% [8], a definition later also used in an expert consensus document [48]. The recommendations are emphasized by the significant clinical impact of ID in patients with HF (Table 2), regardless of ejection fraction or disease severity [7, 8]. ID as a medical condition uncoupled from ID anemia was demonstrated in many trials with HF patients. It was shown that the presence of ID affects outcome [7, 49], irrespective of anemia [8, 50]. Patients with HF and ID were associated with poor health status, higher morbidity and mortality [51,52,53,54,55,56]. In some studies, negative outcomes were directly associated with low TSAT levels regardless of ferritin [24, 55]. For example, Ambrosy et al. (2020), showed a prevalence of TSAT < 20% in approx. 50% of the cases, which was associated with higher rates of morbidity and mortality [55]. A persistence of ID with TSAT < 20% in HF patients both at baseline and at 6 months was strongly associated with higher mortality compared with never having ID, superior to ID based on serum ferritin levels [57]. Thus, TSAT may be used as a marker for prognosis in HF patients [57, 58]. As to whether severity of ID is associated with worse outcome is not well investigated. Still, an association between sTfR and health-related quality of life has been found [59].
In conclusion, the best clinical outcomes in patients with HF were observed in patients with healthy iron status (TSAT > 20% and ferritin > 100 µg/L). ID was generally diagnosed with ferritin < 100 µg/L or 100–300 µg/L plus TSAT < 20%. Other iron parameters like the sTfR were rarely used or recommended for ID diagnosis in HF patients. The benefit of treating ID is an independent therapeutic target in HF [4]. Clinical evidence showed that there is a positive effect on management of ID with iv iron (FCM, ferric carboxymaltose) in outcomes: Compared to placebo, the administration of FCM improved NYHA class [60], prolonged 6-min walk test (6MWT) distance [61] and also decreased rates of recurrent cardiovascular (CV) hospitalizations and mortality [62] in HF patients with ID. These findings are supported in the recent AFFIRM-HF study, whereby treatment with FCM significantly reduced the risk of subsequent HF hospitalizations or CV death in iron-deficient HF patients compared to placebo [63]. In a secondary analysis of AFFIRM-HF, patients assigned to FCM had significantly increased health-related QoL [64].
Iron deficiency in chronic kidney disease (CKD)
ID is also common among patients with CKD. Several factors, such as reduced iron absorption, blood loss, chronic inflammation, hyperparathyroidism, drugs (e.g., ACE-I, ARB, aspirin) and erythropoietin deficiency/hyporesponsiveness to erythropoietin, might cause the development of ID/ ID anemia in patients with CKD [4, 42]. Based on different study designs and definitions of ID, the prevalence ranges from 24 to 85%, also depending on the CKD stage [4]. In CKD, ID is often associated with a negative clinical impact (Table 3) [4, 65]. However, it should be noted that the diagnosis and treatment of ID without anemia is not well studied in CKD. Irrespective of the presence of ID with or without anemia, the study results provide a correlation between low iron status (measurement with serum iron and/or serum ferritin and/or TSAT) and clinical outcome in patients with non-dialysis (ND)/hemodialysis (HD)-CKD [65,66,67,68,69,70]. In case of functional ID/anemia, high ferritin levels with a value of > 100–500 or 109–2783 μg/L indicated a higher risk of mortality and cardiovascular hospitalization [66, 67]. In contrast, low TSAT values were significantly associated with a higher mortality risk independent of absolute or functional ID/anemia [68, 71,72,73]. In an analysis of approx. 2500 ND-CKD patients, a significantly lower physical health-related QoL was found for ID (measured by low TSAT level) after adjustment for Hb levels [45]. Further studies explored TSAT as a marker of iron metabolism by its modifying effects on Hb response in dialysis patients [74]. Therefore, TSAT could be a suitable marker for iron supplementation therapy to achieve clinical improvements [75, 76]. The clinical role of sTfR or sTfR–ferritin index for identifying ID in CKD is limited by the small number of studies and their heterogeneous results [77, 78]. The worse outcome of ID in CKD reflects the major importance of its diagnosis and treatment. This is proven by a study with HD patients treated with iv iron (FCM) and epoetin-alfa, which showed the best survival rates with normal to elevated iron values (Hb > 12 g/dL, TSAT > 25%, serum ferritin > 600 μg/L) [69].
Iron deficiency in inflammatory bowel disease (IBD)
ID in IBD is mainly caused by chronic inflammation and impaired gastrointestinal iron absorption, bowel resection and bleeding [4]. The prevalence of ID in IBD is not well known and most variable of all chronic diseases in this review. It ranges from 36 – 90% [79] or even from 13–90% [4], depending on the reviewed literature. A more precise prevalence of ID of approx. 45% in IBD, likely due to the selection of uniform ID threshold values from different studies (defined as serum ferritin < 30 μg/L or < 100 μg/L (if CRP is > 5 mg/L or > 10 mg/L) and TSAT < 16% or < 20%), was presented by the review Dignass et al. [5].
A routine monitoring of serum ferritin and TSAT is recommended to detect and treat ID, although most results about iron laboratory parameters derive from expert recommendations or reviews and clinical impact is not well studied [5]. Diagnosis of ID in quiescent IBD can be made by serum ferritin level < 30 µg/L and in active IBD by serum ferritin < 100 µg/L or TSAT < 20%. In case of elevated ferritin level of 100–300 µg/L, TSAT with a cut-off value of < 20% should be added as a complementary parameter to confirm the ID [5]. Clinical data about ID without anemia in gastroenterology are still rare. Most data about ID in IBD were studied in case of anemia [4]. However, one study found a relation between the treatment of ID and an improvement in the QoL of IBD patients [80]. In non-anemic, iron-deficient patients with IBD, the administration of iv iron significantly increased Hb, serum iron, serum ferritin and TSAT levels, which resulted in an improved QoL [80].
Iron deficiency in cancer
ID is a common concomitant disease in patients with cancer. Iron has an essential role in the cell metabolism and homeostasis, which are mostly affected by cancer and its therapy [6, 11, 81]. The causes of ID in patients with cancer depend on tumor type, localization and extent, but also on its treatment [81]. An ID prevalence of 42.6% defined as TSAT < 20% was identified in oncology patients [6]. ID was more frequent in this trial than ID anemia with a prevalence of 33.0% (Hb ≤ 12 g/dL). Most ID patients showed functional ID (82%; TSAT < 20%, serum ferritin ≥ 30 µg/L), whereas 18% had absolute ID. The highest prevalence was found in pancreatic (63.2%), colorectal (51.9%) and lung cancer (50.7%) [6]. A prospective cohort study found that only one third of cancer patients were tested for iron parameters before the start of an anemia treatment [82]. It appears that the diagnosis of ID is not part of medical routine in oncology [6, 82], although both anemia and ID correlated with tumor stage and disease status and also had a significant impact on QoL [6]. Moreover, a significant correlation between ID prevalence (defined as serum ferritin < 30 µg/L and TSAT < 15%, or functional ID with serum ferritin < 800 µg/L and TSAT < 20%) and tumor response was observed [83]. The use of sTfR/log-ferritin index to detect ID in cancer related anemia compared to non-anemia, identified adverse effect on QoL and overall survival [84]. Overall, oncologic patients with anemia showed worse outcome as those without anemia, related to the progressive stadium of the disease and the fact that anemia can be a limiting factor for cancer treatment [85]. Thus, anemic cancer patients had a higher risk of dose reductions and discontinuation in chemotherapy, poor prognosis and significantly shorter overall survival [86]. Further experimental studies discovered an antitumor effect by macrophage-modulating with iron-nanoparticle, which shows the importance of iron in tumor metabolism [87]. Therefore, the iron status may provide information about medical outcome, making the monitoring and treatment of iron parameters essential. Clinical evidence suggests that treatment of ID with iv iron (with/without ESAs), in contrast to oral iron, improves overall outcomes without increasing the risk of infection or cardiovascular morbidity in oncology patients [86]. Notably, treatment with iv iron (FCM) resulted in sustainable Hb correction in tumor patients with chemotherapy-induced anemia [88]. Compared with oral iron, iv iron reduced blood transfusion requirements and hospital stay [89] and improved QoL in colorectal surgery-treated tumor patients [90].
Finally, ID might be a marker for detecting cancer. Thus, a cohort study showed that men and postmenopausal women with ID defined as TSAT < 15%, had a fivefold increased risk of developing gastrointestinal cancer [91]. Especially, serum iron and TSAT showed an inverse association with the risk of colon cancer [86].
Conclusion
ID in chronic diseases is a multifactorial and complex co-morbidity influenced by the combination of underlying disease (including the disease stages), treatment modalities and chronic inflammatory states. Different interpretations or definitions of ID in guidelines and studies lead to various diagnostic approaches and variable prevalence data, which could be the reason that ID is not fully recognized as a stand-alone medical condition and often overlooked. Significant differences between the different chronic diseases concerning definition and management of ID could be observed. While in HF many clinical data on prevalence, impact on outcome and treatment of ID especially in correlation with a low TSAT level of < 20% exist, ID without anemia is often still underestimated in other chronic diseases like CKD, IBD and cancer. However, an early diagnosis and subsequent treatment of ID is important, since reduced iron levels were associated with negative clinical outcome, e.g., higher risk of morbidity, mortality and reduced QoL within all indications. A higher hospitalization rate was observed in HF and CKD in correlation with ID. Some studies found a possible relationship between ID and cancer development. There are various diagnostic parameters with different threshold values for ID available. However, diagnosis of ID with average threshold values of TSAT < 20% and serum ferritin < 100–300 µg/L is frequently applied, which is independent of the diagnosis of anemia. As serum ferritin may vary depending on inflammatory status, TSAT with a cut-off value of < 20% may be the first indicator of ID, but also of prognostic value in patients with chronic diseases, particularly in HF.
Availability of data and materials
Not applicable.
References
Organization WH. Micronutrient deficiencies 2020. https://www.who.int/nutrition/topics/ida/en/. Accessed 10 June 2020.
Cacoub P, Vandewalle C, Peoc’h K. Using transferrin saturation as a diagnostic criterion for iron deficiency: a systematic review. Crit Rev Clin Lab Sci. 2019;56(8):526–32. https://doi.org/10.1080/10408363.2019.1653820.
Stein J, Dignass AU. Management of iron deficiency anemia in inflammatory bowel disease – a practical approach. Ann Gastroenterol. 2013;26(2):104–13.
Cappellini MD, Comin-Colet J, de Francisco A, et al. Iron deficiency across chronic inflammatory conditions: international expert opinion on definition, diagnosis, and management. Am J Hematol. 2017;92(10):1068–78. https://doi.org/10.1002/ajh.24820.
Dignass A, Farrag K, Stein J. Limitations of serum ferritin in diagnosing iron deficiency in inflammatory conditions. Int J Chronic Dis. 2018;2018:9394060. https://doi.org/10.1155/2018/9394060.
Ludwig H, Müldür E, Endler G, Hübl W. Prevalence of iron deficiency across different tumors and its association with poor performance status, disease status and anemia. Ann Oncol. 2013;24(7):1886–92. https://doi.org/10.1093/annonc/mdt118.
Martens P, Nijst P, Verbrugge FH, Smeets K, Dupont M, Mullens W. Impact of iron deficiency on exercise capacity and outcome in heart failure with reduced, mid-range and preserved ejection fraction. Acta Cardiol. 2018;73(2):115–23. https://doi.org/10.1080/00015385.2017.1351239.
Klip IT, Comin-Colet J, Voors AA, et al. Iron deficiency in chronic heart failure: an international pooled analysis. Am Heart J. 2013;165(4):575-82.e3. https://doi.org/10.1016/j.ahj.2013.01.017.
Aoun M, Karam R, Sleilaty G, Antoun L, Ammar W. Iron deficiency across chronic kidney disease stages: is there a reverse gender pattern? PLoS ONE. 2018;13(1):e0191541. https://doi.org/10.1371/journal.pone.0191541.
Kovesdy CP, Trivedi BK, Kalantar-Zadeh K, Anderson JE. Association of anemia with outcomes in men with moderate and severe chronic kidney disease. Kidney Int. 2006;69(3):560–4. https://doi.org/10.1038/sj.ki.5000105.
Hastka J, Metzgeroth G, Gattermann N. Onkopedia Leitlinien. Eisenmangel und Eisenmangelanämie 2022. https://www.onkopedia.com/de/onkopedia/guidelines/eisenmangel-und-eisenmangelanaemie/@@guideline/html/index.html. Accessed 30 Aug 2022.
Jankowska EA, Kasztura M, Sokolski M, et al. Iron deficiency defined as depleted iron stores accompanied by unmet cellular iron requirements identifies patients at the highest risk of death after an episode of acute heart failure. Eur Heart J. 2014;35(36):2468–76. https://doi.org/10.1093/eurheartj/ehu235.
Hentze MW, Muckenthaler MU, Galy B, Camaschella C. Two to tango: regulation of Mammalian iron metabolism. Cell. 2010;142(1):24–38. https://doi.org/10.1016/j.cell.2010.06.028.
Mircescu G, Crichton R, Geisser P. Iron therapy in renal anaemia. Bremen: UNI-MED Verlag AG; 2013.
Cappellini MD, Musallam KM, Taher AT. Iron deficiency anaemia revisited. J Intern Med. 2020;287(2):153–70. https://doi.org/10.1111/joim.13004.
Metzgeroth G, Hastka J. Diagnostic work-up of iron deficiency/Diagnostisches Vorgehen bei Eisenmangel. 2004.
Archer NM, Brugnara C. Diagnosis of iron-deficient states. Crit Rev Clin Lab Sci. 2015;52(5):256–72. https://doi.org/10.3109/10408363.2015.1038744.
Elsayed ME, Sharif MU, Stack AG. Transferrin saturation: a body iron biomarker. Adv Clin Chem. 2016;75:71–97. https://doi.org/10.1016/bs.acc.2016.03.002.
Wish JB. Assessing iron status: beyond serum ferritin and transferrin saturation. Clin J Am Soc Nephrol. 2006;1(Suppl 1):S4-8. https://doi.org/10.2215/CJN.01490506.
Aapro M, Beguin Y, Bokemeyer C, et al. Management of anaemia and iron deficiency in patients with cancer: ESMO clinical practice guidelines. Ann Oncol. 2018;29(Suppl 4):iv96–110. https://doi.org/10.1093/annonc/mdx758.
Dignass AU, Gasche C, Bettenworth D, et al. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohns Colitis. 2015;9(3):211–22. https://doi.org/10.1093/ecco-jcc/jju009.
KDIGO. KDIGO Clinical practice guideline for anemia in chronic kidney disease. Official J Int Society Nephrol. 2012. https://doi.org/10.1038/kisup.2012.4.
McDonagh TA, Metra M, Adamo M, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021. https://doi.org/10.1093/eurheartj/ehab368.
Grote Beverborg N, Klip IT, Meijers WC, et al. Definition of iron deficiency based on the gold standard of bone marrow iron staining in heart failure patients. Circ Heart Fail. 2018;11(2):e004519. https://doi.org/10.1161/circheartfailure.117.004519.
Peyrin-Biroulet L, Williet N, Cacoub P. Guidelines on the diagnosis and treatment of iron deficiency across indications: a systematic review. Am J Clin Nutr. 2015;102(6):1585–94. https://doi.org/10.3945/ajcn.114.103366.
Ho JC, Stevic I, Chan A, Lau KK, Chan HHW. Serum ferritin is not sensitive or specific for the diagnosis of iron deficiency in patients with normocytic anemia. Blood. 2015;126(23):955. https://doi.org/10.1182/blood.V126.23.955.955.
Lok CN, Loh TT. Regulation of transferrin function and expression: review and update. Biol Signals Recept. 1998;7(3):157–78. https://doi.org/10.1159/000014542.
Thomas C, Thomas L. Biochemical markers and hematologic indices in the diagnosis of functional iron deficiency. Clin Chem. 2002;48(7):1066–76.
Oustamanolakis P, Koutroubakis IE. Soluble transferrin receptor-ferritin index is the most efficient marker for the diagnosis of iron deficiency anemia in patients with IBD. Inflamm Bowel Dis. 2011;17(12):E158–9. https://doi.org/10.1002/ibd.21881.
Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the heart failure Society of America. J Am Coll Cardiol. 2017;70(6):776–803. https://doi.org/10.1016/j.jacc.2017.04.025.
Drüeke TB, Parfrey PS. Summary of the KDIGO guideline on anemia and comment: reading between the (guide)line(s). Kidney Int. 2012;82(9):952–60. https://doi.org/10.1038/ki.2012.270.
Kliger AS, Foley RN, Goldfarb DS, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for anemia in CKD. Am J Kidney Dis. 2013;62(5):849–59. https://doi.org/10.1053/j.ajkd.2013.06.008.
Locatelli F, Bárány P, Covic A, et al. Kidney Disease: Improving Global Outcomes guidelines on anaemia management in chronic kidney disease: a European Renal Best Practice position statement. Nephrol Dial Transplant. 2013;28(6):1346–59. https://doi.org/10.1093/ndt/gft033.
National Institute for Health and Care Excellence (NICE). Chronic kidney disease: assessment and management. NICE guideline (NG203). Published: 25 August 2021. Last updated: 24 Nov 2021. https://www.nice.org.uk/guidance/ng203. Accessed 10 Sept 2022.
Yamamoto H, Nishi S, Tomo T, et al. 2015 Japanese Society for dialysis therapy: guidelines for renal anemia in chronic kidney disease. Renal Replacement Therapy. 2017;3(1):36. https://doi.org/10.1186/s41100-017-0114-y.
Snook J, Bhala N, Beales ILP, et al. British Society of Gastroenterology guidelines for the management of iron deficiency anaemia in adults. Gut. 2021;70(11):2030–51. https://doi.org/10.1136/gutjnl-2021-325210.
Griffiths E, Roy V, Alwan L, al. Ne. NCCN Guidelines Version 1.2022. Hematopoietic Growth Faktors. Management of Cancer- and Chemotherapy-Induced Anemia: National Comprehensive Cancer Network (NCCN); 2021. Version 1.2022. https://www.nccn.org/professionals/physician_gls/pdf/growthfactors.pdf. Accessed 30 Aug 2022.
World Health O. WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. Geneva: World Health Organization; 2020. p. 2020.
Short MW, Domagalski JE. Iron deficiency anemia: evaluation and management. Am Fam Physician. 2013;87(2):98–104.
BCGuidelines.ca. Iron Deficiency – Diagnosis and Management: British Columbia; 2019. https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/bc-guidelines/iron-deficiency.pdf. Accessed 8 May 2021.
McDonagh T, Macdougall IC. Iron therapy for the treatment of iron deficiency in chronic heart failure: intravenous or oral? Eur J Heart Failure. 2015;17(3):248–62. https://doi.org/10.1002/ejhf.236.
Kazory A, Ross EA. Anemia: the point of convergence or divergence for kidney disease and heart failure? J Am Coll Cardiol. 2009;53(8):639–47. https://doi.org/10.1016/j.jacc.2008.10.046.
Sirbu O, Sorodoc V, Jaba IM, et al. The influence of cardiovascular medications on iron metabolism in patients with heart failure. Medicina (Kaunas). 2019. https://doi.org/10.3390/medicina55070329.
Mrug M, Stopka T, Julian BA, Prchal JF, Prchal JT. Angiotensin II stimulates proliferation of normal early erythroid progenitors. J Clin Invest. 1997;100(9):2310–4. https://doi.org/10.1172/jci119769.
Guedes M, Muenz D, Zee J, et al. Serum biomarkers of iron stores are associated with worse physical health-related quality of life in nondialysis-dependent chronic kidney disease patients with or without anemia. Nephrol Dial Transplant. 2021;36(9):1694–703. https://doi.org/10.1093/ndt/gfab050.
Meer PVD, Lipsic E, Westenbrink BD, et al. Levels of hematopoiesis inhibitor N-Acetyl-Seryl-Aspartyl-Lysyl-Proline Partially explain the occurrence of anemia in heart failure. Circulation. 2005;112(12):1743–7. https://doi.org/10.1161/CIRCULATIONAHA.105.549121.
Drozd M, Jankowska EA, Banasiak W, Ponikowski P. Iron therapy in patients with heart failure and iron deficiency: review of iron preparations for practitioners. Am J Cardiovasc Drugs. 2017;17(3):183–201. https://doi.org/10.1007/s40256-016-0211-2.
Doehner W, Blankenberg S, Erdmann E, et al. Iron deficiency in chronic heart failure: diagnostic algorithm and present-day therapeutic options. Dtsch Med Wochenschr. 2017;142(10):752–7. https://doi.org/10.1055/s-0043-100900.
Jankowska EA, Rozentryt P, Witkowska A, et al. Iron deficiency predicts impaired exercise capacity in patients with systolic chronic heart failure. J Card Fail. 2011;17(11):899–906. https://doi.org/10.1016/j.cardfail.2011.08.003.
Comin-Colet J, Enjuanes C, Gonzalez G, et al. Iron deficiency is a key determinant of health-related quality of life in patients with chronic heart failure regardless of anaemia status. Eur J Heart Fail. 2013;15(10):1164–72. https://doi.org/10.1093/eurjhf/hft083.
Grote Beverborg N, van der Wal HH, Klip IT, et al. Differences in clinical profile and outcomes of low iron storage vs defective iron utilization in patients with heart failure: results from the DEFINE-HF and BIOSTAT-CHF Studies. JAMA Cardiol. 2019;4(7):696–701. https://doi.org/10.1001/jamacardio.2019.1739.
Moliner P, Jankowska EA, van Veldhuisen DJ, et al. Clinical correlates and prognostic impact of impaired iron storage versus impaired iron transport in an international cohort of 1821 patients with chronic heart failure. Int J Cardiol. 2017;243:360–6. https://doi.org/10.1016/j.ijcard.2017.04.110.
Alcaide-Aldeano A, Garay A, Alcoberro L, et al. Iron deficiency: impact on functional capacity and quality of life in heart failure with preserved ejection fraction. J Clin Med. 2020. https://doi.org/10.3390/jcm9041199.
Grammer T, Scharnagl H, Dressel A, et al. Iron Metabolism, hepcidin, and mortality (the Ludwigshafen Risk and Cardiovascular Health Study). Clin Chemis. 2019. https://doi.org/10.1373/clinchem.2018.297242.
Ambrosy AP, Fitzpatrick JK, Tabada GH, et al. A reduced transferrin saturation is independently associated with excess morbidity and mortality in older adults with heart failure and incident anemia. Int J Cardiol. 2020;309:95–9. https://doi.org/10.1016/j.ijcard.2020.03.020.
Núñez J, Comín-Colet J, Miñana G, et al. Iron deficiency and risk of early readmission following a hospitalization for acute heart failure. Eur J Heart Fail. 2016;18(7):798–802. https://doi.org/10.1002/ejhf.513.
Fitzsimons S, Yeo TJ, Ling L, et al. Impact of change in iron status over time on clinical outcomes in heart failure according to ejection fraction phenotype. ESC Heart Failure. 2021. https://doi.org/10.1002/ehf2.13617.
Campodonico J, Nicoli F, Motta I, et al. Prognostic role of transferrin saturation in heart failure patients. Eur J Prev Cardiol. 2021. https://doi.org/10.1093/eurjpc/zwaa112.
Comín-Colet J, Enjuanes C, González G, et al. Iron deficiency is a key determinant of health-related quality of life in patients with chronic heart failure regardless of anaemia status. Eur J Heart Fail. 2013;15(10):1164–72. https://doi.org/10.1093/eurjhf/hft083.
Anker SD, Colet JC, Filippatos G, et al. Rationale and design of Ferinject assessment in patients with IRon deficiency and chronic Heart Failure (FAIR-HF) study: a randomized, placebo-controlled study of intravenous iron supplementation in patients with and without anaemia. Eur J Heart Fail. 2009;11(11):1084–91. https://doi.org/10.1093/eurjhf/hfp140.
Ponikowski P, van Veldhuisen DJ, Comin-Colet J, et al. Rationale and design of the CONFIRM-HF study: a double-blind, randomized, placebo-controlled study to assess the effects of intravenous ferric carboxymaltose on functional capacity in patients with chronic heart failure and iron deficiency. ESC Heart Fail. 2014;1(1):52–8. https://doi.org/10.1002/ehf2.12006.
Anker SD, Kirwan BA, van Veldhuisen DJ, et al. Effects of ferric carboxymaltose on hospitalisations and mortality rates in iron-deficient heart failure patients: an individual patient data meta-analysis. Eur J Heart Fail. 2018;20(1):125–33. https://doi.org/10.1002/ejhf.823.
Ponikowski P, Kirwan B-A, Anker SD, et al. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. The Lancet. 2020;396(10266):1895–904. https://doi.org/10.1016/S0140-6736(20)32339-4.
Jankowska EA, Kirwan B-A, Kosiborod M, et al. The effect of intravenous ferric carboxymaltose on health-related quality of life in iron-deficient patients with acute heart failure: the results of the AFFIRM-AHF study. Eur Heart J. 2021. https://doi.org/10.1093/eurheartj/ehab234.
Mehta RC, Cho ME, Cai X, et al. Iron status, fibroblast growth factor 23 and cardiovascular and kidney outcomes in chronic kidney disease. Kidney Int. 2021;100(6):1292–302. https://doi.org/10.1016/j.kint.2021.07.013.
Cho ME, Hansen JL, Peters CB, Cheung AK, Greene T, Sauer BC. An increased mortality risk is associated with abnormal iron status in diabetic and non-diabetic Veterans with predialysis chronic kidney disease. Kidney Int. 2019;96(3):750–60. https://doi.org/10.1016/j.kint.2019.04.029.
Awan AA, Walther CP, Richardson PA, Shah M, Winkelmayer WC, Navaneethan SD. Prevalence, correlates and outcomes of absolute and functional iron deficiency anemia in nondialysis-dependent chronic kidney disease. Nephrol Dial Transplant. 2019. https://doi.org/10.1093/ndt/gfz192.
Sato M, Hanafusa N, Tsuchiya K, Kawaguchi H, Nitta K. Impact of transferrin saturation on all-cause mortality in patients on maintenance hemodialysis. Blood Purif. 2019;48(2):158–66. https://doi.org/10.1159/000499758.
Pollak VE, Lorch JA, Shukla R, Satwah S. The importance of iron in long-term survival of maintenance hemodialysis patients treated with epoetin-alfa and intravenous iron: analysis of 9.5 years of prospectively collected data. BMC Nephrol. 2009;10(1):6. https://doi.org/10.1186/1471-2369-10-6.
Kalantar-Zadeh K, McAllister CJ, Lehn RS, Liu E, Kopple JD. A low serum iron level is a predictor of poor outcome in hemodialysis patients. Am J Kidney Dis. 2004;43(4):671–84. https://doi.org/10.1053/j.ajkd.2003.12.029.
Yeh SC, Lin YC, Hong YC, Hsu CC, Lin YC, Wu MS. Different effects of iron indices on mortality in patients with autosomal dominant polycystic kidney disease after long-term hemodialysis: a nationwide population-based study. J Ren Nutr. 2019;29(5):444–53. https://doi.org/10.1053/j.jrn.2018.11.004.
Koo HM, Kim CH, Doh FM, et al. The relationship of initial transferrin saturation to cardiovascular parameters and outcomes in patients initiating dialysis. PLoS ONE. 2014;9(2):e87231. https://doi.org/10.1371/journal.pone.0087231.
Eisenga MF, Nolte IM, van der Meer P, Bakker SJL, Gaillard C. Association of different iron deficiency cutoffs with adverse outcomes in chronic kidney disease. BMC Nephrol. 2018;19(1):225. https://doi.org/10.1186/s12882-018-1021-3.
Gaweda AE, Bhat P, Maglinte GA, et al. TSAT is a better predictor than ferritin of hemoglobin response to Epoetin alfa in US dialysis patients. Hemodial Int. 2014;18(1):38–46. https://doi.org/10.1111/hdi.12078.
Kaneko Y, Miyazaki S, Hirasawa Y, Gejyo F, Suzuki M. Transferrin saturation versus reticulocyte hemoglobin content for iron deficiency in Japanese hemodialysis patients. Kidney Int. 2003;63(3):1086–93. https://doi.org/10.1046/j.1523-1755.2003.00826.x.
Hamano T, Fujii N, Hayashi T, Yamamoto H, Iseki K, Tsubakihara Y. Thresholds of iron markers for iron deficiency erythropoiesis-finding of the Japanese nationwide dialysis registry. Kidney Int Suppl. 2015;5(1):23–32. https://doi.org/10.1038/kisup.2015.6.
Gupta S, Uppal B, Pawar B. Is soluble transferrin receptor a good marker of iron deficiency anemia in chronic kidney disease patients? Indian J Nephrol. 2009;19(3):96–100. https://doi.org/10.4103/0971-4065.57105.
Venkatesan M, Saxena S, Kumar A. Evaluation of iron status in patients of chronic kidney disease—a study to assess the best indicators including serum transferrin receptor assay. Indian J Nephrol. 2019;29(4):248–53. https://doi.org/10.4103/ijn.IJN_159_18.
Kulnigg S, Gasche C. Systematic review: managing anaemia in Crohn’s disease. Aliment Pharmacol Ther. 2006;24(11–12):1507–23. https://doi.org/10.1111/j.1365-2036.2006.03146.x.
Çekiç C, İpek S, Aslan F, et al. The effect of intravenous iron treatment on quality of life in inflammatory bowel disease patients with nonanemic iron deficiency. Gastroenterol Res Pract. 2015;2015:582163. https://doi.org/10.1155/2015/582163.
Aapro M, Österborg A, Gascón P, Ludwig H, Beguin Y. Prevalence and management of cancer-related anaemia, iron deficiency and the specific role of i.v. iron. Ann Oncol. 2012;23(8):1954–62. https://doi.org/10.1093/annonc/mds112.
Steinmetz T, Schröder J, Plath M, et al. Antianemic treatment of cancer patients in German routine practice: data from a prospective cohort study-the tumor anemia registry. Anemia. 2016;2016:8057650. https://doi.org/10.1155/2016/8057650.
Saint A, Viotti J, Borchiellini D, et al. Iron deficiency during first-line chemotherapy in metastatic cancers: a prospective epidemiological study. Support Care Cancer: official journal of the Multinational Association of Supportive Care in Cancer. 2020;28(4):1639–47. https://doi.org/10.1007/s00520-019-04938-3.
Kanuri G, Sawhney R, Varghese J, Britto M, Shet A. Iron deficiency anemia coexists with cancer related anemia and adversely impacts quality of life. PLoS ONE. 2016;11(9):e0163817. https://doi.org/10.1371/journal.pone.0163817.
Family L, Xu L, Xu H, et al. The effect of chemotherapy-induced anemia on dose reduction and dose delay. Support Care Cancer. 2016;24(10):4263–71. https://doi.org/10.1007/s00520-016-3258-3.
Aksan A, Farrag K, Aksan S, Schroeder O, Stein J. Flipside of the coin: iron deficiency and colorectal cancer. Front Immunol. 2021;12:635899. https://doi.org/10.3389/fimmu.2021.635899.
Zanganeh S, Hutter G, Spitler R, et al. Iron oxide nanoparticles inhibit tumour growth by inducing pro-inflammatory macrophage polarization in tumour tissues. Nat Nanotechnol. 2016;11(11):986–94. https://doi.org/10.1038/nnano.2016.168.
Steinmetz T, Tschechne B, Harlin O, et al. Clinical experience with ferric carboxymaltose in the treatment of cancer- and chemotherapy-associated anaemia. Ann Oncol. 2013;24(2):475–82. https://doi.org/10.1093/annonc/mds338.
Calleja JL, Delgado S, del Val A, et al. Ferric carboxymaltose reduces transfusions and hospital stay in patients with colon cancer and anemia. Int J Colorectal Dis. 2016;31(3):543–51. https://doi.org/10.1007/s00384-015-2461-x.
Keeler BD, Dickson EA, Simpson JA, et al. The impact of pre-operative intravenous iron on quality of life after colorectal cancer surgery: outcomes from the intravenous iron in colorectal cancer-associated anaemia (IVICA) trial. Anaesthesia. 2019;74(6):714–25. https://doi.org/10.1111/anae.14659.
Ioannou GN, Rockey DC, Bryson CL, Weiss NS. Iron deficiency and gastrointestinal malignancy: a population-based cohort study. Am J Med. 2002;113(4):276–80. https://doi.org/10.1016/s0002-9343(02)01214-7.
Acknowledgements
Not applicable.
Prior presentation
None.
Funding
Vifor Pharma paid for the open access. There was no funding for this investigation.
Author information
Authors and Affiliations
Contributions
MR, VB and HPBR participated in literature search, manuscript drafting and review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
There was no ethics approval necessary because this is a review of the literature.
Consent for publication
All authors gave consent for the publication.
Competing interests
Martina Rohr is employed at Vifor Pharma. Vincent Brandenburg received lecture fees from Vifor Pharma.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rohr, M., Brandenburg, V. & Brunner-La Rocca, HP. How to diagnose iron deficiency in chronic disease: A review of current methods and potential marker for the outcome. Eur J Med Res 28, 15 (2023). https://doi.org/10.1186/s40001-022-00922-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-022-00922-6