Abstract
Background
Acute respiratory distress syndrome (ARDS) has been a prevalent disease in ICU with mortality of up to 27–45%. A considerable proportion of extubated ARDS patients passing spontaneous breathing trial (SBT) still requires reintubation.
Methods
Lung ultrasonography (LUS) was used to predict the success rate of extubation. Ninety-two patients passing the 60-min SBT were included in this prospective research. Their clinical characters including LUS, APACHE II, SOFA, CPIS, EVLWI and PaO2/FiO2 were collected before the SBT. Another two LUS assessments were performed at the end of and 4 h after SBT. LUS results were evaluated and scored by two independent experts, and the correlations of LUS scores, APACHE-II scores, SOFA scores, CPIS and EVLWI with the success rate of extubation and rate of reintubation were analyzed.
Results
Failed weaning and reintubation of ARDS patients were correlated with higher LUS scores both before and after SBT. Post-extubation distress was correlated with higher APACHE-II scores, SOFA scores, CPIS and EVLWI before SBT. There were positive correlations between the LUS score and APACHE-II score, SOFA score, CPIS and EVLWI before SBT, respectively.
Conclusion
LUS score measured at the end of 60-min SBT could be used to predict post-extubation distress in ARDS patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Acute respiratory distress syndrome (ARDS) is a complex syndrome characterized by acute progressive hypoxic respiratory failure post-lung capillary injury [1]. ARDS has been a prevalent disease in intensive care unit (ICU) [2]. Trauma or inflammatory mediators cause pulmonary vascular congestion, vascular endothelial cell damage, increased vascular permeability, and aggregation of inflammatory cells in the alveolar cavity [3]. Related inflammation factors and chest computed tomography (CT) are two important indicators for clinical evaluation of ARDS [4]. However, CT examination is frequently limited in critically ill patients with unstable hemodynamics or patients who cannot move due to assisted ventilation [5].
Ultrasonography began to be used in lung examinations in critically ill and emergency patients such as acute respiratory failure in the late 1990s [6, 7]. As Lichtenstein discovered the application value of lung ultrasonography (LUS) and established feasible operation and scoring rules, the imaging theory and clinical process of LUS have been established [8]. LUS can quickly differentiate and diagnose a variety of lung diseases, with increased diagnostic sensitivity and specificity [9]. LUS provides a lot of effective information for the alterations of lung morphology [10]. Indirect signs shown by ultrasound such as abnormal pleural line, disappearance of A-line, abnormal increase of B-line, lung consolidation and other manifestations can be used for the diagnosis of multiple diseases [11]. Previous studies have demonstrated that lung consolidation accompanied by bronchial inflation, abnormal pleural lines, diffuse pulmonary edema and disappearance of A-line are the main signs of LUS in ARDS patients [12]. Furthermore, pulmonary consolidation, diffuse pulmonary edema and abnormal pleural line are closely related to the onset of ARDS [13].
LUS has become an important method for clinical evaluation of patients’ condition. However, there is still insufficient research for LUS to guide and evaluate the success rate of extubation in ARDS patients. Among ARDS patients who are extubated after spontaneous breathing trial (SBT), a considerable proportion of patients may still need to be reintubated, which brings a serious burden to the patients’ health [14]. Therefore, we designed an evaluation system including LUS score combined with Clinical Pulmonary Infection Score (CPIS), Acute Physiology and Chronic Health Evaluation (APACHE II), Sequential Organ Failure assessment (SOFA), extravascular lung water indices (EVLWI) and SBT to assess the success rate and reintubation rate of ARDS patients in this study.
Methods
Study design
To investigate the correlation between the LUS scores and the incidence of post-extubation distress following SBT in ARDS patients, a prospective clinical trial was performed in this research. We evaluated the characteristics and extubating outcomes of ARDS patients at 48 h post-SBT. This study was approved by the Ethics Committee of the First Affiliated Hospital of Bengbu Medical College.
Participants
The inclusion criteria were: (1) over 18 years old. (2) Participants who were admitted in ICU. (3) Patients who met the diagnostic standard of ARDS (The Berlin definition). Patients who met the following criteria were excluded from our research: (1) less than 18 years old. (2) Patients in pregnancy. (3) Patients with a history of chronic obstructive pulmonary disease, including pulmonary embolism, trauma, undrained pneumothorax, and interstitial lung disease. (4) Patients with severe cardiac insufficiency and acute coronary syndrome. (5) Patients with autoimmune diseases.
A total of 176 ARDS patients were recruited and assessed for the eligibility to our study. Among the patients, 47 participants were excluded because they did not meet the inclusion criteria and 21 patients refused to continue participating in the research. The remaining 108 patients were assessed for their clinical scores including LUS, APACHE II, SOFA, CPIS, EVLWI and PaO2/FiO2 before SBT. Ninety two of them passed the 60-min SBT and received the LUS at the end of and 4 h post the trial. 48 h after SBT, 61 patients ended up with successful weaning of respirator, while 31 patients exhibited extubation distress and needed to be reintubated.
Spontaneous breathing trial
Patients who met all the following conditions were allowed to undergo SBT. (1) Patients whose condition improved or whose disease was cured. (2) Oxygenation index: PaO2/FiO2 ≥ 150 mmHg; PEEP ≤ 5 cmH2O; FiO2 ≤ 40%; pH ≥ 7.25; for COPD patients: pH > 7.30, FiO2 < 35%, PaO2 > 50 mm Hg. (3) Patients with stable hemodynamics, no dynamic changes of myocardial ischemia, and no clinically significant hypotension. (4) Patients with the ability to breathe spontaneously.
Low-level support and continuous positive pressure ventilation (≤ 5 cmH2O or PSV ≤ 7 cmH2O) were used as SBT for 60 min. The clinical indicators of SBT success were: (1) FiO2 < 40%, SpO2 ≥ 90%; PaO2 ≥ 60 mmHg; pH ≥ 7.32; PaCO2 increase ≤ 10 mmHg. (2) Stable hemodynamics: HR < 120 times/min; HR change < 20%; systolic blood pressure < 180 and > 90 mmHg; blood pressure changes < 20%. (3) Respiration RR ≤ 35 times/min; RR changes less than 50%.
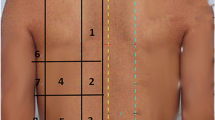
Lung ultrasonography
A senior physician was in charge of lung and ultrasound heart examination. Xario 100 ultrasound machine, phased array convex probe, and ultrasound probe (3.5–10.0 MHz) were used for the ultrasound examination in this study. A total of 12 lung areas on both sides of the front chest wall, side chest wall and back chest wall were examined and video data were recorded. The lungs were divided into three areas: anterior, lateral, and posterior by the parasternal line, anterior axillary line, and posterior axillary line. The left and right lungs were divided into 6 areas with the nipple plane as the upper and lower boundary. Two trained senior physicians separately scored the LUS results. Lung ultrasound images were defined as: (1) normal ventilation zone (N): lung sliding sign with A-line or less than 2 separate B-lines; (2) moderately reduced lung ventilation: multiple, typical B-line (B1 line); (3) severe lung reduced ventilation area: multiple fusion B line (B2-line); (4) consolidation lung area: tissue image with typical bronchial inflation. Each area was scored with the most severe performance: N was 0 points, B1 line was 1 point, B2 line was 2 points, and C was 3 points. The LUS score of one particular patient was the sum of the scores of each area, with 0–36 points.
Extravascular lung water indices
The right subclavian vein of ARDS patients was catheterized and connected with a temperature sensor. The PiCCO catheter was inserted into the patient through the femoral artery, and the catheter electrode was connected to the PiCCO monitor. 10 ml of 0.9% sodium chloride at 0–8 °C was quickly injected into the blood vessel through a deep venous catheter. The injection was repeated for 3 times and the average EVLW score was recorded.
Clinical characteristics
A senior doctor was responsible for collecting clinical data and clinical scores of patients upon admission, including baseline data, hemodynamic parameters, lactate, respiratory parameters, APACHE II, SOFA, CPIS, EVLWI assessment scores following the instructions of previous research before the SBT performance [15,16,17,18].
Statistical analysis
The categorized variables were shown as frequency or percentage. Mean and standard deviation were utilized to demonstrate continuous variables. Chi-square test (or Fisher’s exact test) was used to compare the classification variables. One-way ANOVA and Tukey’s post hoc test were used to analyze the continuous variables, and contingency table Chi-square test was acquired for the comparison of outcomes among different groups. The SAS 17.0 software (SAS Institute Inc., Cary, NC, USA) was purchased for the statistical analysis in this study.
Results
Study design and participants
To investigate the correlation between the LUS scores and the incidence of post-extubation distress following the 60-min SBT in ARDS patients, a retrospective trial was performed in this research. As shown in Fig. 1, a total of 176 ARDS patients were recruited and assessed for their eligibility to our study. Among all the patients, 47 participants were excluded because they did not meet the inclusion criteria and 21 patients refused to participate in this research. The clinical scores including LUS, APACHE II, SOFA, CPIS, EVLWI and PaO2/FiO2 of the rest 108 patients were tested before SBT. Ninety Two of them passed the 60-min SBT and received the LUS at the end of and 4 h post the trial. They were divided into the successfully weaned and failed weaned group according to their extubating outcomes at 48 h post-extubation. 48 h after SBT, 61 patients ended up with successful weaning of respirator, while 31 patients exhibited post-extubation distress and needed to be reintubated.
Clinical characteristics of the study population
Characteristics of the study population are shown in Table 1. The demographic parameters collected from patients of the two groups included age, gender, etiology of ARDS, disease onset time, Berlin diagnostic criteria. As shown in Table 1, there were no significant differences in any of the above characteristics between participants in these two groups at the beginning of our research (p > 0.05).
Post-extubation distress was correlated with higher LUS scores before, at the end of and 4 h after SBT
To demonstrate the correlation between LUS scores and the extubating outcomes of ARDS patients, the LUS scores tested before, at the end of and 4 h after SBT in the two groups are shown in Fig. 2. The LUS scores of patients with post-extubation distress 48 h after SBT were all significantly higher at the three time points than the successfully weaned group, indicating that there were significant differences in the LUS before and after SBT between the successful and unsuccessful extubation groups.
Post-extubation distress was correlated with higher APACHE II, SOFA, CPIS, EVLWI tested before the SBT
To further identify the relationship between the post-extubation distress and the APACHE II, SOFA, CPIS, EVLWI scores, we measured them before the performance of SBT following the instructions of previous research. As shown in Fig. 3, the scores of APACHE II (Fig. 3A), SOFA (Fig. 3B), CPIS (Fig. 3C), EVLWI (Fig. 3D) in the failed weaned group were all statistically higher than the successfully weaned group. These results demonstrated that post-extubation distress was correlated with higher APACHE II, SOFA, CPIS, EVLWI scores, which was also consistent with previous discoveries.
Acute physiology and chronic health evaluation II (APACHE II) scores (a), Sequential Organ Failure Assessment (SOFA) scores (b), clinical pulmonary infection score (CPIS) (c), and extravascular lung water indices (EVLWI) (d) measurements between successfully and failed weaned patients before the spontaneous breathing trial (SBT). Data were presented as mean ± SD showing all the data. One-way ANOVA followed by a Dunn’s multiple comparisons test. ***p < 0.001
Spearman’s correlations between LUS and APACHE II, SOFA, CPIS and EVLWI scores before the SBT
To investigate the correlation between LUS and APACHE II, SOFA, CPIS and EVLWI scores tested before the SBT, Spearman’s correlation analysis was performed. Significant positive liner correlations of LUS score with APACHE II, SOFA, CPIS and EVLWI scores are presented in Fig. 4A–D (r values were 0.291, 0.335, 0.321, 0.360, respectively, and all p < 0.001).
Spearman’s correlations between lung ultrasound scores (LUS) and acute physiology and chronic health evaluation II (APACHE II) scores (a), sequential organ failure assessment (SOFA) scores (b), clinical pulmonary infection score (CPIS) (c), and extravascular lung water indices (EVLWI) (d) in analyzed patients before the spontaneous breathing trial (SBT)
ROC analysis of LUS scores measured at the end of SBT to predict post-extubation distress
To demonstrate the predictive value of LUC scores tested at the end of SBT on the incidence of post-extubation distress of ARDS patients, receiver operating characteristic (ROS) curve was calculated. As presented in Fig. 5, a cut-off value of LUS score tested at the end of SBT was 18 and the corresponding area under curve (AUC) was 0.7345, with sensitivity 77.05% and specificity 61.29%, suggesting that LUC scores tested at the end of SBT exhibited potential to predict post-extubation distress.
Discussion
ARDS is mainly manifested as pulmonary edema and hyaline membrane formation caused by diffuse damage and increased permeability of pulmonary capillaries [19]. As an acute respiratory failure syndrome, its clinical features mainly include respiratory distress and asphyxia [20]. ARDS is harmful for the health of patients. Although its incidence is relatively low, its fatality rate is extremely high [21]. There are many causes of ARDS, including toxic gas inhalation, lung infections (bacteria, viruses, pneumocystis, etc.), drowning, shock, sepsis, lung trauma [22], among which shock, external trauma and infection have been reported as the most common causes [23, 24]. The pathogenesis of ARDS basically includes three processes: the migration and aggregation of inflammatory cells, the release of inflammatory mediators, the damage of pulmonary capillaries and the increase in permeability [25]. As an acute inflammation, ARDS may have no obvious symptoms before the onset. Moreover, because it is mostly caused by some primary diseases, it is often concealed by the symptoms of primary diseases in the diagnosis, which leads to the aggravation of ARDS and even death of the patient [26].
European Society of Intensive Care Medicine (ESICM), the American Thoracic Society (ATS) and the Society of Critical Care Medicine (SCCM) jointly organized and revised the new ARDS diagnostic criteria—the Berlin Definition in 2012 [27]. In Berlin Definition, the gold standard for the diagnosis of ARDS is the imaging findings: there are plaque shadows in both lungs that cannot be fully explained by pleural effusion, atelectasis, or nodules on chest radiograph [28]. The chest CT examination is also known as the most accurate method of ARDS diagnosis, due to its higher sensitivity and accuracy [29]. However, for critically ill patients in ICU, especially patients with unstable hemodynamics or patients who are not suitable to be moved due to tracheal intubation, chest CT examination is rather limited. Although chest X-ray (CXR) can replace CT for bedside examination, it has low sensitivity and specificity [30]. X-ray superimposes the imaging information of the chest on a piece of film. Due to the influence of the heart, mediastinum and diaphragm, lung lesions may be hidden and cannot be displayed. In addition, mobile bedside radiographs have a low diagnostic sensitivity rate for lung bottom infiltration. Accumulating evidence has shown that the consistency of different observers on the presence of infiltration in the same chest radiograph is rather low [31]. The disadvantages of both CT and X-rays are high cost and radiation exposure, which makes chest CT and X-rays especially unsuitable for examinations of special populations such as pregnant women and young children.
In this research, we chose to use an accurate, non-invasive, real-time and more convenient method—LUC to check and evaluate the condition of ARDS patients who cannot move in the ICU. The cost of lung ultrasound is much lower than traditional CT methods due to equipment and principles. More importantly, bedside LUC has the advantages of higher feasibility, smaller instrument footprint and less time consuming compared to bedside CT or X-ray. LUC can reduce the handling and radiation exposure of critically ill patients, and can display the changes in lung morphology in real time. We believe that LUS is also an effective tool for distinguishing acute cardiogenic pulmonary edema and ARDS. LUS can identify ARDS early because its ultrasound abnormalities are earlier than changes in blood gas analysis PaO2/FiO2, and the ultrasound findings are highly consistent with the progression of lung injury and CT images. More importantly, by constructing a LUS scoring system, we can quickly evaluate the prognosis of extubation of ARDS patients with LUS detection, and design the corresponding treatment and nursing strategies, which is otherwise difficult to achieve with only CT or X-ray imaging results.
In recent years, LUS has become a simple and reliable method for the clinical diagnosis of lung diseases, especially in ICU [32]. LUS provides a lot of effective information for changes in lung morphology. Indirect signs through ultrasound, including abnormal pleural line, a disappearance of line, abnormal increase of B-line, and lung consolidation, can assist the doctors to evaluate the progression of lung diseases [33]. The LUS characteristics of ARDS mainly include lung consolidation with bronchial inflation, abnormal pleural lines, diffuse pulmonary edema and disappearance of A-line. When the three signs of pulmonary consolidation, diffuse pulmonary edema and abnormal pleural line are present at the same time, the sensitivity and specificity of LUS diagnosis are both quite high [13]. Therefore, as an emerging bedside imaging diagnostic technology, LUS has the advantages of non-invasive, simple, reproducible, and convenient for dynamic observation. Effective information shown by LUS is of great significance for the early diagnosis, dynamic evaluation and follow-up of a variety of lung diseases.
Interestingly, the results of LUS have been widely used to predict the outcome and prognosis of many lung diseases. For example, Wang et al. reported in 2016 that LUS could be used to predict the therapeutic effect of prone position on ARDS and the prognosis of ARDS patients [34]. Zhao et al. reported in 2015 that LUS images could be used to measure the EVLW of ARDS patients [35]. In this study, we tried to use the LUS score to predict the post-extubation distress in ARDS patients passing the SBT. We performed LUS examinations on ARDS patients before, at the end, and 4 h later, and determined whether the extubated patients can be successfully free of the ventilator after 48 h as outcomes. We found that patients with higher LUS scores tend to exhibit post-extubation distress. The LUS score examined at the end of SBT has the potential to predict the onset of post-extubation distress.
In fact, the clinical application of LUS also has some limitations. LUS is mainly applied to the lesions involving the pleura. The application of LUS in deep lung lesions that do not involve the pleura is limited. For example, the lung consolidation caused by tumors is often mixed with gas, which could hinder the propagation of sound waves, resulting in unclear LUS images or even undetectable reality. We will continue to pay attention to this issue in our future studies.
Conclusion
In conclusion, we tried to illustrate the predictive effect of LUS scores measured at different time points on the outcome of ARDS patients 48 h after extubation in this study. We demonstrated that post-extubation distress correlated with higher LUS scores measured before SBT, at the end of 60-min SBT, and four hours after SBT. The LUS score measured before SBT and other predicted post-extubation distress assessments including APACHE II, SOFA, CPIS, EVLWI showed positive linear correlations. The LUS score examined at the end the 60-min SBT can be used to predict the incidence of post-extubation distress in ARDS patients.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- SBT:
-
Spontaneous breathing trial
- LUS:
-
Lung ultrasonography
References
Peck TJ, Hibbert KA. Recent advances in the understanding and management of ARDS. F1000Res. 2019. https://doi.org/10.12688/f1000research.20411.1.
Maca J, Jor O, Holub M, Sklienka P, Bursa F, Burda M, et al. Past and present ARDS mortality rates: a systematic review. Respir Care. 2017;62(1):113–22.
Grawe ES, Bennett S, Hurford WE. Early paralysis for the management of ARDS. Respir Care. 2016;61(6):830–8.
Papazian L, Calfee CS, Chiumello D, Luyt CE, Meyer NJ, Sekiguchi H, et al. Diagnostic workup for ARDS patients. Intensive Care Med. 2016;42(5):674–85.
Bein T, Grasso S, Moerer O, Quintel M, Guerin C, Deja M, et al. The standard of care of patients with ARDS: ventilatory settings and rescue therapies for refractory hypoxemia. Intensive Care Med. 2016;42(5):699–711.
Noirez L, Nicod LP. Lung and pleural space ultrasonography for pulmonologist. Rev Med Suisse. 2017;13(583):1990–5.
Zhang H, Han K. High intensity focused ultrasound enhances anti-tumor immunity through promoting CD4 Th1 effector T cell response. STEMedicine. 2020;1(4):e65.
Lichtenstein DA. BLUE-protocol and FALLS-protocol: two applications of lung ultrasound in the critically ill. Chest. 2015;147(6):1659–70.
Bianco F, Bucciarelli V, Ricci F, De Caterina R, Gallina S. Lung ultrasonography: a practical guide for cardiologists. J Cardiovasc Med. 2017;18(7):501–9.
Bello G, Blanco P. Lung ultrasonography for assessing lung aeration in acute respiratory distress syndrome: a narrative review. J Ultrasound Med. 2019;38(1):27–37.
Picano E, Pellikka PA. Ultrasound of extravascular lung water: a new standard for pulmonary congestion. Eur Heart J. 2016;37(27):2097–104.
Guerin C, Gattinoni L. Assessment of oxygenation response to prone position ventilation in ARDS by lung ultrasonography. Intensive Care Med. 2016;42(10):1601–3.
Haddam M, Zieleskiewicz L, Perbet S, Baldovini A, Guervilly C, Arbelot C, et al. Lung ultrasonography for assessment of oxygenation response to prone position ventilation in ARDS. Intensive Care Med. 2016;42(10):1546–56.
Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, et al. Methylprednisolone infusion in early severe ARDS: results of a randomized controlled trial. Chest. 2007;131(4):954–63.
Cheng Z, Yang YJ, Jing XG, Dai LL, Wang X, Jia LQ, et al. Diagnostic value of HBP, PCT combined with APACHE score respectively in ventilator-associated pneumonia. Zhonghua Yi Xue Za Zhi. 2019;99(22):1698–702.
de Grooth HJ, Geenen IL, Girbes AR, Vincent JL, Parienti JJ, Oudemans-van Straaten HM. SOFA and mortality endpoints in randomized controlled trials: a systematic review and meta-regression analysis. Crit Care. 2017;21(1):38.
Chen C, Yan M, Hu C, Lv X, Zhang H, Chen S. Diagnostic efficacy of serum procalcitonin, C-reactive protein concentration and clinical pulmonary infection score in Ventilator-Associated Pneumonia. Med Sci. 2018;34:26–32.
Ma S, Zhao ML, Wang K, Yue YF, Sun RQ, Zhang RM, et al. Association of Ang-2, vWF, and EVLWI with risk of mortality in sepsis patients with concomitant ARDS: a retrospective study. J Formos Med Assoc. 2020;119(5):950–6.
Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436(7047):112–6.
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 Pt 1):818–24.
Guerin C, Papazian L, Reignier J, Ayzac L, Loundou A, Forel JM, et al. Effect of driving pressure on mortality in ARDS patients during lung protective mechanical ventilation in two randomized controlled trials. Crit Care. 2016;20(1):384.
Reilly JP, Calfee CS, Christie JD. Acute respiratory distress syndrome phenotypes. Semin Respir Crit Care Med. 2019;40(1):19–30.
Fowler AA 3rd, Truwit JD, Hite RD, Morris PE, DeWilde C, Priday A, et al. Effect of vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: The CITRIS-ALI Randomized Clinical Trial. JAMA. 2019;322(13):1261–70.
Ambrosino N, Makhabah DN. Comprehensive physiotherapy management in ARDS. Minerva Anestesiol. 2013;79(5):554–63.
Rezoagli E, Magliocca A, Catenacci SS. Identification of biological phenotypes in acute respiratory distress syndrome. From biomarkers to clinical outcome. Am J Respir Crit Care Med. 2018;197(9):1209–11.
Sjoding MW, Hofer TP, Co I, Courey A, Cooke CR, Iwashyna TJ. Interobserver reliability of the Berlin ARDS definition and strategies to improve the reliability of ARDS diagnosis. Chest. 2018;153(2):361–7.
Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38(10):1573–82.
Chen Y, Lu GP. Advances in the diagnosis and treatment of pediatric acute respiratory distress syndrome. Zhongguo Dang Dai Er Ke Za Zhi. 2018;20(9):717–23.
Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA. 2018;319(7):698–710.
Kopp R, Breuer T. Electrical impedance tomography, useful bedside monitoring for severe acute respiratory distress syndrome? Minerva Anestesiol. 2020. https://doi.org/10.23736/S0375-9393.20.14867-3.
Hagaman JT, Rouan GW, Shipley RT, Panos RJ. Admission chest radiograph lacks sensitivity in the diagnosis of community-acquired pneumonia. Am J Med Sci. 2009;337(4):236–40.
Pradhan S, Shrestha PS, Shrestha GS, Marhatta MN. Clinical impact of lung ultrasound monitoring for diagnosis of ventilator associated pneumonia: a diagnostic randomized controlled trial. J Crit Care. 2020;58:65–71.
Bouhemad B, Dransart-Raye O, Mojoli F, Mongodi S. Lung ultrasound for diagnosis and monitoring of ventilator-associated pneumonia. Ann Transl Med. 2018;6(21):418.
Wang XT, Ding X, Zhang HM, Chen H, Su LX, Liu DW, et al. Lung ultrasound can be used to predict the potential of prone positioning and assess prognosis in patients with acute respiratory distress syndrome. Crit Care. 2016;20(1):385.
Zhao Z, Jiang L, Xi X, Jiang Q, Zhu B, Wang M, et al. Prognostic value of extravascular lung water assessed with lung ultrasound score by chest sonography in patients with acute respiratory distress syndrome. BMC Pulm Med. 2015;15:98.
Acknowledgements
None.
Funding
The study was supported by Key projects of Education Department of Anhui Province (KJ2019A0382).
Author information
Authors and Affiliations
Contributions
RW, BQ, XZ, LM: data curation, data analysis, drafting of the article, final approval of the version to be published. XW: study supervision, coordination, funding support, design of this study, drafting of the article, final approval of the version to be published. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the First Affiliated Hospital of Bengbu Medical College. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for publication
All participants have given consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, R., Qi, B., Zhang, X. et al. Prophetic values of lung ultrasound score on post-extubation distress in patients with acute respiratory distress syndrome. Eur J Med Res 27, 27 (2022). https://doi.org/10.1186/s40001-022-00652-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-022-00652-9