Abstract
Diabetes mellitus is a widespread endocrine disorder, which is categorized as the fourth leading cause of global mortality. Allopathic medicine has yet to provide a satisfactory cure for this condition. Consequently, there is an urgent demand for innovative antidiabetic treatment approaches with enhanced management and minimum side effects and costs. The study investigated the synergistic antidiabetic potential of combining selenium nanoparticles (Se NPs) and plasma-rich platelets (PRP) in diabetic mice. Antidiabetic activity of the proposed combination (Se NPs and PRP) was evaluated from histopathological and biochemical perspectives. The experiment involved alloxan monohydrate induced diabetic mouse model. In the in vivo study, several biochemical parameters for assessing the antidiabetic effect of the novel combination of (Se NPs and PRP) were performed such as blood glucose levels, body weight, lipid profiles, and liver damage markers (AST and ALT). Scavenging antioxidant activity was assessed by evaluation levels of hepatic and renal GSH, MDA, SOD, and CAT activities. Complete histopathological examinations of vital internal organs were carried out. Results revealed that combining Se NPs and PRP presents a novel approach for better diabetes management and reduced complications associated with the disease. These findings have therapeutic implications for managing diabetes mellitus.
Similar content being viewed by others
Introduction
Selenium (Se) is an essential element in our diet. It may improve the symptoms of diabetes [1]. According to Hwang and colleagues, selenium (Se) in diabetic mice functions similarly to insulin. It modulates the activity of enzymes that are crucial for gluconeogenesis and glycolysis, and it aids in the transport of glucose into cells [2]. However, poisoning could happen if Selenium blood levels are raised. As opposed to selenomethionine or selenite, Se NPs are more biocompatible, with higher affinity, and have no or low toxicity. Se nanoparticles also exhibit high permeability, intestinal absorption, and antioxidant activities. The antioxidant activity is due to the single-step reduction from selenium atom to selenide anion. Such reduction is required to activate redox cycling with oxygen to produce Reactive Oxygen Species (ROS) [3]. Currently, one of the scientific disciplines with the most cutting-edge discoveries is nanotechnology [4, 5]. Its transdisciplinary character benefits various fields by making molecular and atomic engineering possible [6, 7].
Recent years have seen a lot of interest in plasma. One of the diabetes treatments that uses a cutting-edge strategy for cell regeneration is (PRP). A large number of bioactive molecules, the majority of which are platelet-derived growth factor (PDGF) protein, transforming growth factor (TGF-), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), insulin-like growth factor (IGF), and fibroblast growth factor (FGF), are present in PRP, which can speed up cell proliferation. Diabetes Mellitus (DM), a metabolic disease caused by the pancreas’s inability to produce insulin, particularly in -cells, causes an increase in blood glucose levels (hyperglycemia). Insulin resistance causes hyperglycemia because it interferes with the transfer of GLUT-4 from the cell to the plasma membrane, which prevents the cell from receiving the glucose regulation mechanism [8, 9]. Exogenous insulin delivery is replaced by pancreas or islet transplantation [10]. However, this method has a lot of drawbacks, such as the risk of significant invasive surgery and the adverse effects of immunosuppressive medications [11]. Accordingly, developing alternative techniques for generating cells from endogenous sources became a necessity to avoid issues with tissue matching during surgery and transplants. To this point, a variety of renewal procedures have been investigated for causing -cell regeneration, including activating residual-cell proliferation (neo-genesis), creating islets from scratch using pancreatic progenitor cells, and transdifferentiating and converting non-cells in the pancreas into cells. The easiest, most direct, and least invasive way to increase cell mass is through this induction technique.
Growth Factors (GFs) are naturally occurring biological mediators that control cell division and growth and play a role in tissue regeneration and repair [12]. A recent study found that chronic injection of low-dose EGF-induced ductal cell neogenesis and cell differentiation in DM mice [13]. The majority of GF is produced by platelets [14].
PRP is a procedure that delivers significant amounts of autologous GF [15]. Three to five times as many autologous platelets as whole blood platelets are present in PRP [16]. A relatively new regenerative medicine technique called PRP therapy has received a lot of attention lately [17]. Red, white, and platelet blood cells are all present in platelet-rich plasma (PRP), a blood product. Organic and inorganic molecules and ions that make up plasma together carry out the actions of other substances. Plasma that is rich in platelets is extracted via centrifugation. In PRP, platelets are 20 times more plentiful and have a higher protein content than in blood. PRP can speed up healing since it includes bioactive substances that are known to act as growth factors in tissues [18, 19]. El Tahawy and colleagues have demonstrated that using PRP in treating DM rats for the pancreas organ regeneration response can stimulate the growth of new lobes and initiate tissue, ductal cell, and cell repair or creation of acinar cells [20]. The most prevalent growth factor in PRP is the platelet-derived growth factor (PDGF). Simultaneously, PDGF functions mitogenically and chemotactically to activate angiogenic cells and produce mesenchymal cells, which are then stimulated by Transforming GF- to proliferate fibroblasts and boost collagen in the tissue. Then, Fibroblast Growth Factor (FGF) causes an increase in fibroblast proliferation after Insulin-Like Growth Factor (IGF) boosts collagen synthesis, differentiation, and proliferation of fibroblasts, while Vascular Endothelial Growth Factor (VEGF) promotes angiogenesis and tissue regeneration. Numerous medical research studies have discovered PRP as a therapeutic approach. Particularly in diabetic diseases, PRP may help to improve structural changes in the endocrine pancreas during recovery [6, 21].
In a recent study conducted by Karas et al. in 2024, it was found that the combination of Se NPs (selenium nanoparticles) and PRP (platelet-rich plasma) has shown promising potential in modulating wound healing in diabetic mice. This discovery has motivated us to further investigate the potential antidiabetic effects of this combination and explore any histological changes in internal organs resulting from the treatment. Previous research has indicated the antidiabetic properties of Se NPs, while PRP has been recognized as an effective approach for reducing blood glucose levels in the treatment of diabetes mellitus [6,7,8,9]. The novelty of our study lies in the combination of Se NPs and PRP. Additionally, we have conducted a comprehensive histopathological examination of vital internal organs, including the liver, kidney, pancreas, heart, lung, spleen, and brain. It is worth noting that most studies focusing on antidiabetic activity typically only examine the pancreas, liver, and kidney. Furthermore, we have utilized two special stains, Masson’s trichrome and aldehyde fuchsin, in addition to the routine stain (Hematoxylin and eosin H&E), for assessing certain tissues. The objectives of the study are to evaluate the antidiabetic properties of selenium nanoparticles (Se NPs) / plasma-rich platelets (PRP) combination in a diabetic mouse model, to monitor the impact of Se NPs and PRP on various physiological parameters in diabetic mice, including blood glucose levels, body weight, and lipid profiles, to assess liver functions by measuring enzyme markers of liver damage, such as AST and ALT, and to determine the antioxidant status of diabetic mice by measuring levels of hepatic and renal glutathione (GSH), malondialdehyde (MDA), superoxide dismutase (SOD), and catalase (CAT). Also, to conduct histopathological examinations of multiple organs to observe the therapeutic effects of Se NPs and PRP at the tissue level.
The research investigating the synergistic antidiabetic potential of combining selenium nanoparticles (Se NPs) and platelet-rich plasma (PRP) is motivated by addressing multiple problems associated with diabetes mellitus. By exploring this novel combination, the study aims to tackle several challenges in diabetes management, thereby making the findings more relevant and impactful. Diabetes mellitus is a chronic condition for which allopathic medicine has not yet provided a satisfactory cure. The research seeks to contribute to the development of innovative and effective antidiabetic treatments that can improve patient outcomes. One of the primary goals of the study is to identify new approaches for better diabetes management. By investigating the combination of Se NPs and PRP, the research aims to discover potential strategies that can complement or enhance existing treatment modalities, leading to more effective glycemic control and improved overall management of the disease. Another critical problem in antidiabetic therapy is the occurrence of side effects associated with certain medications or interventions. By exploring the use of Se NPs and PRP, the study seeks to identify a treatment approach that offers the potential for minimal side effects, thereby improving patient safety and tolerability. Diabetes management can be financially burdensome for individuals and healthcare systems. The research aims to explore an innovative treatment approach that may offer cost-effectiveness compared to current therapies, potentially reducing the economic burden associated with diabetes management. By addressing these multiple problems, the findings of the research can have direct relevance and impact in the field of diabetes management. The study aims to provide insights into a novel approach that may offer improved glycemic control, reduced complications, enhanced patient safety, and potentially more cost-effective treatment options for individuals living with diabetes mellitus.
Results
Characterisation of Se NPs/PRP combination
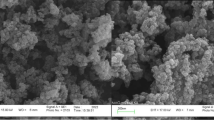
The TEM analysis revealed that the Se NPs are spherical with an average size of about 31.6 ± 1.3 nm (Fig. 1A). The reaction between sodium selenite and ascorbic acid reduced the selenium to its elemental form (Se0), which was evident from the solution’s colour transition from clear to orange, signifying the reduction process and the creation of Se NPs. When combined with PRP, the Se NPs showed a slight increase in size to approximately 35 ± 0.6 nm (Fig. 1B). This combination also caused a shift in the UV-visible absorption spectrum, with the peak absorbance moving from 258 nm for Se NPs alone to 273 nm for the Se NPs/PRP complex, while PRP alone had peak absorbance at 287 nm and 412 nm (Fig. 1C).
The FTIR spectrum of Se NPs (Fig. 2A) displayed peaks corresponding to various functional groups: hydroxyl groups (OH) in water at 3438 cm− 1, cyanide groups (CN) in polyvinylpyrrolidone (PVP) at 2034 cm− 1, carbonyl groups (C = O) in PVP at 1635 cm− 1, amide groups in PVP at 1116 cm− 1, and selenium-oxygen (Se-O) bonds at 690 cm− 1. The purified PRP, characterized separately, showed strong hydroxyl group absorption between 3000 and 3500 cm− 1 and ether signals (C-O-C) in sugar units at 2800 to 2950 cm− 1, with an additional band related to aliphatic hydrogen at 1050 to 1150 cm− 1. The Se NPs and PRP combination introduced new peaks in the same range at 2800–2950 cm− 1 as the ether signals of PRP, indicating an interaction between them. The XRD analysis of the Se NPs (Fig. 2B) confirmed the crystalline structure of the Se NPs. Sharp peaks were observed at specific angles 23.63º, 30.04º, 41.23º, 44.46º, 45.71º, 52.01º, and 56.49º corresponding to well-defined crystal planes (100), (101), (110), (102), (111), (200), (201), and (003) in hexagonal selenium. These peaks match those found in the standard reference card for hexagonal selenium. When combined with PRP, the Se NPs did not exhibit any significant changes in their XRD pattern. This is expected as XRD is not typically used for analysing PRP, which is a complex biological mixture that does not produce clear XRD patterns. The Se nanosuspension demonstrated a zeta potential of + 44 mV (Fig. 2C), indicating a stable suspension. In contrast, PRP alone had a zeta potential of -14 mV (Fig. 2D). However, when Se NPs were combined with PRP, the zeta potential was + 16.8 mV (Fig. 2E), suggesting a moderately stable suspension according to the criteria from Colorado State University. This moderate stability may be due to the interaction between the surface coating of Se NPs and the various components in PRP, which can affect the overall surface charge. Factors such as the pH and ionic strength of the suspension medium can also influence the zeta potential, with lower pH or higher ionic strength typically reducing the zeta potential’s magnitude.
The effect of Se NPs / PRP combination on weight, in diabetic mice. Until day 7, there was no discernible weight change across all groups. However, Group 1 exhibited a slight, positive trend towards better health. Conversely, Group 2 displayed a significant downward trend in weight. Groups 3 and 4 demonstrated a moderate decrease in weight. On the other hand, Groups 5, 6, and 7 experienced a negligible decline in weight
Body weight
There was no noteworthy change in body weight of all the groups until the 7th day of treatment (Fig. 3). After 2 weeks, group 2 (the diabetic untreated mice) showed significant body weight loss as compared to normal control due to insulin deficiency and severe hyperglycemia. The body weight of group 2 continued to decrease steadily. Groups 3 and 4 showed less weight loss than group 2. Group 1 showed a non-significant healthy upward trend. There were no obvious differences between the drug-administered groups (5, 6, and 7) with trivial weight loss which reflects improvement in blood sugar levels. The results indicated that Se NPs/PRP groups showed better results than Se NPs or PRP, separately on physiological indexes in diabetic mice.
Blood sugar
Initially, the blood glucose levels in groups 2–7 were elevated above 200 mg/dL, in contrast to normal control (group 1), which consisted of healthy, non-diabetic mice (Fig. 4). After two weeks, a reduction in blood glucose was observed in the groups from 4 to 7. The treatment with Se NPs-PRP did not exhibit a dose-dependent effect on glucose levels, as the response was similar across different dosages (Se NPs: PRP ratios of 2:1 and 1:2), indicating that the lowest dose (75 microns) was sufficient to achieve the maximum effect. However, the effectiveness of glucose reduction was dependent on the duration of treatment, with the most significant impact observed after two weeks. The most notable improvements were seen in groups 5, 6, and 7, with blood glucose levels recorded at 168.89, 159.98, and 165.12 mg/dL, respectively. Meanwhile, group 4 experienced a modest decrease in blood glucose levels, with readings of 191.03 mg/dL.
Lipid profile
In comparison to the other groups, Group 2 exhibited the highest levels of cholesterol (Chol.) and triglycerides (TG). The administration of selenium nanoparticles combined with plasma-rich platelets (Se NPs/PRP) led to a reduction in both Chol. and TG levels, as detailed in Fig. 5. The decrease in Chol. was significant in groups 5, 6, and 7 compared to the positive control group (group 2). However, the decrease in Chol. and TG was insignificant in the groups 3 and 4. Conversely, administering Se NPs and PRP individually resulted in only a marginal reduction in Chol. and TG levels.
displays the impact of Se NPs - PRP on the lipid profile of diabetic mice, specifically measuring plasma cholesterol and triglyceride levels. Among the groups, Group 2 exhibited the highest levels of both cholesterol and triglycerides. Conversely, Groups 5, 6, and 7 demonstrated significant decreases in cholesterol and triglyceride levels. Groups 3 and 4, on the other hand, showed slight reductions in cholesterol and triglyceride levels
Liver functions test
Liver function tests are commonly used in medical settings to screen for liver conditions. These tests typically measure serum aminotransferases, alkaline phosphatase, bilirubin, albumin, and prothrombin time. Chronic hyperinsulinemia can raise transaminase levels and increase the liver’s susceptibility to insulin resistance. This is frequently caused by insulin’s incapacity to accurately indicate an elevation in insulin receptor substrate-2. Additionally, there is an upregulation of sterol regulatory element-binding protein 1c (SREBP-1c), which leads to increased lipogenesis. However, despite a reduction in insulin receptor substrate-2-mediated insulin signaling in states of insulin resistance, the activation of SREBP-1c and the subsequent stimulation of new fat production within the liver can increase the internal levels of triglycerides, contributing to the development of a fatty liver. This process also enhances the assembly and secretion of very low-density lipoproteins (VLDL). Therefore, hyperinsulinemia can directly cause hepatic insulin resistance accompanied by fatty alterations in the liver.
According to Fig. 6 (A)., the ALT and AST activities in group 1 (the normal control group) were measured at 99.51 and 125 U/L, respectively. Groups 2 and 3 experienced a severe increase in both ALT and AST levels, while groups 4, 5, 6, and 7 showed a moderate increase in these enzyme activities. In groups 5, 6, and 7, the SOD, CAT, and GSH activities were similar to those of the normal control group, indicating high antioxidant activity (Fig. 6 (C&D)). The GSH-Px level in group 3 showed a mild improvement There were no significant differences observed in the MDA levels in groups 5, 6, and 7, as their values were close to those of group 1 (Fig. 6 (B)). However, group 2 exhibited a remarkable increase in the MDA level, reaching 6.16 µmol/l.
Kidney function test
In this study, the levels of urea and creatinine were measured as biochemical parameters. The administration of Se NPs-PRP significantly reduced both urea and creatinine levels in groups 4, 5, 6, and 7 compared to group 2 (diabetic untreated), as shown in Fig. 7. Total protein and albumin showed a slight decrease in groups 4, 5, 6, and 7, and a moderate decrease in group 2 and 3. These results were consistent with the moderately increased urine albumin levels in groups 4, 5, 6, and 7 (Fig. 7 (A)). The activities of SOD and CAT are presented in Fig. 7 (C). The administration of Se NPs-PRP appeared to restore normal SOD activity. Groups 5, 6, and 7 exhibited high SOD levels (14.98, 15.5, and 16 U/mg protein) close to the control group (18.77 U/mg protein). Groups 3 and 4 showed slight improvement. The antioxidant activity of PRP and Se NPs administered separately was lower than that of Se NPs-PRP. The analysis of MDA levels revealed that groups 5, 6, and 7 had values similar to group 1 (control group), while there was a significant increase in groups 2 and 3(Fig. 7 (B)).
The effect of Se NPs / PRP combination on liver function test and oxidative stress in diabetic mice. (A) ALT and AST levels significantly increased in Groups 2, 3, and 4. In contrast, Groups 5, 6, and 7 showed moderate increases in ALT and AST levels. (B) Group 2 exhibited a severe increase in MDA levels, suggesting higher oxidative stress. However, Groups 4, 5, 6, and 7 displayed improved MDA levels, indicating a reduction in oxidative stress. C & D) The SOD and CAT activities in Groups 5, 6, and 7 were comparable to those in Group A, indicating similar antioxidant enzyme levels. Additionally, GSH levels in Groups 5, 6, and 7 showed a moderate increase, suggesting enhanced antioxidant defense
The effect of Se NPs / PRP combination on kidney function tests, oxidative stress, and urinary analysis in diabetic mice. (A) Groups 4, 5, 6, and 7 exhibited enhanced renal functions, as evidenced by improvements in parameters such as creatinine, uric acid, albumin, total protein, and urine albumin. (B) Groups 5, 6, and 7 demonstrated significant improvements in MDA levels, indicating a decrease in oxidative stress. (C) There was a noticeable increase in the activities of SOD, GSH, and CAT in Groups 5, 6, and 7, suggesting enhanced antioxidant defense mechanisms
Histopathological findings
Liver
In Group 1, which served as the normal control, the liver’s portal vein and sinusoids were free from any abnormal changes, maintaining a healthy hepatic structure (Fig. 8 (1 L)). Conversely, the liver samples from Group 2, the positive control, exhibited widespread hydropic degeneration of hepatocytes and signs of microvesicular steatosis (Fig. 8 (2La&b)). These changes were characterized by irregular and partially rounded vacuoles within the hepatocyte cytoplasm, alongside congestion in the central vein. Additionally, mild fibrosis and infiltration of inflammatory cells were noted in the portal areas (Fig. 8 (2Lc)). The Masson Trichrome stain highlighted this fibrosis, showing blue collagen fibers within the portal tract (Fig. 8 (2Ld)). In contrast, these pathological features were less pronounced in the livers of mice from treated Groups 3 and 4, where only localized hydropic degeneration and limited portal tract inflammation were observed (Fig. 3 (3 L)). Similarly, Groups 5, 6, and 7 displayed only localized hydropic degeneration, indicating a reduction in liver pathology due to the treatment (Fig. 8 (4 L)).
(1 L): Normal hepatic architecture with no obvious abnormal changes (Group 1), H&E stained (X 400 original magnification). 2La: Extensive hydropic degeneration in hepatocytes and microvesicular steatosis with congestion in the central vein in the liver in (Group 2), H&E stained (X 200 original magnification). 2Lb: Extensive hydropic degeneration in hepatocytes and microvesicular steatosis in the liver in (Group 2), H&E stained (X 400 original magnification). 2Lc: Mild fibrosis, and inflammatory cell infiltration were detected in portal areas in the liver (in Group 2), H&E stained (X 400 original magnification). 2Ld: Mild fibrosis in portal areas in the liver (in Group 2), Masson trichrome stained (X 400 original magnification). 3 L: Hydropic degeneration and focal portal tract inflammation in the liver in (Groups 3&4), H&E stained (X 400 original magnification). 4 L: Focal hydropic degeneration in the liver in (Groups 5, 6 & 7), H&E stained (X 400 original magnification)
Kidney
In the study, Group 1, which served as the normal control, exhibited typical kidney histology (Fig. 9 (1 K)). Group 2, the positive control, showed various kidney abnormalities, including thickened basement membranes, cell death, and swelling of the tubular epithelial cells. Additionally, bleeding and localized inflammation of the kidney interstitium were observed (Fig. 9 (2Ka, b & c)). The glomeruli displayed slight enlargement, increased cellularity, and localized cell death. In contrast, Groups 3 and 4, which received treatment, showed only mild swelling in the tubular epithelial cells, along with slight inflammation and expansion of the mesangial cells (Fig. 9 (3 K)). Notably, Groups 5, 6, and 7 demonstrated considerable improvement, with healthier tubular structures (Fig. 9 (4 K)).
1 K: Normal histological features of kidney in (Group 1), H&E stained (X 400 original magnification). 2Ka: Tubular epithelial hydropic degeneration, necrosis, basement membrane thickening, focal interstitial nephritis, and interstitial hemorrhage were seen. Glomeruli revealed focal necrosis, mild mesangial expansion, and focal hypercellularity in the kidney (Group 2), H&E stained (X 400 original magnification). 2Kb: Glomeruli revealed mild mesangial expansion and focal hypercellularity in the kidney (Group 2), H&E stained (X 400 original magnification). 2Kc: Glomeruli revealed focal necrosis [black arrow] and Tubular epithelial hydropic degeneration in the kidney [black arrowhead] (Group 2), H&E stained (X 400 original magnification). 3 K: Mild hydropic degeneration in some parts of the tubular epithelial cells with mild inflammation and mild mesangial expansion (Groups 3 & 4), H&E stained (X 400 original magnification). 4 K: Improved tubules and glomeruli in the kidney (Groups 5, 6 & 7), H&E stained (X 400 original magnification)
Pancreas
In the normal control group (Group 1), it was noted that the islets of Langerhans were big and regular with a normal histologic appearance (Fig. 10 (1P)). The most notable alteration seen in the positive control group (Group 2) is a notable decrease in the width of islet cells, accompanied by a noticeable loss of cells (Fig. 10 (2 Pa&b)). The Aldehyde Fuchsin Stain was used to highlight these changes through the absence of purple to violet insulin granules in islets of Langerhans (Fig. 10 (2Pc)). A mild improvement was observed in the islet of Langerhans in the treated groups 3 and 4 (Fig. 5 (3P)). On the other hand, there is marked improvement and restoration of healthy islets of Langerhans in treated groups 5, 6, and 7) (Fig. 10 (4P)).
1P: Normal histological appearance of islets of Langerhans with an average diameter in the pancreas in Group 1, H&E stained (X 200 original magnification). 2 Pa: Significant reduction in diameter of islet cells in the pancreas in group 2, H&E stained (X 200 original magnification). 2Pb: Significant reduction in diameter of islet cells with marked cell loss in the pancreas in group 2, H&E stained (X 400 original magnification). 2Pc: Absence of purple to violet insulin granules in islets of Langerhans in the pancreas in group 2, Aldehyde fuchsin stained (X 400 original magnification). 3P: Mild improvement was observed in the islet of Langerhans in treatment (Group 3 & 4), H&E stained (X 200 original magnification). 4P: Marked improvement and restoration of healthy islets of Langerhans with average normal diameter (Groups 5, 6 &7), H&E stained (X 200 original magnification)
Heart
In the histological examination of the heart, Group 1, which served as the normal control, displayed typical heart tissue structure with cardiomyocytes of regular size. These cells featured single, oval nuclei situated centrally and were surrounded by well-organized cardiac muscle fibers (Fig. 11 (1 H)). In contrast, Groups 3 to 7 exhibited a slight disorganization in the arrangement of cardiac muscle fibers when compared to Group 1, which was indicative of protein degradation associated with diabetes mellitus (Fig. 11 (2 H)). Additionally, Group 2, which was the positive control, showed a marked increase in blood vessel density and signs of congestion within the heart tissue (Fig. 11 (2 H)).
1 H: Normal histological features and normal cardiomyocyte sizes with single, oval, and centrally located nuclei with regularly arranged cardiac myofibres in group 1, H&E stained (X 40 original magnification. 2 H: Myocardial fibers disarray in groups 2, 3, 4, 5, 6 & 7, H&E stained (X 40 original magnification). 3 H: More vasculature and congestion in the myocardium in group 2, H&E stained (X 40 original magnification)
Lung
In the histological examination of the lungs, Group 1 (the normal control) displayed standard lung tissue structure (Fig. 12 (1G)). Group 2 (the positive control) exhibited signs of congestion within the lung tissue (Fig. 12 (2Ga)). Furthermore, this group also presented with inflammation and changes indicative of emphysema (Fig. 12 (2Gb)). In contrast, Groups 3 through 7 showed only the presence of emphysematous alterations, with a complete resolution of inflammation and congestion noted (Fig. 12 (3G)).
Brain and spleen
Figure 13 (1B) showed that there are no particularly abnormal alterations in brain histology across all groups. The spleen sections showed a normal microscopic image in every group (Fig. 13 (1 S)), excluding the mild congestion in the positive control group’s spleen (Group 2) (Fig. 13 (2 S)).
1G: Normal histological features of the lung seen in (Group 1), H&E stained (X 20 magnification). 2G: Congestion in the lung (Group 2), H&E stained (X 20 original magnification. Emphysematous changes and inflammation in lung (Group 2), H&E stained (X 20 original magnification). (3G): Emphysematous changes with the total improvement of inflammation and congestion in Groups 3, 4, 5, 6, and 7, H&E stained (X 20 original magnification)
Discussion
The study investigated a range of key parameters to comprehensively evaluate the antidiabetic potential of the combination of Se NPs and PRP. These parameters were carefully selected based on their relevance to diabetes management and their potential to provide valuable insights into the therapeutic effects of the novel combination.
The primary parameters assessed in the study included: Measurement of blood glucose levels is a fundamental indicator of diabetes and its management. Monitoring changes in blood glucose levels after treatment with Se NPs and PRP helps assess the antidiabetic effect of the combination. Changes in body weight can reflect alterations in metabolic processes and overall health. Monitoring body weight provides valuable information on the impact of the treatment on weight management in diabetic mice. Diabetes is often associated with dyslipidemia, characterized by abnormal lipid levels in the blood. Evaluating lipid profiles, including cholesterol and triglyceride levels, helps assess the lipid-regulating effects of the combination treatment. Diabetes can contribute to liver dysfunction and damage. Assessment of liver damage markers, such as aspartate aminotransferase (AST) and alanine aminotransferase (ALT), provides insights into the potential hepatoprotective effects of the combination treatment.
In addition to these parameters, the study also evaluated the scavenging antioxidant activity by measuring the levels of hepatic and renal glutathione (GSH), malondialdehyde (MDA), superoxide dismutase (SOD), and catalase (CAT) activities. These parameters offer insights into the antioxidant defence mechanisms and oxidative stress status in the treated diabetic mice. Regarding the choice of these specific parameters, they represent key aspects of diabetes management and are commonly used in preclinical studies to assess the efficacy and safety of antidiabetic interventions. However, it is important to note that the selection of parameters can vary depending on the research objectives and experimental design. It is worth noting that the sensitivity of these parameters and their impact on the results can be influenced by various factors, including the characteristics of the diabetic mouse model, administration protocols, dosage of Se NPs and PRP, and the duration of the study. To establish the robustness and generalizability of the findings, it is important for future studies to explore the sensitivity of these parameters and potentially investigate alternative parameter sets to further elucidate the effects of the combination treatment on diabetes management and associated complications.
The Histochemical outcomes demonstrated that Se NPs/PRP has notable hypoglycemia effects at all three doses stated. AST serum concentration dropped a substantial increase in the maximum dose. When compared to the diabetic control group, the minimal dose dramatically reduced the serum level of albumin. The serum creatinine level was significantly lower in groups 4, 5, 6, and 7. Insulin resistance in organs such as the liver, skeletal muscle, and adipose tissue is a hallmark of the onset of diabetes mellitus. This leads to hyperglycemia, changed lipid profiles, and an increased risk of coronary heart disease. Selenium has a detrimental influence on diabetes to the point where a rise in serum selenium levels increases the chance of developing diabetes mellitus [22]. In contrast, some studies demonstrate selenium’s protective role in the Fig8t against diabetes [23,24,25]. In these studies, non-diabetics were shown to have greater serum selenium levels, whereas diabetics were found to have lower serum selenium levels. In this investigation, blood glucose levels significantly decreased while receiving treatment with Se NPs/PRP compared to the diabetic untreated mice as Se NPs mediate the actions of insulin. Several theories have been proposed to explain how selenium lowers blood sugar (hypoglycemia). Firstly, through its antioxidant activity, selenium can significantly improve diabetes by reducing oxidative stress and lipoprotein oxidation. Secondly, numerous studies have proposed that selenium has a variety of impacts on the control of blood sugar, including pyruvate metabolism, glycolysis, and insulin signaling. Finally, sodium selenite stimulates glucose uptake in fat cells isolated from rats [26].
The liver is essential for the metabolism of glucose and free radical detoxification. Elevated blood sugar is linked to liver damage. AST and ALT are examples of transaminase. Alloxan is found to be selectively toxic to liver hepatocytes and induces liver injury, which results in the spilling of AST, ALT, and ALP enzymes from the cytosol of enlarged liver into the circulation, leading to an increase of these enzymes in serum [27, 28].
In this study, ALP levels dropped in the groups treated with Se NPs. However, the modifications were not substantial. In groups 4, 5, 6, and 7 the levels of AST declined, but the changes were not substantial. By prolonging treatment until 28 days, a considerable drop in all liver enzyme values is observed. Al-Quraishy et al.‘s findings confirmed the importance of selenium in eliminating free radicals and enhancing liver function. This occurs by restoring elevated serum levels of AST, ALT, and ALP to normal levels [29]. Se NPs had a positive impact on hepatic steatosis. As is shown in Fig. 8 (2 L), there was a high degree of steatosis with severe cytoplasmic vacuoles, bleeding, and swelling of hepatocytes in group 2 (positive control) [30]. Figure 3(3 L & 4 L) of groups 3, 4, 5, 6, and 7 showed less fat deposition in hepatocytes and improvement of steatosis related to the control group. In addition, the diabetic control group as shown in Fig. 0.8 (1 L) showed extensive hydropic degeneration in hepatocytes, microvesicular steatosis, mild fibrosis, and inflammatory cell infiltration [29]. These findings were found to be mildly decreased in the liver of mice in groups 3 & 4 and significantly decreased in groups 5, 6, and 7 (Fig. 0.8 (3&4 L)). These changes in the diabetic control group are nearly the same obtained by studies [31, 32]. The improvement of liver histopathological changes in treatment groups is also observed in the literature [33,34,35] in which histopathological examination of the liver revealed a significant number of repair changes in treated diabetic animals compared to the untreated ones.
According to Nabi et al., diabetes also results in renal impairment and elevated serum levels of urea, creatinine, and uric acid. According to the study’s findings, compared to diabetic controls, serum albumin levels fell in groups 4, 5, 6, and 7 [36]. This decrease was more pronounced in the groups 6 and 7. In comparison to group 2 (diabetic untreated mice), serum creatinine levels were reduced in all four groups receiving selenium nanoparticles, groups 4, 5, 6, and 7 experienced a sizable drop in this amount. A remarkable decrease was observed in group 6 (1.4 mg/dl). In the same way, urea levels were reduced in all four groups receiving Se NPs. In group 6, this reduction was more pronounced (30.3 mg/dl), according to the study [34]. The treatment with selenium nanoparticles improves and decreases the elevated level of urea and creatinine in diabetic-induced rats. These findings are compatible with the findings of this study.
Based on the findings of this investigation, the kidney had interstitial bleeding, necrosis, tubular epithelial hydropic degeneration, and thickening of the basement membrane. As seen in Fig. 9(2k), the diabetic control group had localized necrosis, modest mesangial enlargement, and focal hypercellularity compared to the control group, Fig. 9 (1k). These outcomes were significantly reduced in the treatment groups due to improved tubules and glomeruli, Fig. 4(3&4k). According to Cruz et al., a diabetic group that was not receiving treatment had nearly identical histological results that showed symptoms of nephropathy with widespread mesangial expansion [31]. The findings align with the research conducted [33,34,35], which all demonstrated that the treatments provided protective effects on kidney function, helping to restore normal conditions in tubular cells and glomerular structures.
The pancreatic islets of Langerhans significantly improved in treated groups (3, 4, 5, 6, and 7), Fig. 10(3&4P), compared to untreated diabetic mice (group 2), Fig. 10 (2P). This is consistent with findings published by Monday et al., who discovered that treated groups had recovered their pancreatic B cells [37]. This is also in agreement with a study done by Safitri et al. [34]. On the other hand, Qazi et al., noted hypertrophy and vacuolations of Langerhans β cells, little recovery, and hemorrhage in different treatment groups [33].
In the cardiac section, there was more vasculature, congestion, and slight cardiac myofiber disarray in the diabetic untreated mice group Fig. 11 (2 H), compared to the control group Fig. 11 (1 H). This observation is consistent with that reported by Cruz et al., who found heart tissue histology did not reveal major differences between the different groups [31]. However, SeNPs treated diabetic mice groups Fig. 11 (3 H) showed normal cardiac myofiber disarray without any significant morphological disruptions in comparison to control.
The lung showed congestion, inflammation, and emphysematous in a diabetic untreated group Fig. 12 (2G), with total improvement in treated groups Fig. 12 (3G) related to the control group Fig. 12 (1G). Interestingly, there were no remarkable histopathological changes in brain and spleen histology between different groups (Fig. 13).
The findings of the research indicate that a combination of selenium nanoparticles (Se NPs) and plasma-rich platelets (PRP) could be an effective therapeutic approach for diabetes. This potential treatment appears to enhance the body’s biochemical balance and strengthen its inherent antioxidant mechanisms.
This study investigated the potential of combining selenium nanoparticles (Se NPs) with plasma-rich platelets (PRP) for treating diabetes. In diabetic mice, Se NPs/PRP treatment effectively reduced blood sugar levels, cholesterol, and triglycerides. Additionally, markers of kidney and liver function improved, as shown by decreased levels of urea, creatinine, ALT, and AST enzymes. Since a balance between antioxidants and oxidants is crucial in diabetes management, the study also observed an increase in antioxidant activity with Se NPs treatment. Histological analysis further supported these findings, suggesting potential therapeutic benefits. These promising results highlight the significance of Se NPs/PRP as a novel approach to manage diabetes by restoring biochemical balance and enhancing the body’s natural defenses.
Materials and methods
Preparation of Se NPs/PRP combination
Se NPs were synthesized using a straightforward wet chemical technique. Initially, 100 mg of polyvinylpyrrolidone was dissolved in 40 mL of deionized water, with the mixture being stirred continuously. Next, 600 mg of ascorbic acid was introduced to the solution and stirred for an additional 5 min. Following this, 1mL of a 0.96 g/mL cetyltrimethylammonium chloride solution was added to the mix. After stirring for another 5 min, 1mL of a 0.25 M sodium selenite solution was added gradually, drop by drop, leading to a color transition in the solution from clear to orange [23, 38].
To prepare PRP, a healthy cohort of mice was utilized for whole blood collection. The blood was drawn via venipuncture and collected in acid citrate dextrose (ACD) tubes, which were then kept at room temperature. This was followed by a gentle centrifugation process. The supernatant, which contained the platelets, was then moved to a new sterile tube that lacked anticoagulant and subjected to a more vigorous centrifugation. The upper two-thirds of the tube, containing platelet-poor plasma (PPP), was discarded, leaving the concentrated PRP in the bottom third of the tube [6].
Characterization of Se NPs/ PRP combination
The process for preparing and analysing selenium nanoparticles (Se NPs) combined with plasma-rich platelets (PRP) involved the following steps: a solution was created by dissolving 4 mL of plasma in an equal volume of deionized water and then adding 75 microns of the synthesized nanoparticles. The UV-VIS absorption spectra were captured using a Cary series UV-Vis-NIR spectrophotometer. Transmission Electron Microscopy (TEM) images were taken with a Talos F200i high-resolution microscope at 200 kV. X-ray diffraction (XRD) analysis was performed with a Philips PW1710 diffractometer using Cu Ka radiation (λ = 1.54186 Å). The diffraction patterns were recorded from 20° to 70° 2θ, with a step size of 0.020° 2θ and a 10-second collection time per step. Fourier-transform infrared (FT-IR) spectroscopy was conducted using a Nicolet 6700 spectrophotometer to identify the functional groups on the nanoparticle surface. Lastly, charge density measurements were made using a Malvern Panalytical Zetasizer Nano ZS.
Experimental animals
This research utilized forty-two adult male BALB/c mice (Mus musculus) from the National Cancer Institute at Cairo University, Egypt. These mice, aged approximately 2–3 months and weighing between 24 and 25 g, had unrestricted access to food and water. They were acclimatized to standard laboratory conditions, including a 12-hour light-dark cycle, for 28 days in a room maintained at 23 ± 0.5 ºC [39]. The study adhered to the ethical guidelines with approval number CU/I/F/42/21 from the Cairo University Institutional Animal Care and Use Ethics Committee (CU-AICUC). For the induction of diabetes, the mice received an intraperitoneal injection of 150 mg/kg alloxan monohydrate after fasting for 16 h [40]. Hyperglycemia was confirmed five days later, with diabetic mice identified by blood glucose levels exceeding 200 mg/dl. The mice were divided into seven groups (n = 7) (Table 1). Group 1 represents untreated mice that received only food and water for 28 days. The other six groups (2–7) represent diabetic mice.
Biochemical analyses
Blood sugar and body weight determination
After sanitizing the tail, a minor cut was made at the end to collect blood from each mouse. The blood glucose levels were measured weekly from the start of the study to week four, adhering to the glucose-oxidase method. The body weight of the mice was recorded before the study started and regularly during the study using an electronic scale [41].
Oxidative stress tests (liver and kidney)
Superoxide dismutase (SOD) and catalase (CAT) activities
The liver and kidney tissues were processed separately by homogenizing them in a cold phosphate buffer solution (0.1 M, pH 7.4) with 1.17% potassium chloride (KCl), using a Polytron homogenizer. This mixture was then centrifuged at 10,500 × g for 15 min at a temperature of 4 °C. The resulting supernatant was utilized for enzyme activity assays. The activity of Superoxide Dismutase (SOD) was determined using a specific Activity Assay Kit (Catalog #: CB-P052-K). Enzyme activity is quantified in units per milligram of protein, where one unit of enzyme activity is the amount required to inhibit 50% of nitrite formation. Catalase (CAT) activity was measured following the method established by Johansson and Borg [42].
The assay mixture, with a total volume of 3 mL, was composed of 1.95 mL of phosphate buffer (0.1 M, pH 7.0), 1.0 mL of 0.019 M hydrogen peroxide (H2O2), and 0.05 mL of the tissue supernatant. The absorbance shifts were monitored at a wavelength of 240 nm, and the results were expressed as micromoles of H2O2 consumed per minute per milligram of protein in the solution.
Malondialdehyde (MDA) and glutathione (GSH) activities
Following the centrifugation of the tissue homogenate (10% w/v) at 10,500 × g for 15 min, a 1 mL sample of the supernatant was collected. To this, 0.5 mL of 30% trichloroacetic acid (TCA) and 0.5 mL of 0.8% thiobarbituric acid (TBA) were added. The mixture was then heated to 70 °C for 30 min in a thermostatic shaking water bath. Subsequently, the samples were cooled in water for 10 min and centrifuged again for 10 min. The absorbance of the samples was measured at 540 nm. The concentration of malondialdehyde (MDA) was determined using a calibration curve created with tetraethoxypropane, and lipid peroxidation levels were quantified as micromoles of MDA per milligram of protein. Additionally, a Glutathione Assay kit (CS0260-1KT) was employed to measure GSH levels in pancreatic tissue, which were reported as nanomoles of GSH per milligram of protein.
Histopathology tests
Hematoxylin and eosin staining
Using conventional protocols, a histological examination of the lung, heart, brain, spleen, liver, pancreas, and kidney was carried out. After being put into cassettes, autopsied organs were immersed in 10% neutral buffered formalin. Formalin-fixed tissues are processed for paraffin (wax) embedding. Sections of 5-µm-thick paraffin-embedded sections were taken and underwent hematoxylin and eosin (H&E) staining, then examined under light microscopy for pathology. A comparison of the obtained tissues was made between different treated groups [43].
Aldehyde fuchsin staining
Pancreatic tissue samples were initially rinsed with ice-cold saline. They were then preserved in a 10% neutral formalin solution for 24 h, embedded in paraffin wax, and cut into Sect. 5 micrometers thick. These sections were stained using Gormori’s aldehyde fuchsin staining solution, which consists of 0.5 g of pararosaniline, 100 mL of 70% ethanol, 1 mL of paraldehyde, and 1 mL of hydrochloric acid. The sections were then cleared of wax and rehydrated. Subsequently, they were oxidized with Lugol’s iodine solution and decolorized with sodium thiosulfate. The final step involved staining the sections with aldehyde fuchsin to highlight specific tissue features [43].
Statistical analysis
Statistical analysis was performed using Graphpad prism version 9, one-way ANOVA with Tukey’s posttest. For quantitative variables of triplicate determinations, data were presented as Mean and standard deviation (SD) [6].
Data availability
The dataset supporting the conclusions of this article is available in the [https://www.sciencedirect.com/science/article/abs/pii/S0946672X2400049X] repository.
References
Pillai SS, Sugathan JK, Indira M (2012) Selenium downregulates RAGE and NFκB expression in diabetic rats. Biol Trace Elem Res 149(1):71–77
Hwang D, Seo S, Kim Y, Kim C, Shim S, Jee S, Lee S, Jang M, Kim M, Yim S, Lee SK, Kang B, Jang I, Cho J (2007) Selenium acts as an insulin-like molecule for the down-regulation of diabetic symptoms via endoplasmic reticulum stress and insulin signalling proteins in diabetes-induced non-obese diabetic mice. J Biosci 32(4):723–735
Deng W, Wang H, Wu B, Zhang X (2019) Selenium-layered nanoparticles serving for oral delivery of phytomedicines with hypoglycemic activity to synergistically potentiate the antidiabetic effect. Acta Pharm Sin B 9(1):74–86
AlBasher G, Alfarraj S, Alarifi S, Alkhtani S, Almeer R, Alsultan N, Alharthi M, Alotibi N, Al-Dbass A, Abdel Moneim AE (2020) Nephroprotective Role of Selenium Nanoparticles against Glycerol-Induced Acute Kidney Injury in rats. Biol Trace Elem Res 194(2):444–454
Li S, Dong X, Xu L, Wu Z (2023) Nephroprotective effects of Selenium nanoparticles against Sodium Arsenite-Induced damages. Int J Nanomed 18:3157–3176
Karas R, Alexeree S, ElSayed H, Attia Y (2024) Assessment of Wound Healing Activity in Diabetic mice treated with a Novel Therapeutic combination of selenium nanoparticles and platelets Rich plasma. Sci Rep 14:5346
Khurana A, Tekula S, Saifi MA, Venkatesh P, Godugu C (2019) Therapeutic applications of selenium nanoparticles. Biomed Pharmacother Biomedecine Pharmacother 111:802–812
Wienaldi, Lister NE (2022) Antidiabetic effects of the platelet Rich plasma (PRP): a review. Int J Res Pharm Sci 13(3):Art. 3.
Barman A, Mukherjee S, Sinha MK, Sahoo J, Viswanath A (2021) The benefit of platelet-rich plasma injection over institution-based physical therapy program in adhesive capsulitis patients with diabetes mellitus: prospective observational cohort study. Clin Shoulder Elb 24(4):215–223
Okere B, Lucaccioni L, Dominici M, Iughetti L (2016) Cell therapies for pancreatic beta-cell replenishment. Ital J Pediatr 42:62
Pagliuca FW, Melton DA (2013) How to make a functional β-cell. Dev Camb Engl 140(12):2472–2483
Raja S, Byakod G, Pudakalkatti P (2009) Growth factors in periodontal regeneration. Int J Dent Hyg 7(2):82–89
Zhang M, Lin Q, Qi T, Wang T, Chen CC, Riggs AD, Zeng D (2016) Growth factors and medium hyperglycemia induce Sox9 + ductal cell differentiation into β cells in mice with reversal of diabetes. Proc Natl Acad Sci USA 113(3):650–655
Sonker A, Dubey A, Bhatnagar A, Chaudhary R (2015) Platelet growth factors from allogeneic platelet-rich plasma for clinical improvement in split-thickness skin graft. Asian J Transfus Sci 9(2):155–158
Cavallo C, Roffi A, Grigolo B, Mariani E, Pratelli L, Merli G, Kon E, Marcacci M, Filardo G (2016) Platelet-Rich Plasma: The Choice of Activation Method Affects the Release of Bioactive Molecules. Biomed Res Int 2016:6591717
Knezevic NN, Candido KD, Desai R, Kaye AD (2016) Is platelet-rich plasma a future therapy in Pain Management? Med Clin North Am 100(1):199–217
Pavlovic V, Ciric M, Jovanovic V, Stojanovic P (2016) Platelet Rich plasma: a short overview of certain bioactive components. Open Med Wars Pol 11(1):242–247
Martín-Solé O, Rodó J, García-Aparicio L, Blanch J, Cusí V, Albert A (2016) Effects of platelet-rich plasma (PRP) on a model of renal ischemia-reperfusion in rats. PLoS ONE 11(8):e0160703
Salem N, Helmi N, Assaf N (2018) Renoprotective Effect of Platelet-Rich Plasma on Cisplatin-Induced Nephrotoxicity in Rats. Oxid Med Cell Longev 2018:e9658230
El-Tahawy NF, Rifaai RA, Saber EA, Saied SR, Ibrahim RA (2017) Effect of platelet Rich plasma (PRP) injection on the endocrine pancreas of the Experimentally Induced Diabetes in male albino rats: a histological and immunohistochemical study. J Diabetes Metab 08:3
Dhurat R, Sukesh M (2014) Principles and methods of Preparation of platelet-rich plasma: a review and author’s perspective. J Cutan Aesthetic Surg 7(4):189–197
Laclaustra M, Navas-Acien A, Stranges S, Ordovas JM, Guallar E (2009) Serum selenium concentrations and hypertension in the US Population. Circ Cardiovasc Qual Outcomes 2(4):369–376
Hassan RM, Elsayed M, Kholief TE, Hassanen NHM, Gafer JA, Attia YA (2021) Mitigating effect of single or combined administration of nanoparticles of zinc oxide, chromium oxide, and selenium on genotoxicity and metabolic insult in fructose/streptozotocin diabetic rat model. Environ Sci Pollut Res 28(35):48517–48534
Jablonska E, Reszka E, Gromadzinska J, Wieczorek E, Krol MB, Raimondi S, Socha K, Borawska MH, Wasowicz W (2016) The Effect of Selenium supplementation on glucose homeostasis and the expression of genes related to glucose metabolism. Nutrients 8(12):772
Tarmizi AAA, Adam SH, Ramli NNN, Abd Hadi NA, Maisarah AM, Gee, Tang SH, Mokhtar MH (2023) The ameliorative effects of selenium nanoparticles (SeNPs) on diabetic rat model: a narrative review. Sains Malays 52(7):2037–2053
Ojeda ML, Nogales F, Carrasco López JA, Gallego-López MC, Carreras O, Alcudia A, Pajuelo E (2023) Microbiota-liver-bile salts Axis, a novel mechanism involved in the Contrasting effects of Sodium Selenite and Selenium-Nanoparticle supplementation on adipose tissue development in adolescent rats. Antioxidants 12:1123
Di Naso FC, Simões Dias A, Porawski M, Marroni NAP (2011) Exogenous Superoxide dismutase: action on liver oxidative stress in animals with Streptozotocin-Induced diabetes. Exp Diabetes Res 2011:754132
Djeffal A, Messarah M, Boumendjel A, Kadeche L, Feki AE (2015) Protective effects of vitamin C and selenium supplementation on methomyl-induced tissue oxidative stress in adult rats. Toxicol Ind Health 31(1):31–43
Al-Quraishy S, Dkhil MA, Abdel Moneim AE (2015) Anti-hyperglycemic activity of selenium nanoparticles in streptozotocin-induced diabetic rats. Int J Nanomed 10:6741–6756
Alexeree SMI, Abdel-Harith M (2023) Monitoring the cytotoxic effect of novel nanoconjugates during and after in-vivo photodynamic therapy. AIP Conf Proc 2620(1):060001
Cruz D, Lichten M, Berg K, George P (2022) Developmental trauma: conceptual framework, associated risks and comorbidities, and evaluation and treatment. Front Psychiatry 13:800687
Rivai H, Bakhtra D, Purba T (2018) Development and Validation of Analysis Methods of Captopril in tablets with methods of Area under curves and Absorbance by Ultraviolet-Visible Spectrophotometry. Int J Pharm Sci Med 3(4):1–10
Qazi A, Simsekler MCE, Al-Mhdawi MKS (2023) Exploring network-based dependencies between country-level sustainability and business risks. J Clean Prod 418:138161
Safitri A, Tirto Sari DR, Refsilangi B, Roosdiana A, Fatchiyah F (2021) Histopathological Profiles of Rats (Rattus norvegicus) Induced with Streptozotocin and Treated with Aqueous Root Extracts of Ruellia tuberosa L. Vet Med Int 2021:e6938433
Yaman T, Uyar A, Çelik İ, Alkan E, Keleş Ö, Yener Z (2017) Histopathological and Immunohistochemical Study of Antidiabetic Effects of Heracleum Persicum Extract in experimentally Diabetic rats. Indian J Pharm Educ Res 51(3):2017
Nabi SA, Kasetti RB, Sirasanagandla S, Tilak TK, Kumar MVJ, Rao CA (2013) Antidiabetic and antihyperlipidemic activity of Piper longum root aqueous extract in STZ induced diabetic rats. BMC Complement Altern Med 13:37
Monday OM, Uzoma AI (2013) Histological changes and antidiabetic activities of Icacina Trichantha tuber extract in beta–cells of alloxan induced diabetic rats. Asian Pac J Trop Biomed 3(8):628–633
Keshta AT, Fathallah AM, Attia YA, Salem EA, Watad SH (2023) Ameliorative effect of selenium nanoparticles on testicular toxicity induced by cisplatin in adult male rats. Food Chem Toxicol 179(4):113979
Alexeree SMI, Youssef D, Abdel-Harith M (2023) Using biospeckle and LIBS techniques with artificial intelligence to monitor phthalocyanine-gold nanoconjugates as a new drug delivery mediator for in vivo PDT. J Photochem Photobiol Chem 440:114687
Katsumata K, Katsumata K, Katsumata Y, Ozawa T (1994) Acute and chronic effect of ethanol on the occurrence of alloxan diabetes in rats. Horm Metab Res 26(4):166–168
Beach EF, Turner JJ (1958) An enzymatic method for glucose determination in body fluids. Clin Chem 4(6):462–475
Johansson LH, Borg LA (1988) A spectrophotometric method for determination of catalase activity in small tissue samples. Anal Biochem 174(1):331–336
Suvarna SK, Layton C, Bancroft JD (2019) Bancroft’s theory and practice of histological techniques. Elsevier doi. https://doi.org/10.1016/C2015-0-00143-5
Acknowledgements
The authors extend their appreciation to Taif University, Saudi Arabia, for supporting this work through project number (TU-DSPP-2024-150).
Funding
This research was funded by Taif University, Saudi Arabia, Project No. (TU-DSPP-2024-150)
Author information
Authors and Affiliations
Contributions
The hypothesis, as well as the conception and design of the experiments, were created by YAA, SA, SHA, and RK. Experiments were carried out by RK, SA, NE, and YAA. The manuscript was written, reviewed, revised, and edited by NE, RK, SHA, and YAA. The final manuscript was read and approved by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karas, R.A., Alexeree, S., Elzohery, N. et al. Antidiabetic potential of Selenium nanoparticles and plasma-rich platelets in diabetic mice. Appl Biol Chem 67, 62 (2024). https://doi.org/10.1186/s13765-024-00907-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13765-024-00907-5