Abstract
Background
Pseudomonas infections are among the most common infections encountered in hospitalized patients, especially those with chronic illnesses or an immunocompromised state. Management of these infections has become challenging due to increased antibiotic resistance. Therefore, this study examines the antibiotic resistance profiles of Pseudomonas spp. and the associated factors among patients admitted to a large tertiary hospital in a developing country.
Methods
This retrospective observational chart review study assessed patients admitted to a large tertiary hospital in a developing country with a positive culture growth of Pseudomonas from anybody site. Antibiotic susceptibility of the isolated Pseudomonas and patient characteristics were studied from the start of 2021 to the end of 2022. The study ground consisted of 185 patients.
Results
The study included 185 patients with positive Pseudomonas isolates. Males constituted 54.6% of the sample, while 45.4% were females. The median age of the patients was 53 years. Patient comorbidities and risk factors for Pseudomonas infection and multidrug resistance were assessed. Antibiotic resistance to the Pseudomonas regimens showed the highest resistance to meropenem and ciprofloxacin (23.4%, similarly) among isolates of Pseudomonas aeruginosa. Multidrug resistance (MDR) was found in 108 (58.4%) isolates. The most commonly used antibiotic for treatment was piperacillin-tazobactam, accounting for 33.3% of cases, followed by aminoglycosides at 26.6%.
Conclusions
Pseudomonas aeruginosa isolates were resistant to meropenem and ciprofloxacin. Over half of the isolates were multidrug-resistant, which was worrying. Piperacillin-tazobactam and aminoglycosides were the most often utilized antibiotics, highlighting the significance of susceptibility testing. Implementing antimicrobial stewardship programs and infection control measures can help reduce drug resistance and improve outcomes in Pseudomonas infections.
Similar content being viewed by others
Introduction
Pseudomonas aeruginosa is an opportunistic Gram-negative pathogen that can live in various hosts, such as plants, animals, and people [1]. Even in environments with inadequate nutrient levels, it can persist in both community and hospital settings [2, 3]. The prevalence of hospital-acquired infections (HAI) exceeds that of community-acquired infections (CAI) [4, 5]. Patients with community-acquired pneumonia (CAP) in Africa (5.5%), Asia (5.2%), South America (4.9%), North America (4.3%), and Europe (3.8%) are more likely to have P. aeruginosa isolates [6]. Numerous nosocomial infections, including bacteremia, urinary tract infections (UTIs), wound infections, and ventilator-associated pneumonia (VAP), are linked to P. aeruginosa [7]. It is the fourth most prevalent nosocomial pathogen, with mortality rates among critically ill patients ranging from 27 to 48% [8, 9].
According to the INFORM database, the rates of multidrug-resistant (MDR) P. aeruginosa infections in healthcare settings consistently range from 11.5 to 24.7% [10]. The World Health Organization (WHO) has classified carbapenem-resistant P. aeruginosa as a priority 1 or “critical” pathogen that requires urgent development of new therapies to address the emerging public health crisis of drug resistance [11]. The Center for Disease Control and Prevention (CDC) has also recognized MDR-P. aeruginosa as a significant threat for the past decade, with an estimated 32,600 cases, 2,700 deaths, and healthcare costs amounting to US $767 million annually [12]. A national study in the United States found that patients with MDR-P. aeruginosa respiratory infections had higher mortality rates, approximately seven days longer hospital stays, increased readmission rates, and an additional cost of US $20,000 per infection compared to those with non-MDR-P. aeruginosa infections [12].
A history of chronic obstructive pulmonary disease (COPD), prolonged hospitalization or intensive care unit (ICU) admission, prior P. aeruginosa infection, use of invasive medical devices (such as tracheostomy tubes, urethral catheters), or prior surgery are risk factors for multidrug-resistant P. aeruginosa infection [13, 14]. Other common hospital-acquired infections caused by Pseudomonas include pneumonia by a ventilator and urinary tract infections by catheters [15]. Individuals with invasive medical devices, such as catheters or endotracheal tubes, are at an increased risk because it can form difficult-to-treat biofilms [16]. There is a 23% [17] chance that patients who contract infections in the ICU will have P. aeruginosa, and a 48.7% [18] chance that they will have multidrug-resistant P. aeruginosa.
Hospitalized patients who are chronically ill or immunocompromised are at significant risk for Pseudomonas infections, especially if they are brought on by strains resistant to antibiotics. The development of Pseudomonas strains resistant to antibiotics has made treating these infections even more challenging. In addition to examining the patterns of antibiotic resistance of Pseudomonas in patients admitted to a significant tertiary hospital in a developing country, this study will also examine the contributing factors to these patterns. By providing antibiotic resistance profiles, this study will aid clinicians in selecting the most effective antibiotics for Pseudomonas infections. This information will improve patient outcomes and reduce Pseudomonas-associated mortality rates. Understanding the factors that contribute to the antibiotic resistance of Pseudomonas can aid healthcare facilities in implementing targeted infection control measures to prevent the spread of resistant strains and reduce healthcare-associated infections. This study examines Pseudomonas infections in a developing country in order to increase our knowledge of antimicrobial resistance and its effect on global healthcare systems. The findings will guide local, national, and international efforts to combat antibiotic resistance and promote prudent antibiotic use. In addition, this study contributes to the epidemiology and management of Pseudomonas infections by shedding light on antibiotic resistance in Pseudomonas infections in developing countries, thereby filling a research gap and advancing the study of Pseudomonas infections. Its findings will inform future research and clinical practices based on evidence.
Methods
Study design and setting
The research was a retrospective observational analysis of An-Najah National University Hospital (NNUH) patient charts. The study focused on patients admitted to NNUH who had positive culture growth of Pseudomonas spp. from any part of their body. NNUH is a tertiary teaching hospital in Palestine that handles complex cases, surgeries, and procedures from various locations, and it has a total of 127 beds. We studied the epidemiology of Pseudomonas pathogens among admitted patients, patients’ clinical characteristics and antibiotic susceptibility of the isolated Pseudomonas from the start of January 2021 to December 2022.
Study population and sample size
The study included all patients who had Pseudomonas growth in the inpatient setting from all ages in all hospital departments (surgical, medical, pediatrics, cardiac departments, intensive care units, bone marrow transplant, vascular surgery and emergency department). Both Pseudomonas from active surveillance testing and clinical samples were studied. Outpatient samples, including hemodialysis center patients, were excluded because the data were incomplete. Regarding patients with multiple samples, we studied the first nonduplicate from each site and remarked on all sites from where it was isolated and then concluded that the patient had Pseudomonas growth from multiple sites as a variable. After excluding 13 patients, data were collected, studied, and analysed for 185 patients during the study period.
Lab methods
The microbiology lab uses the VITEK® 2 Compact (bioMérieux. Marcy l’Etoile, France) for bacterial identification and antibiotic susceptibility. The VITEK® 2 GN cards were used for identification and VITEK® 2 AST – N222 were used for antibiotic susceptibility. The AST-N222 contains the following antibiotics: amikacin, aztreonam, cefipem, ceftazidime, ciprofloxacin, gentamicin, imipenem, meropenem, minocycline, pefloxacin, piperacillin, piperacillin/tazobactam, rifampicin, ticarcillin, ticarcillin/clavulanic acid, and tobramycin.
Data collection
Patient data, including demographic and clinical information, were collected from electronic medical records and the hospital’s microbiology system. A standardized data collection sheet was used to record details such as age, sex, comorbidities, history of previous admissions and history of antibiotic use. The sheet also captured information on the department where the culture was obtained, any invasive devices inserted, the timing of bacterial growth onset, and the specific site from which Pseudomonas was isolated. Additionally, the study examined the Pseudomonas species, the antibiotics used for infection treatment, and the antibiotic sensitivity of the pathogen.
Ethical considerations
The study protocol, which involved accessing and utilizing patient clinical information, received approval from the Institutional Review Boards (IRBs) of An-Najah National University. The data and information were treated as confidential and solely used for clinical research objectives. Patient-specific identifiable information was not disclosed, and numerical codes were used instead of names to ensure privacy.
Statistical analysis
Data were coded, categorized, and entered into the Social Science Statistical Package (IBM-SPSS), version 21.0. Descriptive statistics were conducted with frequencies and percentages for categorical variables and medians and interquartile ranges (IQRs) for continuous variables. The Pearson test was used to assess the correlations. Either the chi-square or Fisher’s exact test, as appropriate, was used to test the significance between categorical variables. The Mann‒Whitney test was used for differences in the means between categories. The significance level was established at a p-value < 0.05.
Results
Demographics and clinical profile of the study population
A total of 185 patients met the inclusion criteria for our study. 101 (54.6%) were males, while 84 (45.4%) were females. The median age of the patients was 53 years, with an interquartile range (IQR) of 30 to 66. Regarding comorbidities, 58 (31.4%) patients had solid malignancies, and 34 (18.4%) had hematological malignancies. Additionally, 70 (37.8%) patients had cardiovascular disease, 55 (29.7%) had diabetes mellitus, and 28 (15.1%) had renal abnormalities. Among the population, 13 (7.0%) patients were undergoing dialysis, as shown in Table 1. Approximately 36.2% of the patients were admitted to our hospital due to various infectious causes, while 14.1% were found to be neutropenic at the time of admission. Additionally, 3.2% of the patients were primarily admitted due to COVID-19 infections. In terms of inserted devices, 59 (31.9%) patients had a Foley catheter inserted prior to the isolation of Pseudomonas, 49 (26.5%) had a central line, and 36 (19.5%) were intubated for more than 48 h before Pseudomonas growth on culture. Among the patients, 41.1% had a previous hospitalization within the last three months, and 29.2% had a history of prior antibiotic use. For further details, please refer to Table 1.
Bacterial isolates
Table 2 displays the distribution of the 185 patients who exhibited Pseudomonas growth among different hospital wards. The highest proportion was observed in the internal medicine department, with 39 patients (21.1%), followed by the surgery department, with 37 patients (20.0%), and the surgical intensive care unit, with 22 patients (11.9%). Regarding the onset of Pseudomonas acquisitions, most isolates (63.8%) were present on admission, defined as a positive culture obtained within the first three calendar days of admission. Additionally, 29.7% of the patients had the pathogen isolated from multiple body sites. P. aeruginosa accounted for 97.8% of the reported Pseudomonas species in our patient population, as shown in Table 3. Among the clinical samples (a total of 111 nonduplicate samples) that exhibited Pseudomonas growth, urine cultures were the most frequently reported site (36.9%). Regarding active surveillance testing, rectal swabs predominated in detecting Pseudomonas growth, accounting for 87.9% of the samples. For more specific information, please refer to Table 4.
Antibiotic utilization and resistance pattern
Piperacillin-tazobactam was the most commonly prescribed antipseudomonal agent for the treatment of Pseudomonas infections, accounting for 33.3% of cases, followed by aminoglycosides at 26.6%. Table 5 provides further details on the utilization of antipseudomonal regimens, with approximately 23.3% of patients receiving combination therapy for the management of Pseudomonas infection. Please refer to Table 5 for more comprehensive information on the treatment regimens.
Regarding the susceptibility of P. aeruginosa, the study found resistance rates of 23.4% for meropenem and 22.4% for imipenem. Among the tested agents, P. aeruginosa exhibited the highest sensitivity to amikacin. Notably, no cases of resistance to either carbapenem were observed in P. putida.
The resistance rates of P. aeruginosa isolates to piperacillin-tazobactam and ceftazidime were found to be 20.6% and 18.7%, respectively. Additionally, the resistance rate to cefepime in P. aeruginosa was 19.6%. In contrast, P. putida exhibited complete resistance to cefepime, ceftazidime, gentamicin, and amikacin. Among the cases of P. stutzeri, 33.3% showed resistance to each of these agents. Please refer to Table 6 for a comprehensive overview of the resistance rates of Pseudomonas species to different antimicrobial agents.
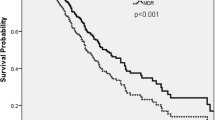
MDR isolates and their correlations with risk factors
Of the 185 patients included in the study, 108 (58.4%) were found to have a multidrug-resistant (MDR) isolate. The presence of MDR showed no statistically significant association with sex, age, or the presence of various comorbidities but was significantly correlated with intubation or ventilation history at the current admission and before obtaining the culture, in which 28 (25.9%) MDR patients were intubated, while among non-MDR patients, only 8 (10.4%) were intubated (p = 0.009). Furthermore, neutropenia on admission was significantly associated with MDR isolates as well (p = 0.008). For further details, please refer to Table 7. In terms of risk factors for Pseudomonas acquisition onset, either as present on admission or hospital-onset, age was of statistical significant difference (p = 0.035) between the two groups along with invasive devices inserted; which were all related to hospital onset Pseudomonas (p < 0.001) as shown in Table 8.
Relations between risk factors and being infected or colonised with Pseudomonas were also studied as illustrated in Table 9. The only statistically significant difference was noted with gender; in which females were more prone to colonisation than males (p = 0.005).
Discussion
Given that 97.8% of the isolates in the study were identified as P. aeruginosa, this discussion will primarily focus on this specific subtype. P. aeruginosa can potentially cause severe and life-threatening infections in patients, particularly due to the global rise in antimicrobial resistance. The increasing resistance of P. aeruginosa poses a significant public health threat that requires effective management strategies [19, 20].
The study encompassed a cohort of 185 patients with Pseudomonas isolates comprising 101 (54.6%) males and 84 (45.4%) females. The median age of the patients was 53 years, suggesting a higher susceptibility to Pseudomonas infections among older adults. Interestingly, our findings align with a previous study conducted in 2022 at a tertiary care center, which also reported a higher proportion of males (51.5%) but with a lower mean age of 37 years among patients with Pseudomonas infections [21]. Additionally, a 2019 Zhejiang University survey revealed that men made up 66.2% of the population and that the average age was 58 years [22].
Notably, in 29.7% of the clinical samples, Pseudomonas was isolated from multiple sites within the same patient. Among our study participants, most Pseudomonas isolates were obtained from urine samples (36.9%), followed by wound cultures (28.8%). These results align with previous studies, where Pseudomonas was commonly found in urine samples, indicating a similar prevalence pattern across different research findings [21].
Comorbid illnesses could predispose patients to Pseudomonas acquisition. Our study revealed that diabetes mellitus was found in 29.7% of the patients with Pseudomonas isolates. However, cardiovascular and renal diseases were found in 37.8% and 15.1% of the population, respectively. Regarding malignancy, solid malignancies affected 31.4% of the patients, while 18.4% of them had hematological malignancies. In accordance with this, a study in Turkey showed that 32% of patients with positive Pseudomonas cultures had a chronic illness, and 20% had malignancy [23].
Secondary bacterial infections are a common outcome of viral respiratory tract infections, contributing significantly to increased illness and mortality [24]. Among patients with coronavirus disease 2019 (COVID-19), P. aeruginosa was identified as a bacterial respiratory pathogen in 8% of co-infections in the study conducted by Westblade et al. [25]. This finding aligns with the low prevalence of Pseudomonas reported in our study involving COVID-19 patients (3.2%). Consequently, these results support the recommendation that routine empirical treatment for P. aeruginosa is generally unnecessary unless the patient has a history of infection caused by this organism or suffers from a chronic lung condition associated with P. aeruginosa pneumonia, such as bronchiectasis [6].
P. aeruginosa, as an opportunistic pathogen, primarily causes infection in patients who have been hospitalized for an extended period of time and have undergone medical applications [23]. Approximately 41% of the patients included in our study had a history of multiple previous hospitalizations, indicating a potential risk factor for P. aeruginosa infection. Additionally, approximately 29% of the patients had been exposed to broad-spectrum antibiotics in the last 3 months, further increasing their susceptibility to P. aeruginosa infections. Moreover, various physical breaches in host defenses, such as surgical incisions, urinary and vascular catheter insertion, and endotracheal intubation, can compromise the body’s natural barriers and contribute to developing P. aeruginosa infections. These factors collectively enhance the likelihood of P. aeruginosa acquisition and infection [26]. Our study found that 19.5% of the patients had an endotracheal tube, 26.5% had a central venous catheter and 31.9% were urinary catheterized. In agreement with this, 71% of the patients had invasive intravascular or urinary catheters, and 40% had undergone previous surgery [23].
The location of patients during hospitalization played a crucial role in our study. We observed that Pseudomonas infections occurred in 35% of patients admitted to intensive care units (ICUs), including medical, surgical, cardiac, and pediatric units. ICUs are regarded as high-risk units where patients, mostly immunocompromised, will be provided with special interventions, care and monitoring in addition to the advent of invasive procedures and instrumentation. These multiple risk factors increase the likelihood of acquiring an opportunistic infection. This result was similar to a study which found that most of the isolated Pseudomonas were from the ICU [27], in addition to an Indian study that showed that the ICU department was the second highest department from which Pseudomonas was isolated [28]. P.aeruginosa had a prevalence of 14.5%, of which 48.7% were multidrug resistant [29].
Multiple studies investigated the resistance pattern in the matter of antibiotic resistance of Pseudomonas organisms. The first was a study in Poland that showed a resistance rate of 67.8% to imipenem, 42.6% to cefepime, and 39.6% to both piperacillin-tazobactam and ciprofloxacin, while an overall lower resistance rates to gentamicin, ceftazidime, amikacin, and meropenem were 37.6%, 33.2%, 30.2%, and 29.2%, respectively [30]. Another study that was carried out in Palestine in 2020 showed that the resistance rate to imipenem was 49%, meropenem 45.1%, ceftazidime 25.5%, and ciprofloxacin 21.6% [31]. Furthermore, a previous study conducted in the haematology department at the same hospital as our study showed 60% resistance to ciprofloxacin, which was the highest among the tested antimicrobial agents, followed by imipenem (59.3%), piperacillin (54.2%), meropenem (48%), and gentamicin (48%). On the other hand, resistance to cefepime and ceftazidime was the lowest (16% and 24%, respectively) [32]. In contrast, our findings in this study revealed the more susceptibility rates of Pseudomonas to the tested anti-pseudomonal agents (imipenem and ciprofloxacin 23.4% for each), meropenem (22.4%), gentamicin (21.5%), and piperacillin-tazobactam (20.6%). These results support the findings that the most commonly utilized antipseudomonal agent was piperacillin-tazobactam in 33.3% of the patients who needed treatment, followed by ceftazidime in 31.1%. It is worth mentioning that in our hospital, carbapenems are among the restricted antibiotics; for this, they are only prescribed as per infectious disease team consultation for critically ill patients when other agents cannot be prescribed for any reason, including resistance to those carbapenem-preserving agents.
P. aeruginosa is deemed to be multidrug resistant (MDR) if it exhibits resistance to at least one agent in three or more antipseudomonal classes (carbapenems, fluoroquinolones, penicillins, cephalosporins, and aminoglycosides) [33]. Approximately 108 (58.4%) of the Pseudomonas isolates in our study were multidrug-resistant (MDR), which is higher than previous national studies. Notably, a study conducted in the Middle East and North Africa region reported a prevalence of 47.6% for MDR P. aeruginosa, specifically in Palestine [34]. Worldwide data reported a prevalence of MDR Pseudomonas of 55% in Pakistan [35], 47.8% in 2017 in Africa, and 56% in Egypt [35]. The extensive literature review indicates that resistance to P. aeruginosa has progressively increased over time in all countries, including Palestine. This rise in resistance can be attributed, in part, to the distinctive characteristics of P. aeruginosa. Notably, this bacterium possesses a large genome consisting of 6.3 million base pairs, which is the largest among all known bacteria. [35].
Another possible interpretation for the higher prevalence of MDR Pseudomonas isolates in our set up might be due to the increased rate of active surveillance testing according to the in-house screening policy; nevertheless, this does not rule out that the organism has become aggressive due to the overuse of antibiotics, which promotes antibiotic resistance. However, in this study, 70.8% of the patients did not have any documented history of previous use of antibiotics within the last 3 months. In fact, this might be the result of the intensive awareness campaigns and the national action plan for antimicrobial resistance that developed for the years 2020–2024 [36] or the result of the limited access to data on previous admission or antibiotic exposure.
MDR risk factors have raised significant concerns and have been extensively studied. In Colombia, a study investigated suspected risk factors and compared them between susceptible Pseudomonas and multidrug-resistant Pseudomonas isolates (n = 40). Among these patients, 10% had diabetes mellitus, 11% had renal disease, and 8% had malignancies. The study also revealed that males were more commonly affected by MDR infections, accounting for 51.9% of the cases. These findings align with similar studies, such as research conducted in Brazil, which also reported a higher incidence of MDR infections among males (55.1%) [37].
In the previous three months of admission in a study, 41 patients had received antibiotics. During the same admission or within 48 h before admission, 22 patients had a central line, 26 had a urinary catheter, and 11 had mechanical ventilation [38]. Comparatively, our study found that among patients with MDR infections, 31.5% had diabetes mellitus, 15.7% had kidney diseases, 25.9% had solid malignancies, and 18.5% had hematological malignancies. Among the 108 patients with MDR infections, 42.6% had undergone surgery in the last three months, and 73.1% had used antibiotics in the same time frame. The prevalence of invasive procedures such as central line, urinary catheter, and mechanical ventilation was 29.6%, 37.0%, and 25.9%, respectively).
Strengths and limitations
This is one of the first studies conducted in Palestine to identify the antibiotic resistance patterns displayed by Pseudomonas isolates from patients in tertiary hospitals. In addition, the study aims to determine the prevalence of multidrug-resistant Pseudomonas infections in the study population and to examine the utilization of antibiotics for treating Pseudomonas infections in a hospital setting. Nevertheless, our study had some limitations. First, relying on retrospective data from medical records introduces the possibility of missing or insufficient data mainly in the aspect of sensitivity pattern of the colonization pathogens. Dependent on the medical records’ quality are the data’s accuracy and completeness. Second, the study was conducted at a single tertiary care hospital in Palestine, which may have limited the findings’ applicability to other settings or populations. In addition, the sample size of 185 patients was relatively small, which may have limited the statistical power required to detect certain associations or patterns. The trial period was limited to two years, with no long-term patient monitoring. As a result, the study lacked the ability to assess the outcomes and long-term consequences of Pseudomonas infections.
Conclusions
In conclusion, this retrospective observational study included patients admitted to a large tertiary hospital in developing countries to examine antibiotic resistance in Pseudomonas infections. Pseudomonas infections are difficult to treat due to antibiotic resistance, particularly in elderly or immunosuppressed hospitalized patients. The emergence of meropenem and ciprofloxacin resistance in some Pseudomonas aeruginosa isolates is particularly concerning. The isolates had a 58.4% prevalence of MDR, highlighting the significance of choosing the best course of action and antibiotics. The most frequently prescribed antipseudomonal medication was piperacillin-tazobactam, followed by aminoglycosides. Larger samples and multicenter studies need to be used to learn more about Pseudomonas infections in the developing world. Understanding the effects of multidrug resistance on patient outcomes, mortality rates, and healthcare costs requires longitudinal studies that follow patients over time. Implementing antimicrobial stewardship programs and infection control measures can help reduce drug resistance and improve outcomes in Pseudomonas infections.
Data Availability
Data and materials used in this work are available from the corresponding author upon request.
Abbreviations
- NNUH:
-
An-Najah National University Hospital
- P. aeruginosa :
-
Pseudomonas aeruginosa
- P. maltophilia :
-
Pseudomonas maltophilia
- P. putida :
-
Pseudomonas putida
- P. stutzeri :
-
Pseudomonas stutzeri
- P. putrefaciens :
-
Pseudomonas putrefaciens
- ICU:
-
Intensive care unit
- AIDS:
-
Acquired immunodeficiency syndrome
- MDR:
-
Multidrug-resistant
- IRBs:
-
Institutional Review Boards
- SPSS:
-
Statistical Package for The Social Sciences
- IQR:
-
Interquartile Range
- COVID-19:
-
Coronavirus Disease 2019
References
Diggle SP, Whiteley M. Microbe Profile: Pseudomonas aeruginosa: opportunistic pathogen and lab rat. Microbiol (Reading). 2020;166(1):30–3.
Moradali MF, Ghods S, Rehm BH. Pseudomonas aeruginosa Lifestyle: a paradigm for Adaptation, Survival, and persistence. Front Cell Infect Microbiol. 2017;7:39.
Qin S, Xiao W, Zhou C, Pu Q, Deng X, Lan L, Liang H, Song X, Wu M. Pseudomonas aeruginosa: pathogenesis, virulence factors, antibiotic resistance, interaction with host, technology advances and emerging therapeutics. Signal Transduct Target Ther. 2022;7(1):199.
Sando E, Suzuki M, Ishida M, Yaegashi M, Aoshima M, Ariyoshi K, Morimoto K. Definitive and indeterminate Pseudomonas aeruginosa Infection in adults with community-acquired Pneumonia: a prospective observational study. Ann Am Thorac Soc. 2021;18(9):1475–81.
Balkhy HH, Cunningham G, Chew FK, Francis C, Al Nakhli DJ, Almuneef MA, Memish ZA. Hospital- and community-acquired Infections: a point prevalence and risk factors survey in a tertiary care center in Saudi Arabia. Int J Infect Dis. 2006;10(4):326–33.
Restrepo MI, Babu BL, Reyes LF, Chalmers JD, Soni NJ, Sibila O, Faverio P, Cilloniz C, Rodriguez-Cintron W, Aliberti S. Burden and risk factors for Pseudomonas aeruginosa community-acquired Pneumonia: a multinational point prevalence study of hospitalised patients. Eur Respir J 2018, 52(2).
Reynolds D, Kollef M. The epidemiology and Pathogenesis and treatment of Pseudomonas aeruginosa Infections: an update. Drugs. 2021;81(18):2117–31.
Hafiz TA, Bin Essa EA, Alharbi SR, Alyami AS, Alkudmani ZS, Mubaraki MA, Alturki NA, Alotaibi F. Epidemiological, microbiological, and clinical characteristics of Multi-resistant Pseudomonas aeruginosa isolates in King Fahad Medical City, Riyadh, Saudi Arabia. Trop Med Infect Disease. 2023;8(4):205.
Pagani L, Afshari A, Harbarth S. Year in review 2010: critical care–Infection. Crit Care. 2011;15(6):238.
Sader HS, Castanheira M, Duncan LR, Flamm RK. Antimicrobial susceptibility of Enterobacteriaceae and Pseudomonas aeruginosa isolates from United States Medical centers stratified by Infection type: results from the International Network for Optimal Resistance Monitoring (INFORM) Surveillance Program, 2015–2016. Diagn Microbiol Infect Dis. 2018;92(1):69–74.
Tacconelli E, Carrara E, Savoldi A, Harbarth S, Mendelson M, Monnet DL, Pulcini C, Kahlmeter G, Kluytmans J, Carmeli Y, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and Tuberculosis. Lancet Infect Dis. 2018;18(3):318–27.
Tabak YP, Merchant S, Ye G, Vankeepuram L, Gupta V, Kurtz SG, Puzniak LA. Incremental clinical and economic burden of suspected Respiratory Infections due to multi-drug-resistant Pseudomonas aeruginosa in the United States. J Hosp Infect. 2019;103(2):134–41.
Hafiz TA, Bin Essa EA, Alharbi SR, Alyami AS, Alkudmani ZS, Mubaraki MA, Alturki NA, Alotaibi F. Epidemiological, microbiological, and clinical characteristics of Multi-resistant Pseudomonas aeruginosa isolates in King Fahad Medical City, Riyadh, Saudi Arabia. Trop Med Infect Dis 2023, 8(4).
Alhussain FA, Yenugadhati N, Al Eidan FA, Al Johani S, Badri M. Risk factors, antimicrobial susceptibility pattern and patient outcomes of Pseudomonas aeruginosa Infection: a matched case-control study. J Infect Public Health. 2021;14(1):152–7.
Cole SJ, Records AR, Orr MW, Linden SB, Lee VT. Catheter-associated urinary tract Infection by Pseudomonas aeruginosa is mediated by exopolysaccharide-independent biofilms. Infect Immun. 2014;82(5):2048–58.
Tuon FF, Dantas LR, Suss PH, Tasca Ribeiro VS. Pathogenesis of the Pseudomonas aeruginosa biofilm: a review. Pathogens. 2022;11(3):300.
Vincent JL, Sakr Y, Singer M, Martin-Loeches I, Machado FR, Marshall JC, Finfer S, Pelosi P, Brazzi L, Aditianingsih D, et al. Prevalence and outcomes of Infection among patients in Intensive Care Units in 2017. JAMA. 2020;323(15):1478–87.
Ribeiro ÁCdS, Crozatti MTL, Silva AAd, Macedo RS. Machado AMdO, Silva ATdA: Pseudomonas aeruginosa in the ICU: prevalence, resistance profile, and antimicrobial consumption. Rev Soc Bras Med Trop 2019, 53.
Chatzinikolaou I, Abi-Said D, Bodey GP, Rolston KV, Tarrand JJ, Samonis G. Recent experience with Pseudomonas aeruginosa bacteremia in patients with cancer: retrospective analysis of 245 episodes. Arch Intern Med. 2000;160(4):501–9.
Spagnolo AM, Sartini M, Cristina ML. Pseudomonas aeruginosa in the healthcare facility setting. Reviews and Research in Medical Microbiology. 2021;32(3):169–75.
Maharjan N. Pseudomonas aeruginosa isolates among clinical samples showing growth in a Tertiary Care Centre: a descriptive cross-sectional study. JNMA J Nepal Med Assoc. 2022;60(252):676–80.
Shi Q, Huang C, Xiao T, Wu Z, Xiao Y. A retrospective analysis of Pseudomonas aeruginosa bloodstream Infections: prevalence, risk factors, and outcome in carbapenem-susceptible and -non-susceptible Infections. Antimicrob Resist Infect Control. 2019;8(1):68.
Yetkin G, Otlu B, Cicek A, Kuzucu C, Durmaz R. Clinical, microbiologic, and epidemiologic characteristics of Pseudomonas aeruginosa Infections in a University Hospital, Malatya, Turkey. Am J Infect Control. 2006;34(4):188–92.
Gupta RK, George R, Nguyen-Van-Tam JS. Bacterial Pneumonia and pandemic Influenza planning. Emerg Infect Dis. 2008;14(8):1187.
Westblade LF, Simon MS, Satlin MJ. Bacterial coinfections in coronavirus Disease 2019. Trends Microbiol. 2021;29(10):930–41.
Kerr KG, Snelling AM. Pseudomonas aeruginosa: a formidable and ever-present adversary. J Hosp Infect. 2009;73(4):338–44.
Gupta RS, Shrestha N. Clinical significance and antibiogram of Pseudomonas aeruginosa isolated from tertiary care hospital of Birgunj, Nepal. Indian J Med Res Pharm Sci. 2019;6(8):7–10.
Varaiya A, Kulkarni N, Kulkarni M, Bhalekar P, Dogra J. Incidence of metallo beta lactamase producing Pseudomonas aeruginosa in ICU patients. Indian J Med Res. 2008;127(4):398–402.
Ribeiro ÁCDS, Crozatti MTL, Silva AAD, Macedo RS, Machado AMO, Silva ATA. Pseudomonas aeruginosa in the ICU: prevalence, resistance profile, and antimicrobial consumption. Rev Soc Bras Med Trop. 2019;53:e20180498.
Brzozowski M, Krukowska Ż, Galant K, Jursa-Kulesza J, Kosik-Bogacka D. Genotypic characterisation and antimicrobial resistance of Pseudomonas aeruginosa strains isolated from patients of different hospitals and medical centres in Poland. BMC Infect Dis. 2020;20(1):693.
Adwan G, Shtayah A, Adwan K, Al-Sheboul S, Othman S. Prevalence and molecular characterization of P. Aeruginosa isolates in the West Bank-Palestine for ESBLs, MBLs and integrons. J Appl Life Sci Int. 2016;8(2):1–11.
Arman G, Zeyad M, Qindah B, Abu Taha A, Amer R, Abutaha S, Koni AA, Zyoud SH. Frequency of microbial isolates and pattern of antimicrobial resistance in patients with hematological malignancies: a cross-sectional study from Palestine. BMC Infect Dis. 2022;22(1):146.
Saderi H, Owlia P. Detection of multidrug resistant (MDR) and extremely drug resistant (XDR) P. Aeruginosa isolated from patients in Tehran, Iran. Iran J Pathol. 2015;10(4):265.
Al-Orphaly M, Hadi HA, Eltayeb FK, Al-Hail H, Samuel BG, Sultan AA, Skariah S. Epidemiology of Multidrug-Resistant Pseudomonas aeruginosa in the Middle East and North Africa Region. mSphere 2021, 6(3).
Farooq L, Memon Z, Ismail MO, Sadiq S. Frequency and antibiogram of multi-drug resistant pseudomonas aeruginosa in a Tertiary Care Hospital of Pakistan. Pakistan J Med Sci. 2019;35(6):1622.
Esiovwa R, Connolly J, Hursthouse A, Mukherji S, Mukherji S, Parasnis A, Sachwani K, Henriquez F. Bridging the gaps in the global governance of antimicrobia l resistance: the UN sustainable development goals and globa l health security agenda [version 1; peer review: 1 approved]. 2022.
Multidrug-Resistant Hospital Bacteria. Epidemiological factors and susceptibility Profile. Microb Drug Resist. 2021;27(3):433–40.
Ossa-Giraldo AC, Echeverri-Toro LM, Santos ZM, García MG, Agudelo Y, Ramírez F, Ospina S. [Risk factors for multidrug-resistant Pseudomonas aeruginosa Infection, in a tertiary hospital in Colombia]. Rev Chil Infectol. 2014;31(4):393–9.
Acknowledgements
We thank An-Najah National University Hospital for helping us find patient data and review medical records.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
The first draft of the manuscript was written by S.S., S.A., and M.W.S., who also collected data and performed the analysis. A.S., H.T.S., and A.A. offered logistical support, designed the study, and assisted in producing the final version of the manuscript. Meanwhile, B.A. and S.H.Z. conceptualized and designed the study, analyzed and coordinated the data, organized and supervised the field study, critically reviewed the manuscript, interpreted the results, and contributed to writing the final version. Finally, all authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Boards (IRBs) of An-Najah National University approved the study protocol, and the collected data were only used for clinical research purposes. The information was kept confidential and was not used for any other purpose. Patient information was coded to protect their identities. Since retrospective data were used, the IRB of An-Najah National University waived the requirement for informed consent. The authors confirmed that all the methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shbaita, S., Abatli, S., Sweileh, M.W. et al. Antibiotic resistance profiles and associated factors of Pseudomonas Infections among patients admitted to large tertiary care hospital from a developing country. Antimicrob Resist Infect Control 12, 149 (2023). https://doi.org/10.1186/s13756-023-01355-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-023-01355-4