Abstract
Background
The approval of ethanol by the Biocidal Products Regulation has been under evaluation since 2007. This follows concern over alcohol uptake from ethanol-based hand rubs (EBHR). If ethanol is classified as carcinogenic, mutagenic, or reprotoxic by the European Chemicals Agency (ECHA), then this would affect infection prevention and control practices.
Aim
A review was performed to prove that ethanol is toxicological uncritical and indispensable for hand antisepsis because of its unique activity against non-enveloped viruses and thus the resulting lack of alternatives. Therefore, the following main points are analyzed: The effectiveness of ethanol in hand hygiene, the evidence of ethanol at blood/tissue levels through hand hygiene in healthcare, and the evidence of toxicity of different blood/tissue ethanol levels and the non-comparability with alcoholic consumption and industrial exposure.
Results
EBHR are essential for preventing infections caused by non-enveloped viruses, especially in healthcare, nursing homes, food industry and other areas. Propanols are effective against enveloped viruses as opposed to non-enveloped viruses but there are no other alternatives for virucidal hand antisepsis. Long-term ingestion of ethanol in the form of alcoholic beverages can cause tumours. However, lifetime exposure to ethanol from occupational exposure < 500 ppm does not significantly contribute to the cancer risk. Mutagenic effects were observed only at doses within the toxic range in animal studies. While reprotoxicity is linked with abuse of alcoholic beverages, there is no epidemiological evidence for this from EBHR use in healthcare facilities or from products containing ethanol in non-healthcare settings.
Conclusion
The body of evidence shows EBHRs have strong efficacy in killing non-enveloped viruses, whereas 1-propanol and 2-propanol do not kill non-enveloped viruses, that pose significant risk of infection. Ethanol absorbed through the skin during hand hygiene is similar to consumption of beverages with hidden ethanol content (< 0.5% v/v), such as apple juice or kefir. There is no risk of carcinogenicity, mutagenicity or reprotoxicity from repeated use of EBHR. Hence, the WHO Task Force strongly recommend retaining ethanol as an essential constituent in hand rubs for healthcare.
Similar content being viewed by others
Introduction
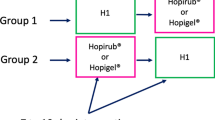
The Biocidal Products Regulation regulates the market entry and use of biocidal products. This consists of two stages: 1. approval of a biocidally active substance for certain types of products within the framework of a European procedure, and 2. authorization of a biocidal product at the national or EU level. According to the CLP Regulation (EU) No 1272/2008, biocidal active substances shall normally be subject to the provisions on harmonized classification and labelling [1]. Unless authorised in accordance with Regulation No 528/2012 [2], biocidal products should neither be made available on the market nor used. Approval of ethanol as an active substance has been under evaluation by the responsible Greece authority since 2007 (Table 1). The first decision on classification from the Board was the proposal that ethanol might be classified as ‘’CMR’’ (carcinogen; mutagen; and reprotoxic). In the “Registry of intention” on classification and labelling (CLH), the Greek authority updated a harmonized classification and labelling of ethanol on 27 July 2020 [3]. The current intention of extending harmonized classification provides, inter alia, a classification as reproductive toxicity category 2 (“suspected to have CMR potential for humans”) (Table 1). This is clearly a downgrade from the classification as carcinogenic category 1A and reproductive toxicity 1A (“known to have CMR potential for humans, based largely on human evidence”). However, it is important to note that the Risk Assessment Committee (RAC) of ECHA is not bound by the proposed classification, so that classifying ethanol as carcinogenic and/or reproductive toxicity category 1 by the ECHA still cannot be excluded. Category 1 classification means that ethanol would be marketable as a so-called substitution candidate for a maximum of 5 years. CMR substances of categories 1A and 1B may only be used or placed on the market after the corresponding transitional regulations (sunset date) have been approved by the European Commission according to specific use. Manufacturers, importers and downstream users must apply for these approvals exclusively from the ECHA. In addition, possible alternatives must be analyzed for technical and economic substitutability. The aim is to gradually replace “Substances of Very High Concern” with suitable alternatives.
The CLH dossier from 27 July 2020 should have been submitted to the European Chemicals Agency (ECHA) by 31 December 2020, but this has not yet happened. A final decision on classification from the Board is expected soon.
In October 2020, the German Association for Applied Hygiene published a comment supported by the Federal Association of Public Health Physicians, German Society of Hygiene & Microbiology, German Society for Hospital Hygiene, German Association for Control of Virus Diseases, German Veterinary Society, European Committee on Infection Control, German Virology Society, German Society for Hygiene, Environmental and Preventive Medicine, Austrian Society for Hygiene, Microbiology and Preventive Medicine and Robert Koch Institute, which culminated in the following conclusion:
Ethanol is indispensable as a biocidal product for hygienic hand antisepsis due to its efficacy against non-enveloped viruses, because no alternative exists [4].
The following memorandum of the alcohol-based hand rub (ABHR) Task Force, the WHO Collaborating Centre on Patient Safety and the Commission for Hospital Hygiene & Infection Prevention (KRINKO), supported by the Working Group of Hospital & Practice Hygiene and Working Group of (German) Scientific Medical Societies (AWMF), pursues 2 goals:
-
Development of a comprehensive risk–benefit assessment with refutation of classification of ethanol as reproductive toxicity category 2 and justification of the retention of ethanol for hand antisepsis due to the lack of alternatives for inactivation of non-enveloped viruses,
-
to draw attention to the possible consequences for infection prevention in healthcare settings if the currently proposed classification as “reproductive toxicity category 2” is chosen.
Health-related and economic consequences of the proposed classification of ethanol as reproductive toxicity category 2
This EU classification would lead to an international distortion of competition. Companies in non-EU Member countries would be able to produce, use and market EBHR without CMR classification and relevant restrictions. Such classification would also contradict the recital (4)5 of the CLP Regulation, which anticipates a benefit for companies from global harmonization of classification and labelling.
A simple, patent-free hand rub formulation with 80% (v/v) ethanol was recommended in 2009 by the WHO for low-income countries, since it is a less expensive alternative to commercially available preparations and can be produced locally [5]. Of course, WHO formulations could continue to be produced and used outside the EU. But if the marketability in the EU were no longer an option, it is implied that people living in countries outside the EU would be exposed to a risk which the EU excludes for its citizens. This is tantamount to discrimination.
Specific value of ethanol for virucidal hand antisepsis
Non-enveloped viruses have a significantly higher stability towards chemical agents than enveloped viruses. Of the three alcohols used in hand rub formulations (ethanol, 2-propanol and 1-propanol), only ethanol-based formulations proved to be effective within 30–60 s against non-enveloped viruses such as adeno-, polio-, human entero-, human papilloma-, polyoma-, echo- and coxsackie viruses in quantitative suspension assays [12,13,14,15,16]. Formulations containing 2-propanol and 1-propanol are not sufficiently active (Table 2). 1-propanol was not effective against coxsackie, poliovirus and human enterovirus 71 at a 90% concentration within 5 min [16]. Within 2 min, 80%, 90% and 97% 1-propanol and 2-propanol, and within 3 min, 70% and 90% 1-propanol and 2-propanol, were ineffective against poliovirus [personal communication, Schwebke I]. In contrast, ethanol was effective in concentrations of ≥ 70% in suspension and in vivo on hands [17]. One way to improve the activity of ethanol is to add acids, so that formulations based on 45%, 55%, 60%, 69.4% and 73.5% ethanol (w/w) achieve sufficient activity against poliovirus type 1 within 30 s or 1 min [18,19,20,21,22]. Ethanol activity against polyomavirus SV 40, as surrogate of papillomaviruses, can also be enhanced by adding acids [19, 22]. No comparable findings are available for 2-propanol or 1-propanol [23]. Since ethanol is more effective against non-enveloped viruses, it was chosen as the positive control for assessing the efficacy of hand rubs against viruses on artificially contaminated hands in prEN 17,430:2019 [24].
Virucidal hand antisepsis is necessary to interrupt cross-infection with non-enveloped hydrophilic viruses [41, 42] as well as inhibit fomite transmission, which occurs in both gastrointestinal and respiratory infections [43, 44]. This is also the case for norovirus outbreaks on cruise ships [45]. Nosocomial and foodborne outbreaks may be controlled by virucidal hand antisepsis in combination with virucidal surface disinfection (i.e. [46,47,48,49]).
While ABHR are standard hygiene procedures in healthcare, recommendations on hand hygiene for the food sector prioritize hand washing, since wet and/or soiled hands may reduce the efficacy of alcohol in inactivating pathogens. Since norovirus is responsible for most (58%) cases of foodborne illness of known etiology [50], causing 125 million (95% UI 70–251 million) cases globally [51], there have been studies to compare hand washing vs ABHR. There is clear evidence to support modifying the FDA Model Food Code to allow the use of EBHR as an alternative to hand washing when heavy soiling is absent [52]. Indeed, medical staff consider hand washing to be inadequate for hand hygiene, especially for bacterial pathogens. Organisms such as Escherichia coli, Pseudomonas aeruginosa and Staphylococcus aureus are only reduced by 2–2.5 log levels after washing with soap [8]. Only ABHR hand sanitizers are active against murine norovirus (MNV), both in vitro and in vivo [53]. Study antimicrobial soaps could not inactivate MNV [35]. Another in vivo hand-wash study with MNV, conducted according to EN 1499, found soap with CHG 4% to be less effective than handwashing with plain soap [54]. Comparable studies using feline calicivirus, a surrogate virus for human noroviruses, led to a reduction of 1.26 log using liquid soap [55]. Another study showed that EBHR containing 72.4% v/v ethanol was only effective against norovirus after 30 s at twice the volume (6 ml), while a high-ethanol content product (89.5% v/v) was effective after 15 s/3 ml [17]. Handwashing was better than EBHR in one study [56], but the effect was only mechanical. For viral inactivation, it is necessary to use virucides to interrupt further spread. When using virucidal hand rubs as no-rinse formulations, the virus is inactivated directly on hands and the risk of cross-infection is eliminated [53]. Therefore, indication-based use of EBHR is also considered necessary in the food service industry: "It should be possible to differentiate between times when a traditional full handwash (10–15-s scrub followed by rinsing under warm water and drying) must be performed, and when alternative methods, such as a brief hand rinse under warm water, use of a disposable alcohol-based hand wipe, or use of an ethanol-based hand rub, might suffice “ [57].
Considering the contact frequency of staff during patient care, even for isolated patients, and the need for hand antisepsis after each contact with the patients and their surroundings, repeated soap washing is associated with high risk for irritant dermatitis. Therefore, hand washing should be performed only when hands are visibly soiled or contaminated, especially with blood or other body fluids[7]. While dispensers for ABHR can be installed anywhere, access should be restricted in paediatric and psychiatric departments for obvious reasons.
Should a non-enveloped virus, instead of enveloped SARS-CoV-2, cause another pandemic, there would be no sufficiently effective ABHR to prevent transmission if EBHRs with activity against non-enveloped viruses are unavailable.
Table 3 lists examples of non-enveloped viruses that have been detected on hands and for which transmission via hands has led to nosocomial infections and outbreaks. If there is an infection due to one of these viruses, only hand antiseptics based on ethanol 95% or with reduced ethanol content and synergistic additives can be used to interrupt potential transmission.
Since non-enveloped viruses such as HAV and rotaviruses retain infectivity on the skin for up to 6 h [92], it is not surprising that spread has been confirmed experimentally (Table 4).
Toxicological evaluation of EBHR use
Evidence for a reprotoxic effect of ethanol originates from experiences with the consumption of alcoholic beverages by pregnant women [97]. There is no epidemiological foundation of toxicity for workers from handling ethanol-containing chemical products in industrial workplaces or from the use of EBHR in healthcare facilities or of ethanol-containing products in the non-healthcare setting. Neither is accidental oral ingestion of EBHR a hazard for healthcare workers.
For 1-propanol and 2-propanol in ABHR, unlike ethanol, there is no suspicion of toxicity from excessive consumption, including carcinogenesis, because neither of these agents are consumed as alcoholic beverages. Because of distinct differences between the three alcohols in terms of metabolically-mediated physiological blood levels, the increase of alcohol blood level above baseline after EBHR was about 157-fold, but after use of 1- and 2-popanol it increased > 1.800- and > 10.000-fold, respectively (Table 5). At the same, in volunteers before the use of ABHR 91 of 107 blood samples (85%) for propan-1-ol, 67 of 107 samples (62.6%) for propan-2-ol and 86 of 107 (80.4%) for ethanol were below the detection limit of 0.13 mg/L, 0.03 mg/L and 0.14 mg/L respectively [102]. The median maximum blood concentration of 11 mg/L after the simulated worst case by 10 surgical hand rubs within 80 min underlines the safety of using EBHR (Table 5).
Absorption after hand rub with ABHR
After excessive exposure (Table 6), only 0.5% to 2.3% of applied ethanol is absorbed, with the highest median blood levels identified between 6.9 and 30.1 mg/L [103]. These findings are in line with the results observed by Miller et al. [104], where five subjects repeatedly (50 times over 4 h) applied 5 mL of an EBHR (62% denatured ethyl alcohol) to both hands and rubbed until dry. The blood ethanol level was < 50 mg/L for all 5 study participants.
To clarify potential adverse effects on the pancreas after hand antisepsis by teaching nurses, the following scenario was considered: total rubbing of hands (3 mL of 70% EBHR) consisting of 30 persons 3 times/day in the same room (116 cm3) over a period of 48 h interrupted by one night (90 hand rubs/day in the room). Blood ethanol concentrations were predicted using a physiologically-based pharmacokinetic model, which allowed simulation of inhalation and dermal exposure. In the worst-case scenario, the simulation showed that the maximum blood ethanol concentration predicted-5.9 mg/L [104]-is of the same order of magnitude as endogenous ethanol concentration (mean = 1.1 mg/L; median = 0.4 mg/L; range = 0–35 mg/L) in humans without prior alcohol consumption [105].
In comparison, a glass of beer contains about 12 g of ethanol [106], which corresponds to a blood level of 150–250 mg/kg for a 70-kg adult, and produces a peak blood ethanol concentration of 250 mg/L. Fruit juices may contain up to 3 g ethanol per L, and apple juice contains 1 g ethanol per 500 mL [106]. Assuming an absorption rate of 90%, drinking 500 ml of apple juice will result in a blood alcohol concentration of about 85 mg/L ethanol in a 75-kg man or 125 mg/L ethanol in a 60-kg woman [103]. Non-alcoholic beer, flavored water, and orange juice result in blood ethanol levels similar to those seen after hand antisepsis, or even higher [106]. The concentration of ethanol naturally produced by intestinal bacteria is 1.1 mg/L [102, 107] so internal amounts of ethanol resulting from topical application of EBHR are in the range of those associated with consumption of non-alcoholic beverages, which are considered safe for consumers [108].
These results show that there is no significant risk of developmental or reprotoxicity from repeated occupational exposures and/or high frequency use of EBHR [108].
The use of EBHR induces measurable concentrations of ethanol and its metabolite ethyl glucuronide (EtG), a marker of ethanol consumption, in urine, but the measured concentrations are below any harmful or toxic levels [109]. The results demonstrate that dermal and inhaled ethanol absorption from the use of EBHR alone caused mean urinary ethanol concentrations that, on average, were over 60 times lower than those from permitted use of alcohol-containing drinks, food, or cosmetic products. In the United States, harmful intake of ethanol is defined as more than one alcoholic drink equivalent, defined as containing 14 g of pure alcohol (0.33 L of beer or 0.1 L of wine) for women and 18 g for men per day [110, 111]. Germany, Austria, and Switzerland regard the maximum harmless alcohol intake to be 10 g/day for healthy women and 20 g/day for healthy men [112]. Compared with consumption of alcoholic beverages or exposure to consumer products containing ethanol, the amount of ethanol absorption resulting from EBHR application is negligible. In practice, there is no evidence of any harmful effect from using EBHR as a clinical necessity. The following results were confirmed in a double-blind, randomized phase I experimental study: 20 ml of hand rub (74.1% ethanol content) were applied on a 200-cm2 gauze swab on skin areas; the gauze swab remained on the skin for 10 min (0.1 mL/cm2 treated skin area). Comparing ethanol concentrations at baseline, and after 15 and 60 min, no significant differences could be detected. The detection limit was defined as the ethanol concentration producing an area 3 × larger than the blank area under the curve (0.5 mg/L) [113].
Animal experiments
After oral administration in mice, there was no fetotoxic or teratogenic effect at 15,000 mg ethanol /kg. It takes 25,000 mg/kg to elicit a fetotoxic and teratogenic potential. The blood level reached 3840 mg/L [114]. This is about 100-fold higher than the blood alcohol level after excessive exposure to EBHR. In rabbits, no developmental toxicity could be detected up to the highest administered dose of 2370 mg/kg [115].
The risk of developmental effects from inhalation exposure during hand antisepsis is negligible, as indicated by experiments in rats [116]. No fertility or developmental effects were seen at inhalation exposures up to 16,000 ppm (30,400 mg/m3; [116,117,118]). The lowest reported No Observed Adverse Effect Level (NOAEL) for fertility by the oral route was 2000 mg/kg in rats, equivalent to a blood alcohol concentration of 1320 mg/L, although this was based on a significant increase in the number of small pups rather than a direct effect on fertility; such direct effects are not seen until much higher doses [119].
Summary of risk assessment in the literature
Irvine [120] characterizes the situation as follows: “A specific NOAEL for human developmental toxicity of ethanol is unlikely to be determined from existing epidemiological studies because the results of all such studies are influenced to some extent by confounding nutritional and environmental factors and from the inherent imprecision in the assessment of ethanol exposure that is based on self-reporting. Developmental toxicity may result from drinking alcoholic beverages. This is not, however, considered relevant to the low blood alcohol concentrations resulting from any conceivable inhalation or dermal exposure in the workplace or through the directed use of any consumer product containing ethanol.”
The dermal adsorption of ethanol after hand rub use is below any toxic risk and is also lower than intake from non-alcoholic beverages. Furthermore, ethanol does not accumulate in the body. Concerning repeated dose effects, the lowest reported NOAEL is approximately 2400 mg/kg /day from a dietary study on rats [121]. Since 1959 [122], EBHR have been used in Europe for hand antisepsis and surgical hand preparation without any indication of toxic or reproductive toxicity side effects. It can be concluded from ethanol absorption data after exposure to EBHR that there is no evidence whatsoever that would justify classifying ethanol as a developmental reproductive toxicity category 2 under the EU CLP regulation, if used as intended for hand antisepsis.
Occupational health assessment of ethanol
This may be divided into several categories as listed:
Maximum workplace concentration (MAK value)
380 mg/m3 [123]. Pulmonary absorption of ethanol is most important in the workplace, while percutaneous absorption is of secondary importance [124].
Acute toxicity
No local irritation occurs at ethanol concentrations up to 5000 ppm and no systemic effects occur up to 1000 ppm after many years of occupational experience [125]. In recent testing among volunteers, at 1000 ppm, no exposure-related changes in reaction time, choice response, or short-term memory were noted, nor was discomfort felt. First effects on the central nervous system (CNS) are expected only at much higher concentrations, producing blood alcohol levels in the range of 200 mg ethanol/L [125]. The blood alcohol levels achieved by exposures far above those related to hand antisepsis are on average more than 100-fold lower (Table 6).
When taken orally, CNS performance may already be impaired at blood levels of 200–300 mg ethanol/L; above 600–700 mg/L the CNS is significantly affected in the majority of people [125]. Thus, when EBHR is used for hand antisepsis, a resorption-related influence on the CNS can be absolutely excluded (Table 6).
Chronic toxicity
No data are available on the effects of long-term inhalation exposure, although industrial workplaces where exposure opportunities exist are common.
Chronic consumption of large quantities of alcoholic beverages can lead to toxic effects on almost all organ systems. The liver is particularly affected, where damage initially manifests as fatty degeneration and can progress via necrotic and fibrotic stages to liver cirrhosis. The threshold value for triggering toxic liver damage is assumed to be 20–40 g/day for women and 60—80 g/day of ethanol for men with regular oral intake [125].
Fetotoxic and teratogenic potential
The risk of fetal damage is unlikely provided the MAK value of 380 mg/m3 is not exceeded [126].
A teratogenic effect (alcohol embryopathy) has been demonstrated after oral intake of high doses. However, the ethanol concentrations in maternal blood at which these effects occur are of a magnitude not reached by inhalation exposure in the occupationally relevant concentration range. In animal studies, concentrations up to 20,000 ppm had no effect on the offspring, despite toxic effects on the mothers. A fertility-reducing effect and the influencing of sex hormone levels have likewise been demonstrated in humans and in animal experiments only after oral intake of high doses [126].
Mutagenic potential
In animal studies, mutagenic effects were observed only at doses within the toxic range [126]. Since occupationally permissible ethanol concentrations do not significantly increase lifetime exposure, the mutagenic potential is considered negligible under these conditions.
Carcinogenic potential
Long-term ingestion of large amounts of ethanol in the form of alcoholic beverages can cause tumors of the mouth, pharynx, larynx, oesophagus, liver, and possibly mammary glands and intestines. Since it has been shown that the lifetime internal exposure to ethanol from occupational exposure up to 500 ppm is still within the standard deviation of the endogenous exposure, it is estimated that exposure up to this limit does not contribute significantly to cancer risk [126].
The Poisindex® [127] provides the following classification for ethanol:
-
TLV-TWA (Threshold Limit Value—Time-Weighted Average): Not listed.
-
TLV-STEL (Threshold Limit Value–Short-Term Exposure Limit (TLV-STEL): 1000 ppm.
-
TLV-C (Threshold Limit Value–Short-Term Exposure Limit (TLV-STEL): Not listed.
-
Carcinogenicity Category: A3 (definition: confirmed animal carcinogen with unknown relevance to humans: the agent is carcinogenic in experimental animals at a relatively high dose, by route(s) of administration, at site(s), of histologic type(s), or by mechanism(s) that may not be relevant to worker exposure. Available epidemiologic studies do not confirm an increased risk of cancer in exposed humans. Available evidence does not suggest that the agent is likely to cause cancer in humans except under uncommon or unlikely routes or levels of exposure [128]).
An earlier published assessment with another type of classification came to an analogous conclusion and classified ethanol in category 5, defined “substances with carcinogenic and genotoxic effects, the potency of which is considered to be so low that, provided the MAK and BAT values are observed, no significant contribution to human cancer risk is to be expected. The classification is supported by information on the mode of action, dose dependence and toxicokinetic data pertinent to species comparison” [129].
It should be noted that these assessments were made for continuous occupational exposure during inhalation by handling of ethanol and are not comparable to the use of EBRH for hand antisepsis.
The values for acute and chronic toxicity or fetotoxic, teratogenic, mutagenic and carcinogenic effects refer exclusively to oral exposure. Initial effects are described at blood concentrations > 200 mg/L. Blood alcohol levels achieved with significantly higher-than-real-exposure by hand antisepsis, i.e., 10 applications of EBHR for 3 min each at 5-min intervals, were found to be considerably lower, with a maximum of 30.1 mg ethanol/L (Table 4). Thus, there is no indication of any acute or chronic hazard associated with the use of EBHR for hand antisepsis.
Conclusion
Since 1977, the WHO has maintained a list of critical medications (WHO List of Essential Medicines), last updated in 2019. On that list, ethanol (70%, denatured) appears under antiseptics (15.1. Antiseptics) and under alcohol-based hand antisepsis agents (80% v/v; 15.2. Disinfectants) [130]. Ethanol is featured on the core list of basic-care active substances that should be available.
The doses of ethanol contained in EBHR and absorbed through the skin are in the range of those associated with the consumption of beverages with hidden ethanol content ≤ 0.5% v/v, such as apple juice and kefir, which are considered safe in accordance with EU Regulation No 1169/2011 (alcoholic content of beverages must be declared if it is higher than 1.2%). All studies support the conclusion that there is no significant risk of developmental or reproductive toxicity from repeated use of EBHR. Furthermore, the toxicological assessment concludes that dermal uptake of ethanol by health care workers or consumers would never result in exposure levels that are hazardous to health. Pires et al. [131] conclude “that the dermal and inhaled absorption of ethanol when using EBHR is minor and results in blood and urine concentrations comparable with other widely used alcohol-containing products of daily life.” The modeling approach of ethanol pharmacokinetics predicts that the consumption of one nonalcoholic beverage (estimated content of ethanol 0.5% vol/vol) would result in a peak blood concentration of 12 mg/L [107], an amount comparable with estimates resulting from intensive use of EBHRs. It should be remembered that EBHR can be produced locally from sugar cane, maize, manioc, rice, or several other natural by-products at a very low cost, using the procedure proposed by the World Health Organization, with extensive experience in many countries and health-care settings worldwide [5].
Hence, the WHO Task Force ABHR and KRINKO emphatically recommend maintaining ethanol as a biocidally active ingredient in hand rubs for use in healthcare settings. Ethanol used in EBHR is an effective and safe agent for the prevention of healthcare associated infections and spread of antimicrobial resistance. There are currently no alternatives to challenge the use of EBHR and we advocate continued use. If removed from our arsenal, we would lose a critical weapon against healthcare associated infections and risk a resulting increase in morbidity and mortality among patients worldwide.
Availability of data and material
Not applicable.
References
Regulation (EC) No 1272/2008 of the European Parliament and of the Council of 16 December 2008 on classification, labelling and packaging of substances and mixtures, amending and repealing. Directives 67/548/EEC and 1999/45/EC, and amending Regulation (EC) No 1907/2006. Official Journal of the European Union. L 353 (2008).
Regulation (EU) No 528/2012 of the European Parliament and of the Council of 22 May 2012 concerning the making available on the market and use of biocidal products. Off J Eur Union L 167 (2012).
European Chemical Agency (ECHA). Registry of CLH intentions until outcome. Ethanol, EC / List no: 200-578-6, CAS no: 64-17-5. 2021. https://echa.europa.eu/de/registry-of-clh-intentions-until-outcome/-/dislist/details/0b0236e1852d3d63 Accessed 14 March 2022.
Verbund für Angewandte Hygiene (VAH). As a biocidal active substance, ethanol is indispensable for hygienic hand disinfection. Zentralsterilization. 2020; 28(6):354–9.
World Health Organization (WHO). Guide to local production: WHO-recommended Handrub Formulations. 2010. www.who.int/gpsc/5may/Guide_to_Local_Production.pdf Accessed 14 March 2022.
Bloomfield SF, Aiello AE, Cookson B, O’Boyle C, Larson EL. The effectiveness of hand hygiene procedures in reducing the risks of infections in home and community settings including handwashing and alcohol-based hand sanitizers. Am J Infect Control. 2007;35(10, Suppl 1):S27–64. https://doi.org/10.1016/j.ajic.2007.07.001.
Kampf G, Löffler H. Prevention of irritant contact dermatitis among health care workers by using evidence-based hand hygiene practices: a review. Ind Health. 2007;45(5):645–52. https://doi.org/10.2486/indhealth.45.645.
Kampf G, Löffler H, Gastmeier P. Hand hygiene for the prevention of nosocomial infections. Dtsch Arztebl Int. 2009;106(40):649–55. https://doi.org/10.3238/arztebl.2009.0649.
Kramer A, Bernig T, Kampf G. Clinical double-blind trial on the dermal tolerance and user acceptability of six alcohol-based hand disinfectants for hygienic hand disinfection. J Hosp Infect. 2002;51(2):114–20. https://doi.org/10.1053/jhin.2002.1223.
Meyer B, Matthies W, Nicholson J, Shelanski M. Skin compatibility of two ethanol based virucidal hand disinfectants. Int J Infect Control. 2010;6(2):1–8. https://doi.org/10.3396/ijic.v6i2.010.13.
Ripabelli G, Tamburro M, Guerrizio G, Fanelli I, Agnusdei CP, Sammarco ML. A single-arm study to evaluate skin tolerance, effectiveness and adherence to use of an alcohol-based hand rub solution among hospital nurses. J Infect Prev. 2019;20(5):224–30. https://doi.org/10.1177/1757177419846295.
Kampf G. Efficacy of ethanol against viruses in hand disinfection. J Hosp Infect. 2018;98(4):331–8. https://doi.org/10.1016/j.jhin.2017.08.025.
Steinmann J, Becker B, Bischoff B, Paulmann D, Friesland M, Pietschmann T, et al. Virucidal activity of 2 alcohol-based formulations proposed as hand rubs by the World Health Organization. Am J Infect Control. 2010;38(1):66–8. https://doi.org/10.1016/j.ajic.2009.07.009.
Lin Q, Lim JYC, Xue K, Yew PYM, Owh C, Chee PL, et al. Sanitizing agents for virus inactivation and disinfection. View (Beijing). 2020:e16. https://doi.org/10.1002/viw2.16
Mbithi JN, Springthorpe VS, Sattar SA. Chemical disinfection of hepatitis A virus on environmental surfaces. Appl Environ Microbiol. 1990;56(11):3601–4. https://doi.org/10.1128/aem.56.11.3601-3604.1990.
Noda N, Watanabe M, Yamada F, Fujimoto S. Virucidal activity of alcohols. Virucidal efficiency of alcohols against viruses in liquid phase (author’s transl). Kansenshogaku Zasshi. 1981;55(5):355–66. https://doi.org/10.11150/kansenshogakuzasshi1970.55.355.
Eggers M, Benzinger C, Suchomel M, Hjorth E. Virucidal activity of three ethanol-based hand rubs against murine norovirus in a hand hygiene clinical simulation study. Fut Microbiol. 2020;15:1335–41. https://doi.org/10.2217/fmb-2020-0168.
Ionidis G, Hubscher J, Jack T, Becker B, Bischoff B, Todt D, et al. Development and virucidal activity of a novel alcohol-based hand disinfectant supplemented with urea and citric acid. BMC Infect Dis. 2016;16:77. https://doi.org/10.1186/s12879-016-1410-9.
Kramer A, Galabov AS, Sattar SA, Dohner L, Pivert A, Payan C, et al. Virucidal activity of a new hand disinfectant with reduced ethanol content: comparison with other alcohol-based formulations. J Hosp Infect. 2006;62(1):98–106. https://doi.org/10.1016/j.jhin.2005.06.020.
Steinmann J, Becker B, Bischoff B, Magulski T, Steinmann J, Steinmann E. Virucidal activity of Formulation I of the World Health Organization’s alcohol-based handrubs: impact of changes in key ingredient levels and test parameters. Antimicrob Resist Infect Control. 2013;2(1):34. https://doi.org/10.1186/2047-2994-2-34.
Su Y, Han J, Li J, Ren Z, Huang L, Xu B, et al. Resistance of poliovirus 1 and enterovirus A71 against alcohol and other disinfectants. J Virol Methods. 2021;298:114292. https://doi.org/10.1016/j.jviromet.2021.114292.
Wutzler P, Sauerbrei A. Virucidal efficacy of a combination of 0.2% peracetic acid and 80% (v/v) ethanol (PAA-ethanol) as a potential hand disinfectant. J Hosp Infect. 2000;46(4):304–8. https://doi.org/10.1053/jhin.2000.0850.
Iso-Propanol KG. In: Kampf G, editor. Kompendium Händehygiene. Wiesbaden: mhp; 2017. p. 362–75.
prEN 17430:2019 (Draft). Chemical disinfectants and antiseptics-Hygienic handrub virucidal - Test method and requirements (phase 2/step 2). Berlin: Beuth.
Iwasawa A, Niwano Y, Kohno M, Ayaki M. Virucidal activity of alcohol-based hand rub disinfectants. Biocontrol Sci. 2012;17(1):45–9. https://doi.org/10.4265/bio.17.45.
Uzuner H, Karadenizli A, Er DK, Osmani A. Investigation of the efficacy of alcohol-based solutions on adenovirus serotypes 8, 19 and 37, common causes of epidemic keratoconjunctivitis, after an adenovirus outbreak in hospital. J Hosp Infect. 2018;100(3):e30–6. https://doi.org/10.1016/j.jhin.2018.05.011.
Klein M, Deforest A. Antiviral action of germicides. Soap Chem Special. 1963;39:70–97.
Moldenhauer D. Quantitative evaluation of the effects of disinfectants against viruses in suspension experiments. Zentralbl Bakteriol Mikrobiol Hyg B. 1984;179(6):544–54.
Drulak M, Wallbank AM, Lebtag I. The relative effectiveness of commonly used disinfectants in inactivation of echovirus 11. J Hyg (Lond). 1978;81(1):77–87. https://doi.org/10.1017/s002217240005378x.
Eggers HJ. Experiments on antiviral activity of hand disinfectants. Some theoretical and practical considerations. Zentralbl Bakteriol. 1990;273(1):36–51. https://doi.org/10.1016/s0934-8840(11)80238-0.
Kurtz JB. Virucidal effect of alcohols against echovirus 11. Lancet. 1979;1(8114):496–7. https://doi.org/10.1016/s0140-6736(79)90852-3.
Park GW, Barclay L, Macinga D, Charbonneau D, Pettigrew CA, Vinjé J. Comparative efficacy of seven hand sanitizers against murine norovirus, feline calicivirus, and GII.4 norovirus. J Food Prot. 2010;73(12):2232–8. https://doi.org/10.4315/0362-028x-73.12.2232.
Wolff MH, Schmitt J, Rahaus M, König A. Hepatitis A virus: a test method for virucidal activity. J Hosp Infect. 2001;48(Suppl A):S18–22. https://doi.org/10.1016/s0195-6701(01)90007-6.
Kampf G, Ostermeyer C, Werner H-P, Suchomel M. Efficacy of hand rubs with a low alcohol concentration listed as effective by a national hospital hygiene society in Europe. Antimicrob Resist Infect Control. 2013;2:19. https://doi.org/10.1186/2047-2994-2-19.
Steinmann J, Paulmann D, Becker B, Bischoff B, Steinmann E, Steinmann J. Comparison of virucidal activity of alcohol-based hand sanitizers versus antimicrobial hand soaps in vitro and in vivo. J Hosp Infect. 2012;82(4):277–80. https://doi.org/10.1016/j.jhin.2012.08.005.
Tyler R, Ayliffe GA, Bradley C. Virucidal activity of disinfectants: studies with the poliovirus. J Hosp Infect. 1990;15(4):339–45. https://doi.org/10.1016/0195-6701(90)90090-b.
Schürmann W, Eggers HJ. Antiviral activity of an alcoholic hand disinfectant. Comparison of the in vitro suspension test with in vivo experiments on hands, and on individual fingertips. Antiviral Res. 1983;3(1):25–41. https://doi.org/10.1016/0166-3542(83)90012-8.
Hufbauer M, Wieland U, Gebel J, Steinmann J, Akgül B, Eggers M. Inactivation of polyomavirus SV40 as surrogate for human papillomaviruses by chemical disinfectants. Viruses. 2021;13(11):2207. https://doi.org/10.3390/v13112207.
Savolainen-Kopra C, Korpela T, Simonen-Tikka ML, Amiryousefi A, Ziegler T, Roivainen M, et al. Single treatment with ethanol hand rub is ineffective against human rhinovirus–hand washing with soap and water removes the virus efficiently. J Med Virol. 2012;84(3):543–7. https://doi.org/10.1002/jmv.23222.
Kampf G, Rudolf M, Labadie JC, Barrett SP. Spectrum of antimicrobial activity and user acceptability of the hand disinfectant agent Sterillium Gel. J Hosp Infect. 2002;52(2):141–7. https://doi.org/10.1053/jhin.2002.1281.
Aitken C, Jeffries DJ. Nosocomial spread of viral disease. Clin Microbiol Rev. 2001;14(3):528–46. https://doi.org/10.1128/CMR.14.3.528-546.2001.
Baptiste R, Koziol D, Henderson DK. Nosocomial transmission of hepatitis A in an adult population. Infect Control. 1987;8(9):364–70. https://doi.org/10.1017/s0195941700067424.
Anderson CE, Boehm AB. Transfer rate of enveloped and nonenveloped viruses between fingerpads and surfaces. Appl Environ Microbiol. 2021;87(22):e0121521. https://doi.org/10.1128/aem.01215-21.
Julian TR, Leckie JO, Boehm AB. Virus transfer between fingerpads and fomites. J Appl Microbiol. 2010;109(6):1868–74. https://doi.org/10.1111/j.1365-2672.2010.04814.x.
Flemmer M, Oldfield EC 3rd. The agony and the ecstasy. Am J Gastroenterol. 2003;98(9):2098–9. https://doi.org/10.1111/j.1572-0241.2003.07672.x.
Armbrust S, Kramer A, Olbertz D, Zimmermann K, Fusch C. Norovirus infections in preterm infants: wide variety of clinical courses. BMC Res Notes. 2009;2:96. https://doi.org/10.1186/1756-0500-2-96.
Barclay L, Park GW, Vega E, Hall A, Parashar U, Vinje J, et al. Infection control for norovirus. Clin Microbiol Infect. 2014;20(8):731–40. https://doi.org/10.1111/1469-0691.12674.
Cheng VC, Tai JW, Ho YY, Chan JF. Successful control of norovirus outbreak in an infirmary with the use of alcohol-based hand rub. J Hosp Infect. 2009;72(4):370–1. https://doi.org/10.1016/j.jhin.2009.04.021.
Todd EC, Michaels BS, Holah J, Smith D, Greig JD, Bartleson CA. Outbreaks where food workers have been implicated in the spread of foodborne disease. Part 10. Alcohol-based antiseptics for hand disinfection and a comparison of their effectiveness with soaps. J Food Prot. 2010;73(11):2128–40. https://doi.org/10.4315/0362-028x-73.11.2128.
Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, et al. Foodborne illness acquired in the United States–major pathogens. Emerg Infect Dis. 2011;17(1):7–15. https://doi.org/10.3201/eid1701.P11101.
Kirk MD, Pires SM, Black RE, Caipo M, Crump JA, Devleesschauwer B, et al. Correction: World Health Organization estimates of the global and regional disease burden of 22 foodborne bacterial, protozoal, and viral diseases, 2010: a data synthesis. PLoS Med. 2015;12(12):e1001940. https://doi.org/10.1371/journal.pmed.1001940.
Boyce JM, Schaffner DW. Scientific evidence supports the use of alcohol based hand sanitizers as an effective alternative to handwashing in retail food and foodservice settings when heavy soiling is not present on hands. J Food Prot. 2021;84(5):781–801. https://doi.org/10.4315/JFP-20-326.
Steinmann J, Becker B, Bischoff B, Steinmann E. Alcohol hand rub or soap and water for removal of norovirus from hands-the debate continues. J Hosp Infect. 2015;91(4):371–2. https://doi.org/10.1016/j.jhin.2015.07.015.
Eggers M, Koburger-Janssen T, Ward LS, Newby C, Muller S. Bactericidal and virucidal activity of povidone-iodine and chlorhexidine gluconate cleansers in an in vivo hand hygiene clinical simulation study. Infect Dis Ther. 2018;7(2):235–47. https://doi.org/10.1007/s40121-018-0202-5.
Steinmann J, Becker BBB, Paulmann D, Steinmann J, Steinmann E. Old and new findings on the viral efficacy of hygienic hand disinfection. Hyg Med. 2009;34(1/2):32–40.
Tuladhar E, Hazeleger WC, Koopmans M, Zwietering MH, Duizer E, Beumer RR. Reducing viral contamination from finger pads: handwashing is more effective than alcohol-based hand disinfectants. J Hosp Infect. 2015;90(3):226–34. https://doi.org/10.1016/j.jhin.2015.02.019.
Fraser A, Pittet Arbogast J, Jaykus L. Rethinking hand hygiene in the retail and foodservice industries: are recommended procedures based on the best science and practical under real-world conditions. Food Prot Trends. 2012;32(12):750–9.
Flomenberg P, Kojaoghlanian T, Kaplan SL. Pathogenesis, epidemiology, and clinical manifestations of adenovirus infection (last updated: Jun 07, 2021). 2021. https://www.uptodate.com/contents/pathogenesis-epidemiology-and-clinical-manifestations-of-adenovirus-infection Accessed 14 March 2022.
Oristo S, Ronnqvist M, Aho M, Sovijarvi A, Hannila-Handelberg T, Horman A, et al. Contamination by norovirus and adenovirus on environmental surfaces and in hands of conscripts in two finnish garrisons. Food Environ Virol. 2017;9(1):62–71. https://doi.org/10.1007/s12560-016-9262-4.
Centers for Disease Control and Prevention (CDC). Outbreaks. Adenovirus types that can cause outbreaks. 2019. https://www.cdc.gov/adenovirus/outbreaks.html Accessed 14 March 2022.
Grubman MJ, Baxt B. Foot-and-mouth disease. Clin Microbiol Rev. 2004;17(2):465–93. https://doi.org/10.1128/CMR.17.2.465-493.2004.
Kobayashi H, Shinjoh M, Sudo K, Kato S, Morozumi M, Koinuma G, et al. Nosocomial infection by human bocavirus and human rhinovirus among paediatric patients with respiratory risks. J Hosp Infect. 2019;103(3):341–8. https://doi.org/10.1016/j.jhin.2019.05.002.
Ma E, Fung C, Yip SH, Wong C, Chuang SK, Tsang T. Estimation of the basic reproduction number of enterovirus 71 and coxsackievirus A16 in hand, foot, and mouth disease outbreaks. Pediatr Infect Dis J. 2011;30(8):675–9. https://doi.org/10.1097/INF.0b013e3182116e95.
Nguyen A, Le Nguyen TN, Hoang MTV, Hong N, Tran Tan T, Hang V, et al. Emerging coxsackievirus A6 causing hand, foot and mouth disease. Vietnam Emerg Infect Dis. 2018;24(4):654–62. https://doi.org/10.3201/eid2404.171298.
Bian L, Wang Y, Yao X, Mao Q, Xu M, Liang Z. Coxsackievirus A6: a new emerging pathogen causing hand, foot and mouth disease outbreaks worldwide. Expert Rev Anti Infect Ther. 2015;13(9):1061–71. https://doi.org/10.1586/14787210.2015.1058156.
Modlin JF, Hirsch MS, Bogorodskaya M. Enterovirus and parechovirus infections: Epidemiology and pathogenesis (last updated: Mar 16, 2021). 2021. https://www.uptodate.com/contents/enterovirus-and-parechovirus-infections-epidemiology-and-pathogenesis Accessed 14 March 2022.
Doebbeling BN, Li N, Wenzel RP. An outbreak of hepatitis A among health care workers: risk factors for transmission. Am J Public Health. 1993;83(12):1679–84. https://doi.org/10.2105/ajph.83.12.1679.
Hanna JN, Loewenthal MR, Negel P, Wenck DJ. An outbreak of hepatitis A in an intensive care unit. Anaesth Intensive Care. 1996;24(4):440–4. https://doi.org/10.1177/0310057X9602400405.
Klein BS, Michaels JA, Rytel MW, Berg KG, Davis JP. Nosocomial hepatitis A. A multinursery outbreak in Wisconsin. JAMA. 1984;252(19):2716–21. https://doi.org/10.1001/jama.252.19.2716.
Jensenius M, Ringertz SH, Berild D, Bell H, Espinoza R, Grinde B. Prolonged nosocomial outbreak of hepatitis A arising from an alcoholic with pneumonia. Scand J Infect Dis. 1998;30(2):119–23. https://doi.org/10.1080/003655498750003474.
Krober MS, Bass JW, Brown JD, Lemon SM, Rupert KJ. Hospital outbreak of hepatitis A: risk factors for spread. Pediatr Infect Dis. 1984;3(4):296–9. https://doi.org/10.1097/00006454-198407000-00003.
Azimi PH, Roberto RR, Guralnik J, Livermore T, Hoag S, Hagens S, et al. Transfusion-acquired hepatitis A in a premature infant with secondary nosocomial spread in an intensive care nursery. Am J Dis Child. 1986;140(1):23–7. https://doi.org/10.1001/archpedi.1986.02140150025024.
Drusin LM, Sohmer M, Groshen SL, Spiritos MD, Senterfit LB, Christenson WN. Nosocomial hepatitis A infection in a paediatric intensive care unit. Arch Dis Child. 1987;62(7):690–5. https://doi.org/10.1136/adc.62.7.690.
Watson JC, Fleming DW, Borella AJ, Olcott ES, Conrad RE, Baron RC. Vertical transmission of hepatitis A resulting in an outbreak in a neonatal intensive care unit. J Infect Dis. 1993;167(3):567–71. https://doi.org/10.1093/infdis/167.3.567.
Burkholder BT, Coronado VG, Brown J, Hutto JH, Shapiro CN, Robertson B, et al. Nosocomial transmission of hepatitis A in a pediatric hospital traced to an anti-hepatitis A virus-negative patient with immunodeficiency. Pediatr Infect Dis J. 1995;14(4):261–6. https://doi.org/10.1097/00006454-199504000-00003.
Goodman RA, Carder CC, Allen JR, Orenstein WA, Finton RJ. Nosocomial hepatitis A transmission by an adult patient with diarrhea. Am J Med. 1982;73(2):220–6. https://doi.org/10.1016/0002-9343(82)90182-6.
Edgar WM, Campbell AD. Nosocomial infection with hepatitis A. J Infect. 1985;10(1):43–7. https://doi.org/10.1016/s0163-4453(85)80008-6.
Skidmore SJ, Gully PR, Middleton JD, Hassam ZA, Singal GM. An outbreak of hepatitis A on a hospital ward. J Med Virol. 1985;17(2):175–7. https://doi.org/10.1002/jmv.1890170210.
Teshale EH, Grytdal SP, Howard C, Barry V, Kamili S, Drobeniuc J, et al. Evidence of person-to-person transmission of hepatitis E virus during a large outbreak in Northern Uganda. Clin Infect Dis. 2010;50(7):1006–10. https://doi.org/10.1086/651077.
Teshale EH, Howard CM, Grytdal SP, Handzel TR, Barry V, Kamili S, et al. Hepatitis E epidemic, Uganda. Emerg Infect Dis. 2010;16(1):126–9. https://doi.org/10.3201/eid1601.090764.
Liu Z, Rashid T, Nyitray AG. Penises not required: a systematic review of the potential for human papillomavirus horizontal transmission that is non-sexual or does not include penile penetration. Sex Health. 2016;13(1):10–21. https://doi.org/10.1071/sh15089.
M’Zali F, Bounizra C, Leroy S, Mekki Y, Quentin-Noury C, Kann M. Persistence of microbial contamination on transvaginal ultrasound probes despite low-level disinfection procedure. PLoS ONE. 2014;9(4):e93368. https://doi.org/10.1371/journal.pone.0093368.
Casalegno JS, Le Bail CK, Eibach D, Valdeyron ML, Lamblin G, Jacquemoud H, et al. High risk HPV contamination of endocavity vaginal ultrasound probes: an underestimated route of nosocomial infection? PLoS ONE. 2012;7(10):e48137. https://doi.org/10.1371/journal.pone.0048137.
Ryndock EJ, Meyers C. A risk for non-sexual transmission of human papillomavirus? Expert Rev Anti Infect Ther. 2014;12(10):1165–70. https://doi.org/10.1586/14787210.2014.959497.
Pappas DE, Hirsch MS, Edwards MS, Hall KK. Epidemiology, clinical manifestations, and pathogenesis of rhinovirus infections. 2021. https://www.uptodate.com/contents/epidemiology-clinical-manifestations-and-pathogenesis-of-rhinovirus-infections Accessed 14 March 2022.
Greig JD, Lee MB. A review of nosocomial norovirus outbreaks: infection control interventions found effective. Epidemiol Infect. 2012;140(7):1151–60. https://doi.org/10.1017/s0950268811002731.
Parrón I, Álvarez J, Jané M, Cornejo Sánchez T, Razquin E, Guix S, et al. A foodborne norovirus outbreak in a nursing home and spread to staff and their household contacts. Epidemiol Infect. 2019;147:e225. https://doi.org/10.1017/s0950268819001146.
Adler SP, Manganello AM, Koch WC, Hempfling SH, Best AM. Risk of human parvovirus B19 infections among school and hospital employees during endemic periods. J Infect Dis. 1993;168(2):361–8. https://doi.org/10.1093/infdis/168.2.361.
Modrow S. Parvovirus B19: Ein Infektionserreger mit vielen Erkrankungsbildern. Dtsch Arztebl Int. 2001;98(24):A1620–4.
Niendorf S, Ebner W, Marques AM, Bierbaum S, Babikir R, Huzly D, et al. Rotavirus outbreak among adults in a university hospital in Germany. J Clin Virol. 2020;129:104532. https://doi.org/10.1016/j.jcv.2020.104532.
European Centre for Disease Prevention and Control (ECDC). Disease factsheet about poliomyelitis. (updated 15 Sep 2021). https://www.ecdc.europa.eu/en/poliomyelitis/facts Accessed 14 March 2022.
Kampf G, Kramer A. Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clin Microbiol Rev. 2004;17(4):863–93. https://doi.org/10.1128/cmr.17.4.863-893.2004.
Barker J, Vipond IB, Bloomfield SF. Effects of cleaning and disinfection in reducing the spread of Norovirus contamination via environmental surfaces. J Hosp Infect. 2004;58(1):42–9. https://doi.org/10.1016/j.jhin.2004.04.021.
Rönnqvist M, Aho E, Mikkelä A, Ranta J, Tuominen P, Rättö M, et al. Norovirus transmission between hands, gloves, utensils, and fresh produce during simulated food handling. Appl Environ Microbiol. 2014;80(17):5403–10. https://doi.org/10.1128/aem.01162-14.
Ansari SA, Springthorpe VS, Sattar SA, Rivard S, Rahman M. Potential role of hands in the spread of respiratory viral infections: studies with human parainfluenza virus 3 and rhinovirus 14. J Clin Microbiol. 1991;29(10):2115–9. https://doi.org/10.1128/jcm.29.10.2115-2119.1991.
Ansari SA, Sattar SA, Springthorpe VS, Wells GA, Tostowaryk W. Rotavirus survival on human hands and transfer of infectious virus to animate and nonporous inanimate surfaces. J Clin Microbiol. 1988;26(8):1513–8. https://doi.org/10.1128/jcm.26.8.1513-1518.1988.
Hadi HA, Hill JA, Castillo RA. Alcohol and reproductive function: a review. Obstet Gynecol Surv. 1987;42(2):69–74.
Wittmann S, Gilg T, Dietz HG, Grantzow R, Peschel O, Meyer L. Isopropanol and acetone serum levels after presurgical disinfection with isopropanol containing antiseptics. Blutalkohol. 1992;29:326–35.
Peschel O, Bauer MF, Gilg T, Meyer L. Change in congener analysis caused by percutaneous absorption of propanol-containing antiseptics. Blutalkohol. 1992;29:172–84.
Iffland R, Balling P, Oehmichen M, Lieder F, Norpoth T. Methanol, isopropanol, n-propanol-endogenous formation affected by alcohol? Blutalkohol. 1989;26:87–97.
Tiess D. Endogenes isopropanol (propan-2-ol). Endogenous isopropanol (propan-2-ol). Current state of knowledge, forensic and toxicological relevance (short message). Kriminalistik. 1986;63(64):160–2.
Below H, Partecke I, Huebner NO, Bieber N, Nicolai T, Usche A, et al. Dermal and pulmonary absorption of propan-1-ol and propan-2-ol from hand rubs. Am J Infect Control. 2012;40(3):250–7. https://doi.org/10.1016/j.ajic.2011.03.009.
Kramer A, Below H, Bieber N, Kampf G, Toma CD, Huebner NO, et al. Quantity of ethanol absorption after excessive hand disinfection using three commercially available hand rubs is minimal and below toxic levels for humans. BMC Infect Dis. 2007;7:117. https://doi.org/10.1186/1471-2334-7-117.
Miller MA, Rosin A, Levsky ME, Patel MM, Gregory TJ, Crystal CS. Does the clinical use of ethanol-based hand sanitizer elevate blood alcohol levels? A prospective study. Am J Emerg Med. 2006;24(7):815–7. https://doi.org/10.1016/j.ajem.2006.05.006.
Huynh-Delerme C, Artigou C, Bodin L, Tardif R, Charest-Tardif G, Verdier C, et al. Short communication: is ethanol-based hand sanitizer involved in acute pancreatitis after excessive disinfection? an evaluation with the use of PBPK model. J Toxicol. 2012;2012(3):959070. https://doi.org/10.1155/2012/959070.
Windirsch B, Brinkmann B. H. T. Alkoholgehalte ausgewählter Lebensmittel. Lebensmittelchemie. 2005;59:149–50.
Al-Awadhi A, Wasfi IA, Al Reyami F, Al-Hatali Z. Autobrewing revisited: endogenous concentrations of blood ethanol in residents of the United Arab Emirates. Sci Justice. 2004;44(3):149–52. https://doi.org/10.1016/s1355-0306(04)71707-4.
Maier A, Ovesen JL, Allen CL, York RG, Gadagbui BK, Kirman CR, et al. Safety assessment for ethanol-based topical antiseptic use by health care workers: evaluation of developmental toxicity potential. Regul Toxicol Pharmacol. 2015;73(1):248–64. https://doi.org/10.1016/j.yrtph.2015.07.015.
Gessner S, Below E, Diedrich S, Wegner C, Gessner W, Kohlmann T, et al. Ethanol and ethyl glucuronide urine concentrations after ethanol-based hand antisepsis with and without permitted alcohol consumption. Am J Infect Control. 2016;44(9):999–1003. https://doi.org/10.1016/j.ajic.2016.02.021.
U.S. Department of Agriculture (USDA), U.S. Department of Health and Human Services (HHS). Dietary Guidelines for Americans, 2020–2025. 9th ed. 2020. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf Accessed 14 March 2022.
Goldberg IJ, Mosca L, Piano MR, Fisher EA. Wine and your heart. A science advisory for healthcare professionals from the nutrition committee, council on epidemiology and prevention, and council on cardiovascular Nursing of the American Heart Association. Circulation. 2001;103(3):472–5. https://doi.org/10.1161/01.CIR.103.3.472Circulation.
German Association for Nutrition (DGE), Austrian Nutrition Society (ÖGE), Swiss Society for Nutritional Research (SGE), Swiss Food Association (SVE). Alkohol. In: DGE, ÖGE, SGE, SVE, editors. Referenzwerte für die Nährstoffzufuhr. Frankfurt/Main: Umschau Braus, 2001: 65–7.
Kirschner MH, Lang RA, Breuer B, Breuer M, Gronover CS, Zwingers T, et al. Transdermal resorption of an ethanol- and 2-propanol-containing skin disinfectant. Langenbecks Arch Surg. 2009;394(1):151–7. https://doi.org/10.1007/s00423-007-0237-7.
Randall CL, Taylor WJ. Prenatal ethanol exposure in mice: teratogenic effects. Teratology. 1979;19(3):305–11. https://doi.org/10.1002/tera.1420190305.
Schwetz BA, Smith FA, Staples RE. Teratogenic potential of ethanol in mice, rats and rabbits. Teratology. 1978;18(3):385–92. https://doi.org/10.1002/tera.1420180313.
Nelson BK, Brightwell WS, MacKenzie DR, Khan A, Burg JR, Weigel WW, et al. Teratological assessment of methanol and ethanol at high inhalation levels in rats. Fundam Appl Toxicol. 1985;5(4):727–36. https://doi.org/10.1016/0272-0590(85)90197-6.
Nelson BK, Brightwell WS, Burg JR. Comparison of behavioral teratogenic effects of ethanol and n-propanol administered by inhalation to rats. Neurobehav Toxicol Teratol. 1985;7(6):779–83.
Nelson BK, Brightwell WS, MacKenzie-Taylor DR, Burg JR, Massari VJ. Neurochemical, but not behavioral, deviations in the offspring of rats following prenatal or paternal inhalation exposure to ethanol. Neurotoxicol Teratol. 1988;10(1):15–22. https://doi.org/10.1016/0892-0362(88)90062-1.
Abel EL. Rat offspring sired by males treated with alcohol. Alcohol. 1993;10(3):237–42. https://doi.org/10.1016/0741-8329(93)90042-m.
Irvine LF. Relevance of the developmental toxicity of ethanol in the occupational setting: a review. J Appl Toxicol. 2003;23(5):289–99. https://doi.org/10.1002/jat.937.
Holmberg B, Kronevi T, Ekner A, Swedish National Board of Occupational Safety and Health. Subchronic toxicity investigation of ethyl alcohol : a test for lowest effective dose (LED) to be used in long-term bioassay for carcinogenicity. Solna, Sweden: Arbetarskyddsstyrelsen; 1986.
1. Liste der nach den ''Richtlinien für die Prüfung chemischer Desinfektionsmittel'' geprüften und von der „Deutschen Gesellschaft für Hygiene und Mikrobiologie“ empfohlenen Desinfektionsmittel (Stand: 6.2.1959). Zbl Bakt Hyg 1 Abt Ref. 1959:72–6.
Deutsche Forschungsgemeinschaft (DFG). MAK- und BAT-Werte-Liste 2021. Ständige Senatskommission zur Prüfung gesundheitsschädlicher Arbeitsstoffe. Mitteilung 57. https://series.publisso.de/sites/default/files/documents/series/mak/lmbv/Vol2021/Iss1/Doc001/mbwl_2021_deu.pdf Accessed 10 June 2022.
Hartwig A. MAK Commission. Ethanol. MAK value documentation in German language. MAK Collect Occup Health Saf. 2018;3(2):683–92. https://doi.org/10.1002/3527600418.mb6417d0065.
Ethanol. In: Deutsche Forschungsgemeinschaft (DFG), editor. The MAK‐Collection for Occupational Health and Safety 1998: 1–38. https://doi.org/10.1002/3527600418.mb6417d0026
Institut für Arbeitsschutz der Deutschen Gesetzlichen Unfallversicherung (ifa). Ethanol (GESTIS-Stoffdatenbank). https://gestis.dguv.de/data?name=010420 Accessed 10 June 2022.
Ethanol. In: Poisindex® [database on the Internet]. IBM Corporation: Greenwood Village, CO, USA. 2021. www.micromedexsolutions.com Accessed 6 Decembre 2021.
American Conference of Governmental Industrial Hygienists. 2010 TLVs and BEIs: Based on the documentation of the threshold limit values for chemical substances and physical agents & biological exposure indices. Cincinnati, Ohio 2010.
Deutsche Forschungsgemeinschaft. MAK- und BAT-Werte-Liste 2002. Mitteilung 38, Wiley-VCH, Weinheim 2002.
World Health Organization (WHO). World Health Organization. Model List of Essential Medicines. 21st List, 2019. Geneva: WHO; 2019. https://apps.who.int/iris/rest/bitstreams/1237479/retrieve Accessed 10 June March 2022.
Pires D, Bellissimo-Rodrigues F, Pittet D. Ethanol-based handrubs: safe for patients and health care workers. Am J Infect Control. 2016;44(8):858–9. https://doi.org/10.1016/j.ajic.2016.02.016.
Acknowledgements
Not applicable
Funding
Open Access funding enabled and organized by Projekt DEAL. None. No funding to declare.
Author information
Authors and Affiliations
Contributions
AK conceive and designed the article, analyzed and interpreted the data. AK, MA, ME, DM, and DP were in the core writing group responsible for preparation of the manuscript. BC, SD, ME, ME NM, and IS were responsible for the quality of scientific data and their interpretation. The content of the submitted manuscript draft was reviewed and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing intrests
The authors declare that they have no competing interests. The memorandum was prepared voluntarily without conflicts of interest by the German Commission for Hospital Hygiene and Infection Prevention (Axel Kramer, head of the working group, Mardjan Arvand, Bärbel Christiansen, Stephanie Dancer, Maren Eggers, Martin Exner, Dieter Müller, Niko Mutters, Ingeborg Schwebke) and by the Alcohol Based Hand Rub (ABHR) Task Force of the WHO, Infection Control Programme & WHO Collaborating Centre on Patient Safety, The University of Geneva Hospitals and Faculty of Medicine Geneva, Switzerland (Didier Pittet, head of the task force).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kramer, A., Arvand, M., Christiansen, B. et al. Ethanol is indispensable for virucidal hand antisepsis: memorandum from the alcohol-based hand rub (ABHR) Task Force, WHO Collaborating Centre on Patient Safety, and the Commission for Hospital Hygiene and Infection Prevention (KRINKO), Robert Koch Institute, Berlin, Germany. Antimicrob Resist Infect Control 11, 93 (2022). https://doi.org/10.1186/s13756-022-01134-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-022-01134-7