Abstract
Background
Adolescents in residential substance use disorder (SUD) treatment have poor outcomes post-discharge, with follow-up studies suggesting that most adolescents relapse within 90 days. Parenting practices directly influence adolescent SUD outcomes, but parents of adolescents with SUDs are difficult to engage in traditional behavioral treatments. The current study adapts and evaluates a technology-assisted intervention for parents of adolescents in residential SUD treatment. Based on pilot qualitative data with parents, adolescents, and residential staff, we augment an existing computerized intervention (Parenting Wisely; PW) with four in-person coaching sessions, personalized text messages, and an expert-moderated online parent message board. We hypothesize that parents will find enhanced PW (PW+) both feasible and acceptable, and that adolescents whose parents receive PW+ will have better post-discharge outcomes than adolescents who receive standard care (SC) only.
Methods/design
A two phase approach is used to adapt and evaluate PW+. Phase 1 consists of an open trial with 10 parents of adolescents (age 12–17) in residential SUD treatment. Post-discharge qualitative and quantitative data from parents and adolescents will support PW+ refinement. Phase 2 is a randomized pilot trial with 60 parents testing the effectiveness of adding PW+ to SC. Adolescents and parents will complete assessments at baseline, 6-, 12-, and 24-weeks post-discharge. Primary outcomes will be measures of feasibility and acceptability. Secondary outcomes will include adolescent substance use, truancy, high-risk sexual behavior, and criminal involvement. Two parenting processes (monitoring and communication) are examined as potential mediators of change.
Discussion
This study will adapt and evaluate a technology-assisted parenting intervention as a means of improving adolescent outcomes following residential SUD treatment. Results have the potential to advance the field by: addressing a high-risk population, improving parental engagement; targeting parenting practices (putative mediators of change) that have been linked to adolescent outcomes; and developing a highly disseminable approach.
Similar content being viewed by others
Background
According to the most recent data from the National Survey of Substance Abuse Treatment Services, there are 3450 residential substance use treatment facilities in the United States and 10.3% of all adolescents who seek treatment for a substance use disorder (SUD) will receive treatment in this setting [1]. Adolescents with SUDs who require a residential level of care typically have the most severe symptoms and the highest rates of psychological, behavioral, legal, motivational, environmental, and vocational problems [2, 3]. Adolescents in residential SUD treatment are also at extremely high risk of relapse, with follow-up studies suggesting that 60% of adolescents discharged from residential SUD facilities will relapse within 90 days [4–6]. Despite such high relapse rates, the majority of adolescents in residential treatment either do not link to or only participate minimally in continuing care after discharge [7, 8]. In recognition of these challenges, a review of the continuing care literature [9] advised treatment developers to supplement or replace traditional clinic-based approaches with new service delivery approaches that are of lower burden and greater convenience, and that facilitate sustained contact with the patient for an extended period of time. Consistent with these recommendations, this study aims to adapt and evaluate a flexible, low cost, low intensity treatment model for parents preparing for their teen’s discharge from residential treatment.
Rationale for targeting parents
Parents have been established as a critical influence on adolescents’ initiation and maintenance of substance use [10], as well as their substance use outcomes and likelihood of relapse following treatment [11]. Two parenting processes that appear to be particularly important protective factors against adolescent SUDs are monitoring and supervision [12] and communication with the adolescent [13]. Parental monitoring has been identified as a pivotal factor in the initiation of adolescent substance use [10, 14–17] and several studies have implicated parental monitoring as a mechanism underlying adolescent substance use. For instance, one study of 4731 adolescents found that perceived parental monitoring had unique mediating effects on adolescent substance use [18], while other studies concluded that lax parental monitoring was one of the pathways through which parental substance use influenced adolescent substance use [19, 20]. Parental communication also appears to have important protective influences for adolescents with SUDs [10, 21, 22], with studies suggesting that the content, context, style and timing of communication about substance use are all important deterrents of use [23]. Several studies suggest that parenting interventions should target parent-teen communication about the parents’ attitudes toward substance use [24, 25]. One study [26] found that communicating strong parental norms against teen substance use reduced the risk of initiation in early adolescence, while two studies found that communicating disapproval of substance use predicted less alcohol use later in adolescence [24, 27].
Systematic reviews and meta-analyses of treatment approaches for adolescents with SUDs [28–31], including one conducted by this protocol’s Principal Investigator (PI; protocol first author) [32], have found that intervention models that include parents outperform other approaches and are supported by high quality evidence. In Kumpfer et al.’s [33] review of interventions for adolescents with SUDs, family-based interventions that involved a parent or caregiver had average effect sizes 2–9 times larger than adolescent-only interventions. A more recent meta-analysis by Tanner-Smith and colleagues [31] similarly found that family-based interventions outperformed other evidence-based behavioral treatment approaches. Numerous other studies have provided evidence that parent involvement in treatment can improve adolescent engagement, retention, and substance use outcomes [34–36]. This body of research provides justification for: (1) working with the parents of adolescents in residential treatment for SUDs and (2) for targeting parenting skills as a potential mechanism of change in adolescent SUD treatment outcome.
Limitations of prior parenting interventions
A key limitation of existing interventions for parents of adolescents with SUDs is the difficulty ensuring that parents receive an adequate “dose” of the intervention. In a 2014 systematic review of adolescent SUD interventions [28], those family models identified as “well-established” or “probably efficacious” ranged in intensity from 12 to 24 in-person sessions. Such a high dose of in-person sessions may be especially challenging for parents of adolescents transitioning out of residential SUD treatment, who are often difficult to engage in follow-up care [5]. Studies of adolescents discharged from residential SUD treatment demonstrate that only 36% will attend any continuing care sessions in the community [37]. Moreover, data from community treatment samples indicate that most adolescents who do attend treatment will drop out prematurely [38]. The few studies that have reported high retention rates of parents (i.e., [5, 8]; average of 14.4 sessions of continuing care) have predominantly relied upon home-based sessions or visits, an approach that may be challenging to implement within community programs that often lack adequate staffing and financial resources [39]. To date, there are no treatment models designed specifically to enhance parental engagement or increase parenting skills following the adolescent’s discharge from residential treatment. Thus, the current protocol addresses gaps in extant treatment options by adapting a low-cost, low intensity treatment model that addresses parent engagement and targets key parenting processes (i.e., monitoring and communication) within the prototypic constraints of an acute community residential program.
Rationale for technology-assisted interventions
To improve upon currently available parenting interventions, it is critically important that any new approach is not only effective, but also acceptable and feasible for both residential treatment center staff and parents. Technology-assisted interventions can potentially better fit the needs of both clinical staff and parents in a number of ways [40, 41]. First, technology-assisted programs have the key advantage of balancing flexibility with fidelity, by allowing the content to be individually tailored to the patient’s specific needs, while retaining core content elements. Second, technology-assisted interventions can be delivered at low-cost with low burden on staff time, thereby ameliorating well-documented challenges to implementing evidence-based interventions such as limited financial resources, front line staff availability, and supervisory support [42, 43]. Third, online programs delivered via computer or smartphone are especially promising due to ease of access. Eighty-seven percent of American adults report using the internet, including 77% of adults in households that earn below $30,000 [44]. Rates of internet usage among adults age 30–49 (a common age range of parents of adolescents) are even higher at 91% [44]. Fourth, recent studies have provided promising support for the effectiveness of computerized or online treatments for adolescents with substance-related problems as additives or alternatives to clinic-based therapy [45–49]. However, these studies have primarily focused on cigarette use [50], prevention rather than intervention [51, 52], and on the adolescent only without involving parents [53].
One online parenting intervention that has promise for parents of adolescents in residential SUD treatment is Parenting Wisely (PW [54]). PW is an internet-based, self-paced program that consists of nine modules. Each module addresses how to handle a common parenting problem including: addressing adolescent substance misuse, monitoring friends, and improving parent–child communication. Five prior studies (two open trials [53, 55], one control-matched trial [56], and two small randomized controlled trials [57, 58]) have specifically tested PW as an intervention for parents of children with behavior problems. Findings across these studies indicated that parental receipt of PW is associated with improvements in parental knowledge and social problem solving skills and reductions in child problem behaviors (measured by the Eyberg Child Behavior Inventory [59]), with medium to large effect sizes.
A recent NIDA funded pilot study (R44 DA026658) was the first to evaluate PW as an adjunct intervention among parents of adolescents with SUDs, all of whom were court referred due to marijuana use. The study compared an educational substance use intervention to a motivational enhancement therapy (MET) with PW. Unpublished pilot analyses of the 3-month outcomes (Don Gordon, private communication) based on 128 cases demonstrated that MET + PW had statistically significant beneficial effects relative to education on parent reports of adolescent emotional problems, conduct problems and total behavior problems. In addition, MET + PW produced reductions in adolescent alcohol and drug use relative to education, but the difference was not statistically significant. Further analyses indicated a significant dosage effect for PW: completion of more PW modules was associated with significantly greater reductions in adolescent alcohol and drug use. Effect sizes were generally small in magnitude. This body of work provides evidence in support of PW as a means of reducing child behavior problems [36–38], with some pilot data suggesting that PW has the potential to address adolescent SUDs.
Although the data in support of PW are promising, use of the program is limited when delivered online only. For instance, a 2013 study [60] compared four different PW delivery models and found that delivery of PW content via 5 weeks of in-person groups resulted in significantly larger improvements in parenting skills than PW delivery via internet only. This is consistent with data indicating that new technology-delivered applications are often limited by lack of sustained use; for instance, in 2015, 25% of phone apps that were downloaded were only used once in the first 6 months of ownership [61]. The true challenge therefore is not developing new and exciting technology-delivered interventions, but the “need for collaborative techniques to enhance and maintain usage in vivo to improve therapy outcomes” [62]. A number of studies of adults and adolescents have shown that technology-delivered interventions have positive, sustained effects when combined with low intensity in-person support [63–65]. Thus, instead of comparing in-person versus online delivery, this protocol tests the potential value of an additive (in person + online) technology-assisted approach. Furthermore, this protocol augments the PW program with other technology-assisted parental engagement strategies.
Overview of adaptations to Parenting Wisely tested in this protocol
This protocol examines three adaptations to the PW online model based on qualitative pilot data from 13 parents (7 parents of females, 6 parents of males), 11 adolescents (5 females, 6 males) in residential treatment, and three residential treatment staff (see Table 1 for summary of themes) that were collected as part of a larger qualitative study [66, 67]. First, based on qualitative data indicating that parents did not want to lose the “human element” of treatment, we offer parents up to four in-person coaching sessions. The first two sessions are offered while the adolescent is receiving residential treatment, the time parents described as easiest to attend sessions, in order to capitalize upon parental involvement with the residential treatment program. Second, in response to feedback that parents wanted convenient access to an expert and to other parents post-discharge, parents will receive access to an expert-facilitated online message board. Finally, in order to reinforce usage of PW and the online parent board, parents will receive two text messages weekly containing links to videos of parenting skills, messages of encouragement, and links to the online message board. Such supports are designed to sustain parental engagement, reinforce important parenting skills, and provide easier access to a treatment provider during a time when adolescents are at high risk of negative outcomes, but parents reported it was especially difficult to attend in-person sessions.
Study objectives and specific aims
The overarching goal of this protocol is to evaluate the feasibility, acceptability, and preliminary effectiveness of the adapted PW model (PW+) among parents of adolescents (age 12–17) preparing for discharge from acute residential SUD treatment. The project has two phases. In Phase 1, a pilot open trial tests the PW+ protocol with 10 parent-adolescent dyads. Feedback from residential staff, parents, and adolescents will be used to: (a) finalize a manual for adjunct individual coaching sessions, (b) develop coach training materials, and (c) refine the delivery and content of technology-assisted engagement strategies. During Phase 2, a pilot randomized controlled trial with 60 parent-adolescent dyads will evaluate the effectiveness of the PW+ intervention as an adjunct to residential standard care (SC). Combined, the activities in these two study phases will address three Specific Aims.
Specific aim 1
To examine the feasibility and acceptability (primary protocol outcomes) of the PW+ technology-assisted intervention among parents of adolescents in residential SUD treatment.
Specific aim 2
To examine the preliminary effectiveness of the PW+ technology-assisted protocol on adolescent substance use and associated high-risk behaviors (secondary protocol outcomes) over the first 24 weeks post-discharge.
Specific aim 3
To examine the preliminary effects of the PW+ technology-assisted on parental monitoring and communication (putative mediators of the intervention) over the first 24 weeks post-discharge.
Methods
Timing of key protocol elements
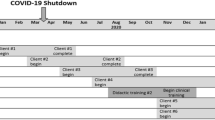
Table 2 depicts the timing of key protocol elements including enrollment, allocation (in the randomized trial), intervention, and assessments. Two issues related to the timing of protocol components bear mention. First, key procedures (i.e., consent, baseline assessment, randomization, intervention) are conducted immediately after the adolescent’s admission to residential treatment. We start the protocol immediately instead of waiting until after discharge, due to qualitative pilot data (see Table 1) indicating that parents viewed the post-discharge period as overwhelming, and that parents had concerns about their ability to schedule face-to-face sessions during this period. Starting immediately after admission also capitalizes upon a critical intervention window while the teen is in residential treatment. Second, the open trial has one follow-up assessment at 6-weeks post-discharge that focuses on feasibility and acceptability, while the pilot randomized trial has a longer follow-up assessment schedule of 6-, 12-, and 24-weeks post-discharge focused on preliminary effectiveness. Prior studies by members of our team [68, 69], have suggested that brief interventions have their strongest effect between baseline and 24 week follow-up, with significantly less change over subsequent assessments. Having three follow-up assessments during the first 24 weeks post-discharge will serve to elucidate the change that is likely to occur immediately following treatment.
Residential center
Evaluation of the PW+ intervention will occur at the only acute residential community SUD treatment program in Rhode Island. The facility contains 16 beds and is located about 20 min outside the state capital in a suburban area. It recently affiliated with the local hospital, but continues to operate as an independent community-based program. Average length of stay is 6–10 days. About five adolescents are admitted per week on average, which equates to approximately 260 admissions per year. Based on past year census data, about 30% of adolescents at the residential treatment center are racial/ethnic minorities, with Hispanic (about 20%) and African-American (about 10%) being the most commonly represented minority groups. There is approximately even representation of male and female adolescents. In the pilot qualitative sample, median household income was $30,000, with an extremely wide range from $18,000 to over $200,000.
Participants
A total of 70 parent-adolescent dyads (10 in Phase 1/open trial and 60 in Phase 2/pilot randomized trial) will be recruited from the acute residential treatment center. To qualify for the study, parents must meet these inclusion criteria: (1) be the parent or legal guardian of an adolescent, aged 12–17 years; (2) had adolescent admitted to residential treatment due to problems related to substance use; (3) will be the primary guardian living with the adolescent immediately post-discharge; (4) willing to receive a parenting intervention; (5) fluent in English or Spanish; and (6) willing to provide written consent and adolescent willing to provide written assent. Adolescents automatically qualify if their parents meet these criteria. The only exclusion criteria are conditions that might preclude the adolescent’s participation in a 2–3 h interview (e.g., mania, psychosis, and cognitive impairment). Based on recent enrollment data, we conservatively expect at least 50% of new admissions to be eligible (with discharge to another facility, discharge to another caregiver, or parent unwilling to receive an intervention as primary reasons for exclusion). To meet our recruitment goal of 70 parent-adolescent dyads, we will need to enroll 25–30% of eligible parents over the first 2 years of the study.
Study enrollment and randomization
In accordance with institutional review board procedures at Brown University and Rhode Island Hospital, parents of all newly admitted adolescents will receive a Consent to Contact (CoC) form as part of the standard intake process at the residential center. Parents that sign a CoC form will then be contacted by research staff in one of two ways. If the adolescent is admitted Monday through Friday during normal business hours (which accounts for about 80% of new intakes), research staff located on site will immediately approach the parents and invite them to initiate the consent process. If the adolescent is admitted after hours or on weekends, research staff will contact the parents using the preferred contact information provided.
Parents will provide written informed consent and adolescents will provide written assent in separate private rooms at the residential center. If an adolescent chooses not to participate, the parent will be given general feedback that the family did not qualify so as to protect the adolescent’s privacy. Parents and adolescents may choose to conduct the informed consent process and all other study procedures in English or Spanish.
Parents will be given the choice whether to return for the baseline assessment or complete it immediately following informed consent. In the Phase 2 trial, randomization will occur within 24 h after the baseline assessment. Parent-adolescent dyads will be randomized to either SC or PW+ using urn randomization balanced on sex, severity of substance use, and preferred language (English vs. Spanish). Randomization will be conducted by a Co-Investigator, not involved with the assessment process, as soon as a parent consents to participate. Condition assignments will be placed in sealed envelopes and given to the independent evaluator. The evaluator will give parents their sealed envelope indicating that their treatment condition immediately after completion of the baseline assessment. If the parent is assigned to PW+, the evaluator will schedule the first in-person coaching session.
Therapist training, fidelity, and competence
Treatment will be delivered by two parent coaches. The coaches are part-time BA-level research staff, one of whom is bilingual in English and Spanish. The decision to use research staff as parent coaches was made in consultation with leaders of the residential facility, who wanted indication that the PW+ intervention was viewed favorably by parents before allocating substantial staff effort to the program. We specifically agreed to hire BA-level research staff with no clinical experience since these credentials are lower than those of program staff. Each coach will deliver both PW+ and SC sessions to prevent confounding of therapist effects. The study PI will train the two coaches. Parent coaches will review the PW computerized program and the manual for in-person sessions. Acting as a standardized patient, a study Co-Investigator with extensive experience treating adolescents with SUDs will role-play the four coaching sessions with each coach. These role plays will be recorded. The study PI will view these role plays, complete measures of therapist adherence and competence, and provide feedback to each counselor. Competency will be rated with six items that comprise the “General Therapeutic Skills” section of the Cognitive Therapy Rating Scale (CTRS) [70, 71]. A score >24 is the criterion to indicate competence. A 12-item adherence checklist for each coaching session has been developed. The coaches will be required to earn a satisfactory consensus CTRS score of >24 on three of four role plays and satisfactory adherence ratings (9 out of 12 elements) to be assigned an actual participant. Once the coaches are assigned participants, the PI will review and rate the first two tapes for adherence and competence. If ratings are satisfactory, the PI and a study Co-Investigator will collectively review 25% of tapes moving forward. The team will also rate 25% of SC sessions to ensure there is not drift between PW+ and SC sessions. The PI will meet weekly with the coaches for supervision focused on how to deliver PW+ with adherence, while flexibly tailoring content to each parent’s unique presenting concerns.
Standard care (SC)
SC consists of the standard treatment elements offered to all residential patients at the partner residential center. Adolescents receive about 25 h of treatment per week. Before an adolescent is discharged (typical length of stay 6–10 days), parents are typically offered two family therapy sessions (which typically use a family systems approach and include case management planning). Adolescents receive four to 5 h of individual and group therapy sessions per day, consisting of psychoeducation and general skills building. Medication management is offered by a psychiatrist as needed. Prior to discharge, parents also receive standard discharge planning, which consists of either a referral to a new outpatient therapy provider or return to a prior outpatient therapy provider. As indicated, adolescents also receive referrals to a psychiatrist or local self-help groups. Post discharge, families are offered up to two check-in sessions to review the adolescent’s progress and troubleshoot any difficulties complying with the treatment plan.
Adapted PW program
In addition to the SC elements, parents in the PW+ condition will receive the following elements: PW online modules, in-person coaching sessions, personalized texting, and an expert-moderated online parent board. All study materials will be translated into Spanish by a bilingual English and Spanish research staff member, and reviewed for accuracy by a Study Co-Investigator. Parents will be able to choose whether they prefer to receive materials in English or Spanish.
PW online modules
PW (Parenting Wisely/Ser Padres Con Sabiduría) is a self-administered, interactive, multimedia online program. PW contains video vignettes of ten common family problems (e.g., adolescent substance abuse, curfews, household chores, monitoring of friends, sibling conflict, improving in school, getting up on time, sharing technology, etc.). For each problem, parents progress through three activities: viewing of a video clip of a family struggling with the problem; selection of one of three possible solutions to the problem; and receipt of feedback about the solution selected. Feedback is presented via a video enactment of the selected solution and an explanation of the solution’s pros and cons. The goals of the feedback are to explain why ineffective solutions lead to problems and discuss how effective parenting solutions can prevent and resolve common family issues. Each vignette emphasizes six core behaviors: (1) problem solving; (2) limit setting; (3) praising; (4) effective communication through “I messages” and active listening; (5) supervision and monitoring, and (6) clear communication of adolescent’s behavioral expectations. Parents receive a parent workbook outlining all 10 vignettes, along with the potential problems and solutions. The workbook also contains a glossary of terms, sample behavior charts, and practice exercises. Parents create a unique login upon enrollment and can complete sessions at their own pace. Depending on the user’s speed and depth of use, the PW program typically takes between 3 and 5 h to complete.
Individual coaching sessions
Individual coaching sessions are designed to individually tailor the PW skills to each parent’s presenting concerns. The in-person coaching sessions correspond with four of the PW vignettes: substance use, limit setting, parental monitoring, and parental communication. The initial session is 60–75 min and consists of three sections: (1) rationale for parenting skills, (2) review of PW substance use module (in session), and (3) practice applying the skill to a current problem. Subsequent sessions follow the same outline and last 45–60 min, with active use of the PW program comprising about half the session. If parents introduce problems/complaints about their adolescent, the coach will first provide validation and then discuss how to apply a pertinent PW skill. Following discharge, the coach will also direct the parent to use the online parent board for additional support.
Text-based messaging
Following discharge, parents will receive text messages twice weekly for 12 weeks. The texts are intended to: (a) reinforce PW skills, (b) motivate continued PW usage, and (c) encourage participation in the online parent message board. In recognition of the ubiquity of text messaging in the general population [44] as well as in health-related research and clinical care [72], the PW developer has developed a set of text messages and videos to be delivered in conjunction with PW. In the open trial (Phase 1), it is possible that we will refine the text-messaging protocol (e.g., content, format, and frequency) based on feedback from parents during the exit interviews (described further below). One of the weekly messages will reinforce material taught in PW (e.g., a reminder statement about a parent strategy such as monitoring or communication) along with a link to a video clip enacting a core PW skill.
The second weekly text message will be encouragement for the parent to either practice PW vignettes or participate in the online parent message board. This protocol intentionally does not use interactive texting; instead, text messages will direct parents to ask questions via the parent board, an approach that we believe will ultimately be more transportable. Nonetheless, this limited application of texting is a potentially important ingredient to extending parents’ engagement in the parenting skills intervention, similar to the use of texting to provide support for smoking cessation [73] and to promote uptake of flu vaccinations [74] and outpatient clinic attendance [75].
Online parent board
Parents will be given access to a secure, expert-moderated website containing basic substance use and parenting skills information, links to sections of PW, as well as an interactive message board. Parents will be able to submit questions anonymously using the same unique login as for the PW program. All submitted questions will be reviewed by the project team to determine suitability for the board. Questions posted on the message board will be answered by the research team within 48 h. At the start of the treatment program, parents will be informed that the purpose of the parent online message board is to ask parenting related questions and not to request crisis support; requests for crisis support will be handled by the PI, a licensed clinical psychologist, and will not be shared on the message board. Answers to questions posted on the message board will direct parents to a specific PW module(s) most relevant to their parenting question. Participation on the message board will be encouraged for 12 weeks post-discharge, with the link to the board continually reinforced through text messages. The online message board will use the same login and password as the PW website, and the online message board will continually provide links to the PW website, to promote consistent use across platforms.
Exit interviews
During the open trial phase, parents will complete exit interviews about their impressions of the PW+ program after the 6-week follow-up. Parent exit interviews contain questions about each aspect of the intervention, including the in-person sessions (e.g., number, content, format), text messages (e.g., content, frequency, format), and online message board (e.g., ease of access, content, format). Parents will also complete the 16-item Consumer Satisfaction Questionnaire (CSQ; [76]), which rates their satisfaction with treatment delivery, their adolescent’s treatment progress, and their ability to manage their adolescent’s problems. Parents rate 11 items along a 7-point scale (α = .91) and answer five open-ended questions about their experience in treatment. If more than one parent expresses the same concern with a protocol element (e.g., the frequency/number of in-person sessions, the frequency/content of texts, an aspect of the message board), then the element will be flagged for possible modification by the research team.
Assessments
Parents and adolescents will complete a baseline assessment in-person shortly after their admission to residential treatment. Adolescents will be assured of confidentiality and a National Institute of Health Certificate of Confidentiality (CoC) will be obtained, as adolescent self-report use has shown reliability when confidentiality is assured [77–80]. The CoC will allow the research team to refuse to disclose names or other identifying characteristics of research participants in response to legal demands such as subpoena of records. Follow-up assessments will be conducted by an independent evaluator who is blind to condition. During the open trial, there will be follow-up assessment at 6 weeks post-discharge, while during the pilot randomized trial there will be three follow-up assessments at 6, 12, and 24 weeks post-discharge. Follow-up assessments will be scheduled in-person at the residential treatment center; if a parent no-shows more than twice for a follow-up assessment, then research staff will attempt to conduct the follow-up sessions at a location of the family’s choosing (i.e., home, school). The baseline assessment will be 1.5–2 h and the follow-up assessments will be about 1.5 h (see Table 3 for overview of measures).
We selected adolescent measures to be as consistent with SC as possible. The residential center typically obtains a urine screen and administers a comprehensive adolescent interview to assess substance use and functioning across multiple life domains. We therefore combine biological markers with the Global Appraisal of Individual Needs—Quick (GAIN-Q3 [81]), a well-validated structured interview that assesses adolescents’ problems across several domains: substance use, school, mental health, physical health, risk behaviors, work, and sources of stress. The GAIN-Q3 substance use scales used in this protocol have demonstrated sound psychometric properties including internal consistency [82], high concurrence with the Timeline Followback Method [83], ability to predict SUD diagnoses made by blind raters (κ = .91) [84], and ability to predict substance-related problems as well or better than biometric markers [82]. The PI is a certified trainer of the GAIN family of instruments with experience analyzing GAIN data [85–88] and will train the independent evaluators.
To explore potential mediators of change, we augment the GAIN-Q3 with two brief measures of parental monitoring [89] and communication [90] (completed by both the parent and adolescent), as well as an in vivo parent-adolescent interaction task [91, 92]. The self-report measures have demonstrated good internal consistency and have correlated well with adolescent involvement in risky behavior, adolescent maladjustment, and family discord [89, 90], while the in vivo task has shown high inter-rater reliability [69]. These parenting measures will only be completed by those parents with have primary custody of their adolescent. If a parent loses custody post-discharge, parenting measures will not be administered (treating parent data as missing).
Retention procedures
Multiple steps will be taken to prevent attrition from the study follow-up assessments. First, during the baseline assessment, multiple sources of contact information will be recorded for parents and adolescents. In addition to extensive personal contact information, parents will provide detailed contact information of two friends or family members (“locators”) who can be contacted if research staff is unable to reach them. Follow-up reminders will be made via phone, text, and/or mail, depending on the parents’ preferences. The research team will meet weekly to review no-shows and outreach attempts, and discuss plans to connect with missing participants. Parents and adolescents will each receive an escalating schedule of compensation in the form of gift cards for completing the baseline ($40) and three follow-up assessments ($50, $50, $60, respectively).
Data analysis plan
All 60 parents will be included in statistical analyses consistent with an intent-to-treat (ITT) model. Prior to the main analyses, descriptive statistics will be run on key variables to examine distributional properties, identify outliers, and transform variables as needed. The two treatment conditions will be compared on baseline demographic and clinical variables using basic two-group independent sample t-tests. Using a p < .05 criterion, significant pre-existing baseline differences between conditions on any variables will be controlled in subsequent analyses.
GAIN-Q3 data will be entered into the GAIN’s proprietary software, which offers instant error checks and validation reports to prevent missing data. Other forms will be entered directly into study laptops using REDCap (Research Electronic Data Capture), a secure web-based application, to reduce missing data and entry errors. Attrition analyses will compare follow-up completers and non-completers on baseline clinical and demographic variables to determine if they differ systematically. If no systematic differences are found between completers and non-completers, then missing data will be estimated using multiple imputation methods with five datasets, an approach that has been shown to generate unbiased estimates when data are missing at random or missing completely at random [93].
Primary outcomes: feasibility and acceptability
In the open trial and randomized controlled pilot trial, feasibility will be examined via enrollment rates (>80%) and indicators of parental engagement, with the following preliminary targets: attendance of >1 coaching sessions pre-discharge and >1 sessions post-discharge for >75% of parents, and online usage patterns of 2+ PW logins, 2+ parent board logins, and 1+ h logged in for >75% of parents. Criteria for acceptability include withdrawal rates (<20%), satisfaction ratings (>80% of items on the CSQ rated “agree” or “strongly agree”) and positive feedback from exit interviews with parents and therapists. Criteria will be finalized based on parent and staff feedback in Phase 1.
Secondary outcomes: adolescent variables
Secondary outcomes include adolescent substance use and associated high risk behaviors (i.e., sexual risk-behavior, truancy, and criminal involvement). Analyses will compare trajectories of use over the post-discharge period, controlling for baseline status as a covariate. For each dependent variable, separate repeated measures Analysis of Covariance will test the influence of condition, controlling for the following covariates: baseline status on the dependent variable, baseline differences between groups, and any mental health or substance use treatment received over the follow-up period. The effect of PW dosage on each dependent variable will be calculated and partial eta squared (η2) will be used to estimate the proportion of variance caused by PW. The primary analytical goal will be to provide measures of association and 95% confidence intervals to reveal the effect size of PW on each dependent variable.
Putative mediators: parental communication and monitoring
The study will be underpowered to test mediation, but will examine the effects of PW on putative mediators. A repeated measures Analysis of Covariance will whether assignment to the PW+ condition has a significant effect on either of the putative mediators, controlling for any treatment received. In addition, we will calculate change in the putative mediators over each time interval as well as change in the dependent variables over each time interval. Correlations between change in the putative mediators and change in the dependent variables will be examined; significant positive correlations greater than r = .20 will be flagged as worthy of further analysis in a future trial. The goal of these analyses is to find promising trends to pursue in a larger fully powered trial.
For both the secondary outcome analyses and the mediator analyses, the investigators will also attempt to fit latent growth models to the data. Latent growth models represent a flexible approach to analyzing change that enable a comparison of conditions at each time point while accounting for the correlation of observations over time [94]. Although convergence is challenged in a small sample, latent growth models have been fit to samples as small as n = 22 [95, 96]. The study PI has conducted multiple analyses using latent growth models [32, 97, 98] and will lead the longitudinal analyses.
Sample size and power
The study will recruit 60 participants for the randomized trial. Estimating that 15–20% may be lost to follow-up, there will likely be 50 participants with complete parent-adolescent data. We will use these participants to make judgments regarding feasibility and acceptability. Effect size estimates in prior PW studies have ranged from small to very large; the only study conducted among adolescent substance users found small to medium effects, but unlike this application, that study did not offer in-person support or an online parent board (supports that may contribute to larger effect sizes). Furthermore, even small effects, if obtained by delivering content electronically via a highly scalable platform that can reach large numbers of parents, can have significant public health implications. Despite issues with effect size stability in small samples [99], a small to medium effect paired with high levels of feasibility and acceptability would therefore be an indication that the adapted PW intervention should be tested in a larger trial. Based on the detected effect size, post hoc power analyses will be conducted to determine the number of parents required for a fully powered trial. For instance, for power of .8, a small effect size (d = .3) would require a sample of 175 per group, while a medium effect size (d = .5) would require a much smaller sample of 64 per group.
Discussion
This protocol evaluates whether a technology-assisted parenting intervention can improve the treatment outcomes of adolescents discharged from acute residential treatment. The approach builds upon qualitative data collection with parents of adolescents in residential treatment and combines both in-person and technology-delivered intervention elements to improve parental engagement at a time when parents have especially poor attendance.
Findings from this protocol will be subject to important limitations. First, the residential program is based in Rhode Island about 15 min from a major urban center. Results of this protocol may not generalize to programs in other states or more rural regions. Second, the PW+ condition and the SC condition do not offer an equivalent dose of contact time. It is therefore possible any favorable results associated with PW+ may be accounted for by a higher “overall” dose of treatment (e.g., coaching sessions, text messages, time spent on the parent message board, time spent completing the computer program). Because this is a treatment development protocol, we focus our resources on developing and pilot testing the experimental condition. If results are promising, we will attempt to control for contact time in a fully powered trial.
By adapting and evaluating an intervention for parents of adolescents in residential treatment, this protocol has the potential to advance treatment by: (1) addressing a high-needs population; (2) targeting parenting skills (putative mediators) that have been shown to influence adolescent substance use and related risk behaviors; (3) working with parents at a critical treatment juncture (i.e., immediately prior to and following the adolescent’s discharge from residential treatment); and (4) developing a model with potential for widespread dissemination in community residential programs. If results of this protocol are promising, future research will attempt to evaluate the PW+ protocol in a fully powered protocol. To accelerate the translation of research to practice, the fully powered trial will use a type 1 hybrid effectiveness-implementation design that simultaneously gathers data on the effectiveness of the model under real-world conditions and collects data on barriers and facilitators to effective implementation [100].
Abbreviations
- CSQ:
-
consumer satisfaction questionnaire
- CTRS:
-
Cognitive Therapy Rating Scale
- GAIN-Q3:
-
global appraisal of individual needs—quick version
- PI:
-
principal investigator
- PW:
-
Parenting Wisely
- SC:
-
standard care
- SUD:
-
substance use disorder
References
Center for Behavioral Health Statistics and Quality. 2013 State profile—United States: National Survey of Substance Abuse Treatment Services (N-SSATS); 2013.
Dennis ML, Dawud-Noursi S, Muck RD, McDermeit M. The need for developing and evaluating adolescent treatment models. In: Stevens SJ, Morral AR, editors. Adolescent substance abuse treatment in the United States: exemplary models from a national evaluation study. Binghampton: Haworth Press, Inc; 2003. p. 3–34.
Dennis ML, Scott CK, Godley MD, Funk R. Predicting outcomes in adult and adolescent treatment with case mix vs. level of care: finding from the drug outcome monitoring study. Drug Alcohol Depend. 2000;60(suppl 1):s51.
Catalano R, Hawkins J, Wells E, Miller J, Brewer D. Evaluation of the effectiveness of adolescent drug abuse treatment, assessment of risks for relapse, and promising approaches for relapse prevention. Int J Addict. 1990–1991;25(9A–10A):1085–140.
Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL. The effect of assertive continuing care on continuing care linkage, adherence and abstinence following residential treatment for adolescents with substance use disorders. Addiction. 2007;102(1):81–93.
Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addict Behav. 1989;14:291–300.
Alford GS, Koehler RA, Leonard J. Alcoholics Anonymous-Narcotics Anonymous model inpatient treatment of chemically dependent adolescents: a 2-year outcome study. J Stud Alcohol. 1991;52(2):118–26.
Godley MD, Godley SH, Dennis ML, Funk R, Passetti LL. Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. J Subst Abuse Treat. 2002;23(1):21–32.
McKay JR. Continuing care research: what we have learned and where we are going. J Subst Abuse Treat. 2009;36(2):131–45 (PMC2670779).
Chilcoat HD, Anthony JC. Impact of parent monitoring on initiation of drug use through late childhood. J Am Acad Child Adolesc Psychiatry. 1996;35(1):91–100.
Vakalahi HF. Adolescent substance use and family-based risk and protective factors: a literature review. J Drug Educ. 2001;31(1):29–46.
Tobler AL, Komro KA. Trajectories of parental monitoring and communication and effects on drug use among urban young adolescent. J Adolesc Health. 2010;46(6):560–8 (PMC2872631).
Kafka RR, London P. Communication in relationships and adolescent substance use: the influence of parents and friends. Adolescence. 1991;6(103):587–98.
Baumrind D, Moselle KA. A developmental perspective on adolescent drug abuse. Adv Alcohol Subst Abuse. 1985;4(3–4):41–66.
Brown BB, Mounts N, Lamborn SD, Steinberg L. Parenting practices and peer group affiliation in adolescence. Child Dev. 1993;64(2):467–82.
Dishion TJ, Loeber R. Adolescent marijuana and alcohol use: the role of parents and peers revisited. Am J Drug Alcohol Abuse. 1985;11(1–2):11–25.
Fletcher AC, Darling N, Steinberg L. Parental monitoring and peer influences on adolescent substance use. In: McCord J, editor. Coercion and punishment in long-term perspectives. New York: Cambridge Press; 1998. p. 259–71.
Latendresse SJ, Rose RJ, Viken RJ, Pulkkinen L, Kaprio J, Dick DM. Parenting mechanisms in links between parents’ and adolescents’ alcohol use behaviors. Alcohol Clin Exp Res. 2008;32(2):322–30.
Chassin L, Pillow DR, Curran PJ, Molina BS, Barrera M Jr. Relation of parental alcoholism to early adolescent substance use: a test of three mediating mechanisms. J Abnorm Psychol. 1993;102(1):3–19.
Chassin L, Curran PJ, Hussong AM, Colder CR. The relation of parent alcoholism to adolescent substance use: a longitudinal follow-up study. J Abnorm Psychol. 1996;105(1):70–80.
Chassin L, Presson CC, Rose JS, Sherman SJ. Maternal socialization of adolescent smoking: intergenerational transmission of smoking-related beliefs. Psychol Addict Behav. 1998;12(3):206.
Jackson C, Henriksen L. Do as I say: parent smoking, antismoking socialization, and smoking onset among children. Addict Behav. 1997;22(1):107–14.
Jaccard J, Turrisi R. Parent-based intervention strategies to reduce adolescent alcohol-impaired driving. J Stud Alcohol Drugs. 1999;13:84–93.
Ary DV, Tildesley E, Hops H, Andrews J. The influence of parent, sibling, and peer modeling and attitudes on adolescent use of alcohol. Subst Use Misuse. 1993;28(9):853–80.
Zhang L, Welte JW, Wieczorek WF. Peer and parental influences on male adolescent drinking. Subst Use Misuse. 1997;32(14):2121–36.
Kosterman R, Hawkins JD, Guo J, Catalano RF, Abbott RD. The dynamics of alcohol and marijuana initiation: patterns and predictors of first use in adolescence. Am J Public Health. 2000;90(3):360–6.
Ellickson PL, Hays RD. On becoming involved with drugs: modeling adolescent drug use over time. Health Psychol. 1992;11(6):377–85.
Hogue A, Henderson CE, Ozechowski TJ, Robbins MS. Evidence base on outpatient behavioral treatments for adolescent substance use: updates and recommendations 2007–2013. J Clin Child Adolesc Psychol. 2014;43(5):695–720.
Stanton MD, Shadish WR. Outcome, attrition, and family–couples treatment for drug abuse: a meta-analysis and review of the controlled, comparative studies. Psychol Bull. 1997;122(2):170–91.
Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. J Clin Child Adolesc Psychol. 2008;37(1):238–61.
Tanner-Smith EE, Wilson SJ, Lipsey MW. The comparative effectiveness of outpatient treatment for adolescent substance abuse: a meta-analysis. J Subst Abuse Treat. 2013;44(2):145–58.
Becker SJ, Curry JF. Outpatient interventions for adolescent substance abuse: a quality of evidence review. J Consult Clin Psychol. 2008;76(4):531–43.
Kumpfer KL, Alvarado R, Whiteside HO. Family-based interventions for substance use and misuse prevention. Subst Use Misuse. 2003;38(11–13):1759–87.
Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: results of a randomized clinical trial. Am J Drug Alcohol Abuse. 2001;27(4):651–88.
Santisteban DA, Szapocznik J, Perez-Vidal A, Kurtines WM, Murray EJ, LaPerriere A. Efficacy of intervention for engaging youth and families into treatment and some variables that may contribute to differential effectiveness. J Fam Psychol. 1996;10(1):35–44.
Ozechowski TJ, Liddle HA. Family-based therapy for adolescent drug abuse: knowns and unknowns. Clin Child Fam Psychol Rev. 2000;3(4):269–98.
Godley SH, Godley MD, Dennis ML. The assertive aftercare protocol for adolescent substance abusers. In: Wagner EF, Waldron HB, editors. Innovations in adolescent substance abuse interventions. New York: Pergamon; 2001. p. 313–31.
Substance Abuse and Mental Health Services Administration, Treatment Episode Data Set (TEDS): 2011. In: Discharges from substance abuse treatment services. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
Leonard K. Teens with addiction have few recovery programs. In: US news & world report. http://health.usnews.com/health-news/best-childrens-hospitals/articles/2014/06/10/teens-with-addiction-have-few-recovery-programs; 2014.
Portnoy DB, Scott-Sheldon LA, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988–2007. Prev Med. 2008;47(1):3–16.
Copeland J, Martin G. Web-based interventions for substance use disorders: a qualitative review. J Subst Abuse Treat. 2004;26(2):109–16.
Miller WR, Sorensen JL, Selzer JA, Brigham GS. Disseminating evidence-based practices in substance abuse treatment: a review with suggestions. J Subst Abuse Treat. 2006;31(1):25–39.
McHugh RK, Barlow DH. The dissemination and implementation of evidence-based psychological treatments: a review of current efforts. Am Psychol. 2010;65(2):73–84.
Internet User Demographics. In: Pew research center internet project survey. Pew Research Center; 2014.
Linke S, Murray E, Butler C, Wallace P. Internet-based interactive health intervention for the promotion of sensible drinking: patterns of use and potential impact on members of the general public. J Med Internet Res. 2007;9:10.
Campbell AN, Nunes EV, Miele G, Matthews M, Polsky D, Ghitza UE, Turrigiano E, Bailey GL, VanVeldhuisen P, Chapdelaine R, et al. Design and methodological considerations of an effectiveness trial of a computer-assisted intervention: an example from the NIDA Clinical Trials Network. Contemp Clin Trials. 2012;33:386–95.
Rooke S, Thorsteinsson E, Karpin A, Copeland J, Allsop D. Computer-delivered interventions for alcohol and tobacco use: a meta-analysis. Addiction. 2010;105(8):1381–90.
Bickel WK, Marsch LA, Buchhalter AR, Badger GJ. Computerized behavior therapy for opioid-dependent outpatients: a randomized controlled trial. Exp Clin Psychopharmacol. 2008;16(2):132–43.
Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, Gordon MA, Portnoy GA, Rounsaville BJ. Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. Am J Psychiatry. 2008;165(7):881–8.
Pallonen UE, Velicer WF, Prochaska JO, Rossi JS, Bellis JM, Tsoh JY, Migneault JP, Smith NF, Prokhorov AV. Computer-based smoking cessation interventions in adolescents: description, feasibility, and six-month follow-up findings. Subst Use Misuse. 1998;33(4):935–65.
Paperny DM, Aono JY, Lehman RM, Hammar SL, Risser J. Computer-assisted detection and intervention in adolescent high-risk health behaviors. J Pediatr. 1990;116(3):456–62.
Marsch LA, Bickel WK, Grabinski MJ. Application of interactive, computer technology to adolescent substance abuse prevention and treatment. Adolesc Med State Art Rev. 2007;18(2):342–56, xii.
Schinke S, Schwinn T. Gender-specific computer-based intervention for preventing drug abuse among girls. Am J Drug Alcohol Abuse. 2005;31(4):609–16.
Gordon DA. Parenting wisely program workbook. Athens: Family Works; 2005.
Cefai J, Smith D, Pushak RE. Parenting wisely: parent training via CD-ROM with an Australian sample. Child Fam Behav Ther. 2010;32(1):17–33.
Gordon D, Kacir C, Pushak R. Effectiveness of an interactive parent training program for changing adolescent behavior for court-referred parents. Manuscript submitted to the SAMHSA National Registry for Effective Programs and Practices 2008 1997, 9(01):2007.
Segal D, Chen PY, Gordon DA, Kacir CD, Gylys J. Development and evaluation of a parenting intervention program: integration of scientific and practical approaches. Int J Hum Comput Int. 2003;15(3):453–67.
Kacir C, Gordon DA. Parenting adolescents wisely: the effectiveness of an interactive videodisk parent training program in appalachia. Child Fam Behav Ther. 1999;21(4):1–22.
Eyberg S, Boggs SR, Reynolds LA. Eyberg child behavior inventory: University of Oregon Health Sciences Center; 1980.
Cotter K, Bacallao M, Smokowski P, Robertson C. Parenting interventions implementation science: how delivery format impacts the parenting wisely program. Drug Alcohol Depend. 2009;100(1–2):178–81.
Percentage of mobile apps that have been used only once during the first six months of ownership from 2011 to 2015. http://www.statista.com/statistics/271628/percentage-of-apps-used-once-in-the-us/.
Aguilera A, Muench F. There’s an app for that: information technology applications for cognitive behavioral practitioners. Behav Ther. 2012;35(4):65–7.
Mohr DC, Cuijpers P, Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J Med Int Res. 2011;13(1):136–46.
Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Rounsaville BJ. Enduring effects of a computer-assisted training program for cognitive behavioral therapy: a six-month follow-up of CBT4CBT. Drug Alcohol Depend. 2009;100(1–2):178–81.
Micco N, Gold B, Buzzell P, Leonard H, Pintauro S, Harvey-Berino J. Minimal in-person support as an adjunct to internet obesity treatment. Ann Behav Med. 2007;33(1):49–56.
Becker SJ, Midoun M, Zeithaml V, Clark M, Spirito A. Dimensions of treatment quality most valued by adolescent substance users and their caregivers. Prof Psychol Res Pract. 2016;47(2):120–9.
Becker SJ, Spirito A, Vanmali R. Perceptions of “evidence-based practice” among the consumers of adolescent substance use treatment. Health Educ J. 2016;75(3):358–69.
Spirito A, Monti PM, Barnett NP, Colby SM, Sindelar H, Rohsenow DJ, Lewander W, Myers M. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. J Pediatr. 2004;145(3):396–402.
Spirito A, Sindelar-Manning H, Colby SM, Barnett NP, Lewander W, Rohsenow DJ, Monti PM. Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department: results of a randomized clinical trial. Arch Pediatr Adolesc Med. 2011;165(3):269–74.
Dobson KS, Shaw BF, Vallis TM. Reliability of a measure of the quality of cognitive therapy. Br J Clin Psychol. 1985;24(4):295–300.
Young J, Beck A. Cognitive therapy scale rating manual. Philadelphia: University of Pennsylvania; 1980.
Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev. 2010;32(1):56–69.
Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, Rodgers A, Cairns J, Kenward MG, Roberts I. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet. 2011;378(9785):49–55.
Stockwell MS, Westhoff C, Kharbanda EO, Vargas CY, Camargo S, Vawdrey DK, Castaño PM. Influenza vaccine text message reminders for urban, low-income pregnant women: a randomized controlled trial. Am J Public Health. 2014;104(S1):e7–12.
Guy R, Hocking J, Wand H, Stott S, Ali H, Kaldor J. How effective are short message service reminders at increasing clinic attendance? A meta-analysis and systematic review. Health Serv Res. 2012;47(2):614–32.
McMahon RJ, Forehand RL. Helping the noncompliant child: Family-based treatment for oppositional behavior. 2nd ed. New York: Guilford Press; 2003.
Haley NJ, Axelrad CM, Tilton KA. Validation of self-reported smoking behavior: biochemical analyses of cotinine and thiocyanate. Am J Public Health. 1983;73(10):1204–7.
Luepker RV, Pechacek TF, Murray DM, Johnson CA, Hund F, Jacobs DR. Saliva thiocyanate: a chemical indicator of cigarette smoking in adolescents. Am J Public Health. 1981;71(12):1320–4.
Needle R, McCubbin H, Lorence J, Hochhauser M. Reliability and validity of adolescent self-reported drug use in a family-based study: a methodological report. Subst Use Misuse. 1983;18(7):901–12.
Pechacek TF, Murray DM, Luepker RV, Mittelmark MB, Johnson CA, Shutz JM. Measurement of adolescent smoking behavior: rationale and methods. J Behav Med. 1984;7(1):123–40.
Dennis ML, White M, Titus JC, Unsicker MS. Global appraisal of individual needs: administration guide for the GAIN and related measures (version 5). Bloomington: Chestnut Health Systems; 2008.
Lennox R, Dennis ML, Scott CK, Funk R. Combining psychometric and biometric measures of substance use. Drug Alcohol Depend. 2006;83(2):95–103.
Dennis ML, Funk R, Godley SH, Godley MD, Waldron H. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction. 2004;99(s2):120–8.
Shane PA, Jasiukaitis P, Green RS. Treatment outcomes among adolescents with substance abuse problems: the relationship between comorbidities and post-treatment substance involvement. Eval Program Plann. 2003;26(4):393–402.
Becker SJ, Curry JF, Yang C. Factors that influence trajectories of change in frequency of substance use and quality of life among adolescents receiving a brief intervention. J Subst Abuse Treat. 2011;41(3):294–304.
Becker SJ, Curry JF, Yang C. Longitudinal association between frequency of substance use and quality of life among adolescents receiving a brief outpatient intervention. Psychol Addict Behav. 2009;23(3):482–90.
Becker SJ, Stein GL, Curry JF, Hersh J. Ethnic differences among substance-abusing adolescents in a treatment dissemination project. J Subst Abuse Treat. 2012;42(3):328–36.
Hersh J, Curry JF, Becker SJ. The influence of comorbid depression and conduct disorder on MET/CBT treatment outcome for adolescent substance use disorders. Int J Cogn Ther. 2013;6(4):325–41.
Kerr M, Stattin H. What parents know, how they know it, and several forms of adolescent adjustment: further support for a reinterpretation of monitoring. Dev Psychol. 2000;36(3):366–80.
Barnes HL, Olson DH. Parent-adolescent communication and the circumplex model. Child Dev. 1985;438–447(56):438–47.
Forgatch MS. Patterns and outcomes in family problem solving: the disrupting effect of negative emotion. J Marriage Fam. 1989;51(1):115–24.
Robin AL, Foster SL. Negotiating parent-adolescent conflict: a behavioral-family systems approach. New York: Guilford Press; 1989.
Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393.
McArdle JJ. Latent variable modeling of differences and changes with longitudinal data. Annu Rev Psychol. 2009;60:577–605.
Huttenlocher J, Haight W, Bryk A, Seltzer M, Lyons T. Early vocabulary growth: relation to language input and gender. Dev Psych. 1991;27:236–48.
Curran PJ, Obeidat K, Losardo D. Twelve frequently asked questions about growth curve modeling. J Cogn Dev. 2010;11(2):121–36.
Becker SJ, Curry JF, Yang C. Longitudinal association between frequency of substance use and quality of life among adolescents receiving a brief outpatient intervention. Psychol Addict Behav. 2009;23(3):482–90.
Becker SJ, Curry JF, Yang C. Factors that influence trajectories of change in frequency of substance use and quality of life among adolescents receiving a brief intervention. J Subst Abuse Treat. 2011;41(3):294–304.
Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiat. 2006;63(5):484–9.
Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217.
Authors’ contributions
SJB is the Principal Investigator for the study, led the conceptualization of the study and the drafting of the original grant proposal, and developed a first draft of the manuscript. LH, AT, and SC are Co-Investigators of the study and contributed to study conceptualization. LH, AT, and SC also contributed to writing of the original grant proposal and successive drafts of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval
This study protocol has been approved by the Brown University Institutional Review Board (Protocol #1602001412) and the Rhode Island Hospital Institutional Review Board (Protocol #900224). Seven participants have been enrolled in the open trial as of publication of this protocol.
Funding
The current protocol was funded by a grant from NIDA (R34DA039289) awarded to the first author. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIDA or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Becker, S.J., Hernandez, L., Spirito, A. et al. Technology-assisted intervention for parents of adolescents in residential substance use treatment: protocol of an open trial and pilot randomized trial. Addict Sci Clin Pract 12, 1 (2017). https://doi.org/10.1186/s13722-016-0067-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13722-016-0067-4