Abstract
Background
Dyslipidemia is a major risk factor for cardiovascular diseases, but its prevalence and determinants among sedentary occupational population are poorly understood. This study aimed to investigate the prevalence and associated factors for dyslipidemia among a sedentary occupational population in Shanghai, China.
Methods
We collected data from 35,950 sedentary occupational workers on their demographics, social, medical, and family history, lifestyle, anthropometry, and biochemistry. We used the 2016 Chinese guideline for the management of dyslipidemia in adults to define dyslipidemia and its subtypes. We performed multivariate logistic regression to examine the factors associated with dyslipidemia.
Results
The prevalence of dyslipidemia was 29.10%, with 15.86% for high triglycerides (TG), 6.43% for high total cholesterol (TC), 5.37% for high low-density lipoprotein cholesterol (LDL-C), and 14.68% for low high-density lipoprotein cholesterol (HDL-C). Men had a significantly higher prevalence of dyslipidemia than women (39.64% vs. 12.43%, P < 0.01). Factors associated with dyslipidemia included older age, being married, longer sedentary time while resting, frequent intake of animal viscera, current smoking, hypertension, diabetes, and obesity. Current drinking was associated with a 1.24 times higher prevalence of high TG (P < 0.01). Current smokers were less likely to have low HDL-C than non-smokers.
Conclusions
Our present study, in a population of 35,950 sedentary occupational workers from Shanghai, demonstrated a prevalence of dyslipidemia, but lower than in other previous studies without the limitation of occupational characteristics. Prevention and control measures for dyslipidemia should take into account the characteristics and related factors for this population group.
Similar content being viewed by others
Text box 1. Contributions to the literature |
|---|
• There is limited evidence on the prevalence of dyslipidemia and associated factors among sedentary occupational population. |
• Current smoking, hypertension, diabetes, and obesity are associated with both high TG and low HDL-C. Animal viscera and adequate vegetable intake are associated with high TC and high LDL-C. |
• Effective strategies targeting associated factors among sedentary occupational population are needed. |
Background
Dyslipidemia is a disorder of lipid metabolism that results in abnormal blood levels of lipids, such as total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C) [1]. Dyslipidemia is a major risk factor for cardiovascular disease (CVD), the leading cause of death and disability worldwide accounting for 32% in 2019, by causing atherosclerosis, inflammation, and thrombosis [2,3,4]. Dyslipidemia is becoming more prevalent globally, especially in developing countries and among the elderly [5]. Based on national health survey data, the prevalence of dyslipidemia was 53% in America and continued to grow in Japan, especially in the elderly [5, 6]. An analysis of 134,074 Canadian adults showed that 35.8% had at least one abnormal lipid component [7]. On the basis of cardiovascular health measures of the household population in 2017, Canadian adults (aged 20–79 years) had a mean TC level of 3.7 mmol/L [8]. The national survey in 2012 showed that the mean TC level of Chinese adults was 4.5 mmol/L, and the prevalence of dyslipidemia in adults was 40.4% [9]. In 2021, the prevalence of dyslipidemia among the elderly in China was 47.0% [10]. Without timely and effective intervention, the burden of dyslipidemia and its complications will continue to grow. However, many Chinese adults have low awareness and control of dyslipidemia, which poses a great challenge for CVD prevention in China [5, 11]. Therefore, it is important to identify the potential factors influencing dyslipidemia and to implement targeted management strategies from a public health perspective.
Many studies have found that sedentary behavior is a risk factor for chronic diseases, such as obesity and metabolic syndrome, and in particular increases the risk of dyslipidemia [12,13,14]. Adults usually spend approximately 1/2 of their weekday awake time working, and the pattern of sedentary behavior varies by occupation [15]. In urban areas, occupational population with sedentary work patterns mainly come from three groups: government-related units, social service agencies (including educational institutions, public health institutions, social welfare institutions, etc.) and enterprises. These groups have a common feature: high mental work and less physical activity. However, they may face different challenges and opportunities for dyslipidemia prevention and control than other occupational groups. For example, they may have more access to health education and screening services, but also more exposure to stress and sedentary working pattern. It is difficult to change the pattern or activity in the workplace, so understanding their burden of dyslipidemia and related factors from a public health management perspective is an effective path to prevent and manage dyslipidemia among sedentary occupational population. Previous epidemiological studies have mainly examined the regional and gender differences of dyslipidemia, as well as its prevalence in the elderly population [16,17,18,19]. There is a lack of research to determine the burden of dyslipidemia among sedentary occupational population in the last few years, and related factors of dyslipidemia in sedentary occupational population are rather limited and outdated. Therefore, this study aims to investigate the prevalence and types of dyslipidemia among sedentary occupational population in Shanghai using a cross-sectional survey design. The study also aims to identify the potential factors that influence dyslipidemia among this occupational group using multivariate logistic regression analysis. The findings of this study may help to provide evidence-based recommendations for preventing and controlling dyslipidemia among sedentary occupational population in China.
Methods
Study population
Study participants were recruited from 226,296 people who underwent a health checkup in Huadong Sanatorium from January 2019 to December 2021. This hospital is a medical institution in Shanghai taking health checkups as its main business and serving for the occupational population, from enterprises, social service agencies, and some government-related units. The agency set up a routine health questionnaire in 2019–2021 as part of the agency’s “book a checkup – fill out a questionnaire – conduct a checkup” process. This practice aims to collect information on the demographic and social characteristics, medical history and family history, and lifestyle factors, so that doctors can provide more precise diagnoses and follow-up health management based on the results of checkup. People booked online fill in the online questionnaire mainly. People booked offline or booked online without completing the questionnaire will be instructed to fill out the questionnaire by nurses before or doctors during the health checkup. All people were signed with electronic informed consent before filling in.
Study subjects were selected using a two-stage cluster sampling. In the first phase, based on the nature of institution, the physical examination groups were divided into enterprise workers, social service agencies workers, and government-related units workers. A total of 5,538 institutions were involved. In the second phase, we randomly sampled 1,108 institutions at 20% from institutions of different nature. A total of 52,924 people were involved. After excluding those who were pregnant, lactating, or had severe mental or physical illnesses, and whose questionnaire filling time was more than 6 months apart from the health checkup time, 42,259 people were included in this sample. Excluding people whose information was incomplete or inconsistent, the final sample size was 35,050 participants. The study was approved by the Ethics and Research Committee of Huadong Sanatorium Health Examination Center (approval number: ECHS2023-07).
Data collection
We conducted a cross-sectional survey to examine the prevalence and related factors of dyslipidemia among sedentary occupational population. The questionnaire was designed to gather information on demographic and social characteristics (including age, sex, attribute of work organization, marital status, educational level), medical history and family history (including hypertension, diabetes, coronary heart disease (CHD)), and lifestyle factors (including regular diet, nighttime diet, vegetable intake, meat intake, fat intake, animal viscera intake, sugary beverages intake, sedentariness time at rest, smoking status, drinking status, physical activity, average sleep times).
For demographic and social characteristics, the attributes of work organization were divided into social service agencies, enterprises, and agency units. We classified the educational attainment as primary school or below, junior school, middle school, bachelor’s degree, master degree or above, and the marital status as married, divorced or widowed, and single.
For health behaviors, nighttime diet was classified into never, occasional (< 1 time per week), and frequent (≥ 1 time per week) [20, 21]. Based on 2022 Dietary Guidelines for Chinese Residents, vegetable intake was categorized as poor (< 300 gram per day), adequate (≥ 300 gram per day) and meat intake was categorized as poor (< 120 gram per day), adequate (120–250 gram per day), excessive (> 250 gram per day) [22]. Fat intake and animal viscera intake were classified into one of the following categories: never, occasional (1–2 times per week), frequent (≥ 3 times per week). Sugary beverage intake was divided into never or occasional (1–2 times per week), frequent (3–5 times per week), and every day (> 5 times per week) [23]. Sedentariness was defined as continuous sitting for more than 2 h based on the Canadian Sedentary Behavior Guidelines [24]. Former drinking and former smoking were defined as participants who didn’t drink or smoke during the past 12 months [25]. Physical activity was classified according to the number and time of aerobic exercise per week as insufficient (< 3 times per week with sessions shorter than 30 min), adequate (> 3 times per week with sessions longer than 30 min), general (< 3 times per week with sessions longer than 30 min, or > 3 times per week with sessions shorter than 30 min) [26]. This part of the data was obtained by participants’ recall.
Physical examinations
Physical examinations were administered in the morning after overnight fasting by professional nurses who received standardized training. Two consecutive blood pressure measurements were taken at a 45-min interval using a mercury sphygmomanometer with an appropriate cuff size. The mean blood pressure value of the two readings was used [27, 28]. Serum TC, TG, LDL-C, HDL-C, and fasting blood glucose (FBG) were measured by an automatic analyzer with a fasting blood sample using enzymatic methods. The coefficients of variation for all biochemical assays were less than 5%. Weight and height were measured with the participants wearing light weight clothes and no shoes. Body mass index (BMI) was calculated by dividing body weight in kilograms by height in meters squared. The waist circumference (WC) was horizontally measured at the level of their navel using a nonstretchable tape.
Definitions
According to the 2016 Chinese Guidelines for Prevention and Treatment of Dyslipidemia in Adults [29], dyslipidemia was defined as the presence of any of these four indicators: TC ≥ 6.22 mmol/L, TG ≥ 2.26 mmol/L, LDL-C ≥ 4.14 mmol/L, HDL-C < 1.04 mmol/L. Hypertension was considered with systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg or having been diagnosed by doctors according to the 2018 Chinese Guidelines for Prevention and Treatment of Hypertension [30]. Diabetes was considered with FPG ≥ 7.0 mmol/L or having been diagnosed by doctors according to the Chinese Guidelines for Prevention and Control of type 2 diabetes [31]. BMI was calculated as weight in kilograms divided by height in meters squared. Participants with BMI ≥ 28.0 kg/m2 were diagnosed with obesity according to the Guidelines for Prevention and Control of Overweight and Obesity in Chinese Adults [32,33,34].
Statistical analysis
We used descriptive and inferential statistics to analyze the data. Descriptive statistics were used to summarize the characteristics of the study population and compare the differences between groups. Continuous variables were expressed as mean ± standard deviation (SD) and categorical variables as frequencies and percentages. The unpaired Student’s t-test or Wilcoxon rank sum test, and Pearson’s chi-square test were used to compare differences between groups. Inferential statistics were used to identify the risk factors for dyslipidemia and its subtypes using multiple logistic regression models. We used a stepwise selection procedure with an entry criterion of p < 0.05 and a removal criterion of p > 0.10 to select the variables for the final models. The association between dyslipidemia and risk factors was assessed by adjusted odds ratios (ORs) and 95% confidence intervals (CIs). All statistical analyses were carried out using STATA version 13.0 (Stata Corp LP., College Station, TX, USA). A two-sided p-value of less than 0.05 was considered statistically significant.
Results
Demographic characteristics
A total of 35,950 participants were included in this study, including 22,017 males (61.24%) and 13,933 females (38.76%). The mean age of the participants was 45.13 (SD = 10.31) years, ranging from 20 to 89 years. Participants from social service agencies, enterprises, and agency units accounted for 23.43%, 38.64%, and 37.93%, respectively. Of the 35,950 participants in this study, 34,439 (93.02%) had a bachelor’s degree or above, 20.59% smoked, 45.87% drank alcohol, 44.04% had insufficient physical activity, 72.23% had sedentary behavior, and 13.30% had obesity. The mean levels of TC, TG, HDL-C and LDL-C were 4.83 ± 0.89 mmol/L, 1.51 ± 1.25 mmol/L, 1.36 ± 0.33 mmol/L, and 2.97 ± 0.70 mmol/L, respectively. The demographic characteristics among sedentary occupational population is shown in Table 1 (see Additional file 1: Table 1).
Prevalence of dyslipidemia
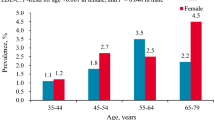
The prevalence of dyslipidemia was 29.10%, with high TG (15.86%) being the most common component, followed by low HDL-C (14.68%), high TC (6.43%) and high LDL-C (5.37%). The prevalence of dyslipidemia and its components among sedentary occupational population is shown in Tables 1 and 2, respectively (see Additional file 1: Table 1; see Additional file 2: Table 2). The prevalence of dyslipidemia was significantly higher in men than in women (39.64% vs. 12.43%, P < 0.01). The prevalence of dyslipidemia increased with increasing age, but decreased in the ≥ 70 years age group (P < 0.01). Marital status, education level, nighttime diet, animal viscera intake, sedentariness in rest, sleep time, physical activity, smoking status and drinking status, chronic diseases, family history, and BMI were also associated with the prevalence of dyslipidemia (P < 0.01 for all). Sedentary occupational population who had insufficient vegetable intake, diabetes, hypertension, CHD, CHD family history or obesity had a higher prevalence of dyslipidemia (P < 0.01). The prevalence of all dyslipidemia components varied by gender, age, education level, work organization, dietary habits, sedentary behavior, sleep time, physical activity, smoking status, drinking status, chronic diseases, family history, and BMI (P < 0.01 for all). The prevalence of high TG and low HDL-C was higher in participants who often ate late at night (P < 0.01 for both). The prevalence of high TG and low HDL-C was also higher in participants who had insufficient physical activity compared with those who had sufficient physical activity (P < 0.05 for both).
Factors influencing dyslipidemia
To identify the main factors associated with dyslipidemia, we performed multivariate stepwise logistic regression analyses with dyslipidemia and its components (high TC, high TG, high LDL-C, and low HDL-C) as the dependent variable and the demographic and lifestyle variables as the independent variables. The results are presented in Table 3 (see Additional file 3: Table 3). The factors that were associated with higher odds of dyslipidemia were male gender (OR = 3.20, P < 0.01), older age, being married or having a partner, longer sedentary time, frequent animal viscera consumption (OR = 1.17, P < 0.05), current smoking (OR = 1.54, P < 0.01), having hypertension (OR = 1.43, P < 0.01), diabetes (OR = 1.81, P < 0.01), or obesity (OR = 2.33, P < 0.01). On the other hand, the factor that was associated with lower odds of dyslipidemia was adequate vegetable intake (OR = 0.88, P < 0.01) and sufficient physical activity (OR = 0.81, P < 0.01). We also found that some factors had different effects on different subtypes of dyslipidemia. Although no effect of drinking status on dyslipidemia was observed, participants with current drinking had a 1.24 fold increased prevalence of high TG (P < 0.01). Male gender, being married or having a partner, and occasional animal viscera consumption increased the risk of high TG but decreased the risk of high TC. Older age (40–69 years), frequent animal viscera consumption, sedentariness for 2–6 h, diabetes, and obesity increased the risk of both high TC and high LDL-C. Current smoking, hypertension, diabetes, and obesity increased the risk of both high TG and low HDL-C. Nighttime diet increased the risk of high TG, but not low HDL-C. Current smokers were less likely to have low HDL-C than non-smokers.
Discussion
Dyslipidemia is a major modifiable risk factor for CVD, which is a leading cause of morbidity and mortality worldwide [35, 36]. Therefore, it is essential to understand the epidemiological characteristics and risk factors of dyslipidemia in different populations and to implement targeted preventive measures. This study is one of the largest research projects that comprehensively assessed the prevalence of dyslipidemia and its associated factors among sedentary occupational population characterized by low physical activity and high mental workload.
We found that the prevalence of dyslipidemia in our study population was 29.10%, which was lower than the national average of 40.4% and also lower than the results reported in previous studies conducted in other regions of China, such as Beijing, Inner Mongolia, Shenzhen, Shandong, and Guizhou [9, 29, 37,38,39]. One possible explanation for this finding is that our study population was mainly from the Shanghai area, which is one of the first pilot cities for the Healthy City initiative in China. Shanghai has implemented various health-related policies and conducted large-scale health education activities in all communities every year to enhance residents’ self-management capabilities in health [40,41,42]. As a result, the health literacy level of Shanghai citizens is higher than the national average. Moreover, our study population had a high level of education, with 93% having a bachelor’s degree or above, and a strong awareness of health. These factors may have influenced their health behaviors, such as dietary habits, physical activity, smoking, and alcohol consumption, which in turn affect their lipid profiles. It could mean that improving health literacy and promoting healthy behaviors are important strategies for preventing and controlling dyslipidemia among occupational populations in China.
We found that the most common abnormal component of dyslipidemia was high triglycerides (TG), which is consistent with previous research findings [20, 35, 43]. The mean levels of TC, TG, HDL-C, and LDL-C in our study were 4.83 mmol/L, 1.51 mmol/L, 1.36 mmol/L, and 2.97 mmol/L, respectively. These levels were higher than those reported by the 2012 Chinese National Nutrition and Health Survey (CNHS), which may attribute to the characteristic of light physical work of occupational population studied in this research [37].
We also observed that the prevalence of dyslipidemia and its components increased with age, especially in the 30–49 age group, in line with earlier studies [35, 44, 45]. This age group is a critical period for controlling blood lipids to prevent cardiovascular diseases, as blood lipid levels tend to rise rapidly during this period [46]. Moreover, we found that male and married status were risk factors for dyslipidemia, high TG, and low HDL-C. Although the reason has not been proven, it is possible that men have a higher prevalence of unhealthy lifestyle such as insufficient vegetable intake, late-night diet, high intake of animal offal or meat, smoking and alcohol consumption, combined with the results of the sample population with dyslipidemia. Furthermore, we noted that hypertension, diabetes, and smoking were risk factors for dyslipidemia, while a history of CHD was a protective factor for dyslipidemia and its components (excluding low HDL-C). This may be explained by the fact that CHD patients are more likely to be aware of their lipid abnormalities and receive treatment and control for them [47].
Our findings revealed a positive association between drinking and TG levels, which is in line with previous studies [48,49,50]. However, this association was not significant after adjusting for other variables in a multivariate regression analysis. This may be due to the complex effects of alcohol intake on blood lipid levels. Previous research has suggested that moderate drinking may have some health benefits, such as reducing the risk of cardiovascular disease and dementia [51, 52]. However, these benefits are not linear, and excessive drinking may increase the risk of various health problems. Therefore, the lack of a clear association between drinking and dyslipidemia in our study may reflect the balance or cancellation of the protective or harmful effects of different levels of alcohol consumption in our sample population. Further studies are needed to explore the optimal range and pattern of drinking for preventing dyslipidemia.
Physical activity is widely recognized as a key factor for maintaining good health, while sedentary behavior is associated with an increased risk of several chronic diseases (such as cardiovascular disease and cerebrovascular events) [53, 54]. Sedentary behavior has become a major public health concern in modern society. For adults, sedentary time could be divided into workplace sedentary time and leisure sedentary time [15]. Our study examined the association between leisure sedentary time and dyslipidemia among sedentary occupational population, and found that leisure sedentary time was a factor associated with dyslipidemia and all its components. We suggest that interventions to reduce sedentary behavior should be tailored to the specific needs and characteristics of different occupational groups, considering their age, social role, and life role. For example, office workers may benefit from regular breaks and physical activities during their own time [55].
Our study has some potential limitations that should be acknowledged. First, this was a single-center study, which may limit the generalizability of our findings to other sedentary occupational populations. However, the large sample size in our study may partly compensate for this limitation. Second, our study relied on self-reported information and recalled data, which may introduce sources of bias such as recall bias and measurement bias. Therefore, the accuracy and validity of the data may be affected by these factors. Third, our study used a cross-sectional design, which precludes the establishment of causal relationships between dyslipidemia and its risk factors. Longitudinal studies are needed to confirm the direction and magnitude of these associations. Fourth, our study did not consider the use of hypolipidemic drugs that might reduce the evidence sources for explaining the prevalence of dyslipidemia.
Conclusions
Our study provides valuable and current epidemiological data on dyslipidemia and its potential risk factors among sedentary occupational populations in China. The prevalence of dyslipidemia among sedentary occupational population in our study was lower than in other previous studies without the limitation of occupational characteristics. Dyslipidemia among sedentary occupational population is associated with several modifiable factors such as BMI, smoking, drinking, physical activity, and dietary habits. These findings could inform the development of effective strategies for the prevention and control of dyslipidemia in sedentary occupational populations, such as health education, lifestyle modification, and regular screening.
Data availability
The data that support this study are not publicly available due to participants’ privacy protection but can be obtained from the corresponding author upon reasonable request. Researchers who are interested in our study can contact the corresponding author Dr. Tiantian Zhang (tiantianzhang18@fudan.edu.cn) who will review the data request.
Abbreviations
- CVD:
-
Cardiovascular disease
- TC:
-
Total cholesterol
- LDL-C:
-
low-density lipoprotein cholesterol
- TG:
-
Triglycerides
- HDL-C:
-
High-density lipoprotein cholesterol
- CHD:
-
Coronary heart disease
- FBG:
-
Fasting blood glucose
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- SD:
-
Standard deviation
- ORs:
-
Odds ratios
- CNHS:
-
Chinese National Nutrition and Health Survey
References
Yan-Ling Z, Dong-Qing Z, Chang-Quan H, et al. Cigarette smoking and its association with serum lipid/lipoprotein among Chinese nonagenarians/centenarians[J]. Lipids Health Dis. 2012;11(1):1–6. https://doi.org/10.1186/1476-511X-11-94 .
Lacy M, Atzler D, Liu R, et al. Interactions between dyslipidemia and the immune system and their relevance as putative therapeutic targets in atherosclerosis[J]. Pharmacol Ther. 2019;193:50–62. https://doi.org/10.1016/j.pharmthera.2018.08.012 .
Roth GA, Johnson C, Abajobir A, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015[J]. J Am Coll Cardiol. 2017;70(1):1–25. https://doi.org/10.1016/j.jacc.2017.04.052 .
Bansilal S, Castellano JM, Fuster V. Global burden of CVD: focus on secondary prevention of cardiovascular disease[J]. Int J Cardiol. 2015;201:1–S7. https://doi.org/10.1016/S0167-5273(15)31026-3 .
Okui T. An age-period-cohort analysis of prevalence and consultation rate for dyslipidemia in Japan[J]. Asia Pac J Public Health. 2021;33(1):46–52. https://doi.org/10.1177/1010539520963643 .
Bays HE, Chapman RH, Fox KM, et al. Comparison of self-reported survey (SHIELD) versus NHANES data in estimating prevalence of dyslipidemia[J]. Curr Med Res Opin. 2008;24(4):1179–86. https://doi.org/10.1185/030079908X280527 .
Asghari S, Aref-Eshghi E, Godwin M, et al. Single and mixed dyslipidaemia in Canadian primary care settings: findings from the Canadian primary care sentinel surveillance network database[J]. BMJ open. 2015;5(12):e007954. https://doi.org/10.1136/bmjopen-2015-007954 .
Pirillo A, Casula M, Olmastroni E, et al. Global epidemiology of dyslipidaemias[J]. Nat Reviews Cardiol. 2021;18(10):689–700. https://doi.org/10.1038/s41569-021-00541-4 .
Zhu JR, Gao RL, Zhao SP et al. Guidelines for the Prevention and Treatment of Dyslipidemia in Chinese adults (revised in 2016) [J].Chinese Circulation Journal,2016,31(10):937–53. https://doi.org/10.3969/j.issn.1000-3614.2016.10.001 .
Chen Z, Jiang Y, Lu Y et al. Dyslipidemia Prevalence in Chinese older adults: a Meta-analysis [J]. Chin Gen Pract 2022,25(01):115–21.
Li SN, Zhang LF, Wang X, et al. Status of Dyslipidemia among adults aged 35 years and above in China [J]. Chin Circulation J. 2019;34(07):681–7. https://doi.org/10.3969/j.issn.1000-3614.2019 . 07.011.
Cicek G, Sedentary, Behavior. Physical activity and Cardiometabolic Diseases[J]. Int J Appl Exerc Physiol. 2020;9(7):80–9.
Fan J, Ding C, Gong W, et al. The relationship between leisure-time sedentary behaviors and metabolic risks in middle-aged Chinese women[J]. Int J Environ Res Public Health. 2020;17(19):7171. https://doi.org/10.3390/ijerph17197171 .
Dunstan DW, Dogra S, Carter SE, et al. Sit less and move more for cardiovascular health: emerging insights and opportunities[J]. Nat Reviews Cardiol. 2021;18(9):637–48. https://doi.org/10.1038/s41569-021-00547-y .
Lim MS, Park B, Kong IG, et al. Leisure sedentary time is differentially associated with hypertension, diabetes mellitus, and hyperlipidemia depending on occupation[J]. BMC Public Health. 2017;17(1):1–9. https://doi.org/10.1186/s12889-017-4192-0 .
Wang M, Hou X, Hu W, et al. Serum lipid and lipoprotein levels of middle-aged and elderly Chinese men and women in Shandong Province[J]. Lipids Health Dis. 2019;18:1–8. https://doi.org/10.1186/s12944-019-1000-0 .
He H, Yu Y, Li Y, et al. Dyslipidemia awareness, treatment, control and influence factors among adults in the Jilin province in China: a cross-sectional study[J]. Lipids Health Dis. 2014;13(1):1–9. https://doi.org/10.1186/1476-511X-13-122 .
Moradinazar M, Pasdar Y, Najafi F, et al. Association between dyslipidemia and blood lipids concentration with smoking habits in the kurdish population of Iran[J]. BMC Public Health. 2020;20(1):1–10. https://doi.org/10.1186/s12889-020-08809-z .
Ni WQ, Liu XL, Zhuo ZP. t al. Serum lipids and associated factors of dyslipidemia in the adult population in Shenzhen[J]. Lipids in Health and Disease,2015, 14:1–11. https://doi.org/10.1186/s12944-015-0073-7 .
Cahill LE, Chiuve SE, Mekary RA, et al. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals[J]. Circulation. 2013;128(4):337–43.
Zheng Y, Zhou Z, Wu T, et al. Association between composite lifestyle factors and cardiometabolic multimorbidity in Chongqing, China: a cross-sectional exploratory study in people over 45 years and older[J]. Front Public Health. 2023;11:1118628. https://doi.org/10.3389/fpubh.2023.1118628 .
Cao QM, Wang WJ, Zhang L et al. The practice of balanced diet model for Chinese residents: interpretation of dietary guidelines for Chinese residents (2022)[J]. Food and Machinery,2022,38(06):22–9. https://doi.org/10.13652/j.spjx.1003.5788.2022.60050 .
Haslam DE, Peloso GM, Herman MA, et al. Beverage consumption and longitudinal changes in lipoprotein concentrations and incident dyslipidemia in US adults: the Framingham heart study[J]. J Am Heart Association. 2020;9(5):e014083. https://doi.org/10.1161/JAHA.119.014083 .
Ross R, Chaput JP, Giangregorio LM, et al. Canadian 24-Hour Movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep[J]. Appl Physiol Nutr Metab. 2020;45(10):57–S102. https://doi.org/10.1139/apnm-2020-0467 .
Jani BD, McQueenie R, Nicholl BI, et al. Association between patterns of alcohol consumption (beverage type, frequency and consumption with food) and risk of adverse health outcomes: a prospective cohort study[J]. BMC Med. 2021;19(1):1–14. https://doi.org/10.1186/s12916-020-01878-2 .
Kutkienė S, Petrulionienė Ž, Laucevičius A, et al. Severe dyslipidemia and concomitant risk factors in the middle-aged Lithuanian adults: a cross-sectional cohort study[J]. Lipids Health Dis. 2018;17:1–6. https://doi.org/10.1186/s12944-018-0731-7 .
Zhao Y, Strauss J, Yang G, et al. China health and retirement longitudinal study–2011–2012 national baseline users’ guide[J]. Beijing: National School of Development, Peking University; 2013. p. 2.
Xi Y, Niu L, Cao N, et al. Prevalence of dyslipidemia and associated risk factors among adults aged ≥ 35 years in northern China: a cross-sectional study[J]. BMC Public Health. 2020;20:1–9. https://doi.org/10.1186/s12889-020-09172-9 .
Joint Committee for Guideline Revision. 2016 Chinese guidelines for the management of dyslipidemia in adults[J]. Journal of Geriatric Cardiology, 2018;15(1):1–29. https://doi.org/10.11909/j.issn.1671-5411.2018.01.011 .
Liu LS, Wu ZS, Wang JG, et al. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of Chinese Guidelines for prevention and treatment of hypertension [J]. J Geriatric Cardiol. 2019;16(3):182–245. https://doi.org/10.11909/j.issn.1671-5411.2019.03.014 .
Chinese Diabetes Society. Guidelines for the prevention and control of type 2 diabetes in China (2017 edition) [J]. Chin J Practical Intern Med. 2018;38(04):292–344. https://doi.org/10.19538/j.nk2018040108 .
China Working Group on Obesity. Guidelines for the Prevention and Control of Overweight and Obesity in Chinese adults (trial) [J]. Acta Nutrimenta Sinica. 2014;011–4. https://doi.org/10.13325/j.cnki.acta.nutr.sin.2004.01.001 .
James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)[J]. JAMA-Journal of the American Medical Association. 2014;311(5):507–20. https://doi.org/10.1001/jama.2013.284427 .
Bao Y, Lu J, Wang C, et al. Optimal waist circumference cutoffs for abdominal obesity in Chinese[J]. Atherosclerosis. 2008;201(2):378–84. https://doi.org/10.1016/j.atherosclerosis.2008.03.001 .
Fan Y, Huang JJ, Sun CM, et al. Prevalence of dyslipidaemia and risk factors in Chinese coal miners: a cross-sectional survey study[J]. Lipids Health Dis. 2017;16(1):1–17. https://doi.org/10.1186/s12944-017-0548-9 .
Liu S, Li Y, Zeng X, et al. Burden of cardiovascular diseases in China, 1990–2016: findings from the 2016 global burden of disease study[J]. JAMA Cardiol. 2019;4(4):342–52. https://doi.org/10.1001/jamacardio.2019.0295 .
Zhang FL, Xing YQ, Wu YH, et al. The prevalence, awareness, treatment, and control of dyslipidemia in northeast China: a population-based cross-sectional survey[J]. Lipids Health Dis. 2017;16(1):1–13. https://doi.org/10.1186/s12944-017-0453-2 .
Nie F, Wang Z, Zeng Q, et al. Health behaviors and metabolic risk factors are associated with dyslipidemia in ethnic Miao Chinese adults: the China multi-ethnic cohort study[J]. BMC Public Health. 2021;21:1–14. https://doi.org/10.1186/s12889-021-10871-0 .
Cai L, Zhang L, Liu A, et al. Prevalence, awareness, treatment, and control of dyslipidemia among adults in Beijing, China[J]. J Atheroscler Thromb. 2012;19(2):159–68. https://doi.org/10.5551/jat.10116 .
Zou SS, Wen TX, Gai YR et al. Comparative analysis of health policies of residents in Shenzhen and Shanghai[J]. China Mod Doctor 2023,61(09):85–8. https://doi.org/10.3969/j.issn.1673-9701.2023.09.021 .
Ma J. Analysis on the practice and development of the construction of Healthy City in Shanghai[J].Health Education and Health Promotion,2018,13(05):470–2. https://doi.org/10.16117/j.cnki.31-1974/r.201805030 .
Pan XF, Ding Y, Chen RJ et al. Strategy study of improving residents’ health literacy under the guidance of Healthy Shanghai Action[J]. Shanghai J Prev Med 2020,32(01):23–9. https://doi.org/10.19428/j.cnki.sjpm.2020.19867 .
Huang Y, Gao L, Xie X, et al. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control[J]. Popul Health Metrics. 2014;12:1–9. https://doi.org/10.1186/s12963-014-0028-7 .
Wang S, Xu L, Jonas JB, et al. Prevalence and associated factors of dyslipidemia in the adult Chinese population[J]. PLoS ONE. 2011;6(3):e17326. https://doi.org/10.1371/journal.pone.0017326 .
Sharma U, Kishore J, Garg A, et al. Dyslipidemia and associated risk factors in a resettlement colony of Delhi[J]. J Clin Lipidol. 2013;7(6):653–60. https://doi.org/10.1016/j.jacl.2013.06.003 .
Zhou H, Ding X, Yang Q, et al. Associations of Hypertriglyceridemia Onset Age with Cardiovascular Disease and all-cause mortality in adults: a cohort Study[J]. J Am Heart Association. 2022;11(20):e026632. https://doi.org/10.1161/JAHA.122.026632 .
Panahi S, Tremblay A. Sedentariness and health: is sedentary behavior more than just physical inactivity?[J]. Front Public Health. 2018;6:258. https://doi.org/10.3389/fpubh.2018.00258 .
Capurso NA, Petrakis I. Dyslipidemia associated with heavy alcohol use[J]. Am J Addictions. 2016;25(3):188–90. https://doi.org/10.1111/ajad.12347 .
Bessembinders K, Wielders J, van de Wiel A. Severe hypertriglyceridemia influenced by alcohol (SHIBA)[J]. Alcohol Alcohol. 2011;46(2):113–6. https://doi.org/10.1093/alcalc/agq088 .
Tada H, Kawashiri M, Nakahashi T, et al. Clinical characteristics of Japanese patients with severe hypertriglyceridemia[J]. J Clin Lipidol. 2015;9(4):519–24. https://doi.org/10.1016/j.jacl.2015.05.004 .
Agarwal DP. Cardioprotective effects of light–moderate consumption of alcohol: a review of putative mechanisms[J]. Alcohol Alcohol. 2002;37(5):409–15. https://doi.org/10.1093/alcalc/37.5.409 .
Ruitenberg A, Van Swieten JC, Witteman JCM, et al. Alcohol consumption and risk of dementia: the Rotterdam Study[J]. The Lancet. 2002;359(9303):281–6. https://doi.org/10.1016/S0140-6736(02)07493-7 .
Dutheil F, Duclos M, Esquirol Y. Sedentary behaviors at Work[J]. Front Public Health. 2020;8:57. https://doi.org/10.3389/fpubh.2020.00057 .
Hupin D, Raffin J, Barth N, et al. Even a previous light-active physical activity at work still reduces late myocardial infarction and stroke in retired adults aged > 65 years by 32%: the PROOF cohort study[J]. Front Public Health. 2019;7:51. https://doi.org/10.3389/fpubh.2019.00051 .
Manini TM, Carr LJ, King AC, et al. Interventions to reduce sedentary behavior[J]. Med Sci Sports Exerc. 2015;47(6):1306. https://doi.org/10.1249/MSS.0000000000000519 .
Acknowledgements
We express our gratefulness to all the participants who supported and cooperated with this study, we also acknowledge the contributions the project team members and colleagues.
Funding
This work was supported by the National Key Research and Development Plan Project (No. 2022YFC3600903), and the National Nature Science Foundation of China(No. 72204048).
Author information
Authors and Affiliations
Contributions
DX Gu and DD Wang conceived and designed the study, performed the formal analysis, and wrote the original draft. QZ Zhu and L Luo provided the resources, reviewed and edited the manuscript. TT Zhang oversaw the study design, implementation, and analysis, and revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Ethics and Research Committee of Huadong Sanatorium Health Examination Center (approval number: ECHS2023-07). All people signed electronic informed consent before filling out the questionnaire. Personal private information was deleted in advance, and statistical analyses were conducted with strict confidentiality and only used for scientific purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
English language editing statement: Each of our co-authors has proofread the revised manuscript and polished the language. We hope it can meet the standard of publication this time. To ensure the quality of the article, we will check the final script again before publication or use a professional English editing service if necessary.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gu, D., Wang, D., Zhu, Q. et al. Prevalence of dyslipidemia and associated factors in sedentary occupational population from Shanghai: a cross-sectional study. Arch Public Health 82, 21 (2024). https://doi.org/10.1186/s13690-024-01245-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-024-01245-0