Abstract
Background
The disproportionate mortality burden racial and ethnic groups endure compared to their non-Hispanic white (NHW) counterparts is a widely known public health issue in the United States.
Methods
We examined disparities in premature mortality through a measure of years of potential life lost (YPLL) among racial and ethnic groups after accounting for individual and place-based risk factors. Data were nearly 400,000 geocoded death records from Washington state mortality records from 2011 to 2018. Decedent records included information on marital status and educational attainment at time of death. We linked these records to census tract indicators of rurality and area deprivation based on residential longitude and latitude coordinates at time of death. We conducted censored Poisson regression to test adjusted associations between racial and ethnic identity and YPLL.
Results
Relative to non-Hispanic whites, non-Hispanic blacks, American Indian and Alaska Natives, Asian or other Pacific Islanders, multiracial, and Hispanic decedents had significantly higher rates of YPLL. Controlling for sociodemographic factors reduced but did not eliminate the disparities in YPLL between non-Hispanic whites and other racial and ethnic groups. Controlling for place-based risk factors did not further attenuate differences.
Conclusions
Racial and ethnic minorities suffer disproportionately from premature mortality. Researchers and policy makers must recognize the disproportionate risks to premature mortality and work together to alleviate them through the delivery of better and more accessible targeted services.
Similar content being viewed by others
Background
The disproportionate mortality burden racial and ethnic groups endure compared to their non-Hispanic white (NHW) counterparts is a widely known public health issue in the United States [8, 16, 30, 32]. American Indian and Alaska Natives (AIANs) and Blacks experience substantially higher rates of death and premature mortality compared to all other racial and ethnic groups across a wide array of causes [19, 21, 31, 34]. On average, NHWs outlive most racial and ethnic minority groups by nearly 13 years [5]. Second, differences in premature mortality burden are continuously observed between men and women. Men are more likely to die prematurely compared to women and the average national life expectancy among women is 80.5 years while men’s life expectancy is 75.1 years [2]. While entire groups are at risk of dying prematurely, uncovering information on how many years of life they have lost in association with major sociodemographic factors that contribute to this disparity are crucial and cannot be understood from broad estimates of mortality risk.
Social determinants of health such as education, income, and place of residence have been examined as causes that drive mortality risk. Socioeconomic status specifically has been coined a fundamental cause of mortality disparities [26]. The theory of fundamental causes states that those who have higher socioeconomic status (SES) are better able to leverage their education and income to access life-saving resources and networks. Lower SES individuals do not have similar access to invaluable resources and higher SES networks and are therefore at higher risk of mortality [4, 22]. Since place of residence is in large part determined by SES, it plays an important role in determining mortality and contributing to racial and ethnic differences in mortality [7]. In terms of premature mortality, we see an unequal distribution of younger deaths across a myriad of causes among those who experience higher socioeconomic deprivation [20]. There are techniques which take age at death and socioeconomic risk factors into account which provides more context to the impact premature mortality has on society.
Premature death has serious economic implications at both state and national levels. This is increasingly important as the youngest of adults in society make up a large portion of the United States work force and their premature mortality negatively impacts the economy. A recent study [32] shows that younger racial and ethnic minorities, such as AIANs age 25–30 years old, were more likely to die prematurely compared to NHWs. Other studies have more explicitly documented the economic benefits of reducing or even eliminating racial and ethnic mortality disparities. For example, a study in Minnesota estimated that eliminating racial disparities in preventable deaths alone would produce 1 to 3 billion dollars in economic savings [24]. These savings occur in increased productivity in the labor market but the benefits to reduced disparities in mortality extend to improved and diversified innovation, entrepreneurship, and political leadership as well.
In this paper, we include two well documented contextual determinants of mortality, rurality and socioeconomic disadvantage. Rurality has negative impacts on individual mortality prospects. Compared to residents of urban areas, rural residents have higher risks of all-cause and cause-specific mortality [12, 14, 15, 27]. Prior to the 1980s, urban dweller areas faced public health crises such as transmission of infectious diseases and higher rates of mortality due to poor infrastructure and population density issues [39]. Currently, however, that trend has changed and evidence suggests that individuals living in rural areas experience what is described as the rural mortality penalty or excess risk of death for those who reside in rural areas [6, 29]. The overwhelming majority of Washington state, 30 of the 39 counties, is designated as rural by the state Department of Health [36].
In addition to rurality, area socioeconomic conditions also impact mortality risk for individuals. In particular, the area deprivation index (ADI) [33], captures important elements of socioeconomic deprivation, economic inequality, and disparities in resource availability across geographic space that are robustly linked to mortality prospects. Previous research has shown that racial and ethnic minorities including AIANs, Black, Asian or Native Hawaiian or other Pacific Islander, and multiracial people have higher odds of premature mortality (dying before the age of 65) compared to Whites, and those racial and ethnic minorities residing in deprived areas have double to quadruple the risk of premature cancer mortality than Whites in affluent areas [23].
In the current study, we provide adjusted estimates of the association of racial and ethnic identity with Years of Potential Life Lost (YPLL) for 4 racial and ethnic minority groups, including decedents of multi-racial identity. YPLL, compared to other mortality estimates, is a particularly valuable measure of premature mortality. YPLL compares observed age at death with life expectancy to estimate the average time an individual would have lived had that individual not died relative to the general population’s expected age of death. Compared to other estimates of mortality such as rate ratios or relative risk, YPLL captures loss resulting from mortality in several domains, social and economic, making this measure stand apart in its ability to expose the impact that premature death has on society.
Methods
Data
Data on registered deaths for Washington State were obtained from the state Department of Health, Center for Health Statistics for the years 2011–2018 [37]. The data file included information on decedents’ age, sex, race, ethnicity, education, marital status, and residential longitude and latitude. Inclusion criteria for this study were individuals who were 25 years and older at the time of death. People at this age are mature and have a more stable level of education than those 18 and younger [13]. Our final data set includes nearly 400,000 decedents from Washington state over the study period.
Measures
Outcome variable
YPLL is calculated by subtracting the age at the time of death from a predetermined end point age [10]. The premature mortality benchmark of 75 has been used based on U.S., Canadian, Australian, and European studies quantifying the burden of premature mortality [1, 3, 28, 40]. For example, using the end point age of 75, an individual who died at the age of 25 would have 50 years of life lost and those who died at age 75 or above would have 0 YPLL. This approach censored YPLL at zero for decedents whose age at death was 75 or above.
Individual-level explanatory variables
Individual-level variables included race and ethnicity (six categories: NHW, NH Black, NH AIAN, NH Asian or Native Hawaiian or other Pacific Islander, NH multiracial (2 or more racial identities), and Hispanics), sex, educational attainment at time of death, and marital status at time of death.
Community-level explanatory variables
Rurality was classified using the Rural–Urban Commuting Area (RUCA) codes based on decedents’ residential location at the time of death. RUCA codes use work commuting information, population data, and measures of urbanization to classify urban and rural areas at the census tract level. RUCA codes of 1–3 were classified as metropolitan areas, codes of 4–6 were classified as micropolitan areas, and codes 7 through 10 were classified as small towns and rural areas [36]. The ADI, a validated composite score of socio-economic disadvantage, was used to quantify the social and economic characteristics of census tracts [17, 33]. The ADI was developed based on 17 Census variables in four domains of poverty, housing, employment, and education. We divided ADI scores into terciles of deprivation (1 = least-deprived, 2 = middle-deprived, 3 = most-deprived).
Statistical analysis
Descriptive statistics included measures of central tendency and variability for continuous variables and frequency distributions and percentages for categorical variables. The Interquartile Range (IQR) will be calculated to determine the midpoint of average death for each racial and ethnic group and determine the spread of death across all groups. We used censored Poisson regression to test the association between race/ethnicity and YPLL controlling for other individual and community-level explanatory variables. This modeling technique was appropriate because we censored YPLL at zero for decedents whose age at death was 75 or above. Preliminary analysis of data showed that a clustering effect was small (intraclass correlation coefficient: 0.01 – 0.03), thus, multilevel estimation was unnecessary.
We start with an adjusted model to examine the relationship between YPLL and race/ethnicity, controlling for sex and year. Next, we progressively adjust for education and marital status of the decedent, and then for residential census tract rurality and area disadvantage. In addition to models on all decedents, we also stratify results and present male and female specific estimates as a priori because average national life expectancy among women and men differs. Associations are presented as incidence risk ratios (IRR) with 95% confidence intervals (CI). Confidence intervals that did not include zero were considered statistically significant. The R-software was used for analysis.
Results
Table 1 shows characteristics of all decedents age 25 and older in Washington State and also stratified by sex. Deaths with residential locations with address matching accuracy of 80% or above were included in the analyses. Less than two percent of deaths were excluded because they occurred before individuals turned 25. For brevity, we focus on a limited number of characteristics for all decedents here. Decedents were predominantly NHW (88.6%). Deaths were evenly distributed among men and women during the study period.
Among all decedents, the mean age at death for NHWs (76) was over a decade longer than that of AIAN (64), multi-racial (65), and Hispanic (65) decedents. More consistent with the literature and because the age at death was not normally distributed, we also show the median age at death in Table 1. Large differences exist here as well. Median age of NHWs was 79 (IQR: 21), while the median age of NH Blacks, NH AIANs, multiracial individuals, and Hispanics were 67 (IQR range: 23), 65 (IQR: 24), 66 (IQR: 27), and 66 (IQR: 29), respectively.
Most decedents lived in metropolitan census tracts (84.5%); roughly 9% lived in micropolitan areas and 7% lived in small towns or rural areas. Less than four percent (3.9%) of deaths were excluded because of missing or inaccurate residential address data. Although differences in median age at death across metropolitan (79), micropolitan (79), and rural (77) neighborhoods were minimal the median age of decedents was higher in less-deprived neighborhoods compared to their peers in the most-deprived neighborhoods (80 [IQR = 22] vs. 76 [IQR = 23].
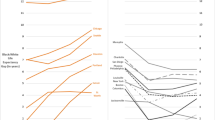
Table 2 shows the results of censored Poisson regression models on YPLL for decedents. In unadjusted models, compared to NHWs, NH Blacks and NH AIANs had, respectively, a rate 1.25 (95% CI = 1.24 – 1.26) and 1.34 (1.33 – 1.35) times higher for YPLL. The rate for NH Asian or Other Pacific Islander decedents was 1.15 (1.14 – 1.15) times higher and for Multiracial and Hispanic decedents 1.46 (1.45 – 1.47) and 1.49 (1.48 – 1.50) times higher compared to NHWs (Model 1).
Estimates for the relationship between YPLL and race/ethnicity (except for NH Asian or Other Pacific Islander) were attenuated across Model 1 and 2. For example, adjusting for sex, marital status and educational attainment in Model 2 results in an IRR for NH Blacks of 1.13 (1.13 – 1.14), down from 1.25 in Model 1; a 48% lower ([1.25–1.13] / [1.25–1.00] * 100) IRR. Importantly, although the IRRs for racial and ethnic minorities are lower in Model 2, compared to Model 1, they remain higher than NHWs. Estimates for the relationship between YPLL and race/ethnicity remained stable across Model 2 and 3. Further adjusting by RUCA and ADI, NH AIANs had a fully adjusted rate 1.22 (1.21 – 1.23) times higher for YPLL compared to NHWs. For NH Blacks and NH Asian or Other Pacific Islander decedents, the rate was 1.12 (1.12 – 1.13) and 1.17 (1.16 – 1.18) times higher, respectively. Multi-racial decedents had a rate 1.34 (1.33 – 1.36) times higher and Hispanics 1.39 (1.39 – 1.40) times higher compared to NHWs (Model 3). Similar patterns were observed in sex stratified models when the results of unadjusted and adjusted models were compared within each sex.
The control variables in these fully adjusted models demonstrate that never married decedents had IRRs 1.81 times higher than married or cohabiting decedents (Model 3); for males this was 1.66 times higher (Model 6) and for females 1.87 times higher (Model 9). Decedents with a bachelor’s degree or more had 0.89 times the rate of YPLL as decedents with no high school diploma. This protection was present for male (IRR = 0.96, Model 6) and female decedents (IRR = 0.86, Model 9) with a bachelor’s degree or more. For all, female and male decedents, living in micropolitan and small town or rural neighborhoods carried lower rates of YPLL, compared to decedents in metropolitan neighborhoods. Lastly, the ADI illustrates that the more disadvantaged the neighborhood the higher the rate of YPLL for all and female decedents but not for male decedents.
Discussion
The burden of premature mortality is widely understood as being a prominent disparity among racial and ethnic groups. Within Washington State we found that all decedents who identified as racial and ethnic minorities had higher rates of YPLL compared to NHWs—including NH Blacks, NH AIANs, NH Asian or Native Hawaiian or other Pacific Islander, NH multi-racial, and Hispanic decedents. Multiracial and Hispanic decedents had the highest rates of YPLL compared to NHWs even after controlling for important individual and place-based risk factors for mortality. Although the life expectancy of the average person has increased over the last several decades, mortality disparities continue to plague racial and ethnic minorities.
Social, economic, and contextual determinants of health such as marital status, individual educational attainment, rurality, and area-level socioeconomic deprivation all contribute to YPLL and can be addressed through effective social and economic policies. In our study, adjusting for sociodemographic characteristics such as marital status and educational attainment attenuated the relationship between race/ethnicity and YPLL and RUCA and ADI did not have much of an effect on YPLL differences. Disparities in YPLL among racial and ethnic groups remain a significant issue and may be explained by other mechanisms underlying racial and ethnic differences. For example, a related study on premature mortality which explores birth cohort effects among Black and NHW individuals that died between 1960–2009 found differences between Black age cohorts who did and did not endure Jim Crow era policies [18]. This study serves as an example of a time period which helps explain an improvement in premature mortality risk. Could there be something in our data that could lend itself to explaining why sociodemographic factors show no difference between our models? Could there be policies in Washington State that could impact racial and ethnic groups and explain some of the differences in YPLL?
Using YPLL may have illuminated a different context under which race matters for reasons beyond SES. Previous studies have shown that context matters and alternative methods and measures such as exploring particular causes of death instead of mortality generally or the effect of historical context amongst particular groups could help further illuminate why race is so important. Future research must address structural racism that restricts access to affordable housing and economic opportunity, prevents equitable political representation, and hampers attaining good health and well-being [11, 38]. Improvements in risk factors for premature death, such as access to quality education, hold promise to close the gaps in length of life by racial and ethnic identity. Nonetheless, other contributors to racial and ethnic minority gaps in longevity remain to be explored.
These analyses have several notable limitations. First, racial misclassification, typically as white, is a limitation of the data we used in this report. For example, AIAN deaths are undercounted by at least 38% nationally [9, 35], especially on death certificates, the source of our data. Second, we only had data on a single timepoint of decedents’ characteristics such as marital status, residential history, and area deprivation. These characteristics may vary over time and can potentially be risk factors for premature mortality. Third, the majority of decedents in our study were NHW, reflecting the demographics of Washington State residents. Our findings may not necessarily reflect patterns in other states with more diverse populations. Fourth, these data do not include deaths from the novel coronavirus, which has been shown to disproportionately infect and kill by race and ethnicity [25].
Conclusion
In summary, despite increasing life expectancy and decreases in the gap in life expectancy between whites and racial and ethnic minority groups, important differences in the mortality experience by racial and ethnic identity remain unexplored. Our findings showed that racial and ethnic minorities continue to experience a disproportionate burden of premature death in Washington state. Researchers and policy makers must recognize the disproportionate risks to premature mortality and work together to alleviate them through the delivery of better and more accessible targeted health services.
Availability of data and materials
Data on all decedents were purchased from the Washington Department of Health. A request to purchase records can be made at https://www.doh.wa.gov/DataandStatisticalReports/WashingtonTrackingNetworkWTN/DataPortal.
References
Adair T, Lopez A. Widening inequalities in premature mortality in Australia, 2006–16. Aust Popul Stud. 2020;4:37–56. https://doi.org/10.37970/aps.v4i1.62.
Arias E, Tejada-Vera B, Ahmad F. Provisional Life Expectancy Estimates for January through June, 2020. Vital Statistics Rapid Release. 2021;10:1–8.
Athens JK, Remington PL, Gangnon RE. Improving the Rank Precision of Population Health Measures for Small Areas with Longitudinal and Joint Outcome Models. PLoS ONE. 2015;10:e0130027. https://doi.org/10.1371/journal.pone.0130027.
Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic Disparities in Health in the United States: What the Patterns Tell Us. Am J Public Health. 2010;100:S186–96. https://doi.org/10.2105/AJPH.2009.166082.
CDC, 2019. From the CDC-Leading Causes of Death-Males Non-Hispanic white 2017 [WWW Document]. Cent Dis Control Prev. URL https://www.cdc.gov/healthequity/lcod/men/2017/nonhispanic-white/index.htm (Accessed 26 Jan 21).
Cosby AG, Neaves TT, Cossman RE, Cossman JS, James WL, Feierabend N, Mirvis DM, Jones CA, Farrigan T. Preliminary Evidence for an Emerging Nonmetropolitan Mortality Penalty in the United States. Am J Public Health. 2008;98:1470–2. https://doi.org/10.2105/AJPH.2007.123778.
Denney JT, Saint Onge JM, Dennis JA. Neighborhood Concentrated Disadvantage and Adult Mortality: Insights for Racial and Ethnic Differences. Popul Res Policy Rev. 2018;37:301–21. https://doi.org/10.1007/s11113-018-9461-9.
Fingerhut LA, MaKuc DM. Mortality among minority populations in the United States. Am J Public Health. 1992;82:1168–70. https://doi.org/10.2105/AJPH.82.8.1168.
Frost F, Tollestrup K, Ross A, Sabotta E, Kimball E. Correctness of Racial Coding of American Indians and Alaska Natives on the Washington State Death Certificate. Am J Prev Med. 1994;10:290–4. https://doi.org/10.1016/S0749-3797(18)30581-6.
Gardner JW, Sanborn JS. Years of potential life lost (YPLL)—what does it measure? Epidemiology. 1990:322–9.
Gee GC, Ford CL. STRUCTURAL RACISM AND HEALTH INEQUITIES. Bois Rev Soc Sci Res Race. 2011;8:115–32. https://doi.org/10.1017/S1742058X11000130.
Hale N, Beatty K, Smith M. The Intersection of Residence, Community Vulnerability, and Premature Mortality. J Rural Health. 2019;35:471–9. https://doi.org/10.1111/jrh.12318.
Heide I. van der, Wang J, Droomers M, Spreeuwenberg P, Rademakers J, Uiters E. The Relationship Between Health, Education, and Health Literacy: Results From the Dutch Adult Literacy and Life Skills Survey. J Health Commun. 2013;18:172–84. https://doi.org/10.1080/10810730.2013.825668.
Henning-Smith C, Hernandez AM, Ramirez M, Hardeman R, Kozhimannil K. Dying Too Soon: County-level Disparities in Premature Death by Rurality, Race, and Ethnicity, Policy Brief. Rural Health Research Center: University of Minnesota; 2019.
James WL. All Rural Places Are Not Created Equal: Revisiting the Rural Mortality Penalty in the United States. Am J Public Health. 2014;104:2122–9. https://doi.org/10.2105/AJPH.2014.301989.
Jones K, Mansfield CJ. Premature Mortality in North Carolina: Progress, Regress, and Disparities by County and Race, 2000–2010. N C Med J. 2014;75:159–68. https://doi.org/10.18043/ncm.75.3.159.
Knighton AJ, Savitz L, Belnap T, Stephenson B, VanDerslice J. 2016. Introduction of an Area Deprivation Index Measuring Patient Socioeconomic Status in an Integrated Health System: Implications for Population Health. eGEMs 4. https://doi.org/10.13063/2327-9214.1238
Krieger N, Chen JT, Coull BA, Beckfield J, Kiang MV, Waterman PD. Jim Crow and premature mortality among the US Black and White population, 1960–2009. Epidemiology. 2014;25:494–504.
Lee-Rodriguez C, Wada PY, Hung Y-Y, Skarbinski J. Association of Mortality and Years of Potential Life Lost With Active Tuberculosis in the United States. JAMA Netw Open. 2020;3:e2014481–e2014481. https://doi.org/10.1001/jamanetworkopen.2020.14481.
Lewer D, Jayatunga W, Aldridge RW, Edge C, Marmot M, Story A, Hayward A. Premature mortality attributable to socioeconomic inequality in England between 2003 and 2018: an observational study. Lancet Public Health. 2020;5(1):e33–41.
Li C, Ekwueme DU, Rim SH, Tangka FK. Years of Potential Life Lost and Productivity Losses From Male Urogenital Cancer Deaths—United States, 2004. Urology. 2010;76:528–35. https://doi.org/10.1016/j.urology.2010.04.030.
Link BG, Phelan J. Social Conditions As Fundamental Causes of Disease. J Health Soc Behav. 1995;35:80–80. https://doi.org/10.2307/2626958.
Monsivais P, Amiri S, Denney JT, Amram O. Area deprivation amplifies racial inequities in premature mortality: Analysis of 242,667 deaths in Washington State, USA 2011–15. Health Place. 2020;61:102261.
Nanney MS, Myers SL, Xu M, Kent K, Durfee T, Allen ML. The economic benefits of reducing racial disparities in health: the case of Minnesota. Int J Environ Res Public Health. 2019;16:742.
National Center for Health Statistics. Health Disparities: Provisional Death Counts for Coronavirus Disease 2019 (COVID-19). Retrieved from https://www.cdc.gov/nchs/nvss/vsrr/covid19/health_disparities.htm. Accessed 8 Aug 2021.
Phelan JC, Link BG, Diez-Roux A, Kawachi I, Levin B. “Fundamental Causes” of Social Inequalities in Mortality: A Test of the Theory. J Health Soc Behav. 2004;45:265–85. https://doi.org/10.1177/002214650404500303.
Pugh LD. Geographic Patterns of Years of Potential Life Lost for Mahoning County, Ohio, Census Tracts, 2010. Pap Appl Geogr. 2016;2:342–51. https://doi.org/10.1080/23754931.2015.1014684.
Renard F, Deboosere P. Mapping premature mortality to explore underlying socioeconomic disparities: the case of Belgium: Françoise Renard. Eur. J. Public Health. 2014;24. https://doi.org/10.1093/eurpub/cku151.048
Roth AR, Denney JT, Amiri S, Amram O. Characteristics of place and the rural disadvantage in deaths from highly preventable causes. Soc Sci Med. 2020;245:112689. https://doi.org/10.1016/j.socscimed.2019.112689.
Roy B, Kiefe CI, Jacobs DR, Goff DC, Lloyd-Jones D, Shikany JM, Reis JP, Gordon-Larsen P, Lewis CE. Education, Race/Ethnicity, and Causes of Premature Mortality Among Middle-Aged Adults in 4 US Urban Communities: Results From CARDIA, 1985–2017. Am J Public Health. 2020;110:530–6. https://doi.org/10.2105/AJPH.2019.305506.
Ruhm CJ. Drug Mortality and Lost Life Years Among U.S. Midlife Adults, 1999–2015. Am J Prev Med. 2018;55:11–8. https://doi.org/10.1016/j.amepre.2018.03.014.
Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA, Hartge P, Rosenberg PS, Thomas D, Freedman ND, de Gonzalez AB. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet. 2017;389:1043–54. https://doi.org/10.1016/S0140-6736(17)30187-3.
Singh GK. Area Deprivation and Widening Inequalities in US Mortality, 1969–1998. Am J Public Health. 2003;93:1137–43. https://doi.org/10.2105/AJPH.93.7.1137.
Stahre M, Roeber J, Kanny D, Brewer RD, Zhang X. Contribution of Excessive Alcohol Consumption to Deaths and Years of Potential Life Lost in the United States. Prev Chronic Dis. 2014;11:130293. https://doi.org/10.5888/pcd11.130293.
Stehr-Green P, Bettles J, Robertson LD. Effect of Racial/Ethnic Misclassification of American Indians and Alaskan Natives on Washington State Death Certificates, 1989–1997. Am J Public Health. 2002;92:443–4. https://doi.org/10.2105/AJPH.92.3.443.
Washington State Department of Health. Rural and Urban Counties. 2017.
Washington State Department of Health Services Center for Health Statistics: Death Data. 2020. https://www.doh.wa.gov/DataandStatisticalReports/HealthStatistics/Death.
Williams DR. Miles to Go before We Sleep. J Health Soc Behav. 2012;53:279–95. https://doi.org/10.1177/0022146512455804.
Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–16. https://doi.org/10.1016/S0033-3549(04)50068-7.
Zygmunt A, Kendall CE, James P, Lima I, Tuna M, Tanuseputro P. Avoidable Mortality Rates Decrease but Inequity Gaps Widen for Marginalized Neighborhoods: A Population-Based Analysis in Ontario, Canada from 1993 to 2014. J Community Health. 2020;45:579–97. https://doi.org/10.1007/s10900-019-00778-8.
Acknowledgements
Not applicable
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Study concept and design: SA, SS, JTD; data acquisition: SA, JTD; statistical analysis: SA, JTD; drafting the manuscript: SA, SS, JTD; Interpretation of data and analysis: SA, JTD, DB; Supervision: JTD, DB. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This evaluation of de-identified death records did not use living human subjects and did not require review or approval by an institutional review board for human subjects.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial competing interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amiri, S., Stanley, S.L., Denney, J.T. et al. Disparities in years of potential life lost among racial and ethnic groups in Washington state. Arch Public Health 80, 211 (2022). https://doi.org/10.1186/s13690-022-00969-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-022-00969-1