Abstract
Background
Tetanus is a vaccine-preventable disease that can occur in all populations, with neonates and pregnant women being at the most risk. Ethiopia has the highest maternal and neonatal tetanus morbidity and mortality rates. Besides, only 49% of mothers get vaccinated with adequate tetanus toxoid in Ethiopia which is below the world health organization recommendation. To date, there is limited evidence on the individual and community level determinants of poor tetanus toxoid (TT) immunization. Therefore, this study aimed to assess individual and community-level factors associated with poor TT immunization coverage in Ethiopia.
Method
Secondary data analysis was conducted using the 2016 Ethiopian demographic and health survey. A total of 7043 pregnant women were included in the current study. A multilevel logistic regression model was used to identify individual and community level determinants of poor tetanus toxoid immunization. Finally, the adjusted odds ratio with a 95% confidence interval was reported.
Results
In the multilevel logistic regression model adjustment, having no Antenatal care visit (AOR = 5.64; 95% CI:2.48,7.30) and having one to three antenatal care visit (AOR = 1.50; 95% CI: 1.19–1.82); poor wealth index (AOR = 1.26; 95% CI: 1.03, 1.54); not being exposed to media (AOR = 1.29; 95% CI: 1.10, 1.51); maternal unemployment (AOR = 1.15; 95% CI: 1.10, 1.31); rural residence (AOR = 1.13; 95% CI: 1.08, 1.72); and high community illiteracy (AOR = 1.28; 95% CI: 1.03, 1.58) were associated with higher odds of poor tetanus toxoid immunization. Whereas, iron uptake during pregnancy (AOR = 0.59; 95% CI: 0.51, 0.68), was associated with lower odds of poor tetanus toxoid immunization.
Conclusion
In this study tetanus toxoid (TT) vaccine utilization was affected by both community and individual-level factors. Therefore, focusing on antenatal care services especially encouraging pregnant women to have at least four visits, consulting women to be exposed to media, improving community literacy and maternal employment will help to minimize TT underutilization.
Similar content being viewed by others
Background
Tetanus is a life-threatening bacterial disease caused by spores of Clostridium tetani found throughout the world [1]. It is common in areas of poor hygiene, the most disadvantaged, economically poor, and without access to adequate health services [2]. Although tetanus can occur in all age groups, neonates, and women with recent pregnancies are most at risk, especially when childbirths take place under unhygienic conditions [3].
Case fatality rates from tetanus in resource-limited settings can be up to 100%, though with adequate medical care it can be reduced to 10–20% [4]. Estimates indicate that in 2004 tetanus caused 128,250 newborns and 30,000 maternal deaths, mainly in Africa and Asia [5]. Even though there is a great stride in the reduction of maternal and neonatal mortality through maternal and neonatal tetanus elimination initiatives, Ethiopia is among 21 countries that had not yet attained the elimination of the disease [6].
Prevention of maternal and neonatal tetanus can be achieved through simple hygienic birth-related practices and tetanus toxoid vaccination of mothers [7, 8]. This is strengthened by the evidence from a systematic review that demonstrates the TT immunization of women of childbearing age reduces the risk of neonatal tetanus [9]. Besides, a meta-analytic study shows that TT immunization of pregnant women with at least two doses (TT2) can decrease neonatal mortality due to tetanus by 94% [10]. Therefore, the World Health Organization (WHO) recommends a total of five doses of TT vaccine for women with no history of tetanus toxoid (TT) immunization. The first two doses are given in the first trimester, each within a range of 1 month, and another dose during the next pregnancy or within a 1-year interval.
Globally, 40 million pregnant mothers remained in need of immunization against maternal tetanus. The number of mothers living in high-risk areas and protected with at least two doses of TT vaccination during the 1999–2006 supplementary immunization activities was only 73 million [11]. Currently, TT2+ immunization coverage among pregnant mothers accounts for 75% worldwide ranging from 95% in South East Asia to 53% in the East Mediterranean and 63% in Africa [12].
Ethiopia has the highest maternal and neonatal tetanus morbidity and mortality rates in the world due to low TT immunization coverage. The Ethiopian Demographic and Health Survey (EDHS) report of 2011 indicated that only 48% [13] of mothers were protected against tetanus at birth [13]. Very static progress had been shown up to 2016 as evidenced by only 49% of mothers were protected at birth [14]. Despite the country’s effort of interventional policy to meet the WHO goals towards Maternal and Newborn Tetanus Elimination (MNTE) through extended immunizations and campaigning tetanus toxoid vaccinations, Ethiopia continues to have the higher tetanus morbidity and mortality rates [14].
Poor access to vaccines and lack of knowledge are primary factors for poor vaccination coverage in Bangladesh [15]. Other reasons for low coverage include lack of knowledge of time and place for TT immunization and misconceptions of vaccines as contraceptive agents [16]. Moreover, different sociodemographic factors such as antenatal care visit [17, 18], wealth index [17, 19], women’s employment [17], maternal age at delivery, maternal education [19, 20], place of residence [19, 21], multiparity [21], health care decision making, contraceptive use and husband education [19] have an association with tetanus toxoid immunization.
In Ethiopia, though the 2016 Demographic and Health Survey (EDHS) demonstrated the under-utilization of TT immunization during pregnancy [14], to date there is limited evidence on the contributing factors to this poor immunization. Furthermore, the previous studies primarily focused on the effect of individual-level factors. The neighborhood/community factors were largely overlooked. A multilevel analysis allows the simultaneous examination of within- and between-community variability in outcomes [22, 23] and of the extent to which between community variability is “explained” by individual and community-level factors. Studies using these approaches can usually provide the simultaneous effect of community characteristics and individual-level covariates on the health outcome [24, 25].
Therefore, the current study aimed to identify the individual and community level factors influencing the uptake of sufficient TT immunization among pregnant women in Ethiopia. The implication of the study was just to provide an insight to tackle the hindering factors of TT immunization in Ethiopia by providing the evidence for policymakers to enable them to strengthen currently ongoing immunization programs.
Method
Data source, study design and setting
This study utilized secondary data from the 2016 Ethiopian Demographic and Health Survey (EDHS). The data are analyzed using bivariate and multivariate multilevel logistic regression. The survey data were downloaded from the Measure DHS website after reasonable request and data use permission was fully guaranteed. The 2016 EDHS is part of the worldwide MEASURE DHS project which was funded by the United States Agency for International Development (USAID) and was implemented by the Ethiopian Central Statistical Agency. A DHS is undertaken every 5 years and the 2016 survey is the fourth Demographic and Health Survey in Ethiopia which covers all the nine regions and two administrative cities.
Sample size and sampling procedure
The Ethiopian Demographic and Health Survey program (EDHS) has collected data on national representative samples of all age groups and key indicators including tetanus toxoid immunization among pregnant women. The information on the sociodemographic, socioeconomic, and maternal-related variables was also included in the survey.
A stratified two-stage cluster sampling procedure was employed to select study participants. In the 2016 survey, a total of 645 EAs (202 urban and 443 rural) were selected. From these enumeration areas, 18,008 households and from those households a total of 15,683 reproductive-age women were included in the survey. The relevant information on the sampling procedure and data quality can be accessed elsewhere [14]. For the current study, a total of 7043 pregnant women/who gave birth in five years preceding the survey were included (Fig. 1). The sampling weight was applied during the analysis to produce reliable estimates.
Dependent variable
The dependent variable is defined as whether or not women received sufficient TT immunizations during their last pregnancy. A woman is considered to have sufficient TT if her immunization status corresponds to the WHO guidelines for the appropriate interval for protection at birth (PAB). According to this guideline, sufficient TT immunization is operationalized as receiving two or more doses during current pregnancy; or one dose during current pregnancy and at least one dose during before current pregnancy; or at least two TT doses before the current pregnancy of which the last dose was < 3 years before the birth; or three doses within the 5 years before the current pregnancy; or four doses with the last dose < 10 years before the pregnancy or receiving five doses or more before the current pregnancy [6]. Therefore, for the current study pregnant women who uptake two and above tetanus toxoid vaccine were considered as sufficiently immunized otherwise poorly immunized.
Independent variables
From the 2016 EDHS dataset educational status of mother (no formal education, primary, secondary, higher) and husband (no formal education primary, secondary, higher), maternal age (15–20, > 20), maternal employment (not working, working), parity (primipara, multipara, grand multipara), wealth status (poor, middle, rich), the nature of pregnancy (wanted then, wanted later, no more wanted), antenatal care (ANC) visit (no visit, 2–3 visits, ≥4 visits), health care decision making (self, husband), health insurance (no, yes), perception of distance from the health facility (big problem, not a big problem), place of delivery (home, health facility), iron supplementation (yes, no), and media exposure (no, yes) were considered as individual-level variables.
The aggregate community level explanatory variables (community poverty level, community media exposure level, community illiteracy level, and community ANC utilization) were constructed by aggregating individual-level characteristics at the community (cluster) level. They were dichotomized as high or low based on the distribution of the proportion values computed for each community after checking the distribution by using the histogram. If the aggregate variable was normally distributed mean value and if not, normally distributed median value was used as a cut-off point for the categorization.
Multilevel logistic regression analysis
Data Extraction, recoding, and both descriptive and analytical analysis were carried out using STATA version 14 software. Weighting was done to restore the representativeness of the sample so that the total sample looks like the country’s actual population. Descriptive analysis was conducted using cross-tabulation. As a result, frequencies and percentages were reported. The multilevel analysis was fitted due to the hierarchical nature of the demographic health survey data.
Consequently, four models were fitted. The first was the null model containing no exposure variables which was used to check variation in community and provide evidence to assess random effects at the community level. This model was used to assess the applicability of multi-level analysis by checking the random effects. The second model was the multivariable model adjustment for individual-level variables and model three was adjusted for community-level factors. In the fourth model, both individual and community-level variables were fitted with the outcome variable simultaneously. The regression equation is given as follows [26];
Where;
-
πij is the probability of having poor TT uptake
-
(1-πij) is the probability of good TT uptake
-
βo is log odds of the intercept
-
β1, ... βn are effect sizes of individual and community-level factors
-
x1ij... xnij are independent variables of individuals and communities
-
The quantities uoj and eij are random errors at cluster levels and individual levels respectively.
The odds ratio was used to estimate the association between the likelihood of poor TT immunization and explanatory variables at both community and individual levels and were expressed as odds ratios with a 95% confidence interval. Regarding the measures of variation (random-effects) intracluster correlation coefficient (ICC) and Proportional Change in Community Variance (PCV) were used.
Results
Sociodemographic characteristics of study participants
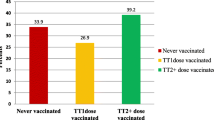
In this study, a total of 7043 pregnant women were included. Nearly two-thirds (66%) of study subjects had no formal education. The majority (70%) of respondents were unemployed and nearly half (50.39%)of them were poor. Regarding the place of delivery, about two-third (63%) of the participants were delivered at home. Moreover, 35.08 and 55% of participants did not receive ANC service and iron supplementation respectively. Most (96.54%) of respondents were not covered by health insurance had about 61% of respondents had no media exposure. Regarding the perception of distance to the health facility, nearly half (52%) of respondents perceived distance from the health facility as a big problem (Table 1).
Regarding the community-level characteristics, the majority (79.24%) of participants were from rural communities and 47.88% of them were from communities with high illiteracy levels. Looking at community ANC utilization, nearly half (50.49%) of study subjects were from communities with high ANC utilization (Table 1).
Random effect and model comparison
In the null model, variance component analysis was performed to decompose the total variance of poor TT immunization. The community-level variance which indicates the total variance of poor TT immunization that can be attributed to the context of the community in which the women were living was estimated. The applicability of multi-level analysis was justified by the significance of the community-level variance [community variance = 1.14; standard error (SE) = 0.11; P-value = 0.001], indicating the existence of significant differences between communities regarding poor TT vaccine utilization. This was further supported by the ICC in the null model which showed that about 26% of the variation of poor TT immunization among pregnant women was attributed to the difference at community-level factors. Besides, the higher PCV value (65%) in the final model indicates that about 65% of the variation of poor TT immunization among pregnant women was attributable to both the individual level and community-level factors. Regarding model comparison, we used deviance to assess model fitness. Consequently, the model with the lowest deviance value (Model IV) was found to be the best-fitted model (Table 2).
Factors associated with poor TT immunization
In the multilevel logistic regression analysis (model IV), antenatal care visit, iron supplementation, media exposure, maternal occupation, and wealth index were significantly associated with poor TT immunization. Regarding the community-level factors, place of residence and community illiteracy level had a significant association with poor TT immunization (p < 0.05).
The odds of poor TT immunization among pregnant women with no ANC visit and those who had one to three visits was 5.64[Adjusted odds ratio (AOR) = 5.64; 95% CI:2.48,7.30] and 1.50 (AOR = 1.49; 95% CI: 1.19–1.82) respectively times higher as compared to women who had more than three ANC visits. Looking to wealth status pregnant women from poor households had 26% (AOR) = 1.26; 95% CI: 1.03, 1.54) increased odds of poor TT immunization as compared to women from rich households. The odds of poor TT immunization was 41% (AOR = 0.77; 95% CI: 0.51, 0.68) lower among pregnant women who had received iron during pregnancy as compared to their counterparts. The odd of having poor TT immunization was 1.29 (AOR = 1.29; 95% CI: 1.10, 1.51) times higher among women who were exposed to media as compared to women who weren’t exposed to media. The likelihood of having poor TT immunization was 1.15 (AOR = 1.15; 95% CI: 1.10, 1.31) times higher among unemployed women as compared to their counterparts.
Regarding the place of residence, the odds of poor TT immunization among women from rural communities was 1.13 (AOR = 1.13; 95% CI: 1.08, 1.72) times higher as compared to women who live in urban communities. Moreover, pregnant women from communities with higher illiteracy had 28% (AOR = 1.28; 95% CI: 1.03, 1.58) higher odds of poor TT immunization as compared to their counterparts (Table 2).
Discussion
This study examined the association between several demographic, socioeconomic, and health care access-related factors with poor tetanus toxoid (TT) immunization during pregnancy.
Although the proportion of pregnant women receiving 4 or more antenatal care (ANC) visits has no necessary relationship with the actual tetanus toxoid vaccine uptake, it is used prominently as a global benchmark indicator to track maternal health program performance [27]. Thus, the odds of poor TT immunization among pregnant women who didn’t have antenatal care visit was strongly higher than those who have at least four visits. This result is similar to findings in other studies [17, 18]. Thus, strategies aimed at improving antenatal care attendance among pregnant women would be a step in the right direction towards increasing TT immunization. Likewise, antenatal care providers should encourage women and provide information about the importance of getting immunized since ANC follow-up provides an opportunity to convey such a critical message to pregnant women so as to increase TT uptake.
Although global poverty has fallen dramatically over the past decades, it has still pronouncing effect on inequality in health service utilization especially in developing countries [28]. The asset indices are used as diagnostic tools for private household wealth and basic public goods access for better health service utilization [29]. Thus the current study highlighted the effect of the household wealth index on the uptake of the TT vaccine. Therefore, women from households with poor household wealth index had higher odds of poor TT immunization as compared to those from rich households. This is supported by the finding in Bangladesh [19]. This might be because the economic status is one of the prominent determinants of maternal healthcare-seeking behavior [30,31,32] possibly this will lead to low maternal health service utilization including immunization for those women from poor households. Moreover, the availability of free or subsidized services is known to improve the uptake of maternal services among the poor [32, 33].
Similarly, the likelihood of poor tetanus toxoid immunization was higher among unemployed mothers as compared to their counterparts. This finding is consistent with the finding in Bangladesh [19]. The possible justification could be an employed woman might involve in social communication which could create a context for learning and engagement in health-related dialogues, particularly during pregnancy. As a result, the workplace might operate as social support and motivational venue enhancing the utilization of health care services. Besides, The previous evidence indicates that formal employment is associated with a range of social outcomes and behaviors that are typically associated with higher levels of social development [34].
Consistent with studies in Eastern Ethiopia [21] and Bangladesh [19] the current study identified that the odds of TT vaccine uptake was lower among rural women as compared to those from urban communities. In the rural communities, most of the time TT immunization was provided through outreach and there is a lack of awareness among women to continue taking the doses even after delivery especially in remote areas of Ethiopia [35]. This is further supported by the evidence in the current study where more than half of participants perceived the distance from health facilities as a big problem (Table 1).
Though it doesn’t show a significant effect on TT immunization in India [36], media exposure is another important factor associated with tetanus toxoid utilization among pregnant women in the current study. Thus, the likelihood of poor TT immunization among non-exposed mothers was higher as compared to those who are exposed to media. The health service-related messages including immunization are commonly conveyed through media by the ministry of health and other stakeholders which builds their knowledge of TT immunization. Since knowledge of TT immunization is an important determinant of TT vaccine uptake in Ethiopia [20], those women who weren’t exposed to media may miss this opportunity.
The particular interest in this study is the effect of iron supplementation on tetanus toxoid vaccine utilization. This study indicated that the odds of poor TT immunization was lower in those mothers who were supplemented with an iron tablet during pregnancy as compared to their counterparts. Iron supplementation was a routine service during pregnancy like the TT vaccine in Ethiopia. Therefore, those mothers who received iron could have a high probability of getting TT immunization.
Moreover, in our study higher community illiteracy level was another important factor that was associated with higher odds of having poor TT immunization. Another study also revealed that maternal health service utilization is associated with literacy level in the community in which mothers from communities with higher illiteracy levels had a lower chance of utilizing maternal health services [37].
In general maternal and neonatal tetanus is considered to be a public health problem in Subsaharan Africa. Interventions to improve vaccination outcomes are commonly grouped into those targeting health services delivery such as improving human resources training, logistics, cold chain maintenance, and vaccine storage, effective financing, monitoring and evaluation, and supportive supervision. The most recent review considered shows that much remains to be done to improve immunization coverage among women in Subsaharan Africa [38]. Besides, identifying potential hindering factors of TT uptake is vital for policymakers. Thus, the findings in this study could have positive implications to improve the coverage of TT immunization among pregnant women and then reduce related maternal and neonatal adverse outcomes in Ethiopia.
The main strength of this study was the use of nationally representative data which will provide good evidence for policymakers at the national level. The other strength is the use of an appropriate model (multilevel) for analyzing the data. However, this study is not free of limitations. First, the cross-sectional nature of the study leads to difficulty to show the temporal relationship between the factors and the outcome. Second, immunization status was primarily collected through self-report making it susceptible to recall bias. Besides, variables such as lack of knowledge on the immunization schedule, the attitude of women towards TT immunization, level of community mobilization interventions, and other health care provider-related factors were not assessed owing to the secondary data analysis.
Conclusion
In this study, both individual and community-level factors were associated with poor TT immunization among pregnant women. Accordingly, antenatal care (ANC) visits, media exposure, employment, place of residence, iron supplementation, and community illiteracy had a significant statistical association with poor TT immunization.
Therefore, focusing on antenatal care services especially encouraging pregnant women to have at least four visits, consulting women to be exposed to media, improving community literacy and maternal employment will help to minimize poor TT immunization. Besides, this study particularly focused on pregnant women. Thus it provides new evidence about the influence of socioeconomic factors on inequalities in the maternal health sector. This has implications for secondary policy priorities, such as the need to address uneven fertility transitions in sub-Saharan Africa and their wider interaction with poverty reduction efforts at the individual and community-level in developing countries [39].
Availability of data and materials
All relevant data are available within the manuscript.
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odds Ratio
- CSA:
-
Central Statistical Agency
- EAs:
-
Enumeration Areas
- EDHS:
-
Ethiopia Demographic and Health Survey
- MNTE:
-
Maternal and Neonatal Tetanus Elimination
- SNNP:
-
South Nation Nationality and People
- TT:
-
Tetanus Toxoid
- WHO:
-
World Health Organization
References
Cook T, Protheroe R, Handel J. Tetanus: a review of the literature. Br J Anaesth. 2001;87(3):477–87.
Sheffield JS, Ramin SM. Tetanus in pregnancy. Am J Perinatol. 2004;21(04):173–82.
Khan R, Vandelaer J, Yakubu A, Raza AA, Zulu F. Maternal and neonatal tetanus elimination: from protecting women and newborns to protecting all. Int J Womens Health. 2015;7:171.
Organization WH. Tetanus vaccines: WHO position paper–February 2017. Wkly Epidemiol Rec. 2017;92(6):53–76.
Zarocostas J. Unicef aims to eliminate tetanus in mothers and babies by 2012. BMJ (Online). 2008;337.
Organization WH. Protecting all against tetanus: guide to sustaining maternal and neonatal tetanus elimination (MNTE) and broadening tetanus protection for all populations. 2019.
Blencowe H, Cousens S, Mullany LC, Lee AC, Kerber K, Wall S, et al. Clean birth and postnatal care practices to reduce neonatal deaths from sepsis and tetanus: a systematic review and Delphi estimation of mortality effect. BMC Public Health. 2011;11(S3):S11.
Organization WH. Health topics: tetanus. Geneva: WHO; 2011.
Demicheli V, Barale A, Rivetti A. Vaccines for women for preventing neonatal tetanus. Cochrane Database Syst Rev. 2015;7.
Blencowe H, Lawn J, Vandelaer J, Roper M, Cousens S. Tetanus toxoid immunization to reduce mortality from neonatal tetanus. Int J Epidemiol. 2010;39(suppl_1):i102–i9.
Organization WH. State of the World's vaccines and immunization: World Health Organization; 2009.
Organization WH. WHO vaccine preventable diseases: monitoring system: 2005 global summary. Geneva: World Health Organization; 2005. WHO publication WHO/IVB/2010 R296–349 http://apps who int/iris/bitstream/10665/70535/1/WHO_IVB_2010_eng pdf Accessed. 2015;22
CSACEaI. Ethiopia Demographic and Health Survey 2011. Addis Ababaand Rockville: CSA and ICF; 2011.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey. Addis Ababa and Rockville: CSA and ICF; 2016.
Perry H, Perry H, Weierbach R, El-Arifeen S, Hossain I. A comprehensive assessment of the quality of immunization services in one major area of Dhaka City, Bangladesh. Tropical Med Int Health. 1998;3(12):981–92.
Hasnain S, Sheikh N. Causes of low tetanus toxoid vaccination coverage in pregnant women in Lahore district, Pakistan. EMHJ. 2007;13(5):1142–52.
Haile ZT, Chertok IRA, Teweldeberhan AK. Determinants of utilization of sufficient tetanus toxoid immunization during pregnancy: evidence from the Kenya demographic and health survey, 2008–2009. J Community Health. 2013;38(3):492–9.
Roosihermiatie B, Nishiyama M, Nakae K. Factors associated with TT (tetanus toxoid) immunization among pregnant women, in Saparua, Maluku, Indonesia. Southeast Asian J Trop Med Public Health. 2000;31(1):91–5.
Rahman M. Tetanus toxoid vaccination coverage and differential between urban and rural areas of Bangladesh. East Afr J Public Health. 2009;6(1).
Facha W, Yohannes B, Duressa G. Tetanus toxoid vaccination coverage and associated factors among pregnant women in Duguna Fango District, Southern Ethiopia. Int J Health Sci Res. 2018;8(1):148–54.
Gebremedhin TS, Welay FT, Mengesha MB, Assefa NE, Werid WM. Tetanus toxoid vaccination uptake and associated factors among mothers who gave birth in the last 12 months in Errer District, Somali regional state, Eastern Ethiopia. Biomed Res Int. 2020;2020.
Bullen N, Jones K, Duncan C. Modelling complexity: analysing between-individual and between-place variation—a multilevel tutorial. Environ Plan A. 1997;29(4):585–609.
Snijders TA, Bosker RJ. Modeled variance in two-level models. Sociol Methods Res. 1994;22(3):342–63.
Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–9.
Ellen IG, Mijanovich T, Dillman K-N. Neighborhood effects on health: exploring the links and assessing the evidence. J Urban Aff. 2001;23(3–4):391–408.
Snijders TA, Bosker RJ. Multilevel analysis: an introduction to basic and advanced multilevel modeling: sage; 2011.
Hodgins S, D'Agostino A. The quality–coverage gap in antenatal care: toward better measurement of effective coverage. Glob Health Sci Pract. 2014;2(2):173–81.
Wietzke FB. Poverty, inequality, and fertility: the contribution of demographic change to global poverty reduction. Popul Dev Rev. 2020;46(1):65–99.
Wietzke FB. Who is poorest? An asset-based analysis of multidimensional wellbeing. Dev Policy Rev. 2015;33(1):33–59.
Amin R, Shah NM, Becker S. Socioeconomic factors differentiating maternal and child health-seeking behavior in rural Bangladesh: a cross-sectional analysis. Int J Equity Health. 2010;9(1):9.
Islam MR, Odland JO. Determinants of antenatal and postnatal care visits among indigenous people in Bangladesh: a study of the Mru community; 2011.
Simkhada B. Teijlingen ERv, porter M, Simkhada P. factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008;61(3):244–60.
Zafar AA, Ehiri JE, Anyanwu EC. Use of antenatal services in Kampung District, Cambodia. Sci World J. 2003;3:1081–92.
Wietzke F-B. Pathways from jobs to social cohesion. World Bank Res Obs. 2015;30(1):95–123.
Kidane T, Yigzaw A, Sahilemariam Y, Bulto T, Mengistu H, Belay T, et al. National EPI coverage survey report in Ethiopia, 2006. Ethiop J Health Dev. 2008;22(2):148–57.
Thind A. Determinants of tetanus toxoid immunization in pregnancy in rural Bihar. Trop Dr. 2005;35(2):75–7.
Singh PK, Kumar C, Rai RK, Singh L. Factors associated with maternal healthcare services utilization in nine high focus states in India: a multilevel analysis based on 14 385 communities in 292 districts. Health Policy Plan. 2014;29(5):542–59.
Vouking MZ, Tadenfok CN, JME E. Strategies to increase immunization coverage of tetanus vaccine among women in Sub Saharan Africa: a systematic review. Afr Med J. 2017;27(Suppl 3).
Bongaarts J, Casterline J. Fertility transition: is sub-Saharan Africa different? Popul Dev Rev. 2013;38(Suppl 1):153.
Acknowledgments
The authors would like to thank measure DHS for their permission to access theEDHS datasets.
Authors’contributions
AML and HGA are involved in the design and conception of the study, data analysis, interpretation and write-up of the manuscript. Both the authors read and approved the final manuscript.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was approved by an Institutional ethical Review committee of the Institute of Public Health, College of Medicine and Health Sciences, University of Gondar. The approval letter for the use of the EDHS data set was also gained from the Measure DHS (ORC MACRO). No information obtained from the data set was disclosed to any third person.
Consent for publication
Not applicable.
Competing interests
Both authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liyew, A.M., Ayalew, H.G. Individual and community-level determinants of poor tetanus toxoid immunization among pregnant women in Ethiopia using data from 2016 Ethiopian demographic and health survey; multilevel analysis. Arch Public Health 79, 92 (2021). https://doi.org/10.1186/s13690-021-00622-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-021-00622-3