Abstract
Objective
Acute ischemic stroke (AIS) is a significant health burden in China, affecting a sizable portion of the population. Conventional pharmacological treatments frequently fall short of desirable outcomes. Therefore, exploring alternative therapies is crucial. Remote ischemic postconditioning (RIPostC) is a noninvasive and cost-effective adjunctive therapy. This study aimed to investigate the efficacy and safety of RIPostC as an adjunctive therapy for AIS to inform clinical practice.
Methods
A comprehensive search was conducted across the PubMed, Embase, Web of Science, China National Knowledge Infrastructure (CNKI), WanFang, Weipu (VIP), and China Biology Medicine disc (CBM) databases up to October 2023. All included studies underwent bias risk assessment using the Cochrane risk-of-bias assessment tool. The primary outcome measure was the National Institute of Health Stroke Scale (NIHSS), with secondary outcomes including the Barthel index (BI), D-dimer, C-reactive protein (CRP), fibrinogen (FIB), brain-derived neurotrophic factor (BDNF), modified Rankin scale (mRS), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α) levels. The data were analyzed using fixed-effects and random-effects models in Review Manager, with mean differences (MDs) and 95% confidence intervals (CIs) calculated for each outcome. The grading of recommendations, assessment, development, and evaluations (GRADE) approach was used to evaluate the level of evidence for each outcome measure.
Results
This meta-analysis included 38 studies, encompassing 4334 patients. Compared with the control group, the RIPostC group had significantly lower NIHSS scores, serum CRP, D-dimer, IL-6, TNF-α, and FIB levels, and increased BDNF levels. Moreover, it improved the patient’s BI and mRS scores. According to the GRADE approach, the quality of evidence for mRS was deemed “moderate,” while the NIHSS, BI, and CRP were rated as “low” quality. IL-6, TNF-α, FIB, D-dimer, and BDNF received “very low” quality ratings.
Conclusion
The findings suggest that RIPostC activates endogenous protective mechanisms, providing benefits to patients with AIS.
Similar content being viewed by others
Introduction
Stroke is a significant neurological disorder characterized by high incidences of disability and mortality, ranking as the fifth leading cause of death in the United States and the primary cause in China [1,2,3]. Ischemic stroke, constituting approximately 70% of stroke cases in China [4], has a complex pathogenesis. Pathologies such as atherosclerosis and thrombosis in cerebral arteries may induce vascular spasms, stenosis, or occlusion, resulting in softening and necrosis of brain tissue and neurological deficits [5, 6]. Although intravenous thrombolysis is the primary treatment for acute cerebral infarction, its efficacy is limited by a narrow therapeutic window and contraindications associated with thrombolytic medications. Consequently, a considerable number of patients experience fatal outcomes or severe disabilities, significantly impacting their quality of life [4, 7]. Therefore, identifying effective strategies to counteract pathological alterations at the ischemic site and enhance recovery and quality of life is imperative. With the limited availability of exogenous methods to promote recovery from cerebral ischemia, exploring endogenous mechanisms for rehabilitation has become a focal point of interest.
Remote ischemic postconditioning (RIPostC) is an innovative and straightforward approach for safeguarding ischemic brain tissue. Its principle involves inducing brief, nonfatal ischemic episodes in noncritical organs following a life-threatening ischemic event in vital organs. This process triggers innate ischemic tolerance mechanisms, protecting the ischemic and damaged brain tissue [8]. RIPostC activates these endogenous protective mechanisms by subjecting specific organs or tissues to recurrent episodes of ischemia and reperfusion, which are insufficient to cause irreversible organ or tissue damage. However, these transient episodes stimulate the body’s internal protective response through RIPostC [9]. The precise mechanisms through which RIPostC exerts its protective effects are poorly understood; they are conventionally divided into fluid and immune-inflammatory regulatory mechanisms, with some interactions between them.
Regarding humoral regulation mechanisms, emerging research suggests that ischemic events prompt the body or tissues to produce anti-ischemic compounds or soluble substances, such as nitric oxide, adenosine, bradykinin, and vascular endothelial growth factor. These substances circulate in the bloodstream upon reperfusion, delivering bodily protective benefits. Moreover, RIPostC can stimulate local vascular endothelial cells to release cell vesicles containing proteins or microRNAs (miRNAs), which travel to the brain and modulate cellular activity, exerting a neuroprotective effect [10, 11].
Concerning immune-inflammatory regulatory mechanisms, both preclinical and clinical studies have indicated that RIPostC can inhibit proinflammatory responses, promote the transcription of anti-inflammatory and antiapoptotic genes, alleviate immune-inflammatory responses, and regulate peripheral immune cells, such as CD3+CD8+ T cells, B cells, CD3+/CD161a+ NKT cells, and anti-inflammatory CD43+/CD172a+ monocytes. Furthermore, it can adjust TNF-α and IL-6 levels to provide neuroprotection [12,13,14].
The primary evidence supporting the neuroprotective effects of RIPostC comes from animal studies, highlighting the involvement of various endogenous factors, including regulatory T cells, heat shock protein 70 (Hsp70), miRNAs, neuronal nitric oxide synthase, and brain-derived neurotrophic factor (BDNF) [15,16,17,18,19,20]. Clinical trials further support the potential of RIPostC to enhance recovery in patients with stroke, as evidenced by improved NIHSS scores, reduced high-sensitivity (hs)-CRP levels, diminished brain tissue infarct volume, and enhanced cognitive function post-stroke [21,22,23,24,25]. Theoretically, remote ischemic conditioning holds promise for facilitating disease recovery. However, the outcomes of a high-quality randomized controlled trial suggest that remote ischemic preconditioning may not significantly influence disease progression or recovery following acute ischemic stroke (AIS) [26]. Four systematic reviews and meta-analyses concerning RIPostC’s use in treating AIS have been examined; two focused on animal studies, potentially offering significant insights for researchers. The remaining two analyses pertained to clinical trials. However, these studies have relatively narrow outcome indicators, limiting a comprehensive understanding of RIPostC’s endogenous protective mechanisms. Consequently, this study was initiated to comprehensively assess the potential benefits of RIPostC in rehabilitating patients who have experienced AIS, incorporating a broader array of original research and outcome measures.
Methods
Systematic review protocol and registration
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [27] and is registered with the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42021261145).
Search strategy
A comprehensive search was implemented in PubMed, Embase, Web of Science, China National Knowledge Infrastructure (CNKI), WanFang, Weipu (VIP), and China Biology Medicine disc (CBM) databases, extending the search timeframe up to April 2024. Keywords used in the search encompassed stroke, ischemic stroke, cerebral infarction, acute ischemic stroke, RIPostC, remote ischemic postconditioning, and randomized controlled trials, among others. The search strategy combined electronic database searches with manual efforts to ensure a thorough literature collection. The Additional file 1 details the search strategies (see Additional file 1).
Eligibility criteria
Inclusion criteria were as follows:
-
1)
Diagnosis of AIS with significant symptoms, including unilateral facial or limb numbness, facial asymmetry, blurred vision, impaired visual rotation, balance issues, altered consciousness, convulsions, speech difficulties, hemiplegia, hemianopia, and hemisensory disorders
-
2)
2) Head CT or MRI confirming the absence of cerebral hemorrhage
-
3)
Patients aged between 18 and 90 years
-
4)
Inclusion of the National Institute of Health Stroke Scale (NIHSS) among outcome indicators
-
5)
Approval from the ethics committee of the conducting hospital
-
6)
Utilization of a randomized controlled trial design
-
7)
Comparison between a control group receiving intravenous thrombolysis or conventional drug therapy and an experimental group undergoing RIPostC alongside intravenous thrombolysis or conventional drug therapy
-
8)
Research studies conducted in China
Exclusion criteria encompassed the following:
-
1)
Duplicate entries, animal studies, review articles, conference abstracts, and case reports
-
2)
Studies not aligning with the diagnosis of acute ischemic stroke, including transient ischemic attacks
-
3)
Studies with incomplete outcome data that could not be extracted
-
4)
Studies with intervention times and outcome indicators unsuitable for subgroup analysis with other studies
-
5)
Inaccessibility of full texts
-
6)
Outcome indicators not presented as mean ± standard deviation
-
7)
Use of additional intervention measures alongside RIPostC and drug therapy
-
8)
Studies conducted outside of China.
-
9)
Non-randomized controlled trials (RCT)
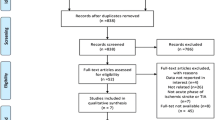
Study selection and data extraction
Two researchers (M. Y. and J. W.) independently screened records for eligibility. After removing 125 duplicate records from the initial 457 retrieved records, 55 reviews and 68 animal experiments were excluded based on title and abstract. Full-text retrievals were attempted for the remaining records; however, nine were inaccessible. Full texts were reviewed for the remaining records, excluding 2 non-randomized studies, 1 non-RCT study, 132 studies not meeting the inclusion and exclusion criteria, and 25 studies with continuous variables not presented as mean ± standard deviation. Two records were excluded due to the inability to merge and analyze with any study at the intervention time point; the remaining 38 records met study requirements and were included. Disagreements were resolved by consulting a third reviewer (Q. C.), although the two researchers reached a unanimous agreement. Data extraction included first author, publication year, study design, participant demographics, interventions, control actions, duration of intervention, outcome measures, and adverse effects, with continuous data recorded as mean ± standard deviation in Excel sheets. The study screening methodology is illustrated in Fig. 1. The data extraction process is provided in the Additional files 2–5 (see Additional files 2–5).
Statistical analysis
Statistical analyses were performed using Review Manager 5.3 (provided by the Cochrane Collaboration, Copenhagen, Denmark). The impact of RIPostC on continuous outcomes was assessed by calculating mean differences (MDs) with 95% confidence intervals (CI). The meta-analyses employed Mantel–Haenszel fixed-effects models in instances devoid of significant statistical heterogeneity among the studies. A significance threshold of 5% was maintained throughout the research. Heterogeneity among the studies was assessed using Cochran’s Q test and I2 methods. Acceptable homogeneity was defined as P > 0.1 and I2 < 50%, warranting a fixed-effects model; conversely, heterogeneity was assumed, prompting analysis via a random-effects model. The source of heterogeneity was explored through sensitivity analysis and subgroup examination.
Target outcome indicators
The primary outcome measure was the National Institute of Health Stroke Scale (NIHSS), with additional outcome measures including the Barthel index (BI), D-dimer (D-D), C-reactive protein (CRP), fibrinogen (FIB), BDNF, modified Rankin scale (mRS), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α).
Results
Study collection and characteristics
A total of 457 studies were retrieved, and after following the screening process, 38 randomized controlled trials [4, 28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64] conducted in China were selected for this meta-analysis. These studies, published between 2012 and 2023, involved 4324 participants, with 2166 in the control group and 2158 in the experimental group. All included studies were categorized based on the duration of RIPostC implementation to enhance the reliability of our data analysis. This categorization included a 3-day group with 3 studies [59,60,61], a 7-day group comprising 9 studies [29, 35,36,37, 41, 42, 47, 58, 64], a 10-day group with 3 studies [44,45,46], a 14-day group consisting of 15 studies [4, 28, 31, 40, 48,49,50,51,52,53, 55,56,57, 60, 61], a 3-month group with 2 studies [30, 38], and a 6-month group encompassing 6 studies [32,33,34, 39, 43, 54]. Detailed information and characteristics of the studies are listed in Tables 1 and 2.
Outcome measurements
The National Institutes of Health Stroke Scale (NIHSS)
All included studies reported NIHSS scores. For a thorough meta-analysis, these studies were categorized based on the NIHSS measurement timelines: 3-day, 7-day, 10-day, 14-day, and 6-month groups. A higher NIHSS score indicates more severe nerve damage in the patient, while a lower score indicates better recovery of damaged nerves.
3-day group
This group comprised 710 participants [59,60,61], with 355 each in the experimental and control groups. The outcomes at 14-day post-treatment were collectively reported; hence, the analysis focused on these results. The meta-analysis showed that RIPostC significantly lowered NIHSS scores compared to the control group, employing a random-effects model (MD: −2.70; 95% CI: −4.95, −0.81; P = 0.005). However, substantial heterogeneity across these trials was observed (χ2 = 123.94; I2 = 98%; P < 0.00001; Fig. 2).
7-day group
This cohort included 349 participants in the experimental group and 341 in the control group, with outcomes reported on both the 7th day (across 6 studies [29, 36, 37, 41, 42, 47]) and the 14th day (across four studies [29, 35, 58, 64]) of treatment. The meta-analysis indicated a significant reduction in NIHSS scores by RIPostC on the 7th day compared to the control group, as determined through a random-effects model (MD: −2.04; 95% CI: −3.64, −0.45; P = 0.01; Fig. 3A). Significant heterogeneity was observed among the included trials. A subsequent sensitivity analysis revealed that the study by Zhou et al. [47] significantly influenced this heterogeneity. Upon its exclusion, heterogeneity was no longer present (MD: −1.33; 95% CI: −1.96, −0.71; P < 0.0001; Fig. 3B). Similarly, by the 14th-day post-treatment, RIPostC was found to reduce the NIHSS scores compared to the control group (MD: −0.76; 95% CI: −1.83, 0.31; P = 0.16; Fig. 3C).
10-day group
This group comprised 100 participants in the experimental group and 100 in the control group, with results reported on the 10th day of treatment [44, 46]. Compared to the control group, the experimental group exhibited a significant reduction in NIHSS scores, as depicted in Fig. 4, using a fixed-effects model (MD: −2.56; 95% CI: −3.02, −2.10; P < 0.00001).
14-day group
This group comprised 15 studies, with 938 participants in the experimental group and 937 in the control group. Twelve studies [4, 28, 31, 39, 48, 49, 52, 55,56,57, 60, 61] reported results on day 14 using a random-effects model (MD: −2.23; 95% CI: −3.20, −1.25; P < 0.00001; Fig. 5A). Three studies [40, 48, 52] reported results 1-month post-treatment using a fixed-effects model (MD: −1.40; 95% CI: −1.81, −0.99; P < 0.00001; Fig. 5B). Furthermore, five studies [40, 48, 49, 52, 53] reported 3-month posttreatment outcomes via a fixed-effects model (MD: −1.56; 95% CI: −1.92, −1.20; P < 0.00001; Fig. 5C). Across all three datasets, RIPostC significantly reduced the NIHSS scores compared to the control group.
6-month group
This group comprised 6 studies with 743 participants, reporting results at 1-month and 6-month post-treatment. At the 1-month mark [34, 43, 54], a meta-analysis using a random-effects model indicated that the RIPostC group outperformed the control group in reducing NIHSS scores (MD: −1.39; 95% CI: −2.27, −0.52; P < 0.002; Fig. 6A). In the 6th month [32,33,34, 39, 43, 54], NIHSS scores in the RIPostC group were significantly lower than those in the control group, as determined by a random-effects model (MD: −2.78; 95% CI: −4.05, −1.50; P < 0.0001; Fig. 6B).
Barthel index (BI)
For the BI, only data from the 7-day and 14-day groups were suitable for meta-analysis. The 7-day group provided outcomes on the 7th and 14th days of treatment. However, the 14-day group reported results on the 14th-, 30th-, and 90th-day post-treatment. According to Fig. 7, RIPostC significantly enhanced the patients’ BI scores compared to the control group. The BI measures the patient’s ability to engage in daily activities, with a higher score indicating more substantial independence in activities, reflecting the patient’s recovery situation.
In the 7-day group on the 7th day [29, 37, 42], the analysis showed a significant improvement (MD: 11.01; 95% CI: 7.16, 14.86; P < 0.00001; heterogeneity: χ2 = 1.58; I2 = 0%; P = 0.45; Fig. 7A).
On the 14th day [29, 35, 64], a considerable improvement was observed (MD: 8.55; 95% CI: 2.95, 14.14; P = 0.003; heterogeneity: χ2 =5.30; I2 = 62%; P = 0.07; Fig. 7B).
The 14-day group on the 14th day [4, 40, 48] experienced varied results (MD: 7.85; 95% CI: −3.47, 19.17; P = 0.17; heterogeneity: χ2 =63.69; I2 = 97%; P < 0.00001; Fig. 7C).
On the 30th day [40, 48], a slight improvement was observed (MD: 3.06; 95% CI:0.26, 5.86; P = 0.03; heterogeneity: χ2 = 0.02; I2 = 0%; P = 0.90; Fig. 7D).
By the 90th day [31, 40, 45, 53], an improvement was still evident (MD: 4.73; 95% CI:1.92, 7.55; P = 0.001; heterogeneity: χ2 = 6.61; I2 = 55%; P = 0.09; Fig. 7E).
Modified Rankin Scale (mRS)
For the mRS outcome metric, reports were exclusively provided by the 7-day and 14-day groups, covering treatments over 7 days and 90 days, and for the 14-day group, an additional report at 90-day post-treatment. These datasets exhibited no heterogeneity, affirming the meta-analysis results as highly dependable. Consequently, fixed-effects models were applied across the board, demonstrating that RIPostC effectively enhanced mRS scores in patients when compared to the control group. The mRS is used to evaluate the prognosis of various types of patients with stroke and to determine the efficacy of functional disability levels in rehabilitation patients. A lower score indicates a better prognosis and recovery.
In the 7-day group at 7 days [37, 41], the analysis indicated a marginal improvement (MD: −0.21; 95% CI: −0.48, 0.06; P = 0.14; with zero heterogeneity: χ2 = 0.00; I2 = 0%; P = 0.14; Fig. 8A).
In the 7-day group at 90 days [37, 58], a significant enhancement was observed (MD: −0.46; 95% CI: −0.69, −0.23; P < 0.0001; with negligible heterogeneity: χ2 = 0.09; I2 = 0%; P = 0.77; Fig. 8B).
In the 14-day group at 90 days [31, 50, 52, 53], a considerable improvement was also recorded (MD: −0.54; 95% CI: −0.68, −0.39; P < 0.00001; with minimal heterogeneity: χ2 = 0.68; I2 = 0%; P = 0.88; Fig. 8C).
Interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α)
The 14-day group provided IL-6 (ng/L) levels on the 14th day of treatment, while the 6-month group reported both IL-6 and TNF-α (ng/L) levels in the first month of treatment. Despite substantial heterogeneity among these datasets, analyses using a random-effects model indicated that RIPostC significantly impacted these biomarkers favorably compared to the control group. IL-6 and TNF-α are both serum inflammatory factors, and their presence indicates inflammation. Lower levels suggest a milder inflammatory response in the patient’s body. Given the rapid inflammatory response post-stroke, the gradual decrease in inflammatory activity with treatment and time indicates stroke recovery.
At the 14-day mark for the 14-day group [50, 56], IL-6 levels considerably decreased (MD: −5.40; 95% CI: −11.91, 1.11; P = 0.10; heterogeneity: χ2 = 8.96; I2 = 89%; P = 0.003; Fig. 9A).
At the 30-day mark for the 6-month group [34, 54], IL-6 levels significantly reduced (MD: −16.19; 95% CI: −19.91, −12.47; P < 0.00001; heterogeneity: χ2 = 3.22; I2 = 69%; P = 0.07; Fig. 9B).
For TNF-α at the 30-day mark [34, 54], significant changes were not observed (MD: 1.97; 95% CI: −32.10, 36.03; P = 0.91; heterogeneity: χ2 = 145.95; I2 = 99%; P < 0.00001; Fig. 9C).
C-reactive protein (CRP), fibrinogen (FIB), and D-dimer (D-D) levels
CRP (pg/L) levels reported by the 6-month group at 1 month showed significant improvement [34, 54] (MD: −20.05; 95% CI: −23.31, −16.79; P < 0.00001; heterogeneity: χ2 = 0.12; I2 = 0%; P = 0.73; Fig. 12A). FIB (g/L) levels, disclosed by the 7-day group. improved significantly [42, 47] (MD: −0.71; 95% CI: −0.85, −0.57; P < 0.00001; heterogeneity: χ2 = 0.68; I2 = 0%; P = 0.41). D-D (mg/L) levels reported by the 7-day group indicated an insignificant decrease [36, 42] (MD: −0.63; 95% CI: −1.79, 0.54; P = 0.29; heterogeneity: χ2 = 14.72; I2 = 93%; P = 0.0001). Figure 10 illustrates these findings.
CRP is related to the inflammatory response, and the decrease in this indicator reflects the disappearance of inflammation in the patient’s body. The increase in FIB level represents the hypercoagulable state of blood, which is a critical factor in the occurrence of cerebral infarction and hinders the recovery of brain tissue after cerebral infarction. Its decrease represents the gradual withdrawal of the patient’s blood from the hypercoagulable state, which benefits the patient’s recovery. D-D mainly reflects the fibrinolytic function. An increase in D-D levels in plasma indicates the presence of secondary fibrinolysis, with lower levels indicating a better prognosis. These results suggest that RIPostC can modify these three indicators beneficially, although heterogeneity across studies warrants careful interpretation of these results.
Brain-derived neurotrophic factor (BDNF)
The 14-day group provided outcomes for BDNF at 14-day post-treatment [60, 61]. The meta-analysis improved significantly in BDNF (µg/L) compared to the control group. Figure 11 illustrates the following finding. A marginal reduction was noted in the BDNF levels (MD: −0.31; 95% CI: −0.65, 0.03; P = 0.08; with no heterogeneity: χ2 = 0.00; I2 =0%; P = 0.98; Fig.e 11). The minimal change and close-to-significance P-value indicate a modest effect of RIPostC on increasing BDNF levels, albeit without statistical significance. BDNF regulates growth and development, and induces differentiation, while modulating the synaptic connections of embryonic neurons. It simultaneously participates in activity-dependent neuronal plasticity, including regeneration, repair, and protection after injury, especially for cognitive function-related areas such as the frontal lobe and hippocampus. Therefore, higher levels of BDNF are expected to be more beneficial for patients.
Risk-of-bias assessment in the individual study
Cochrane Evaluation Tool 2 (ROB2) was used to evaluate the risk of bias in all included studies, covering five areas: bias risk caused by the randomization process, bias risk caused by deviation from expected intervention measures, missing outcome data, the risk of bias in outcome measurement, and the risk of bias in reporting outcome selection [65]. These areas are divided into “low risk,” “high risk,” or “some concerns”; they are independently completed by two researchers (M. Y. and J. W.), with a third researcher (J. L.) discussing and resolving potential disagreements. The quality assessment of the studies is shown in Figs. 12 and 13. The Additional files 6 and 7 lists specific details (see Additional files 6 and 7).
Sensitivity analysis
Data analyses revealed heterogeneity across nearly all results, leading to using a random-effects model for the meta-analysis. Identifying the precise contributors to this heterogeneity proved challenging even after sensitivity testing was performed. The observed heterogeneity is hypothesized to significantly correlate with factors such as the level of care provided by local hospitals, patient demographics, diversity in treatment approaches, and post-disease management. Despite this heterogeneity, the data suggest that RIPostC is an effective adjuvant therapy. Consequently, this analysis does not delve further into the issue of heterogeneity.
Publication bias
The potential for publication bias was investigated in the 14-day group, which focused solely on the NIHSS score as an outcome measure and included over 10 original studies. The analysis suggested the likelihood of publication bias, which may stem from the small sample sizes of the numerous included studies and the potential for selective reporting by the researchers. The overall quality of the included studies was assessed as low, complicating the identification of the source of this publication bias. The funnel plot detailing this analysis is available in the Additional file 8 (see Additional file 8).
GRADE evidence quality
The evidence quality for the outcomes assessed in the systematic review and meta-analysis was evaluated using the GRADE approach. The mRS was deemed to be of “moderate” quality. In contrast, the NIHSS, BI, and CRP were determined to be of low quality. Furthermore, IL-6, TNF-α, FIB, D-D, and BDNF received “very low” quality ratings. The Additional file 9 details an in-depth grading analysis (see Additional file 9).
Adverse reactions
Adverse reactions were reported in only five studies [33, 36, 47, 48, 64]. Most studies did not report any adverse reactions or were devoid of them. In Jiang et al.’s research [33], two patients reported minor swelling and pain in the limb used for pressure training, which subsided completely after a 30-min rest period. Fang et al.’s [36] study noted a single case of limb numbness in the experimental group, which resolved during treatment. Zhou et al. [47] reported that two patients who gradually adapted initially experienced pain in the upper limbs during training. According to Zhao et al.’s investigation [64], 32 patients experienced pain and numbness in the compressed limb during the RIPostC operation, 4 of whom exhibited subcutaneous bleeding; these symptoms were relieved entirely within 5-min postoperation, and the bruising resolved within a day. Li et al. [48] reported that five patients had bleeding spots and petechiae at the cuff site following treatment, which naturally resolved within 1 to 2 days; three patients developed numbness and swelling in the upper arm, which reduced or vanished upon cuff adjustment or pressure reduction, becoming tolerable after 2 to 3 days of acclimatization.
Discussion
In this meta-analysis, randomized controlled trials of RIPostC were systematically reviewed to assess its efficacy in enhancing the salvage and recovery of patients suffering from AIS. Compared to control groups, RIPostC demonstrated superior outcomes across most measured indicators, showing significant advantages. This meta-analysis included 38 randomized controlled trials involving 4334 patients. The intervention groups underwent RIPostC, while the control groups were treated with standard therapeutic interventions such as thrombolysis, blood pressure management, anticoagulation, antiplatelet therapy, antioxidant treatments, and fluid replenishment. The statistical outcomes revealed that RIPostC significantly reduced the NIHSS scores in patients with acute cerebral infarction, independent of the duration of the intervention or the specific protocols of RIPostC applied. Regarding the BI scores, though only the 7-day and 14-day intervention data were eligible for this meta-analysis, it was observed that RIPostC contributed to significant improvements in BI scores over both short-term (7-day and 14-day) and long-term (90-day) periods. Similarly, the mRS analysis, restricted to the 7-day and 14-day data, indicated that RIPostC effectively enhanced mRS scores in short-term (7-day) and long-term (90-day) assessments, suggesting an improved prognosis for patients receiving RIPostC treatment. In acute inflammation, analyses incorporated IL-6 data from the 14-day and 6-month groups. The findings indicated a significant decrease in IL-6 levels by the 30th day compared to the 14th day, indicating that extended treatment duration with RIPostC enhances anti-inflammatory recovery in patients. TNF-α levels were explicitly reported by the 6-month group, demonstrating RIPostC’s effectiveness. A comparison with shorter-duration data, similar to the IL-6 analysis, would have provided a clearer picture of RIPostC’s impact on reducing TNF-α levels. CRP serves as a marker for chronic inflammation related to atherosclerosis. CRP levels, reported by the 6-month group at 1 month, showed a reduction following RIPostC treatment. Future research should include assessments at varied intervals to comprehensively assess RIPostC’s effect on atherosclerosis-related chronic inflammation. FIB and D-D are indicators of the hypercoagulable state in patients with AIS. Both indicators, reported by the 7-day group on the 7th day, showed reductions post-RIPostC intervention, indicating amelioration of the hypercoagulable state. The limited measurement time points highlight the need for future studies to incorporate multiple assessment moments to depict changes fully. The elevation of BDNF concentration in the cortex could enhance synaptogenesis and dendritic spine development, thereby facilitating cortical functional remodeling in survivors of stroke. Despite only the 14-day group reporting on BDNF levels at 14 days, RIPostC was observed to increase this parameter, suggesting facilitation in the neuronal repair process in patients. Regarding the safety of RIPostC, adverse effects were reported only in five studies, with all incidents being minor and not impacting the course of treatment. This observation suggests that RIPostC is safe, with no cases of recurrent cerebral infarction or death reported among participants across the studies.
RIPostC has been more frequently applied in cardiac ischemia [66,67,68,69,70]; however, its use in treating cerebral ischemic conditions has increased recently. The protective action of RIPostC in patients with ischemia is multifaceted, involving anti-inflammatory and antioxidant effects, inhibition of apoptosis, regulation of protein expression, and modulation of protease activity [71]. These effects activate the body’s innate ischemic tolerance through short cycles of nonfatal, reversible ischemia and reperfusion, mediated by both humoral and immune-inflammatory regulatory mechanisms, conferring protection. Although the serum factors measured in the included studies do not fully cover all aspects of RIPostC’s protective mechanisms, they illustrate its potential benefits. FIB is a coagulation factor in plasma and an inflammatory marker, contributing to atherosclerosis by accumulating in the vessel wall, which can lead to endothelial cell migration, denaturation, and thrombosis due to its role in smooth muscle cell proliferation, hypertrophy, and enhancement of platelet aggregation and blood viscosity. Elevated levels of FIB are closely associated with the onset of acute cerebral infarction. D-D indicates fibrinolytic activity, with its levels increasing in response to active thrombus formation and fibrinolysis within the body’s blood vessels. The presence of covalent cross-links between the Y-chains underpins the structure of D-D, making it a sensitive and specific marker for the early diagnosis of cerebral infarction. Moreover, D-D levels help monitor the effectiveness of thrombolytic therapy and are directly proportional to the severity of cerebral infarction. Patients exhibiting elevated D-D levels in their plasma are at an increased risk of experiencing subsequent cerebral infarctions [72,73,74,75]. Research has documented that an inflammatory cascade is triggered following ischemia-reperfusion injury in the brain. CRP is an inflammatory marker capable of independently predicting future vascular incidents. Elevated CRP levels may serve as an indirect indicator of endothelial cell impairment, activation of inflammatory cytokines, vascular damage, and the predominant thrombotic conditions, all of which are intricately linked to the development and progression of atherosclerosis [76,77,78,79,80]. BDNF is a neurotrophic factor critical in maintaining neuronal survival, growth, differentiation, and repair post-injury. It enhances the proliferation of neural stem cells within the brain, fostering the developmental differentiation and growth necessary for neuronal regeneration. BDNF levels are significantly crucial for the recovery process in patients with ischemic stroke [81,82,83]. Beyond the direct impact of cerebral ischemia due to the depletion of intermediate metabolites and oxygen, the release of various amino acids from the cytosol substantially contributes to postischemic brain damage. The metrics analyzed in this study, including the NIHSS, BI, mRS, IL-6, TNF-α, CRP, FIB, D-D, and BDNF, demonstrate either improvement or reduction due to RIPostC over extended intervention durations. These observations indicate that the benefits of RIPostC become more pronounced with extended intervention periods, highlighting its potential as a treatment for AIS.
The considerable heterogeneity observed across groups for several indicators could stem from substantial differences in either the baseline or endpoint values of these indicators in certain studies, differences in the standard treatments administered, or variations in the duration, number of cycles, timing of ischemia, and reperfusion periods used in RIPostC across studies. Despite these sources of heterogeneity, the findings from the random-effects model meta-analysis are deemed significant.
Comparison with previous studies
In exploring English-language databases, only four meta-analyses and systematic reviews relevant to this field have been identified, with two focusing on animal studies and the other on clinical trials. The reviews of animal studies [84, 85], though encompassing a wide array of primary research and conducted across various species, provided a comprehensive and detailed assessment of the outcomes. These analyses present robust evidence supporting the preclinical efficacy of RIPostC. However, these two animal studies could interest researchers intending to conduct animal-based investigations into RIPostC. The remaining two reviews, focusing on clinical trials, one published in 2022 [86] and the other in 2018 [87], offer crucial insights and serve as significant resources for clinical practitioners during those periods. Both reviews confirmed the therapeutic significance and safety of RIPostC in the treatment of patients with ischemic stroke. However, they were limited by the relatively small number of primary studies they encompassed, and the scope of outcome measures considered was not exhaustive. Furthermore, subgroup analyses were not conducted. While recognizing the significance of these two reviews in evidence-based medicine and their relevance for clinical practitioners, this study incorporates more primary research, a broader range of outcome measures, and subgroup discussions, enhancing the robustness of the analytical results.
Strengths of this study
This review compiles all existing research on RIPostC for AIS treatment in China, categorizing it into detailed segments based on the duration of RIPostC application. It examines up to 10 outcome indicators to elucidate the effects of RIPostC as comprehensively as possible. While medical professionals have recommended RIPostC for cardiac conditions for many years, evidence has highlighted its significant efficacy in stroke treatment. In an era where alternative stroke treatments are actively sought, RIPostC emerges as an effective, safe, and novel adjuvant therapy. This review contributes new evidence-based medical insights for the clinical application of RIPostC, supporting its application beyond traditional heart disease treatments.
Limitations
This study may exhibit a language bias due to the exclusive inclusion of Chinese-language studies. The methodological quality of the included studies was generally low, with no descriptions of allocation concealment or blinding provided, raising concerns about potential researcher bias. Variations in the frequency, pressure of RIPostC application, intervention durations, and inconsistencies in the reported underlying treatments likely contributed to the high heterogeneity across studies. With a total sample size of 4324 participants across single-center trials, the study’s results could be influenced by the subjective perspectives of the researchers, impacting the robustness of the conclusions. The potential effect of the patients’ preexisting conditions on the outcome indicators further limits the extrapolation of the study’s findings. Adverse reactions were reported in only five studies, indicating that a more comprehensive safety assessment across more extensive and diverse clinical studies is warranted. The publication bias, possibly resulting from small study sizes, lack of multicenter trials, and selective reporting by researchers, cannot be ruled out. The overall low quality of the included studies complicates identifying specific causes for this issue.
Conclusions
In summary, the available evidence suggests that RIpostC beneficially impacts the treatment and recovery of patients with acute cerebral infarction compared to standard controls. However, the inherent limitations in the design quality of the included trials may influence the outcomes of our analysis, introducing a degree of bias. Consequently, future research should focus on elucidating the mechanistic underpinnings of RIpostC’s effects on AIS. Furthermore, there is a need for further randomized controlled trials employing rigorous methodologies to substantiate our findings.
Availability of data and materials
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
References
Sun HX, Wang WZ. An epidemiological survey report of cerebrovascular diseases among 600,000 people in China (in Chinese). Chin J Contemp Neurol Neurosurg. 2018;18(02):83–8. https://doi.org/10.3969/j.issn.1672-6731.2018.02.002.
Wang YJ, Cui LY, Ji XM, et al. The China National Stroke Registry for patients with acute cerebrovascular events: design, rationale, and baseline patient characteristics. Int J Stroke. 2011;6:355–61. https://doi.org/10.1111/j.1747-4949.2011.00584.x.
Song S, Liang L, Fonarow Gregg C, et al. Comparison of clinical care and in-hospital outcomes of Asian American and white patients with acute ischemic stroke. JAMA Neurol. 2019;76:430–9. https://doi.org/10.1001/jamaneurol.2018.4410.
Peng B, Liu SW, Kang M, et al. Clinical study of noninvasive limb ischemic preadaptation for acute cerebral infarction (in Chinese) [J]. Chinese J Convalescent Med. 2014;4:299–300. https://doi.org/10.13517/j.cnki.ccm.2014.04.005.
Wang Y, Zhao SS, Zheng YM, et al. Efficacy of safflor yellow combined with argatroban in the treatment of acute cerebral infarction and its effect on serum IL-8, ET-1, NO levels and hemorheology (in Chinese). Chinese J Integrat Med Cardio-/Cerebrovasc Dis. 2018;16(01):86–9. https://doi.org/10.3969/j.issn.1672-1349.2018.01.023.
Hori YS, Kodera S, Sato Y, et al. Eosinopenia as a predictive factor of the short-term risk of mortality and infection after acute cerebral infarction. J Stroke Cerebrovasc Dis. 2016;25(6):1307–12. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.12.007.
Saccaro LF, Aimo A, Emdin M, Pico F. Remote ischemic conditioning in ischemic stroke and myocardial infarction: similarities and differences. Front Neurol. 2021;26(12):716316. https://doi.org/10.3389/fneur.2021.716316.
Pignataro G. Emerging role of microRNAs in stroke protection elicited by remote postconditioning. Front Neurol. 2021;21(12):748709. https://doi.org/10.3389/fneur.2021.748709.
Gho BC, Schoemaker RG, van den Doel MA, Duncker DJ, Verdouw PD. Myocardial protection by brief ischemia in noncardiac tissue. Circulation. 1996;94(9):2193–200. https://doi.org/10.1161/01.cir.94.9.2193. PMID: 8901671.
Cui J, Liu N, Chang Z, Gao Y, Bao M, Xie Y, Xu W, Liu X, Jiang S, Liu Y, Shi R, Xie W, Jia X, Shi J, Ren C, Gong K, Zhang C, Bade R, Shao G, Ji X. Exosomal MicroRNA-126 from RIPC serum is involved in hypoxia tolerance in SH-SY5Y cells by downregulating DNMT3B. Mol Ther Nucleic Acids. 2020;5(20):649–60. https://doi.org/10.1016/j.omtn.2020.04.008. Epub 2020 Apr 25. PMID: 32380415; PMCID: PMC7210387.
Chen Q, Huang M, Wu J, Jiang Q, Zheng X. Exosomes isolated from the plasma of remote ischemic conditioning rats improved cardiac function and angiogenesis after myocardial infarction through targeting Hsp70. Aging (Albany NY). 2020;12(4):3682–93. https://doi.org/10.18632/aging.102837. Epub 2020 Feb 18. PMID: 32074081; PMCID: PMC7066898.
Fujita M, Asanuma H, Hirata A, Wakeno M, Takahama H, Sasaki H, Kim J, Takashima S, Tsukamoto O, Minamino T, Shinozaki Y, Tomoike H, Hori M, Kitakaze M. Prolonged transient acidosis during early reperfusion contributes to the cardioprotective effects of postconditioning. Am J Physiol Heart Circ Physiol. 2007;292(4):H2004–8. https://doi.org/10.1152/ajpheart.01051.2006. Epub 2007 Jan 5 PMID: 17208997.
Shi W, Vinten-Johansen J. Endogenous cardioprotection by ischaemic postconditioning and remote conditioning. Cardiovasc Res. 2012;94(2):206–16. https://doi.org/10.1093/cvr/cvs088. Epub 2012 Feb 9. PMID: 22323534; PMCID: PMC3331613.
Liu ZJ, Chen C, Li XR, Ran YY, Xu T, Zhang Y, Geng XK, Zhang Y, Du HS, Leak RK, Ji XM, Hu XM. Remote ischemic preconditioning-mediated neuroprotection against stroke is associated with significant alterations in peripheral immune responses. CNS Neurosci Ther. 2016;22(1):43–52. https://doi.org/10.1111/cns.12448. Epub 2015 Sep 19. PMID: 26384716; PMCID: PMC6492849.
Doeppner TR, Zechmeister B, Kaltwasser B, Jin F, Zheng X, Majid A, Venkataramani V, Bähr M, Hermann DM. Very delayed remote ischemic post-conditioning induces sustained neurological recovery by mechanisms involving enhanced angioneurogenesis and peripheral immunosuppression reversal. Front Cell Neurosci. 2018;29(12):383. https://doi.org/10.3389/fncel.2018.00383.
Valsecchi V, Laudati G, Cuomo O, et al. The hypoxia sensitive metal transcription factor MTF-1 activates NCX1 brain promoter and participates in remote postconditioning neuroprotection in stroke. Cell Death Dis. 2021;12:423. https://doi.org/10.1038/s41419-021-03705-9.
Geng X, Wang Q, Lee H, Huber C, Wills M, Elkin K, Li F, Ji X, Ding Y. Remote ischemic postconditioning vs. physical exercise after stroke: an alternative rehabilitation strategy? Mol Neurobiol. 2021;58(7):3141–57. https://doi.org/10.1007/s12035-021-02329-6.
Yu HH, Ma XT, Ma X, Chen M, Chu YH, Wu LJ, Wang W, Qin C, Tian DS. Remote limb ischemic postconditioning protects against ischemic stroke by promoting regulatory T cells thriving. J Am Heart Assoc. 2021;10(22):e023077. https://doi.org/10.1161/JAHA.121.023077.
Pignataro G, Esposito E, Sirabella R, Vinciguerra A, Cuomo O, Di Renzo G, Annunziato L. nNOS and p-ERK involvement in the neuroprotection exerted by remote postconditioning in rats subjected to transient middle cerebral artery occlusion. Neurobiol Dis. 2013;54:105–14. https://doi.org/10.1016/j.nbd.2013.02.008.
Vinciguerra A, Cepparulo P, Anzilotti S, Cuomo O, Valsecchi V, Amoroso S, Annunziato L, Pignataro G. Remote postconditioning ameliorates stroke damage by preventing let-7a and miR-143 up-regulation. Theranostics. 2020;10(26):12174–88. https://doi.org/10.7150/thno.48135.
An JQ, Cheng YW, Guo YC, Wei M, Gong MJ, Tang YL, Yuan XY, Song WF, Mu CY, Zhang AF, Saguner AM, Li GL, Luo GG. Safety and efficacy of remote ischemic postconditioning after thrombolysis in patients with stroke. Neurology. 2020;95(24):e3355–63. https://doi.org/10.1212/WNL.0000000000010884.
He YD, Guo ZN, Qin C, Jin H, Zhang P, Abuduxukuer R, Yang Y. Remote ischemic conditioning combined with intravenous thrombolysis for acute ischemic stroke. Ann Clin Transl Neurol. 2020;7(6):972–9. https://doi.org/10.1002/acn3.51063.
Poalelungi A, Tulbă D, Turiac E, Stoian D, Popescu BO. Remote ischemic conditioning may improve disability and cognition after acute ischemic stroke: a pilot randomized clinical trial. Front Neurol. 2021;30(12):663400. https://doi.org/10.3389/fneur.2021.663400.
Li YJ, Liang KK, Zhang L, Pan R, Hu YM, Zhao JH. Remote ischemic post-conditioning may improve post-stroke cognitive impairment: a pilot single center randomized controlled trial. J Stroke Cerebrovasc Dis. 2020;29(11):105217. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105217.
England TJ, Hedstrom A, O’Sullivan S, Donnelly R, Barrett DA, Sarmad S, Sprigg N, Bath PM. RECAST (Remote Ischemic Conditioning After Stroke Trial): a pilot randomized placebo controlled phase II trial in acute ischemic stroke. Stroke. 2017;48(5):1412–5. https://doi.org/10.1161/STROKEAHA.116.016429.
Pico F, Lapergue B, Ferrigno M, Rosso C, Meseguer E, Chadenat ML, Bourdain F, Obadia M, Hirel C, Duong DL, Deltour S, Aegerter P, Labreuche J, Cattenoy A, Smadja D, Hosseini H, Guillon B, Wolff V, Samson Y, Cordonnier C, Amarenco P. Effect of in-hospital remote ischemic perconditioning on brain infarction growth and clinical outcomes in patients with acute ischemic stroke: the RESCUE BRAIN Randomized Clinical Trial. JAMA Neurol. 2020;77(6):725–34. https://doi.org/10.1001/jamaneurol.2020.0326.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12. https://doi.org/10.1016/j.jclinepi.2009.06.005.
Chen JY. Effect of post-adaptation of distal ischemia on NIHSS scores and serum ultrasensitive C-reactive protein levels in patients with acute cerebral infarction (in Chinese). Modern Chinese Doctor. 2016;54(9):72–5.
Fan J, Zha JJ, Qian LN, et al. Effects of remote post-ischemic adaptation intervention on serum miR-21 and miR-24 levels and neurological function in patients with acute cerebral infarction (in Chinese) [J]. Chinese J Diff Compl Cases. 2017;16(11):1085–1088,1092. https://doi.org/10.3969/j.issn.1671-6450.2017.11.002.
Huang C, Ren XY, Zhou HT, et al. Study on the effect of upper limb remote ischemia post-adaptation therapy on neurological function and prognosis of acute cerebral infarction (in Chinese) [J]. Chinese Gen Pract. 2016;19(23):2767–70. https://doi.org/10.3969/J.issn.1007-9572.2016.23.005.
Yao XM, Yang XY, Ma L. Correlation analysis of dynamic changes in serum PTX3 levels in patients with acute cerebral infarction and neuroprotection after distant ischemia (in Chinese) [J]. Hebei Med J. 2022;28(03):417–21. https://doi.org/10.3969/J.issn.1006-6233.2022.03.014.
Liu LL, Feng CF, Liu XJ, et al. The protective value of implementing limb distal ischemic preadaptation in ischemic cerebral infarction on patients’ neurological function (in Chinese) [J]. China Health Care Nutri. 2016;26(33):108–108. https://doi.org/10.3969/j.issn.1004-7484.2016.33.158.
Jiang YL, Wang SP, Zhang YQ. Effect and correlation of ischemic adaptation on NIHSS scores and serum CysC levels in patients with acute cerebral infarction (in Chinese) [J]. Chinese J Gerontol. 2016;36(04):849–51. https://doi.org/10.3969/j.issn.1005-9202.2016.04.036.
Zhou XL, Pan CL. Effect of ischemic preadaptation in the distal limb compartment on the clinical prognosis and inflammatory factor expression levels in patients with cerebral infarction (in Chinese) [J]. Stroke Nerv Dis. 2018;25(2):138–41. https://doi.org/10.3969/j.issn.1007-0478.2018.02.005.
Kuang ZY, Xiang J, Zhang XF, et al. Value of CT perfusion imaging to evaluate post-ischemic adaptation of distal limbs in patients with acute ischemic stroke (in Chinese) [J]. J Pract Med. 2019;35(14):2311–5. https://doi.org/10.3969/j.issn.1006-5725.2019.14.026.
Fang P, Shi XY, Cao L, et al. The effect of distant ischemic postconditioning on short-term prognosis of acute cerebral infarction (in Chinese) [J]. J Anhui Health Voc Tech College. 2020;19(01):21–3. https://doi.org/10.3969/j.issn.1671-8054.2020.01.009.
Obli Mahhaba. The effect of adaptive therapy after distant ischemia on the recovery of neurological function in patients with acute large area cerebral infarction (in Chinese) [D]. Xinjiang Med Univ. 2020. https://doi.org/10.27433/d.cnki.gxyku.2020.000468.
Zhang X, Hu Y, Sui LM. Effect of post-adaptation therapy for distal ischemia on neurological function and yawning phenomenon in patients with ischemic stroke (in Chinese) [J]. Chinese J Med Device. 2020;33(6):91–2. https://doi.org/10.3969/j.issn.1002-2376.2020.06.060.
Liu H, Huang BY, Wang YC. Effect of pre-adaptation of distal limb ischemia on the prognosis of patients with cerebral infarction (in Chinese) [J]. China Modern Med. 2020;27(13):40–3. https://doi.org/10.3969/j.issn.1674-4721.2020.13.012.
Li MY. The effect of remote ischemic adaptation on the recent recovery of neurological function and vascular endothelial function in patients with acute cerebral infarction (in Chinese) [D]. North China Univ Technol. 2021. https://doi.org/10.27108/d.cnki.ghelu.2020.000229.
Li WW. Study on the brain protective mechanism of remote ischemic preconditioning in patients with acute cerebral infarction (in Chinese) [D]. Changchun University of Trad Chinese Med. 2022. https://doi.org/10.26980/d.cnki.gcczc.2020.000522.
Chen RB, Liu XQ, Fang JN, et al. The protective effect of adaptation after distant ischemia on cerebral ischemia in early intravascular treatment of acute cerebral infarction (in Chinese) [J]. New Med. 2020;51(11):830–4. https://doi.org/10.3969/j.issn.0253-9802.2020.11.005.
Lin P, Cui JH, Zhao TC, et al. Effect of distal ischemic preadaptation training on the prognosis of acute ischemic stroke (in Chinese) [J]. Guide China Med. 2020;18(31):23–24,27. https://doi.org/10.15912/j.cnki.gocm.2020.31.009.
Wu G. Therapeutic effect and serum HIF-1 in patients with acute cerebral infarction treated with adaptation after distant ischemia α、the impact of survivin level (in Chinese) [D]. Shenyang Med Coll. 2021. https://doi.org/10.27900/d.cnki.gsyyx.2021.000080.
Liu X. Evaluation of clinical effectiveness and safety of remote ischemic adaptation in the treatment of acute atherosclerotic cerebral infarction (in Chinese) [D]. China Med Univ. 2022. https://doi.org/10.27652/d.cnki.gzyku.2021.001475.
Chen J. The effect of distant ischemic preconditioning on the efficacy and serum peptide and PEDF levels in patients with acute ischemic stroke (in Chinese) [D]. Shenyang Med Coll. 2023. https://doi.org/10.27900/d.cnki.gsyyx.2021.000112.
Zhou ZM. The effect of adaptation after distant ischemia on hemorheology and neurological function in patients with ischemic stroke (in Chinese) [J]. Chinese J Recuperat Med. 2021;30(05):541–3. https://doi.org/10.13517/j.cnki.ccm.2021.05.032.
Li MY, Li CY, Liu B, et al. The effect of adaptation after distant ischemia on neural function and vascular endothelial function in patients with acute cerebral infarction (in Chinese) [J]. Chinese J Geriat Cardiovasc Dis. 2021;23(07):727–30. https://doi.org/10.3969/j.issn.1009-0126.2021.07.015.
Dai LJ. The effect of ischemic adaptation in distant parts of the limbs on neurological function and serum Cys C, hs CRP in patients with acute cerebral infarction (in Chinese) [D]. Shenyang Med Coll. 2023. https://doi.org/10.27900/d.cnki.gsyyx.2022.000013.
Wu JR. The effect of ischemic adaptation in distant parts of the limbs on neurological function and serum IL-6 and MMP-9 in patients with acute cerebral infarction (in Chinese) [D]. Shenyang Med Coll. 2023. https://doi.org/10.27900/d.cnki.gsyyx.2022.000106.
Wang FJ. The effect of ischemic adaptation therapy on neurological deficits and cognitive impairment in patients with acute cerebral infarction in distant parts of the limbs (in Chinese) [D]. Shenyang Med Coll. 2023. https://doi.org/10.27900/d.cnki.gsyyx.2022.000017.
Qu D, Lv XY, Zhang XF, et al. Evaluation of the effectiveness of adaptive treatment for acute cerebral infarction patients after distant ischemia [J]. J Aerospace Med. 2022;33(08):897–901.
Sun WM, Wang GH, Zhan Y, et al. A randomized controlled study on remote ischemic adaptation before intravenous thrombolysis in patients with acute ischemic stroke (in Chinese) [J]. Beijing Med J. 2022;44(12):1081–5+1091. https://doi.org/10.15932/j.0253-9713.2022.12.004.
Feng B, Li Y, Chang LG, et al. Effects of limb remote ischemic preconditioning training on inflammatory factors, brain-derived neurotrophic factors, and prognosis in patients with cerebral infarction (in Chinese) [J]. J Pract Cardiovasc Cerebropulm Vasc Dis. 2022;30(12):91–4+99. https://doi.org/10.12114/j.issn.1008-5971.2022.00.314.
Guo G, Wang XC, Li J. The effect of remote ischemic adaptation combined with ateplase on neurological function and oxidative stress response in patients with acute cerebral infarction (in Chinese) [J]. Clin Med. 2023;43(06):33–5. https://doi.org/10.19528/j.issn.1003-3548.2023.06.010.
Zhao T, Li M, Yan QY. Study on the effect of remote ischemic adaptation in the treatment of acute cerebral infarction (in Chinese) [J]. J Pract Cardio Cerebro Pulm Vasc Dis. 2023;31(09):91–4+98.
Meng M, Sun ML, Wang W, et al. Clinical observation on the effect of post-treatment of distal limb ischemia on serum glutamate concentration in patients with acute cerebral infarction (in Chinese) [J]. J Clin Exper Med. 2016;15(9):841–3. https://doi.org/10.3969/j.issn.1671-4695.2016.09.006.
Shi YH, Zhao JH, Song JL, et al. Efficacy of post-treatment of transient limb ischemia for acute cerebral infarction (in Chinese) [J]. J Apoplexy Nerv Dis. 2017;34(05):436–9. https://doi.org/10.19845/j.cnki.zfysjjbzz.2017.05.011.
Wang BN, He LQ, Wang Y, et al. Clinical observation on the effect of post-acute limb ischemia adaptation on neurological recovery in patients with acute cerebral infarction (in Chinese) [J]. J Apoplexy Nerv Dis. 2012;29(05):439–42. https://doi.org/10.19845/j.cnki.zfysjjbzz.2012.05.014.
Tian XJ, Liu FY. Study on the effects of remote limb ischemia post-treatment on serum BDNF levels and neurological function scores in patients with acute cerebral infarction (in Chinese) [J]. Cardiovasc Dis J integ Trad Chinese Western Med. 2020;8(15):67–8. https://doi.org/10.16282/j.cnki.cn11-9336/r.2020.15.054.
Wang LH, Wang WH, Jin YL, et al. Effect of remote limb ischemia post-treatment on serum BDNF levels and neurological function scores in patients with acute cerebral infarction (in Chinese) [J]. Heilongjiang Med Pharm. 2012;35(5):64–5. https://doi.org/10.3969/j.issn.1008-0104.2012.05.037.
Wu L, Li H, Liu KX, et al. Effects of post-ischemic limb management on serum MMP-2, MMP-9 and hs-CRP in patients with acute cerebral infarction (in Chinese) [J]. Acta Medicinae Sinica. 2019;32(3):1–5. https://doi.org/10.19296/j.cnki.1008-2409.2019-03-001.
Zhang WJ, Song XX, Peng J. Effect of non-invasive post-ischemic adaptation of the distal limb on the recovery of neurological function and changes in biochemical indicators in patients with acute cerebral infarction (in Chinese) [J]. Chinese J Gerontol. 2015;35(22):6401–3. https://doi.org/10.3969/j.issn.1005-9202.2015.22.039.
Zhao S, Zhu YY, Li HH, et al. Effect of post-treatment of distal limb ischemia on the recovery of symptoms of neurological deficits in patients with acute cerebral infarction (in Chinese) [J]. Prevent Treat Cardio Cereb Vasc Dis. 2021;21(3):225–9. https://doi.org/10.3969/j.issn.1009-816x.2021.03.005.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;28(366): l4898. https://doi.org/10.1136/bmj.l4898. PMID: 31462531.
Gaspar A, Lourenço AP, Pereira MÁ, Azevedo P, Roncon-Albuquerque R Jr, Marques J, Leite-Moreira AF. Randomized controlled trial of remote ischaemic conditioning in ST-elevation myocardial infarction as adjuvant to primary angioplasty (RIC-STEMI). Basic Res Cardiol. 2018;113(3):14. https://doi.org/10.1007/s00395-018-0672-3.
Bøtker HE, Kharbanda R, Schmidt MR, Bøttcher M, Kaltoft AK, Terkelsen CJ, Munk K, Andersen NH, Hansen TM, Trautner S, Lassen JF, Christiansen EH, Krusell LR, Kristensen SD, Thuesen L, Nielsen SS, Rehling M, Sørensen HT, Redington AN, Nielsen TT. Remote ischaemic conditioning before hospital admission, as a complement to angioplasty, and effect on myocardial salvage in patients with acute myocardial infarction: a randomised trial. Lancet. 2010;375(9716):727–34. https://doi.org/10.1016/S0140-6736(09)62001-8.
Crimi G, Pica S, Raineri C, Bramucci E, De Ferrari GM, Klersy C, Ferlini M, Marinoni B, Repetto A, Romeo M, Rosti V, Massa M, Raisaro A, Leonardi S, Rubartelli P, Oltrona Visconti L, Ferrario M. Remote ischemic post-conditioning of the lower limb during primary percutaneous coronary intervention safely reduces enzymatic infarct size in anterior myocardial infarction: a randomized controlled trial. JACC Cardiovasc Interv. 2013;6(10):1055–63. https://doi.org/10.1016/j.jcin.2013.05.011.
Yamanaka T, Kawai Y, Miyoshi T, Mima T, Takagaki K, Tsukuda S, Kazatani Y, Nakamura K, Ito H. Remote ischemic preconditioning reduces contrast-induced acute kidney injury in patients with ST-elevation myocardial infarction: a randomized controlled trial. Int J Cardiol. 2015;15(178):136–41. https://doi.org/10.1016/j.ijcard.2014.10.135.
Eitel I, Stiermaier T, Rommel KP, Fuernau G, Sandri M, Mangner N, Linke A, Erbs S, Lurz P, Boudriot E, Mende M, Desch S, Schuler G, Thiele H. Cardioprotection by combined intrahospital remote ischaemic perconditioning and postconditioning in ST-elevation myocardial infarction: the randomized LIPSIA CONDITIONING trial. Eur Heart J. 2015;36(44):3049–57. https://doi.org/10.1093/eurheartj/ehv463.
Li MY, Zhang YB, Niu JZ, Yang MF, et al. Progress of research on the role of postischemic adaptation in cerebral protection and mechanism in ischemic brain injury (in Chinese) [J]. J Apoplexy Nerv Dis. 2010;27(05):473–4. https://doi.org/10.19845/j.cnki.zfysjjbzz.2010.05.032.
Shi D, Xia T, Feng H, Cheng Q. Evaluating the diagnostic value of vWF:Ag, D-D and FDP in patients with acute cerebral infarction using ROC curves. Exp Ther Med. 2014;7(6):1573–7. https://doi.org/10.3892/etm.2014.1665.
Zhang SM. Correlation of antithrombin III, D-dimer, platelet aggregation and fibrinogen assay with acute cerebral infarction (in Chinese) [J]. Lab Med Clin. 2011;8(04):453–4. https://doi.org/10.3969/j.issn.1672-9455.2011.04.041.
Zhang GB, Bai LJ, Zhao WZ, Wen F, et al. Study on the changes of cerebrospinal fluid and plasma coagulation and fibrinolytic indexes in patients with acute cerebral infarction (in Chinese) [J]. J Apoplexy Nerv Dis. 2002;03:43–4.
Zhang J, Song Y, Shan B, He M, Ren Q, Zeng Y, Liu Z, Liu H, Xu J. Elevated level of D-dimer increases the risk of stroke. Oncotarget. 2017;9(2):2208–19. https://doi.org/10.18632/oncotarget.23367.
Emerging Risk Factors Collaboration, Kaptoge S, Di Angelantonio E, Lowe G, Pepys MB, Thompson SG, Collins R, Danesh J. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375(9709):132–40. https://doi.org/10.1016/S0140-6736(09)61717-7.
Han Y, Wu S, Hu Q, Xiao JQ, Wei DM, Liu LL, Li ZZ. Thrombomodulin and high-sensitive C-reactive protein levels in blood correlate with the development of cerebral infarction among Asians. Mol Neurobiol. 2016;53(4):2659–67. https://doi.org/10.1007/s12035-015-9279-y.
Li J, Zhao X, Meng X, Lin J, Liu L, Wang C, Wang Y, Wang Y. CHANCE Investigators. High-sensitive C-reactive protein predicts recurrent stroke and poor functional outcome: subanalysis of the clopidogrel in high-risk patients with acute nondisabling cerebrovascular events trial. Stroke. 2016;47(8):2025–30. https://doi.org/10.1161/STROKEAHA.116.012901.
Elkind SM, Luna JM, McClure LA, Zhang Y, Coffey CS, Roldan A, Del Brutto OH, Pretell EJ, Pettigrew LC, Meyer BC, Tapia J, White C, Benavente OR. LIMITS Investigators. C-reactive protein as a prognostic marker after lacunar stroke: levels of inflammatory markers in the treatment of stroke study. Stroke. 2014;45(3):707–16. https://doi.org/10.1161/STROKEAHA.113.004562.
Xu R, Yin X, Xu W, Jin L, Lu M, Wang Y. Assessment of carotid plaque neovascularization by contrast-enhanced ultrasound and high sensitivity C-reactive protein test in patients with acute cerebral infarction: a comparative study. Neurol Sci. 2016;37(7):1107–12. https://doi.org/10.1007/s10072-016-2557-2.
Colino-Oliveira M, Rombo DM, Dias RB, Ribeiro JA, Sebastião AM. BDNF-induced presynaptic facilitation of GABAergic transmission in the hippocampus of young adults is dependent of TrkB and adenosine A2A receptors. Purinergic Signal. 2016;12(2):283–94. https://doi.org/10.1007/s11302-016-9502-y.
Heitz U, Papmeyer M, Studerus E, Egloff L, Ittig S, Andreou C, Vogel T, Borgwardt S, Graf M, Eckert A, Riecher-Rössler A. Plasma and serum brain-derived neurotrophic factor (BDNF) levels and their association with neurocognition in at-risk mental state, first episode psychosis and chronic schizophrenia patients. World J Biol Psychiatry. 2019;20(7):545–54. https://doi.org/10.1080/15622975.2018.1462532.
Hogarth SJ, Jaehne EJ, van den Buuse M, Djouma E. Brain-derived neurotrophic factor (BDNF) determines a sex difference in cue-conditioned alcohol seeking in rats. Behav Brain Res. 2018;26(339):73–8. https://doi.org/10.1016/j.bbr.2017.11.019.
Liu K, Cai Z, Zhang Q, et al. Determination of significant parameters in remote ischemic postconditioning for ischemic stroke in experimental models: a systematic review and meta-analysis study. CNS Neurosci Ther. 2022;28(10):1492–508. https://doi.org/10.1111/cns.13925. Epub 2022 Jul 27. PMID: 35896511; PMCID: PMC9437239.
Torres-Querol C, Quintana-Luque M, Arque G, et al. Preclinical evidence of remote ischemic conditioning in ischemic stroke, a metanalysis update. Sci Rep. 2021;11(1):23706. https://doi.org/10.1038/s41598-021-03003-6.PMID:34887465;PMCID:PMC8660795.
Lu M, Wang Y, Yin X, et al. Cerebral protection by remote ischemic post-conditioning in patients with ischemic stroke: a systematic review and meta-analysis of randomized controlled trials. Front Neurol. 2022;21(13):905400. https://doi.org/10.3389/fneur.2022.905400.PMID:36212669;PMCID:PMC9532592.
Zhao JJ, Xiao H, Zhao WB, et al. Remote ischemic postconditioning for ischemic stroke: a systematic review and meta-analysis of randomized controlled trials. Chin Med J (Engl). 2018;131(8):956–65. https://doi.org/10.4103/0366-6999.229892.PMID:29664057;PMCID:PMC5912063.
Author information
Authors and Affiliations
Contributions
MY led the design and execution of this study, undertaking the literature review, data collection, and analysis, and drafted the initial manuscript. JL and QC provided oversight on the study’s design, offering critical feedback and revisions on the manuscript’s content. JW and MY were involved in data collection and analysis, contributing statistical software support. All authors contributed to the manuscript and have approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
13643_2024_2568_MOESM4_ESM.xlsx
Additional file 4. Calculated data Table 1.
13643_2024_2568_MOESM5_ESM.xlsx
Additional file 5. Calculated data Table 2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yan, MY., Liu, JM., Wu, J. et al. Impact of remote ischemic postconditioning on acute ischemic stroke in China: a systematic review and meta-analysis of randomized controlled trials. Syst Rev 13, 141 (2024). https://doi.org/10.1186/s13643-024-02568-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-024-02568-3