Abstract
Background
Psychosocial approaches are the first-line treatments for cocaine dependence, although they still present high dropout and relapse rates. Thus, there is a pressing need to understand which variables influence treatment outcomes to improve current treatments and prevent dropout and relapse rates. The aim of this study is to explore predictors of treatment retention and abstinence in CUD.
Methods
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). We searched three databases—PubMed, PsychINFO and Web of Science—for randomized clinical trials (RCTs) published in English and Spanish from database inception through April 1, 2023. We selected all studies that met the inclusion criteria (adults aged ≥ 18, outpatient treatment, CUD as main addiction, and no severe mental illness) to obtain data for the narrative synthesis addressing cocaine abstinence and treatment retention as main outcome variables. After data extraction was completed, risk of bias was assessed using the Cochrane risk-of-bias tool for randomized trials (RoB-2).
Results
A total of 566 studies were screened, and, of those, 32 RCTs were included in the synthesis. Younger age, more years of cocaine use, and craving levels were significant predictors of relapse and treatment dropout. Fewer withdrawal symptoms, greater baseline abstinence, greater treatment engagement, and more self-efficacy were all predictors of longer duration of abstinence. The role of impulsivity as a predictor of CUD is unclear due to conflicting data, although the evidence generally suggests that higher impulsivity scores can predict more severe addiction and withdrawal symptoms, and earlier discontinuation of treatment.
Conclusion
Current evidence indicates which variables have a direct influence on treatment outcomes, including well-studied cocaine use-related variables. However, additional variables, such as genetic markers, appear to have a high impact on treatment outcomes and need further study.
Systematic review registration
This systematic review is registered at PROSPERO (ID: CRD42021271847). This study was funded by the Spanish Ministry of Science, Innovation and Universities, Instituto Carlos III (ISCIII) (FIS PI20/00929) and FEDER funds and Fundació Privada Hospital de la Santa Creu i Sant Pau (Pla d’acció social 2020).
Similar content being viewed by others
Introduction
Cocaine use disorder (CUD) is a chronic condition characterized by frequent relapses. This disorder imposes a significant burden on patients, their families and the community. For this reason, treatment services generally need to work with patients over their entire lifetime to prevent drug-related death and/or relapse during personally challenging times. According to data from the European Union, the time interval between the mean age of first cocaine use and first treatment is > 10 years, with 47% of cocaine users in the clinical sample starting treatment for the first time after this period [1]. This finding implies that most cocaine users initiate treatment only after the addiction has become well-established and thus highly resistant to treatment.
According to available evidence, psychosocial approaches are defined as the first-line treatments for CUD. Unlike other illicit substances such as opioids, there is no specific pharmacological treatment for cocaine, which emphasizes the use of psychosocial treatments in addressing this condition [2, 3]. However, psychosocial approaches still present high dropout and relapse rates, thus, there is a pressing need to understand which variables influence treatment outcomes. For this reason, it is important to continue improving psychosocial interventions to reduce the chronicity of the disorder. Contingency management (CM) and cognitive-behavioral therapy (CBT) are the most appropriate approaches for CUD [2, 4,5,6]. Moreover, there is some evidence to suggest that adding CM to CBT in the treatment of cocaine-related disorders, especially at the beginning of treatment, can help to improve and maintain abstinence at 6-months [3].
Based on the currently available evidence [7], the best predictors of treatment outcomes are 1) treatment retention (measured by urinalysis), 2) craving (measured through the Cocaine Selective Severity Assessment [CSSA]), and 3) impulsivity, regardless of how it is measured [8]. In other words, lower treatment retention rates and higher craving and impulsivity levels predict worse outcomes.
Despite predictive factors of dropout and relapse are relevant to identify deficiencies in cocaine dependence treatment, the last review about this topic was published in 2007 [7]. Therefore, there is a need for a comprehensive update. Our work focuses on exploring all the evidence from published RCTs assessing a wide range of predictors of CUD treatment outcomes from inception until now. This approach has advantages regarding the inclusion of new predictors not previously considered, such as genetic markers to explore new, potentially innovative, ways of personalizing CUD treatment.
The present task involves exploring factors that accumulate substantial evidence that should be incorporated into treatment protocols, as well as those lacking sufficient evidence which warrant exploration to determine their potential relevance in the evolution and prognosis of CUD.
In this context, the aim of the present systematic review was to explore predictors of treatment outcomes in CUD. To perform the review, we searched the main databases to identify all RCTs that have specifically measured predictors of treatment outcomes in CUD.
Method
Search strategy
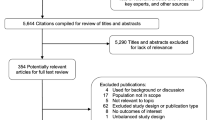
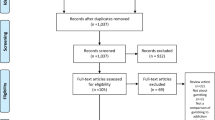
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines (Fig. 1 and additional files 1 and 2) [9]. This review was registered and is available for consultation at PROSPERO, the international prospective register of systematic reviews of the National Institute for Health Research (registration number: CRD42021271847) on October 14, 2021. We searched three databases—PubMed, APA PsychINFO, and Web of Science—from database inception through April 1, 2023. We searched the PubMed database for clinical trials and RCTs, the APA PsychINFO database for journal articles and clinical trials and the Web of Science for journal articles in the main library. Only articles published in English or Spanish were included. The search strategy was the same for the three databases using terms related to the outcome and the population, as follows: (cocaine)AND(treatment outcome)AND(predictors). The search yielded 63 records from PubMed, thirteen from APA PsychINFO, and 490 from Web of Science (see additional file 3).
Selection criteria
The inclusion criteria for the studies were as follows: 1) adults ≥ age 18; 2) outpatient treatments, and 3) CUD as the main addiction according to Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria or to the Mini International Neuropsychiatric Interview (MINI). Exclusion criteria for the studies were: 1) inpatient treatment or treatments other than outpatient treatment and 2) severe mental illness or any main addiction other than CUD. Given the different modalities of treatment settings available (i.e.: inpatient, outpatient, daycare) and that predictors of treatment outcome may differ among modalities, we specifically focused on outpatient treatments. This systematic review forms part of a larger ongoing study registered in ClinicalTrials.gov (registration ID: NCT05207228) that aims to test the efficacy (dropout and abstinence rates) of a web-based treatment in a sample of CUD outpatients.
Main outcome variables
The main outcome variables were cocaine abstinence and treatment retention in patients diagnosed with CUD. All RCTs that specifically measured potential predictors of cocaine use in individuals in outpatient treatment were included.
To guide the analysis, we developed the following review question in accordance with the recommendations in the PICO (Population, Intervention/Exposure, Comparison and Outcome) framework for systematic reviews: “What factors predict cocaine dependence and treatment outcomes in adult outpatients with CUD?”. The target population was comprised of adults in outpatient treatment diagnosed with CUD. Given the highly heterogeneous psychosocial and pharmacological interventions for CUD, we did not specify any specific intervention or comparison. We evaluated the following potential predictors of treatment retention and abstinence: sociodemographic; cocaine use patterns; comorbid pathologies; personality traits; neuroimaging, biological and genetic markers; and treatment variables.
Data extraction
All citations from the databases were exported to Mendeley. Next, we removed duplicate studies and those that could not be located. Next, one of the researchers (APL) screened each citation by title and abstract to identify studies for full review, which were then screened by two authors (APL and NMB) to determine if they met eligibility criteria. If there was any doubt regarding whether a study met the inclusion criteria, the same authors discussed these studies on a case-by-case basis, which were included or not based on a consensus decision. Full-text screening was performed and the data were compiled into an extraction table.
The author APL retrieved the following data for each study: 1) general information (title, author, journal, year); 2) study characteristics (design, objectives/hypothesis, participants, methods, inclusion/exclusion criteria, conditions); 3) participant characteristics (age; gender; sociodemographic data; cocaine use variables; comorbid psychiatric disorders; personality traits; use of other substances; neuroimaging; genetic markers; biological markers); 4) treatment outcomes (retention, dropout, relapse, abstinence after treatment) and type of measurement, which includes time and method of assessment, and measurement instrument; 5) intervention (type of intervention, intervention characteristics [number of sessions, individual/group sessions, duration, and frequency of sessions] and number of post-treatment follow-up sessions), and 6) outcomes (predictors of treatment outcomes of individuals with CUD in outpatient treatment) (Table 1).
Assessment of risk of bias
One researcher (APL) assessed the risk of bias in the individual studies using the revised Cochrane risk-of-bias tool for randomized trials (RoB-2), which includes five different domains: randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result [42]. The Risk of bias synthesis can be seen in Table 1.
Results
Data synthesis strategy
The results are presented as a narrative synthesis. A PRISMA flow-chart was prepared to illustrate the selection process of the RCTs included. The search yielded a total of 566 records; of these, 32 met the selection criteria and were included in the systematic review (Fig. 1 and additional file 4). Next, the data in the extraction table were summarized to perform a qualitative synthesis and to organize the information into sections.
A metanalytic synthesis was not performed, mainly due to the heterogeneity (interventions, treatment duration, follow-up period, outcome variables) of the studies included in this systematic review. Given the wide variability in the interventions performed, it was not possible to unify all of the studies under a single intervention variable. In addition, these studies included numerous other potential predictors of treatment outcomes (treatment duration, follow-up period, and outcome variables), which were also heterogenous among these studies. In short, due to the clinical and methodological heterogeneity, a metanalytic synthesis would have been an inappropriate study design.
Description of studies
After completion of the data extraction process, 32 RCTs (or secondary analyses of data from an RCT) were included in the review. The patients in those 32 RCTs were randomized to a wide range of different treatment conditions, either pharmacological or psychotherapeutic. As a result, the review includes information about different potential predictors of treatment outcomes in cocaine users, which are described below in separate sections by categories, as follows: sociodemographic variables; cocaine use variables; comorbid psychiatric disorders; personality traits; neuroimaging; genetic markers; and biological markers (Table 1).
Numerous variables were evaluated in these RCTs as possible predictors for CUD, which also assessed the association between the variable and treatment outcomes (Table 2).
Narrative synthesis
Sociodemographic variables: age, gender, ethnicity, education and employment status and type of income
Three RCTs found that age was a significant predictor of treatment retention, with younger patients less likely to remain in treatment and more likely to drop out earlier [28, 36, 37]. Even among patients who had completed the stabilization phase, younger patients were more likely to drop out than older patients. Moreover, younger patients randomized to a specific treatment dropped out earlier in the treatment process than older patients [36, 37]. One trial found that older age was a predictor of sustained cocaine abstinence or, among current users, of transitioning to abstinence [28]. The findings of those trials suggest that it may be possible to reduce the likelihood of treatment dropout by identifying and addressing the concerns of younger patients through prevention campaigns.
Two RCTs found that gender was not a predictor of cocaine use at six months posttreatment [22, 24]. Interestingly, [22] observed significant differences between genders in the transition from abstinence to cocaine use, with men transitioning nearly two times as fast as women. In other words, women who use cocaine are more likely to keep using it while women who are abstinent are more likely to remain abstinent. By contrast, men who are abstinent are at higher risk of switching back to cocaine use and vice versa [22]. However, the low proportion of women in both studies (23% in each RCT) could have at least partially influenced these findings, in part by reducing the studies’ power to identify gender as a predictor of treatment outcomes in CUD [22, 24].
Two RCTs reported that ethnicity was a predictor of treatment retention, finding that ethnic minorities tend to remain in treatment during less time and drop out sooner [24, 37]. Interestingly, [37] found that African-American participants living alone remained in treatment longer than those living with a partner or spouse; by contrast, the opposite was true for American Caucasians. Although no data on cocaine use among the patients’ partners was collected, many African-American participants reported difficulties in achieving abstinence or continuing with treatment because people close to them continued using drugs [37]. In their RCT, [24] found that, during treatment for CUD, African-American women had lower rates of past self-disclosure, a lower percent of time at talk, less receipt of advice, and less non-positive feedback that non-Hispanic white women [24]. These data suggest that African-American women, the most vulnerable group, should receive more attention in treatment programs to enhance their motivation to change.
Five of the RCTs in this review found that education and employment status were significant predictors of treatment retention and longest duration of abstinence (LDA) during treatment. In other words, less educated and/or unemployed participants remained in treatment for a shorter period of time, and lower educational levels were associated with a shorter duration of abstinence [28, 32, 33, 36, 37]. Unemployed men remained in treatment longer than unemployed women (82 vs. 56 days), while employed women had higher treatment retention rates than employed men (148 vs. 103 days). These findings suggest that unemployed and less educated women, who are the most vulnerable group, might require treatment interventions that target other psychosocial needs, such as financial concerns or job search skills, in order to increase treatment retention [37]. Only one trial [28] found that a lower educational level predicted continued abstinence or transition to cocaine-free status, with a negative correlation between years of education and transitioning to cocaine abstinence. Based on the mixed evidence in these trials, the role of education and employment status as predictors of treatment retention remains to be clarified.
The role of income received during treatment has received scant attention as a potential predictor of treatment outcomes in CUD. To date, only one study [32] has included this variable as a potential predictor. After controlling for demographic and baseline characteristics, the authors of that study found that income from illegal activities and public assistance were significant predictors of LDA. However, income from public assistance sources was associated with greater LDA whereas illegal income was associated with a shorter LDA [32].
Cocaine use variables: years of cocaine use and current use; mode of use, addiction severity index, cocaine withdrawal symptoms, toxicology screening and duration of abstinence, and craving
Four RCTs found that years of cocaine use, LDA, cocaine use in the 30 days prior to treatment entrance, and current cocaine use were strong predictors of treatment retention and abstinence (based on urine drug tests). Less cocaine use in the 30 days prior to treatment entrance, fewer years of cocaine use, and a greater LDA were all predictive of higher abstinence and treatment retention rates [28, 31, 36]; these same variables were also predictors of a lower frequency and proportion of days of cocaine use [27]. In one study, each additional year of cocaine use decreased the odds of a negative urine drug sample at the 9-month follow-up by 5% [31]. These findings indicate that years of cocaine use and current cocaine use status are robust predictors of treatment outcomes in cocaine users.
The mode of cocaine use has not been widely studied as a predictor of treatment outcomes in cocaine users. However, one RCT [37] found that the mode of use predicted treatment retention. Crack and intravenous cocaine users remained in outpatient treatment fewer days than intranasal users (88 vs. 134 days, respectively), which suggested that crack smokers and intravenous users have a worse prognosis than intranasal users.
Two RCTs found that addiction severity, measured by the Addiction Severity Index (ASI), a tool used to assess the impact of alcohol and drug use on seven potential problem areas (medical, employment/support status, alcohol, drug, legal, family/social and psychiatric) does not predict time in treatment nor time to dropout among patients receiving treatment after completing the stabilization phase [36, 37]. An important finding of that RCT was that the heaviest users spent the same time in treatment as user with less severe addictions [37]. These findings suggest that many of the participants in those studies were not well-suited for outpatient treatment or not yet ready to change; in addition, the heaviest users (those with more days of cocaine use in the previous month) were less likely to complete the stabilization phase and thus less likely to be randomized to treatment [36].
Two RCTs found that lower scores on the CSSA, a tool used to measure cocaine withdrawal symptoms, was a significant predictor of three weeks of continuous abstinence, a 50% reduction in the ASI composite drug scores at the end of treatment, and no self-reported cocaine use during the last four weeks [10, 25]. More specifically, subjects with CSSA scores > 21 were twelve times more likely to fail to reach three continuous weeks of abstinence [25]. These results suggest that psychological treatments that target CUD should emphasize coping strategies to help patients better manage withdrawal symptoms, thereby limiting the potential impact of these symptoms on treatment outcomes, which would likely improve prognosis.
Four RCTs found that a negative urine sample predicted three continuous weeks of abstinence, a 50% reduction in drug problem severity, and no self-reported cocaine use at the end of treatment [10, 21, 25, 32]. This variable was also a significant predictor of long-term abstinence (up to 6 months after treatment completion) [14, 23, 41].
In one study [14], patients who had achieved abstinence at baseline had 70% fewer days of cocaine use compared to patients who were not abstinent at baseline. In addition, patients who were abstinent at baseline but later dropped out of treatment were more likely to become abstinent again at a later time point. Furthermore, patients who achieved abstinence after one month of treatment were 14 times more likely than those who were still using at that time point to remain abstinent at the 6-month follow-up [23].
The predictive capacity of a negative urine test was stronger when combined with cocaine withdrawal symptoms (measured by the CSSA). More specifically, a negative urine drug test combined with lower scores on the CSSA was the best predictor for ≥ 3 continuous weeks of abstinence, a 50% reduction in drug problem severity, and no self-reported cocaine use at the end of treatment [10, 21, 25]. Moreover, a single positive urine test at treatment entry was a significant predictor of non-abstinence at the end of treatment [21].
Two RCTs found that the LDA (consecutive weeks of negative urine samples during treatment) predicted abstinence at 9-months posttreatment. In addition, the greater the number of negative samples submitted during treatment, the higher the long-term abstinence rate [11, 31]. Specifically, [31] and colleagues found that every one week increase in LDA increased the odds of a negative urine test by 21%.
Two RCTs found that baseline craving levels (measured by the CSSA) predicted abstinence and craving intensity during treatment. That is, higher levels of craving at baseline predicted fewer months of consecutive abstinence. In addition, a higher proportion of days per week of craving before the start of treatment predicted a higher craving proportion during treatment [14, 18].
Comorbid conditions: anhedonia, depressive symptoms and psychiatric severity; sleep disturbance, and antisocial personality disorder
Findings regarding the predictive capacity of psychiatric symptoms have been mixed. One RCT showed that self-reported anhedonia symptoms (from Beck’s Depression Inventory [BDI]) were strong predictors of poor treatment response, with higher scores in anhedonia symptoms predicting a worse prognosis [20]. However, when anhedonia symptoms were excluded from the BDI, the total score was not predictive of treatment outcomes [20], which is in line with the finding reported in another RCT, in which psychiatric severity alone was not a predictor of treatment dropout [37]. Nevertheless, four RCTs found that psychiatric symptoms (as measured by the European version of the ASI, EuropASI) and depressive symptoms predicted abstinence and treatment adherence, with more severe psychiatric and depressive symptoms indicating shorter periods of cocaine abstinence and poorer treatment adherence [28, 35, 36, 38]. Importantly, one RCT found that even though participants with depression or depressive symptoms had lower rates of treatment adherence, when these patients did adhere to treatment, they were usually more motivated to continue treatment to alleviate symptoms associated with depression and cocaine use [36].
The role of sleep disturbance as a possible predictor of treatment outcomes in cocaine users is not well-understood, mainly because only limited data are available. However, [40] (a secondary analysis of data from a multi-site RCT) found that, contrary to the initial hypothesis, baseline sleep disturbance were not significant predictors of end-of-treatment abstinence. However, the presence of a sleep disturbance was a significant predictor of three mediators: cocaine craving, anxiety, and depression, which in turn were predictors of low rates of end-of-treatment abstinence [40].
Two RCTs compared patients with and without a diagnosis of antisocial personality disorder (APD) to determine the predictive capacity of this variable. However, APD did not predict differential response to outpatient continuing care treatment. Similarly, APD was not a predictor of relapse or treatment retention among cocaine users [26, 37]. Nevertheless, [26] found that patients with APD had significantly worse medical and psychiatric problems than non-APD patients at the beginning of outpatient continuing care and during follow-up.
Personality traits: impulsivity
Impulsivity plays an important role in substance use disorders, including CUD, and several studies have found that baseline impulsivity is a robust predictor of treatment outcomes. Three of the RCTs included in this review found that baseline impulsivity, measured with the BIS-11, predicted cocaine use, treatment retention, and severity of use and withdrawal symptoms. Compared to low baseline impulsivity levels, high levels of impulsivity at baseline predicted more severe addiction and withdrawal symptoms, a shorter period of time in treatment (i.e., earlier dropout), and a significantly greater cocaine use within the last 30 days of treatment [15, 29, 30]. Schmitz and colleagues performed a secondary analysis of data from [29] and showed that higher scores on indices of non-planning impulsivity predicted ≥ 2 weeks of abstinence; by contrast, indices of the attentional, motor, and inhibitory-control components of impulsivity were not significant predictors of treatment retention [34].
Neurocognitive functioning: baseline response inhibition, cognitive interference, attentional bias; cognitive flexibility and problem solving
The impact of neurocognitive variables on treatment outcomes in cocaine users has received scant attention. An RCT was conducted to evaluate baseline response inhibition, cognitive interference, and attentional bias as possible predictors of treatment retention and crack cocaine use. Those authors found that good response inhibition, low baseline cognitive interference, and low baseline attentional bias did not predict the number of CBT sessions attended. By contrast, those variables predicted fewer days of crack cocaine use during the last 30 days of treatment [30].
One trial evaluated cognitive flexibility and problem solving as potential predictors of treatment outcomes. In that trial, a high percentage of perseverative errors on the Wisconsin Card Sorting Test (WCST), the most widely used tool to assess cognitive flexibility and problem solving, was a robust predictor of treatment dropout. In other words, patients who repeated mistakes on a problem-solving task discontinued treatment earlier than patients who performed better on the WCST [39].
Neuroimaging: brain activation
Brewer and colleagues [16] evaluated brain activation, measured by functional magnetic resonance imaging (fMRI) during performance of the Stroop Task as a potential predictor of treatment outcomes in cocaine users. In that trial, better performance on colour naming and interference predicted greater treatment retention. With regards to cognitive control and behavioral therapy for cocaine use, the results of that trial showed that activation in specific cortico-striatal regions during the Stroop Task was associated with reported abstinence and cocaine-free urine tests. In addition, activation of the dorsolateral prefrontal cortex (dlPFC) was inversely correlated with treatment retention; participants with lower dlPFC activation remained in treatment for a longer period of time. These findings suggest that brain activation might be a more sensitive measure for predicting treatment outcomes.
Genetic markers: catechol-O-methyltransferase (COMT) Gene Val158met polymorphism
Studies on genetic markers as potential predictors of treatment outcomes in CUD are limited. In fact, only one RCT [17] has been conducted to explore the role of the COMT Gene Val158met polymorphism as a possible predictor of treatment outcomes in cocaine users. COMT is a regulator of catecholamines in the brain, and the COMT gene polymorphism (Val158met) predicted greater reductions in cocaine use over time. When subjects with the Val allele were assigned to a web-based, computerized CBT treatment program, they were more likely to achieve ≥ 3 weeks of continuous abstinence and to present a higher percentage of days of abstinence during treatment compared to patients who carried the Met/Met allele [17].
Treatment features: treatment condition; therapeutic alliance and advice giving; expectations for improvement and commitment to abstinence, and acuity for biomedical problems
The treatment condition has emerged as a robust predictor of treatment outcomes, with four different trials finding that contingency management is predictive of long-term abstinence, higher treatment retention rates, and a higher proportion of negative urine samples [11, 32, 33, 35]. One RCT found that CM was especially beneficial in terms of treatment retention in cocaine users who also used marijuana because these patients tend to drop out of treatment relatively quickly without CM [11]. Another RCT found that treatment outcomes were better in patients who received individual and/or group drug counselling compared to patients randomized to other treatments, such as cognitive therapy or supportive-expressive therapy (a psychodynamic approach) [37].
Two RCTs found that stronger therapeutic alliance is not predictive of cocaine use (ASI) at 6 months posttreatment [12, 13]. However, therapeutic alliance does appear to predict cocaine use at one month posttreatment and also improves depressive symptoms (as measured by the BDI) in patients who remain in treatment versus those who discontinue treatment earlier in the process [12]. Moreover, therapeutic alliance can predict retention across various treatment conditions. In patients who received supportive-expressive therapy or individual drug counselling, a stronger alliance predicted a longer period of time in treatment [13]. Another RCT showed that weak therapeutic alliance in patients receiving group drug counselling was a significant predictor of higher drug use (measured by urinalyses and self-report measures) at the next treatment session, and lower treatment retention rates [19].
In the trial performed by Crits-Chrisoph and colleagues, [19] advice giving, whether from other patients or from the counsellor, predicted abstinence and cocaine use. More specifically, a greater use of advice predicted fewer months of abstinence and more days of cocaine use, including next session of cocaine use.
Several other variables can predict cocaine abstinence. Two RCTs found that expectations for improvement and commitment to abstinence were both strong predictors of sustained abstinence. In other words, a higher level of treatment engagement increases the odds of achieving abstinence [18, 28]. According to Crits-Christoph and colleagues [18], the mechanism underlying the association between higher engagement and better outcomes is probably that expectations for improvement increase therapeutic alliance, which is associated with better treatment outcomes. McKay and colleagues [28] found that self-help beliefs, self-help participation, and self-efficacy also play an important role in transitioning from cocaine use to abstinence. Thus, higher levels of those three variables predicted the transition from cocaine use to abstinence. This finding underscores the key role of expectations on improvement and self-efficacy.
One RCT [18] found that concerns about biomedical problems can also impact the course of the addiction. In that trial, a greater acuity for biomedical problems predicted sustained abstinence. In other words, patients who were more concerned about their own biomedical issues were more likely to achieve sustained abstinence [18].
Discussion
Cocaine use disorder is a highly complex condition involving the convergence of numerous variables that modulate the addiction prognosis. Our findings show that three variables—younger age, more years of cocaine use, and more frequent cocaine use in the previous 30 days—were significant predictors of relapse and treatment dropout [28, 36, 37]. Regarding the first variable, although it is still unclear why younger age is a predictor of treatment dropout, the lower likelihood of younger patients maintaining intake appointments could be explained by various factors. These factors may include extensive research monitoring requirements and a lack of community-based efforts to inform these patients about other treatment alternatives [36]. From the neurobiological perspective, during adolescence, the brain is still under development, especially the prefrontal cortical regions responsible for emotion regulation and adult-level judgement. Consequently, impulsivity increases, placing youths at greater risk of engaging in drug and other risky behaviors [43, 44]. Referring to more years of cocaine use, the longer the duration of cocaine use, the higher the resistance to change. Moreover, the odds of submitting a negative long-term urine sample decreases with every year of cocaine use [31]. Individuals with a long history of cocaine use should receive a differentiated and more intensive treatment protocol, regardless of other severity variables, such as current cocaine use. Finally, greater cocaine use in the previous 30 days at the 18-month follow-up emerges as a significant predictor of subsequent cocaine use, with no other treatment-related factor or social functioning variable showing significant predictive power for subsequent cocaine use. This finding suggests a temporal progression in which factors related to cocaine dependence treatment play a more relevant role at the beginning of treatment, while those related to social functioning, unrelated to treatment, become more important during the follow-up phase [27].
In terms of gender, none of the reviewed studies found gender to be a significant predictor of CUD treatment outcomes, which aligns with the existing literature on this topic [45]. Nevertheless, it is worth highlighting the importance of considering gender-specific variables when approaching treatment and incorporating them into the strategies for addressing specific vulnerable groups. For instance, women who are victims of gender-based violence present a greater risk of engaging in substance use behaviors [46]. Higher baseline craving appears to be predictive of relapse in CUD, but only limited data are available [7, 14, 18]. However, it is important to note that craving can have a different impact depending on the setting where it appears. When craving occurs in hospitalization settings its management do not turn out so complex since there are more available resources to face it (e.g. immediate care from nursing staff, availability of pharmacological options to address craving, etc.). In contrast, when craving occurs in outpatient settings the patient needs to be more trained in accessing craving management abilities and strategies to prevent relapse, which is a more probable outcome due to the lack of immediate resources. Despite this, craving is a widely observable component in real-life clinical practice that predicts worse CUD treatment outcomes. In this regard, it would be interesting to further study the effects of craving on treatment outcomes in CUD in order to better understand the role of this variable and, if appropriate, to specifically target it in psychosocial treatments within outpatient settings. By contrast, fewer withdrawal symptoms predict less cocaine use severity (lower ASI scores) and no self-reported cocaine use in the previous weeks [10, 25], as well as longer abstinence at baseline does [14, 23, 41]. In fact, one study emphasizes the importance of longer abstinence at baseline, indicating that participants who achieved abstinence after one month of treatment were over 14 times more likely to remain abstinent after six months post-treatment than those who used cocaine four weeks after treatment [23]. In terms of self-efficacy levels higher scores were also predictors of continued and long-term abstinence [28]. In spite of this, studies on the impact of self-efficacy on addictions treatment are scant; however, the trial conducted by McKay and colleagues [28] demonstrates how focusing on specific treatments and objectives can be highly effective, thus providing a model for future studies.
The available literature shows that greater impulsivity (measured by the total score of BIS-11) is predictive of more severe addiction and withdrawal symptoms, earlier treatment discontinuation, and greater cocaine use in the month prior to treatment initiation [15, 29, 30], which is aligned with the current evidence [8]. However, in the study conducted by Schmitz and colleagues, [34] the non-planning impulsivity index only predicted two weeks of abstinence, which suggests that the significance of these findings should be considered cautiously. In terms of the presence of concomitant psychopathology, higher scores on scales measuring depressive symptoms are associated with a worse prognosis, including higher drug use severity [28, 35, 36, 38]. In light of these findings, it would be interesting to conduct regular screenings for depressive symptoms to promptly identify changes in symptomatology scores when there is suspicion of an increase or intensification of drug use. By doing so, clinical attention could be improved through tailored interventions that address more explicitly depressive symptoms and prevent adverse outcomes in individuals with cocaine dependence. It is worth noting that this is particularly interesting in women, as literature suggests they are more likely than men to switch from abstinence to cocaine use [28]. Crits-Christoph and colleagues [20] found out that the presence of anhedonia symptoms was a strong predictor of poor treatment response; given these findings, it would be valuable to determine whether other specific depression symptoms have a relevant role in the treatment and prognosis of CUD, which would allow us to specify and tailor the treatment approach to very specific conditions.
Evidence on the predictive capacity of genetic markers in CUD is scant and more research is warranted to investigate the impact of genetic markers on both treatment and prognosis. Nonetheless, there is some evidence that suggests that the patients who carry the Val allele of the COMT Gene Val158met polymorphism are more likely to display three or more weeks of continuous abstinence, as well as a greater percentage of days of abstinence during treatment when undergo a CBT intervention [17].
Although there is no consensus regarding which treatment approach predicts better outcomes in CUD, the limited available data suggest that CM predicts long-term abstinence and higher rates of treatment retention. In other words, individuals who undergo CM have a better prognosis [11, 32, 33, 35].
There is a clear need to better elucidate the most important predictors of treatment outcomes in patients with CUD. In this regard, more research is warranted to study other factors, such as those related to emotion regulation. In real-life clinical practice, the important role of emotion regulation in patients undergoing cocaine detoxification treatment is readily apparent, yet we lack data in clinical settings on the role of emotion regulation in CUD [47]. In this regard, it would be interesting to conduct a study to determine whether this variable can predict treatment outcomes in CUD.
This study has some limitations. First, we screened three databases, and thus only manuscripts indexed in those databases were included, which means some relevant studies may have been missed. Subsequently, based on the conducted bibliographic searches, the authors are not aware of the existence of further studies on the current topic. However, given that these three databases are the largest and most important, the likelihood that we missed any important trials is low. Second, we limited our analysis to RCTs alone, excluding other article types, such as observational studies. The inclusion of other types of studies would have provided more data about the predictors evaluated in this review, or about other potential predictors of treatment outcomes that can be better analyzed through other study designs. Third, we included only manuscripts written in English or Spanish; by excluding studies written in other languages, we may have missed some relevant data. Fourth, due to the risk of bias assessment for the majority of the studies included in this review reporting some concerns, it is worth noting that these results cannot be easily generalized, therefore, they should be interpreted carefully.
A final limitation is that CM was a significant predictor of treatment outcomes but CBT was not. This finding was somewhat surprising, but it may be due to the study aims, which was to identify predictors of treatment outcomes rather than treatment efficiency. CM predicts treatment outcomes regardless of time point at which it is assessed, whereas CBT does not. Importantly, all of the main clinical practice guidelines suggest that CBT is a more efficient treatment for CUD in the long term, whereas CM is more efficient in the short term [2, 3, 5]. In fact, CM is considered the main treatment approach in addictions, especially at the beginning of the treatment. This is why CBT is not described as a predictive factor, even though it is commonly used to treat CUD.
Conclusions
Younger age, more years of cocaine use, and higher craving levels were significant predictors of relapse and treatment dropout. By contrast, fewer withdrawal symptoms, greater baseline abstinence, and more self-efficacy were all predictive of longer duration of abstinence. The role of impulsivity as a predictor of CUD is unclear due to conflicting data, although the evidence generally suggests that higher impulsivity scores can predict more severe addiction and withdrawal symptoms, and earlier discontinuation of treatment.
Availability of data and materials
All data analyzed or generated during this study are presented in the primary research articles reviewed or in this published article.
Abbreviations
- CUD:
-
Cocaine Use Disorder
- CM:
-
Contingency Management
- CBT:
-
Cognitive Behavioral Therapy
- CSSA:
-
Cocaine Selective Severity Assessment
- BIS-11:
-
Barratt Impulsiveness Scale
- RCT:
-
Randomized Controlled Trial
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- DSM-5:
-
Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition
- MINI:
-
Mini International Neuropsychiatric Interview
- PICO:
-
Population, Intervention, Comparison, Outcome
- RoB-2:
-
Cochrane Risk of Bias tool for randomized trials
- LDA:
-
Long Duration of Abstinence
- ASI:
-
Addiction Severity Index
- BDI:
-
Beck Depression Inventory
- APD:
-
Antisocial Personality Disorder
- WCST:
-
Wisconsin Card Sorting Test
- fMRI:
-
Functional Magnetic Resonance Imaging
- dlPFC:
-
Dorsolateral Prefrontal Cortex
- COMT:
-
Catechol-O-Methyltransferase
References
European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2021: Trends and Developments. Off. Eur. Union, Luxemb. 2021. https://www.emcdda.europa.eu/publications/edr/trends-developments/2021_en. Accessed 2 May 2022.
Clinical Guidelines on Drug Misuse and Dependence Update 2017 Independent Expert Working Group. Drug Misuse and Dependence: UK guidelines on clinical management. Department of Health. 2017. https://www.gov.uk/government/publications/drug-misuse-and-dependence-uk-guidelines-on-clinical-management. Accessed 16 Apr 2022.
Petitjean SA, Dürsteler-MacFarland KM, Krokar MC, Strasser J, Mueller SE, Degen B, et al. A randomized, controlled trial of combined cognitive-behavioral therapy plus prize-based contingency management for cocaine dependence. Drug Alcohol Depend. 2014. https://doi.org/10.1016/j.drugalcdep.2014.09.785.
World Health Organization & United Nations Office on Drugs and Crime. International standards for the treatment of drug use disorders: revised edition incorporating results of field-testing. 2020.
Bentzley BS, Han SS, Neuner S, Humphreys K, Kampman KM, Halpern CH. Comparison of treatments for cocaine use disorder among adults: a systematic review and meta-analysis. JAMA Netw Open. 2021. https://doi.org/10.1001/jamanetworkopen.2021.8049.
Carroll K. Terapy Manuals for Drug Addiction, Manual 1: A Cognitive-behavioral Approach: Treating Cocaine Addiction. Rockville: National Institute on Drug Abuse; 1998.
Poling J, Kosten TR, Sofuoglu M. Treatment outcome predictors for cocaine dependence. Am J Drug Alcohol Abuse. 2007. https://doi.org/10.1080/00952990701199416.
Loree AMYM, Lundahl LH, Ledgerwood DM. Impulsivity as a predictor of treatment outcome in substance use disorders: review and synthesis. Drug Alcohol Rev. 2015. https://doi.org/10.1111/dar.12132.
Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; https://doi.org/10.1136/bmj.n71.
Ahmadi J, Kampman K, Dackis C. Outcome predictors in cocaine dependence treatment trials. Am J Addict. 2006. https://doi.org/10.1080/10550490600998476.
Alessi SM, Rash C, Petry NM. Contingency management is efficacious and improves outcomes in cocaine patients with pretreatment marijuana use. Drug Alcohol Depend. 2011. https://doi.org/10.1016/j.drugalcdep.2011.03.001.
Barber JP, Luborsky L, Crits-Christoph P, Thase ME, Weiss R, Frank A, et al. Therapeutic alliance as a predictor of outcome in treatment of cocaine dependence. Psychother Res. 1999;9: https://doi.org/10.1080/10503309912331332591.
Barber JP, Luborsky L, Gallop R, Crits-Christoph P, Frank A, Weiss RD, et al. Therapeutic alliance as a predictor of outcome and retention in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. J Consult Clin Psychol. 2001. https://doi.org/10.1037//0022-006x.69.1.119.
Bisaga A, Aharonovich E, Cheng WY, Levin FR, Mariani JJ, Raby WN, et al. A placebo-controlled trial of memantine for cocaine dependence with high-value voucher incentives during a pre-randomization lead-in period. Drug Alcohol Depend. 2010. https://doi.org/10.1016/j.drugalcdep.2010.04.006.
Blevins D, Wang XQ, Sharma S, Ait-Daoud N. Impulsiveness as a predictor of topiramate response for cocaine use disorder. Am J Addict. 2019. https://doi.org/10.1111/ajad.12858.
Brewer JA, Worhunsky PD, Carroll KM, Rounsaville BJ, Potenza MN. Pretreatment brain activation during Stroop task is associated with outcomes in cocaine-dependent patients. Biol Psychiatry. 2008. https://doi.org/10.1016/j.biopsych.2008.05.024.
Carroll KM, Herman A, Devito EE, Frankforter TL, Potenza MN, Sofuoglu M. Catehol-o-methyltransferase gene Val158met polymorphism as a potential predictor of response to computer-assisted delivery of cognitive-behavioral therapy among cocaine-dependent individuals: Preliminary findings from a randomized controlled trial. Am J Addict. 2015. https://doi.org/10.1111/ajad.12238.
Crits-Christoph P, Gibbons MBC, Barber JP, Hu B, Hearon B, Worley M, et al. Predictors of sustained abstinence during psychosocial treatments for cocaine dependence. Psychother Res. 2007. https://doi.org/10.1080/10503300600818210.
Crits-Christoph P, Johnson JE, Connolly Gibbons MB, Gallop R. Process predictors of the outcome of group drug counseling. J Consult Clin Psychol. 2013. https://doi.org/10.1037/a0030101.
Crits-Christoph P, Wadden S, Gaines A, Rieger A, Gallop R, McKay JR, et al. Symptoms of anhedonia, not depression, predict the outcome of treatment of cocaine dependence. J Subst Abuse Treat. 2018. https://doi.org/10.1016/j.jsat.2018.06.010.
Ehrman RN, Robbins SJ, Cornish JW. Results of a baseline urine test predict levels of cocaine use during treatment. Drug Alcohol Depend. 2001. https://doi.org/10.1016/s0376-8716(00)00137-x.
Gallop RJ, Crits-Christoph P, Ten Have TR, Barber JP, Frank A, Griffin ML, et al. Differential transitions between cocaine use and abstinence for men and women. J Consult Clin Psychol. 2007. https://doi.org/10.1037/0022-006X.75.1.95.
Garcia-Fernandez G, Secades-Villa R, Garcia-Rodriguez O, Alvarez-Lopez H, Sanchez-Hervas E, Ramon Fernandez-Hermida J, et al. Individual characteristics and response to Contingency Management treatment for cocaine addiction. Psicothema. 2011;23:114–8.
Johnson JE, Connolly Gibbons MB, Crits-Christoph P. Gender, race, and group behavior in group drug treatment. Drug Alcohol Depend. 2011. https://doi.org/10.1016/j.drugalcdep.2011.05.023.
Kampman KM, Volpicelli JR, Mulvaney F, Rukstalis M, Alterman AI, Pettinati H, et al. Cocaine withdrawal severity and urine toxicology results from treatment entry predict outcome in medication trials for cocaine dependence. Addict Behav. 2002. https://doi.org/10.1016/s0306-4603(01)00171-x.
McKay JR, Alterman AI, Cacciola JS, Mulvaney FD, O’Brien CP. Prognostic significance of antisocial personality disorder in cocaine- dependent patients entering continuing care. J Nerv Ment Dis. 2000. https://doi.org/10.1097/00005053-200005000-00006.
McKay JR, Merikle E, Mulvaney FD, Weiss RV, Koppenhaver JM. Factors accounting for cocaine use two years following initiation of continuing care. Addiction. 2001. https://doi.org/10.1046/j.1360-0443.2001.9622134.x.
McKay JR, Van Horn D, Rennert L, Drapkin M, Ivey M, Koppenhaver J. Factors in sustained recovery from cocaine dependence. J Subst Abuse Treat. 2013. https://doi.org/10.1016/j.jsat.2013.02.007.
Moeller FG, Dougherty DM, Barratt ES, Schmitz JM, Swann AC, Grabowski J. The impact of impulsivity on cocaine use and retention in treatment. J Subst Abuse Treat. 2001. https://doi.org/10.1016/s0740-5472(01)00202-1.
Nuijten M, Blanken P, Van Den Brink W, Goudriaan AE, Hendriks VM. Impulsivity and attentional bias as predictors of modafinil treatment outcome for retention and drug use in crack-cocaine dependent patients: Results of a randomised controlled trial. J Psychopharmacol. 2016. https://doi.org/10.1177/0269881116645268.
Rash CJ, Alessi SM, Petry NM. Contingency management is efficacious for cocaine abusers with prior treatment attempts. Exp Clin Psychopharmacol. 2008. https://doi.org/10.1037/a0014042.
Rash CJ, Andrade LF, Petry NM. Income received during treatment does not affect response to contingency management treatments in cocaine-dependent outpatients. Drug Alcohol Depend. 2013. https://doi.org/10.1016/j.drugalcdep.2013.03.020.
Rash CJ, Burki M, Montezuma-Rusca JM, Petry NM. A retrospective and prospective analysis of trading sex for drugs or money in women substance abuse treatment patients. Drug Alcohol Depend. 2016. https://doi.org/10.1016/j.drugalcdep.2016.03.006.
Schmitz JM, Mooney ME, Green CE, Lane SD, Steinberg JL, Swann AC, et al. Baseline neurocognitive profiles differentiate abstainers and non-abstainers in a cocaine clinical trial. J Addict Dis. 2009. https://doi.org/10.1080/10550880903028502.
Secades-Villa R, Garcia-Fernandez G, Pena-Suarez E, Garcia-Rodriguez O, Sanchez-Hervas E, Ramon F-H. Contingency management is effective across cocaine-dependent outpatients with different socioeconomic status. J Subst Abuse Treat. 2013. https://doi.org/10.1016/j.jsat.2012.08.018.
Siqueland L, Crits-Christoph P, Frank A, Daley D, Weiss R, Chittams J, et al. Predictors of dropout from psychosocial treatment of cocaine dependence. Drug Alcohol Depend. 1998. https://doi.org/10.1016/s0376-8716(98)00039-8.
Siqueland L, Crits-Christoph P, Gallop R, Barber JP, Griffin ML, Thase ME, et al. Retention in psychosocial treatment of cocaine dependence: Predictors and impact on outcome. Am J Addict. 2002. https://doi.org/10.1080/10550490252801611.
Stulz N, Thase ME, Gallop R, Crits-Christoph P. Psychosocial treatments for cocaine dependence: the role of depressive symptoms. Drug Alcohol Depend. 2011. https://doi.org/10.1016/j.drugalcdep.2010.06.023.
Turner TH, LaRowe S, Horner MD, Herron J, Malcolm R. Measures of cognitive functioning as predictors of treatment outcome for cocaine dependence. J Subst Abuse Treat. 2009. https://doi.org/10.1016/j.jsat.2009.03.009.
Winhusen TM, Theobald J, Lewis DF. Substance use outcomes in cocaine-dependent tobacco smokers: a mediation analysis exploring the role of sleep disturbance, craving, anxiety, and depression. J Subst Abuse Treat. 2019. https://doi.org/10.1016/j.jsat.2018.10.011.
Wong CJ, Anthony S, Sigmon SC, Mongeon JA, Badger GJ, Higgins ST. Examining interrelationships between abstinence and coping self-efficacy in cocaine-dependent outpatients. Exp Clin Psychopharmacol. 2004. https://doi.org/10.1037/1064-1297.12.3.190.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019. https://doi.org/10.1136/bmj.l4898.
Shadur JM, Lejuez CW. Adolescent substance use and comorbid psychopathology: emotion regulation deficits as a Transdiagnostic risk factor. Curr Addict Reports. 2015. https://doi.org/10.1007/s40429-015-0070-y.
Volkow ND, Koob GF, McLellan AT. Neurobiologic advances from the brain disease model of addiction. N Engl J Med. 2016. https://doi.org/10.1056/NEJMra1511480.
Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, Mchugh RK, et al. Substance abuse treatment entry, retention, and outcome in women : a review of the literature. Drug Alcohol Depend. 2007. https://doi.org/10.1016/j.drugalcdep.2006.05.012.
Romo N, Lorena A, Concejero T, Pavón L. Addressing gender - based violence in drug addiction Treatment : a systematic mapping review. Int J Ment Health Addict. 2023. https://doi.org/10.1007/s11469-023-01072-4.
Weiss NH, Kiefer R, Goncharenko S, Raudales AM, Forkus SR, Schick MR, et al. Emotion regulation and substance use: a meta-analysis. Drug Alcohol Depend. 2022. https://doi.org/10.1016/j.drugalcdep.2021.109131.
Acknowledgements
We want to thank the Spanish Ministry of Science, Innovation and Universities, Instituto Carlos III (ISCIII) (FIS PI20/00929) and FEDER funds and Fundació Privada Hospital de la Santa Creu i Sant Pau (Pla d’acció social 2020); without their support this review would not be possible.
Funding
This work was supported by a governmental grant from the Spanish Ministry of Science, Innovation and Universities, Instituto Carlos III (ISCIII) (FIS PI20/00929) and co-funded by FEDER funds and Fundació Privada Hospital de la Santa Creu i Sant Pau (Pla d’acció social 2020). The funding sources have played no role in the study design or preparation of this article.
Author information
Authors and Affiliations
Contributions
AP-L: Conceptualization, methodology, data curation, formal analyses, investigation, visualization, writing – original draft; NM-B: Conceptualization, methodology, funding acquisition, investigation, project administration, supervision, writing – review and editing; JT: methodology, supervision, writing – review and editing; SD-S: writing – review and editing; BC: writing – review and editing; MM: writing – review and editing; FB: writing – review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
13643_2024_2550_MOESM3_ESM.pdf
Additional file 3: Supplement 3. Search strategy, including the use of specific search terms, and reporting the number of identified reports for each search in the three consulted databases.
13643_2024_2550_MOESM4_ESM.pdf
Additional file 4: Supplement 4. Reports that were excluded from the narrative synthesis due to not meeting the selection criteria. These excluded reports are categorized based on the specified criteria.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Palazón-Llecha, A., Caparrós, B., Trujols, J. et al. Predictors of cocaine use disorder treatment outcomes: a systematic review. Syst Rev 13, 124 (2024). https://doi.org/10.1186/s13643-024-02550-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-024-02550-z