Abstract
Background
Chronic postsurgical pain (CPSP) is common following musculoskeletal and orthopedic surgeries and is associated with impairment and reduced quality of life. Several interventions have been proposed to reduce CPSP; however, there remains uncertainty regarding which, if any, are most effective. We will perform a systematic review and network meta-analysis of randomised trials to assess the comparative benefits and harms of perioperative pharmacological and psychological interventions directed at preventing chronic pain after musculoskeletal and orthopedic surgeries.
Methods
We will search MEDLINE, Embase, PsycINFO, CINAHL, and the Cochrane Central Register of Controlled Trials from inception to present, without language restrictions. We will include randomised controlled trials that as follows: (1) enrolled adult patients undergoing musculoskeletal or orthopedic surgeries; (2) randomized them to any pharmacological or psychological interventions, or their combination directed at reducing CPSP, placebo, or usual care; and (3) assessed pain at 3 months or more after surgery. Screening for eligible trials, data extraction, and risk-of-bias assessment using revised Cochrane risk-of-bias tool (RoB 2.0) will be performed in duplicate and independently. Our main outcome of interest will be the proportion of surgical patients reporting any pain at ≥ 3 months after surgery. We will also collect data on other patient important outcomes, including pain severity, physical functioning, emotional functioning, dropout rate due to treatment-related adverse event, and overall dropout rate. We will perform a frequentist random-effects network meta-analysis to determine the relative treatment effects. When possible, the modifying effect of sex, surgery type and duration, anesthesia type, and veteran status on the effectiveness of interventions will be investigated using network meta-regression. We will use the GRADE approach to assess the certainty evidence and categorize interventions from most to least beneficial using GRADE minimally contextualised approach.
Discussion
This network meta-analysis will assess the comparative effectiveness of pharmacological and psychological interventions directed at preventing CPSP after orthopedic surgery. Our findings will inform clinical decision-making and identify promising interventions for future research.
Systematic review registration
PROSPERO CRD42023432503.
Similar content being viewed by others
Background
Chronic pain is a prevalent condition, and its burden is estimated to be large and growing [1, 2]. Approximately, one in four patients undergoing surgery experiences chronic pain [3]. Chronic postsurgical pain (CPSP) is defined as pain at or near the site of surgery that persists for more than 3 months after the procedure, which is not otherwise explained by a preexisting condition or infection [4, 5]. The prevalence of CPSP varies by type of surgery but is particularly common after orthopedic surgeries with estimates ranging from 5% for laminectomy and spinal fusion to 85% following limb amputation [4, 6].
Chronic pain after surgery is associated with reduced psychological and physical health, and quality of life [7]. Often, patients with CPSP require additional treatments and healthcare costs, with some cost estimates exceeding US $1 million per patient over their lifetime [8, 9]. Over 310 million surgical procedures are performed globally each year, of which 40 million are orthopedic [10]. The number of patients suffering from chronic pain after musculoskeletal and orthopedic surgeries is therefore considerable.
Several systematic reviews have explored the effectiveness of treatments for the prevention of CPSP including psychotherapy [11], gabapentinoids [12, 13], antidepressants [14], ketamine [15], opioids [16], nonsteroidal anti-inflammatory drugs (NSAIDs) [17], muscle relaxants [18], acetaminophen [19], and corticosteroids [17, 20]. Most existing trials focus on treatment effects of interventions relative to placebo or usual care; however, comparisons between active therapies are more important when deciding between several competing interventions [21]. Additionally, the multiplicity of interventions available most often leads to separate fragmented meta-analyses, instead of a single big picture identifying superior interventions for optimized clinical decision making [22, 23]. Network meta-analysis (NMA) allows for the estimation of comparative effectiveness among treatment options and combines direct and indirect evidence for each comparison which improves the precision of effect estimates [22, 23]. This is especially helpful when considering interventions informed by trials with small numbers of participants, which is often the case for treatments directed at management of CPSP [17].
There is very limited evidence available on relative benefits and harms of different pharmacotherapies and psychological perioperative interventions for preventing CPSP. The occurrence of CPSP depends on type and approach of surgery [4, 24]. There is also considerable variability in risk factors of CPSP across different surgical procedures [4, 24, 25]. To limit heterogeneity in prognostic factors and relative treatment effects, our review will focus on trials of CPSP after musculoskeletal and orthopedic surgeries. Thus, our objective is to perform a comprehensive review to summarize the evidence from existing randomised controlled trials and assess the relative effects of perioperative interventions to prevent chronic pain after musculoskeletal and orthopedic surgeries.
Methods
Registration and reporting
We reported our protocol according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) guideline [26] and registered it in PROSPERO (CRD42023432503). We will report our findings in an open-access journal following PRISMA-NMA guideline [27].
Eligibility criteria
This review will include randomized trials with any design (parallel, crossover, or cluster randomized). Eligible population will be adult patients (≥ 18 years old) undergoing any type of musculoskeletal or orthopedic surgeries. The eligible interventions include any perioperative pharmacotherapy, any individual-based (therapy delivered to a single individual) or group-based (therapy delivered to a group of individuals treated at the same time) perioperative psychological interventions (e.g., online or in-person [cognitive] behavior therapy, psychoeducation, counseling or supportive therapy, guided imagery therapy, pain coping skills training, relaxation or mindfulness-based therapy, and acceptance and commitment therapy), or their combination, aiming at preventing CPSP. Eligible comparisons include any of the interventions listed above or usual care, placebo, waitlist control, or no treatment. Our main outcome of interest is proportion of patients with CPSP (as defined by International Classification of Diseases, 11th revision (ICD-11) or earlier revisions depending on trial publication date). Other outcomes of interest for our review are proportion of patients with moderate-to-severe CPSP, pain severity, physical functioning or disability, emotional functioning, drop-out rate due to treatment-related adverse events, and overall drop-out rate. We will exclude studies that fail to report any of our outcomes of interest or those that only report overall drop-out rate without any effectiveness outcome.
Studies with patients who underwent a variety of surgical procedures will be included if outcomes are reported separately for musculoskeletal and/or orthopedic surgery patients. Examples of eligible surgical procedures for this review include joint arthroplasty and joint replacement surgeries (due to degenerative or inflammatory diseases, trauma, or overuse injuries), discectomy, fusion surgeries (cervical, lumbar, or joint fusion), spine surgeries, soft tissue repair surgeries (e.g., fasciotomy, muscle repair, reconstruction surgeries for tendons and ligaments), fracture fixation, and osteotomy. We will include multi-arm trials with non-eligible interventions when at least two of the trial arms are eligible.
We will exclude dose-finding trials or those that randomize patients to different dosages of the same drug without any other active comparison, usual care, placebo, no treatment, or waitlist control. We will consult with our clinical experts to determine if a trial used a suboptimal dose or if we need to consider splitting a drug node based on dose. In addition, we will exclude trials comparing psychological interventions or pharmacotherapy combined with other active interventions (e.g., physical therapy, exercise, manual therapy) unless co-interventions were provided to all study participants.
Data sources and search strategy
An experienced medical librarian (R. J. C.) developed database-specific search strategies for MEDLINE, Embase, PsycINFO, CINAHL, and the Cochrane Central Register of Controlled Trials through OVID platform (see Additional file 1). We will perform our searches without publication status or language restrictions from inception to 01 July 2023 and will update them every 3 months until submission of our study for publication through automatic alert services from electronic databases [28]. We will screen the reference list of included trials as well as relevant reviews for additional eligible studies not captured through our searches.
Study selection and data extraction
After removing duplicate records from our electronic database searches, pairs of trained reviewers will screen titles and abstracts independently to identify potentially eligible records using DistillerSR, an online systematic review software (Evidence Partners, Ottawa, Canada; https://www.distillersr.com). Subsequently, the same pairs of reviewers will review full reports independently to confirm eligibility. We will use standardized screening forms and will perform calibration exercises to improve reliability of the screening process. Any disagreements will be resolved through discussion or adjudication by a third reviewer.
Using a standardized form, pairs of reviewers will independently extract relevant information from all eligible studies after performing calibration exercises. We will contact study authors to confirm eligibility and to request missing information when required. Data items to be abstracted will include the following: (i) study characteristics (e.g., author’s name, year of publication, study design, country where participants were enrolled, and source of funding), (ii) patient characteristics (e.g., mean age of participants, proportion of female participants, mean body mass index, proportion of veterans, pain level before surgery, percentage of participants diagnosed with psychiatric disorders), (iii) details of surgical procedure (e.g., type and duration of surgery, anesthesia), (iv) details of intervention and comparisons (e.g., dose, duration, route and frequency of administration), and (v) information on outcomes of interest. All effectiveness outcomes will be extracted and analyzed at three follow-up times, 3 to 6 months, 6 to 12 months, and more than 1 year. For these timepoints, when data is available for more than one follow-up time (e.g., data reported every 1 month), we will extract data from the longest follow-up. The exception will be for drop-out rates, where we will abstract data at the longest follow-up time reported.
For data available only in graphical form, we will estimate the numerical values using a freely available online pixel counting tool, WebPlotDigitizer (https://automeris.io/WebPlotDigitizer). For crossover trials, if there is evidence of period effect, we will only extract data from the first period. For cluster trials, we will calculate effective sample size and apply an intracluster correlation coefficient to the number of events or sample mean for continuous outcomes, as suggested by the Cochrane handbook [29]. Any disagreements will be resolved through discussion or adjudication by a third reviewer.
Risk-of-bias assessment
Pairs of reviewers, working independently, will assess the risk of bias for the effect of assignment to the intervention (i.e., the intention-to-treat effect) for each outcome of interest, in each trial, using the Cochrane risk-of-bias tool (RoB 2.0) [29, 30] which assesses whether studies are at high, low risk of bias, or have some concerns across the following domains: [1] bias from the randomization process, (2) bias due to deviations from the intended interventions, (3) bias due to missing outcome data, (4) bias in measurement of the outcome, and (5) bias in selection of the reported results. Studies will be rated as low overall risk of bias if all domains are at low risk of bias, as high risk of bias if one or more domains are rated at high risk of bias, and as having some concerns in all the other cases. We will use versions of RoB 2 that deal with additional issues that arise in trials with cluster randomised or crossover designs and will use the signalling questions from the archived version of RoB 2.0 embedded in an MS Excel tool for RoB assessments (available from: www.riskofbias.info/welcome/rob-2-0-tool). Any disagreements will be resolved through discussion or adjudication by a third reviewer. RoBvis tool (available from https://mcguinlu.shinyapps.io/robvis) will be used to present a visual summary of risk of bias assessments.
Data synthesis and statistical analysis
For pain severity, physical functioning, and emotional functioning, we will calculate the weighted mean difference and associated 95% CI. We will use change from baseline instead of end-of-study scores, and if change scores are not reported, we will calculate them using the baseline and end-of-study values and the associated standard deviation (SD) using a correlation coefficient derived from other studies as described in the Cochrane handbook [29]. We will use the methods described by Weir et al. [31] to impute means and SDs when only median, (interquartile) range, and sample size are reported, and we are unable to acquire these details from trial authors. When studies use different measurement instruments that capture a common construct (e.g., pain), we will first transform all outcomes to a common instrument score using methods explained by Thorlund et al. [32] prior to meta-analysis.
We will assess the feasibility of performing NMA for each outcome by checking network connectivity, ensuring the availability of more trials than number of intervention nodes and having at least 10 trials in any network, and assessing the transitivity assumption using NMA-studio web application (https://www.nmastudioapp.com) [31]. We will consider the distribution of possible prognostic factors (proportion of female participants, mean body mass index, pain level before surgery, percentage of participants diagnosed with psychiatric disorders, and type of anesthesia) across treatment comparisons to investigate potential intransitivity. When it is not feasible to perform NMA, we will perform conventional pairwise meta-analysis using DerSimonian-Laird random-effects model for any comparison informed by at least two trials. When it is not possible or appropriate to pool results using meta-analysis, we will tabulate and narratively describe any relevant data. Network structure and decisions to lump or split interventions will be based on clinical expert opinion, comparative effects of interventions, and consideration of NMA assumptions (network connectivity, transitivity, and incoherence).
When appropriate to perform NMA, we first calculate direct effect estimates using DerSimonian-Laird random-effects model and will use Cochran’s Q statistic and I2 to determine statistical heterogeneity. For binary outcomes (proportion of patients with CPSP, proportion of patients with moderate-to-severe pain, and drop out rates), we will calculate the pooled relative risk (RR) and the associated 95% confidence interval (CI). We then will use NMA estimates and baseline risks derived from the median risk in placebo arms of included trials to calculate the risk difference (RD) and 95% CIs.
To perform NMA, a contrast-based random-effects model with a common heterogeneity estimate using the methodology of multivariate meta-analysis using “network” suite in Stata will be used for all outcomes [32,33,34]. The “design-by-treatment” model will be used to examine the coherence assumption at network level (global test of coherence). The side-splitting method will be used to assess local (loop-specific) incoherence in each closed network loop as the difference between direct and indirect evidence [32, 35]. If significant incoherence is identified within the network, we will investigate the network for the source(s) of incoherence and subsequently expand or exclude the node(s) introducing incoherence. We will create network diagram at the intervention level to visualize the available evidence and will present league table showing relative effect estimates for all interventions.
When at least 10 trials contribute to a meta-analysis of a direct comparison, we will assess small-study effects for that meta-analysis using Harbord’s test [36] for binary outcomes and Egger’s test [37] for continuous outcomes. To explore the impact of important prognostic factors on network estimates of effect, we will examine the following subgroups when feasible by running network meta-regression: (1) veteran vs nonveteran, (2) sex (male vs female), (3) anesthesia type (local, regional, general, or combination), (4) surgical procedure (major vs minor surgical procedures), and (5) risk of bias (low vs high risk). For all listed subgroups except risk of bias, when available, within-study data will be extracted and analyzed. Stata (StataCorp., Release 17.0, College Station, TX, USA) will be used for all data analyses. All comparisons will be two-tailed using a threshold P-value ≤ 0.05.
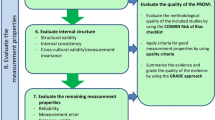
Certainty of evidence assessment
We will follow the GRADE (Grading of Recommendations Assessment, Development and Evaluation) Working Group’s recommended approach to assess the certainty of evidence for each network estimate across different outcomes [38]. This assessment considers both direct and indirect comparisons. Initially, we will evaluate the certainty of direct estimates, based on conventional GRADE guidelines [39, 40] considering the risk of bias, inconsistency, indirectness, and small-study effects. We then will evaluate the certainty of indirect estimates with a focus on the dominant lowest-order loop. Network estimates will be used for precision assessment, and we will use null value as the threshold for imprecision. We may decide to rate the certainty further down if we observe unexplained incoherence between direct and indirect estimates of effect.
GRADE minimally contextualized approach for treatment hierarchy
NMAs often report ranking probabilities and values for surface under the cumulative ranking curves (SUCRA) among competing interventions. However, this approach has important limitations; ranking probabilities and SUCRA values are largely associated with the magnitude of point estimates and ignore the associated precision and certainty of evidence [21, 23]. Thus, we will apply a minimally contextualized approach to develop a treatments hierarchy that takes into consideration the effect estimates from NMA and their certainty of evidence [41, 42].
It is uncommon for a NMA to identify a single intervention that is superior to all others. Therefore, in this approach, interventions are classified into categories from most to least effective. For each outcome, we will classify interventions as follows: group 1, termed “among the least effective,” which includes the reference intervention (e.g., placebo) and any intervention no more effective than the reference; group 2, termed “among the intermediate,” which includes interventions superior to the reference, but not superior to other interventions; and group 3, interventions that prove superior to at least one group 2 intervention, termed “among the most effective.” We will use the same approach for dropouts due to adverse events and all-cause dropouts but will create groups of interventions as follows: (1) no more harmful than the reference, (2) among the intermediate, and (3) among the most harmful. We will then divide interventions in all groups into two categories based on certainty of evidence: those supported by moderate or high certainty evidence and those supported by low or very low certainty evidence.
Discussion
CPSP is a prevalent complication after orthopedic surgery with an important impact on patient function and quality of life. With a current trend and the rate of surgeries, it is not unexpected to see significant rise in the number of patients seeking care to manage CPSP. As such, there is a need for a high-quality review to summarize the evidence on the comparative effectiveness of available perioperative interventions aimed at reducing the development of chronic pain after musculoskeletal and orthopedic surgical procedures.
Most existing trials and current systematic reviews and meta-analyses assess the effectiveness of treatments relative to placebo or usual treatment. Our study will address this limitation by synthesizing novel information about the comparative benefits and harms of available treatments. There is considerable variability in incidence of CPSP across different surgical procedures. Besides the type and approach of surgery, perioperative factors impact the incidence of CPSP. We intend to limit the variability in prognostic factors and reduce the heterogeneity in baseline risks and relative effect of interventions by focusing on musculoskeletal and orthopedic surgeries. Our findings will provide valuable insights to guide optimal pain management strategies and will highlight gaps in current evidence in this area.
Our proposed review will have several strengths. First, our review is restricted to a set of procedures assumed to be associated with higher rate of CPSP, and by limiting the patient population, we had hope to have a more homogeneous set of studies. Second, we will assess the certainty of evidence supporting the effects of interventions using GRADE approach and will apply novel and transparent methods to determine treatment hierarchies. Our review will be limited by the quality of included studies, and the generalizability of our findings to non-orthopedic surgical procedures will be uncertain.
Availability of data and materials
Not applicable.
Abbreviations
- CPSP:
-
Chronic postsurgical pain
- SD:
-
Standard deviation
- NSAID:
-
Nonsteroidal anti-inflammatory drug
- NMA:
-
Network meta-analysis
- RCT:
-
Randomized controlled trial
- SUCRA:
-
Surface under the cumulative ranking curve
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
References
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–59.
Jackson T, et al. A systematic review and meta-analysis of the global burden of chronic pain without clear etiology in low- and middle-income countries: trends in heterogeneous data and a proposal for new assessment methods. Anesth Analg. 2016;123(3):739–48.
Crombie IK, et al. Cut and thrust: antecedent surgery and trauma among patients attending a chronic pain clinic. Pain. 1998;76(1–2):167–71.
Glare P, et al. Transition from acute to chronic pain after surgery. Lancet. 2019;393(10180):1537–46.
Treede RD, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases (ICD-11). Pain. 2019;160(1):19–27.
Richebé P, et al. Persistent postsurgical pain: pathophysiology and preventative pharmacologic considerations. Anesthesiology. 2018;129(3):590–607.
Thapa P, et al. Chronic postsurgical pain: current evidence for prevention and management. Korean J Pain. 2018;31(3):155–73.
Guertin JR, et al. Just how much does it cost? A cost study of chronic pain following cardiac surgery. J Pain Res. 2018;11:2741–59.
Huang A, et al. Chronic postsurgical pain and persistent opioid use following surgery: the need for a transitional pain service. Pain Manag. 2016;6(5):435–43.
Rose J, et al. Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health. 2015;3 Suppl 2(Suppl 2):S13-20.
Wang L, et al. Perioperative psychotherapy for persistent post-surgical pain and physical impairment: a meta-analysis of randomised trials. Br J Anaesth. 2018;120(6):1304–14.
Clarke H, et al. The prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysis. Anesth Analg. 2012;115(2):428–42.
Martinez V, et al. Perioperative pregabalin administration does not prevent chronic postoperative pain: systematic review with a meta-analysis of randomized trials. Pain. 2017;158(5):775–83.
Wong K, et al. Antidepressant drugs for prevention of acute and chronic postsurgical pain: early evidence and recommended future directions. Anesthesiology. 2014;121(3):591–608.
Klatt E, et al. Intra- and postoperative intravenous ketamine does not prevent chronic pain: a systematic review and meta-analysis. Scand J Pain. 2015;7(1):42–54.
Lobova VA, et al. Intraoperative methadone use in cardiac surgery: a systematic review. Pain Med. 2021;22(12):2827–34.
Carley ME, et al. Pharmacotherapy for the prevention of chronic pain after surgery in adults: an updated systematic review and meta-analysis. Anesthesiology. 2021;135(2):304–25.
Choyce A, et al. A systematic review of adjuncts for intravenous regional anesthesia for surgical procedures. Can J Anesth. 2002;49(1):32–45.
McNicol ED, et al. Single-dose intravenous paracetamol or propacetamol for prevention or treatment of postoperative pain: a systematic review and meta-analysis. Br J Anaesth. 2011;106(6):764–75.
Wu H, et al. Can preoperative intravenous corticosteroids administration reduce postoperative pain scores following spinal fusion? A meta-analysis J Invest Surg. 2020;33(4):307–16.
Sadeghirad B, et al. Theory and practice of Bayesian and frequentist frameworks for network meta-analysis. BMJ Evid Based Med. 2023;28(3):204–9.
Rouse B, et al. Network meta-analysis: an introduction for clinicians. Intern Emerg Med. 2017;12(1):103–11.
Salanti G, et al. Introducing the treatment hierarchy question in network meta-analysis. Am J Epidemiol. 2022;191(5):930–8.
Rosenberger DC, et al. Chronic post-surgical pain - update on incidence, risk factors and preventive treatment options. BJA Educ. 2022;22(5):190–6.
Ashoorion V, et al. Predictors of persistent post-surgical pain following total knee arthroplasty: a systematic review and meta-analysis of observational studies. Pain Med. 2023;24(4):369–81.
Moher D, et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Hutton B, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Thomas J, et al. Living systematic reviews: 2. Combining human and machine effort. J Clin Epidemiol. 2017;91:31–7.
Higgins JPT, et al. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions (version 64): John Wiley & Sons. 2023.
Sterne JAC, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Metelli S, et al. NMAstudio: a fully interactive web-application for producing and visualising network meta-analyses. Bern, Switzerland: SRSM Annual Meeting; 2021.
Higgins JP, et al. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Res Synth Methods. 2012;3(2):98–110.
White IR. Network meta-analysis. Stand Genomic Sci. 2015;15(4):951–85.
Chaimani A, et al. Graphical tools for network meta-analysis in STATA. PLoS ONE. 2013;8(10):e76654.
White IR, et al. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res Synth Methods. 2012;3(2):111–25.
Harbord RM, et al. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2006;25(20):3443–57.
Egger M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Brignardello-Petersen R, et al. Advances in the GRADE approach to rate the certainty in estimates from a network meta-analysis. J Clin Epidemiol. 2018;93:36–44.
Guyatt GH, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Puhan MA, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630.
Brignardello-Petersen R, et al. GRADE approach to drawing conclusions from a network meta-analysis using a minimally contextualised framework. BMJ. 2020;371:m3900.
Phillips MR, et al. Development and design validation of a novel network meta-analysis presentation tool for multiple outcomes: a qualitative descriptive study. BMJ Open. 2022;12(6):e056400.
Acknowledgements
The authors would like to thank Karen Dearness of St. Joseph’s Healthcare Hamilton and Maria Tan of the University of Alberta for peer review of the search strategy (PRESS).
Funding
This study is funded by Chronic Pain Centre of Excellence for Canadian Veterans. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
BS is the principal investigator, obtained funding, and will supervise the study. BS and JWB were responsible for the inception and the design of the project. RJC developed all literature database search strategies. AD, IG, MM, JSK, LEC, and BR provided clinical and methodological advice. AT contributed from a patient’s perspective. MAA and KT drafted the manuscript and registered the protocol with PROSPERO. All authors critically reviewed the manuscript for important intellectual content and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
B. Sadeghirad reports receiving research funding from Canadian Institute of Health Research (CIHR) and Michael G. De Groote Institute for Pain Research and Care to perform a review of predictors of postsurgical pain after knee surgery. He has also received funding from PIPRA AG to perform a review of predictors of postoperative delirium. I. Gilron has received funding support from the Canadian Institutes of Health Research SPOR Chronic Pain Network and consultancy fees from CombiGene, GW research, Lilly, and Novaremed. J. W. Busse is funded, in part, by a Canadian Institutes of Health Research Canada Research Chair in Prevention & Management of Chronic Pain. The remaining authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Search strategies for MEDLINE, Embase, PsycInfo, CINAHL, and the Cochrane Central Register of Controlled Trials.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Al-Asadi, M., Torabiardakani, K., Darzi, A.J. et al. Comparative benefits and harms of perioperative interventions to prevent chronic pain after orthopedic surgery: a systematic review and network meta-analysis of randomized trials. Syst Rev 13, 114 (2024). https://doi.org/10.1186/s13643-024-02528-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-024-02528-x